
A Knowledge-based Clinical Decision Support System for Headache
Disorders Management
Maria Carmela Groccia
1 a
, Rosita Guido
1 b
, Domenico Conforti
1 c
and Rosario Iannacchero
2
1
de-Health Lab-Laboratory of Decision Engineering for Health Care Delivery, Department of Mechanical,
Energy and Management Engineering, University of Calabria, Ponte Pietro Bucci 41C, 87036 Rende (Cosenza), Italy
2
Headache Clinic, Neurology Department "Pugliese-Ciaccio" General Hospital,
Viale Papa Pio X 83, 88100 Catanzaro, Italy
Keywords:
Clinical Decision Support System, Headache Diagnosis, Headache Disease, Computer-aided Diagnosis.
Abstract:
Headache is one of the most common neurological problems faced by General Practitioners (GPs) and neu-
rologists. Most of GPs find the diagnosis of headache rather difficult: paper-based guidelines are long and
the diagnostic criteria are complex. Thus, many headache patients do not have an early accurate diagnosis of
headaches’ type and an appropriate treatment. In order to overcome this burden, we present a knowledge-based
Clinical Decision Support System (CDSS) specifically devoted to support GPs in the headache diagnosis and
in the appropriate selection of the diagnostic-therapeutic path. The proposed CDSS has been designed and
developed based on internationally validated guidelines and clinical protocols. The knowledge base contains
the medical-clinical knowledge appropriately formalized in several set of rules. Communication interfaces
compliant with HL7 DSS (Health Level Seven Decision Support Service) international standard were devel-
oped enabling interoperation with other healthcare applications. The CDSS has been tested and assessed in
the GPs’ daily practice of the Calabria Cephalalgic Network. During the evaluation period, a reduced number
of requests for neurological visits and unnecessary and expensive instrumental examinations was registered.
The results obtained from the evaluation period demonstrate that the CDSS turns out to be effective in the
management of headache patients.
1 INTRODUCTION
Headache disorders represent a worldwide problem,
affecting people of all ages, races and geographical
areas (World-Health-Organization, 2016). In Italy,
according to a survey by National Institute of Statis-
tics, the recurrent headache is one of the chronic dis-
eases with higher incidence. It is fourth after arthri-
tis, arterial hypertension and allergic diseases (Istat,
2015). Notwithstanding, many patients with chronic
headaches do not receive effective treatment, mainly
due to the underestimation of the impact of the disease
and to the complexity of diagnostic criteria (World-
Health-Organization, 2016). As a negative conse-
quence, headache attacks are very often self-managed
by patients that progressively increase the assump-
tion of analgesics until they reach a condition of
medication-overuse (Elkind, 1991).
a
https://orcid.org/0000-0001-7570-8458
b
https://orcid.org/0000-0003-1744-2166
c
https://orcid.org/0000-0002-4816-4333
The General Practitioner (GP) has a central role
in the headache diagnosis process as the GP has the
first contact with the patient making a first diagno-
sis. The GP can effectively treat the majority of pa-
tients with headache disorders; only a minor group
requires higher medical specializations as a neurolo-
gist or advanced instrumental examinations (Steiner
et al., 2007). For this reason, it is strategically impor-
tant that the GP be able to make an accurate diagnosis
and therefore has a deep knowledge of the diagnostic
criteria. In this way, patients can immediately get an
effective treatment, reduce pain and discomfort.
A Clinical Decision Support System (CDSS)
could get a great advantage over paper-based proto-
cols and guidelines. Paper-based guidelines to sup-
port headache diagnosis are typically long and diffi-
cult to memorize or refer during patient interviews. A
CDSS instead, has many advantages because it can:
(1) assists the GP for an accurate symptoms’ detec-
tion; (2) provide an accurate support in processing a
large number of data, and (3) offer a level of speci-
Groccia, M., Guido, R., Conforti, D. and Iannacchero, R.
A Knowledge-based Clinical Decision Support System for Headache Disorders Management.
DOI: 10.5220/0010238604010408
In Proceedings of the 14th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2021) - Volume 5: HEALTHINF, pages 401-408
ISBN: 978-989-758-490-9
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
401

ficity for individual patient that is nearly hard to get
by using a paper-based guideline.
In this paper, we design, develop, and evaluate
a knowledge-based CDSS able to support the GP
both in the headache diagnosis and the choice of
best diagnostic-therapeutic path according to patient’s
symptoms. The CDSS uses a rule-based approach.
It has been designed and developed based on inter-
nationally validated guidelines and clinical protocols.
Communication interfaces compliant with HL7 DSS
(Health Level Seven Decision Support Service) inter-
national standard were developed in order to enable
the interoperation with other healthcare applications.
Results from the evaluation of the CDSS in the man-
agement of the Calabria Cephalalgic Network clinical
workflow are presented.
The paper is organized as follows. Section 2 in-
troduces the background on headache disorders and
the main works on CDSSs. Section 3 presents
the Calabria Cephalalgic Network healthcare context.
Section 4 describes the proposed CDSS. Section 5
presents results and a brief discussion. Finally, Sec-
tion 6 concludes the paper.
2 BACKGROUND
As reported in the International Classification of
Headache Disorders (ICHD) published by the In-
ternational Headache Society (IHS) (IHS, 2018),
there are three main categories of headache disor-
ders: primary headaches; secondary headaches and
painful cranial neuropathies; other facial pains and
other headaches. Each category is divided into
sub-categories. The three major primary headache
sub-categories are migraine (with and without aura),
tension-type headache, and cluster headache. Sec-
ondary headaches are due to other disorders (the
so-called comorbidities) such as infections or trau-
mas cranium. In addition, a secondary headache
can be attributed to a substance or its withdrawal,
e.g. medication-overuse headache. In severe cases,
a headache is often an initial warning symptom of se-
rious diseases such as an ischaemic or haemorrhagic
stroke. In these cases, headaches appear along with
other warning symptoms.
In the literature, several tools have already been
proposed and developed to support health profes-
sionals in the diagnosis of headache disorders (Potter
et al., 2018; Aljaaf et al., 2018). Some tools have
been developed to classify only one type of headache.
For instance, the CDSS presented in (Kopec et al.,
2004) is a rule-based expert system that supports clin-
icians to migraine diagnosis. The rules are rep-
resented in the C Language Integrated Production
System. Other tools support clinicians in the diagno-
sis of multiple headache types. The CDSS developed
in (Yin et al., 2015) is specialized to diagnose
migraine and tension-type headaches. It is based
on case-based reasoning. Previous solved cases are
stored in a built-in library, and a k-nearest neighbour
algorithm is used to measure similarity among cases.
More complex is the hybrid system based on both
rules and case-based reasoning in (Yin et al., 2014).
This system is useful to diagnose the main primary
headaches, i.e., migraine, tension-type headache,
and cluster headache: First, patients’ symptoms
are evaluated in a rule-based module and only if a
diagnosis cannot be suggest, the system searches
for the most similar previous case in a case-based
module. Migraine and other secondary headache
diseases can be diagnosed by the CDSS in (Zafar
et al., 2013). An image processing module is also
included to detect brain tumour from MRI scans. A
knowledge-based system that uses yes/no questions
derived from neurology experts is the CDSS in
(Hasan et al., 2012). More specifically, neurologist’s
knowledge has been converted in a tree diagram.
Guideline-based systems are presented in (Simi
´
c
et al., 2008; Eslami et al., 2013; Dong et al., 2014).
The second version of ICHD criteria were codified in
the CDSS of (Eslami et al., 2013) to classify the main
types of primary headaches (i.e., migraine, tension-
type headache and cluster headache). This CDSS pro-
poses a questionnaire to patients and implements a
simple human-like algorithmic reasoning. The same
version of ICHD criteria were also codified in (Simi
´
c
et al., 2008); the difference is that the developed
CDSS uses a fuzzy logic as implementation technol-
ogy. The third version of ICHD criteria were imple-
mented in the CDSS in (Dong et al., 2014): clinicians
are assisted to diagnose primary headache disorders
and medication-overuse headaches.
The CDSSs developed in (Krawczyk et al., 2013;
Çelik et al., 2015; Keight et al., 2017) are on machine
learning techniques based. In (Krawczyk et al., 2013),
the authors defined the diagnosis of primary headache
as a classification task. They compared three fea-
ture selection techniques and several classifiers on the
same set of patients. In (Keight et al., 2017) nine
machine learning based classifiers are compared on a
dataset consisting of primary headaches, and the best
predictive performance was achieved by a stacking
classifier. In (Çelik et al., 2015) Artificial Immune
Systems were used as classification algorithms to di-
agnose migraine, tension-type headache, and cluster
headaches. A further extension of this work evalu-
HEALTHINF 2021 - 14th International Conference on Health Informatics
402
ates an ant-colony optimization algorithm on the same
dataset (Celik and Yurtay, 2017).
The CDSS in (Vandewiele et al., 2018) is one of
the most recent systems for the diagnosis and classi-
fication of the headache disorders. It implements an
automated diagnosis support module that generates an
interpretable decision tree based on data semantically
annotated with expert knowledge.
To summarize, the analysed systems use different
sources of knowledge, architecture and implementa-
tion technology to diagnose headaches. Nevertheless,
these tools support clinicians in headache diagnosis
but not in patient management after a diagnosis. As
a result, in many cases GPs refer patients to headache
specialists for unnecessary examinations.
To the best of our knowledge, there are cur-
rently no systems allowing complete screening of
headaches, that is, primary headache, secondary
headache, and warning symptoms in primary care.
3 CALABRIA CEPHALALGIC
NETWORK: INNOVATION IN
THE CLINICAL WORKFLOW
MANAGEMENT
The Calabria Cephalalgic Network represents a novel
healthcare delivery context. It has been designed in
Calabria (Italy) and it is based on a patient-centred
integrated approach. Its main objective concerns the
management of headache patients through personal-
ized care pathways, ensuring continuity of care at dif-
ferent levels of diagnostic-therapeutic paths.
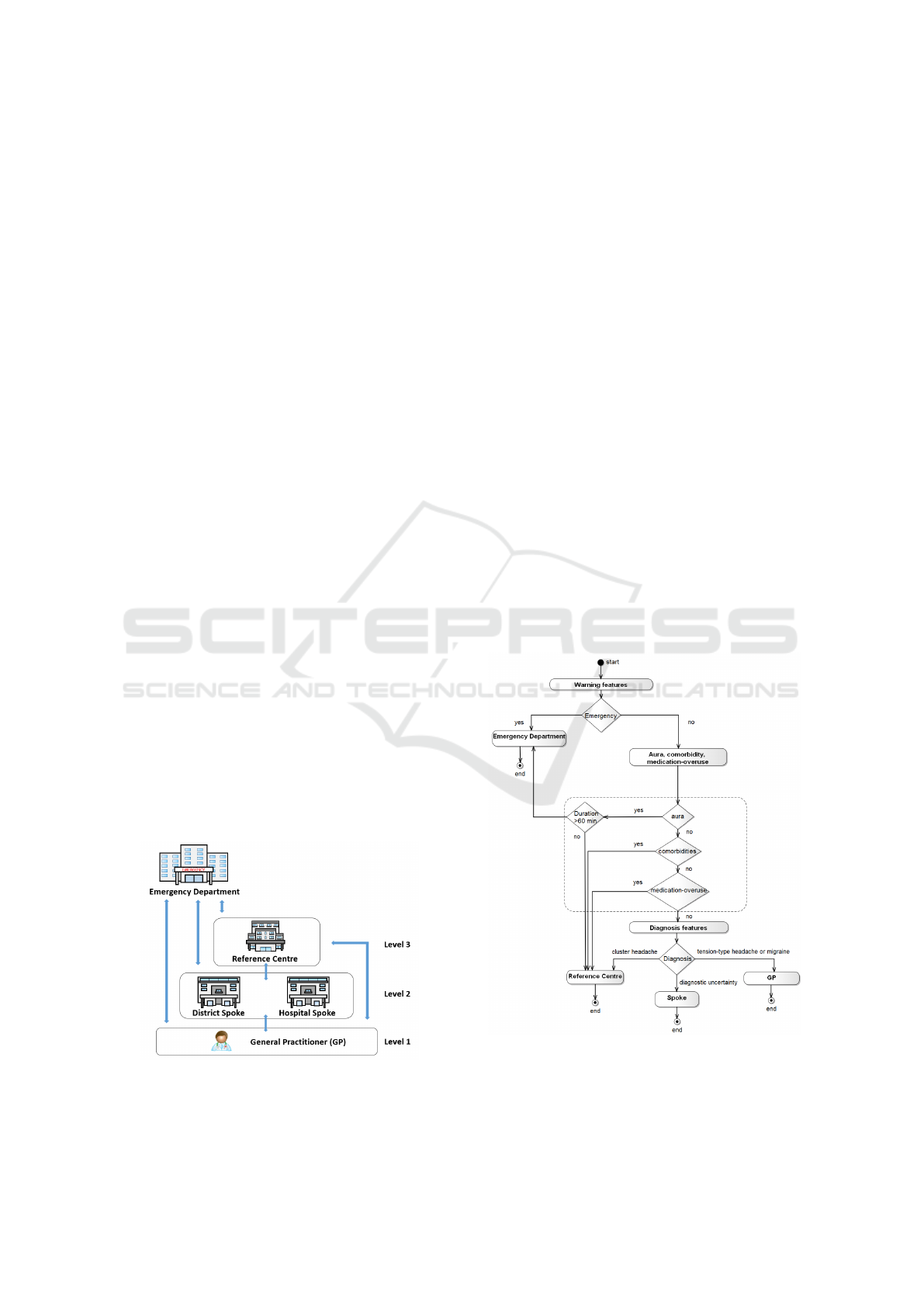
The architectural organization of the network is
reported in Figure 1. The network is organized in
three levels: GPs, Spokes and Reference Centres. All
the levels interact with Emergency Department.
Figure 1: Organization of Calabria Cephalalgic Network.
GPs are in the first level. They represent the core
node of the network since they have the first contact
with patients. GPs acquire patient’s signs and symp-
toms through clinical interviews and refer the patient
to the most appropriate diagnostic-therapeutic path.
In case of diagnostic uncertainty and/or ineffective-
ness of the prescribed therapy, the GPs interact with
the second level; in more complex situations, such
as for instance, headache with aura, serious comor-
bidities, cluster headaches, and medication-overuse
headaches, the GPs interact with the third level.
District Spoke and Hospital Spoke are in the
second level. The District Spoke manages patients
needing specialized clinical assessments, whereas the
Hospital Spoke manages patients needing deeper as-
sessments based on instrumental investigations.
The Reference Centre is the third level. It mainly
manages patients with comorbidities, headaches with
aura focusing on rehabilitation of patients with
medication-overuse headaches. Moreover, it man-
ages patients with cluster headaches and coming from
Spoke with diagnostic uncertainty.
It is important to remark that, at each level, health
professionals follow evidence based specific guide-
lines for patient care, facilitating the coordination
with other health professionals.
Figure 2 shows the GPs’ clinical workflow in the
Calabria Cephalalgic Network.
Figure 2: Clinical workflow for the GPs in the Calabria
Cephalalgic Network.
A Knowledge-based Clinical Decision Support System for Headache Disorders Management
403
The GPs’ clinical workflow can be summarised
as follows. At the baseline visit, a GP has to im-
mediately assess possible emergency conditions. In
case of warning symptoms, the GP refers the patient
to the Emergency Department. Otherwise, the clini-
cal investigation continues and the GP assesses aura
symptoms. If each individual aura symptom lasts less
than 60 minutes, the patient should be referred to the
Reference Centre; otherwise, to the Emergency De-
partment. If there are not aura symptoms, the GP
assesses comorbidities and medication-overuse: se-
rious comorbidities or medication-overuse headaches
prompt the GP to refer the patient to the Reference
Centre. The GP will be able to identify primary
headache subtypes only if all of the health condi-
tions described so far have been ruled out: patients
with cluster headaches should be referred to the Ref-
erence Centre; patients in case of diagnostic uncer-
tainty should be referred to the Spoke; with diagnosis
of migraine or tension-type headache are treated by
the GP.
4 CDSS DESIGN AND
DEVELOPMENT
The CDSS was designed to support GPs in the diag-
nosis and choices of therapeutic paths in a primary
care context. It is fully compliant with clinical guide-
lines and diagnostic-therapeutic paths applied within
the Calabria Cephalalgic Network.
The development of the CDSS followed an itera-
tive approach involving engineers, GPs and neurolog-
ical specialists who collaborated to identify functional
requirements. First, the guideline recommendations
were combined with expert knowledge to determine
system responses based on patient data. Then, the
communication interfaces of the system were devel-
oped.
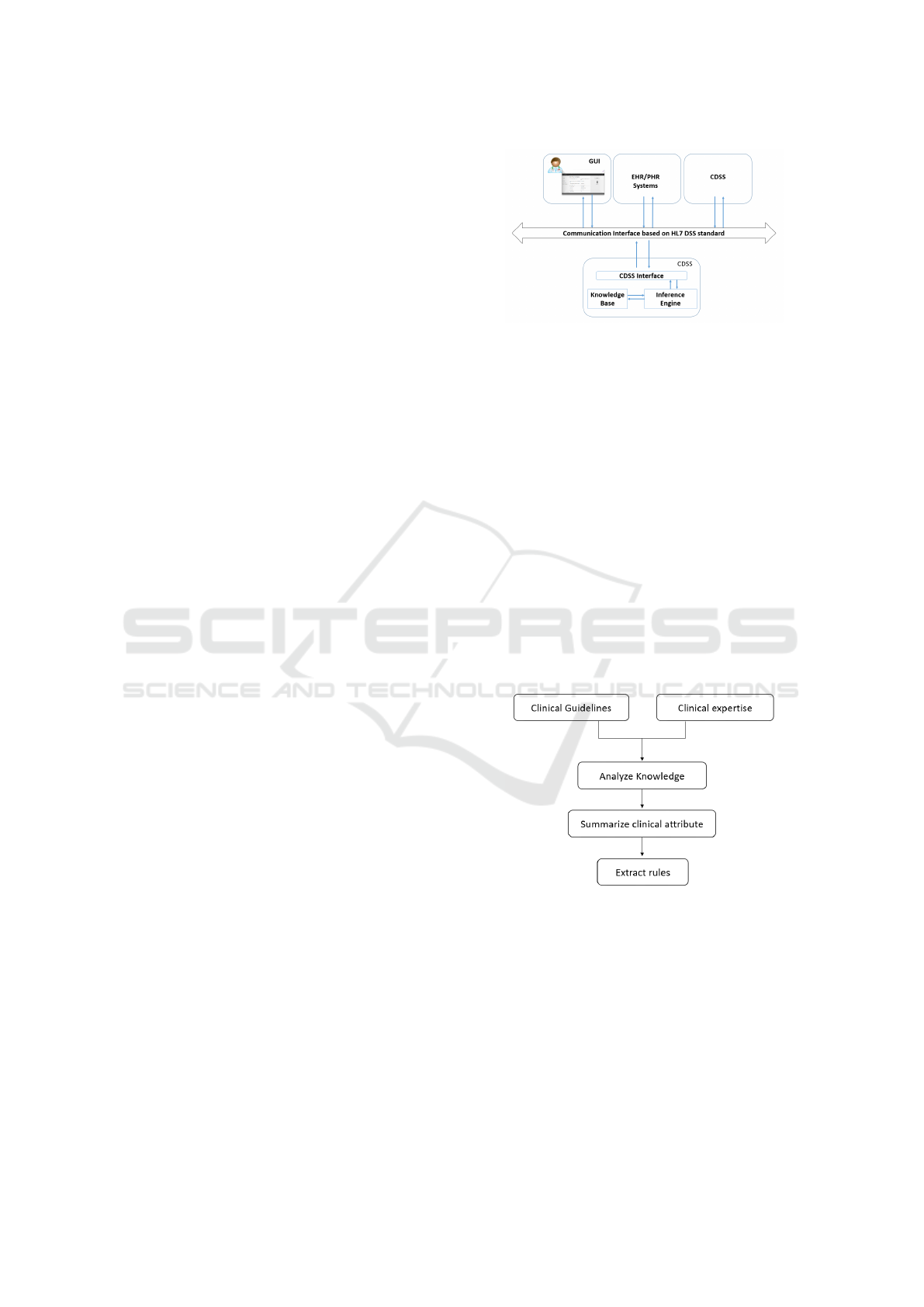
The general architecture of the proposed CDSS is
reported in Figure 3. The CDSS consists of three main
components: knowledge base, inference engine and
CDSS interface. Communication interface and GUI
(Graphical User Interface) complete the architecture
of the system. The CDSS was designed to work in
a collaborative environment. According to this vi-
sion, a user is any external entity that interacts with
the CDSS such as a GUI, another CDSS, an electronic
medical record or any other component and service of
the health environment.
The three main components of the CDSS, the
communication interface and GUI are described in the
next sections. The CDSS interface receives and vali-
Figure 3: CDSS Architecture.
dates the patient data contained in each request.
If the data is correct, it activates the inference engine.
4.1 Knowledge Base
The knowledge base contains the medical-clinical
knowledge appropriately formalized by the relevant
sets of rules. The National Institute for Health
and Care Excellence (NICE) Clinical Guideline for
headache disorders (Carville et al., 2012), the work-
flow of the GPs and health professionals’ experiences
in the Calabria Cephalalgic Network, were appropri-
ately coded as sources of knowledge.
The clinicians’ expertise and their suggestions
have been obtained through various interviews with
both GPs and neurologists.
All rules were coded as IF-THEN statements in
the Java programming language.
Figure 4: Knowledge Acquisition Process.
Figure 4 summarizes the adopted process of
knowledge acquisition for the headache disorders di-
agnosis. First, knowledge from different sources
have been acquired, analysed and expressed in sev-
eral flowcharts. Each flowchart has been validated
by clinicians. Then, headache clinical attributes have
been defined and summarized. The acquired knowl-
edge has been translated in a set of conditional rules.
According to the diagnostic and therapeutic paths
of the Calabria Cephalalgic Network, five sets of
rules have been codified for the diagnosis of headache
HEALTHINF 2021 - 14th International Conference on Health Informatics
404

disorders such as primary headaches (migraine, ten-
sion type and cluster headache), warning symptoms,
aura’s symptoms, comorbidities, medication-overuse
Table 1: Headache features used to create the diagnostic
rules.
Diagnosis Features
Warning
events
Headache that begins after age 50
Headaches increasing in
frequency, duration and severity
Headache subsequent to head
trauma in the previous 3 months
Unusual headache accompanied
by fever and rigor nucalis
Headache with physical exertion
(coughing, sneezing)
Paresthesia of lower limb
Anticoagulant therapy
Limb strength deficit
Sensory deficits
Disorders of consciousness
Speech disorders
Visual disturbances
Disorders of vigilance
Aura,
Comorbidity,
Medication-
overuse
Flashes of light
Lines
Scotomas or spots
Aura duration
Paresthesia
Language disorders
Regular overuse for > 3 months
of one or more drugs
Endocrine and metabolic disorders
Cardiovascular disease
Psychiatric disorders
Severe hypertension
Primary
headache
Pain Location
Pain Quality
Pain Intensity
Effect on activities
Duration of headache
Frequency of headache
Red eye
Watery eye
Nasal congestion
Runny nose
Swollen eyelid
Forehead and facial sweating
Constricted pupil
Drooping eyelid
Vomiting
Nausea
Photophobia
Phonophobia
headaches. Rules for the management of the patient’s
therapeutic path have also been coded. Table 1 reports
the headache features used to create the diagnostic
rules. Table 2 reports one rule for cluster headache
diagnosis.
Each headache clinical attribute is designed as cat-
egorical and identifies the allowed values. Table 3
lists the primary headache categorical attributes.
Table 2: One rule for cluster headache diagnosis.
Rule
Name
Rule Condition
Rule 1 IF (Criterion 1 AND Criterion 2
AND Criterion 3 AND Criterion 4
AND Criterion 5 AND Criterion 6
AND Criterion 7)
THEN Cluster Headache
Criterion 1 IF (Pain Location=Unilateral)
THEN true
Criterion 2 IF (Pain Quality=Variable)
THEN true
Criterion 3 IF (Pain Intensity=Severe
OR Pain Intensity=Very severe)
THEN true
Criterion 4 IF (Effect on activities=Restlessness
OR Effect on activities=Agitation)
THEN true
Criterion 5 IF (Other symptoms=Red eye
OR Other symptoms=Watery eye
OR Other symptoms=Nasal congestion
OR Other symptoms=Runny nose
OR Other symptoms=Swollen eyelid
OR Other symptoms=Forehead and
facial sweating
OR Other symptoms=Constricted pupil
OR Other symptoms=Drooping eyelid)
THEN true
Criterion 6 IF (Duration of headache=
15-180 minutes) THEN true
Criterion 7 IF (Frequency of headache=
1 every other day to 8 per day)
THEN true
4.2 Inference Engine
The inference engine receives and manages all the re-
quests coming via the CDSS interface. Based on the
input patient data, it identifies and activates specific
sets of rules for obtaining a decision support, as illus-
trated in Figure 5. It firstly searches for all the possi-
ble rules that match with the patient input data in the
knowledge base. Then, the execution of the selected
A Knowledge-based Clinical Decision Support System for Headache Disorders Management
405
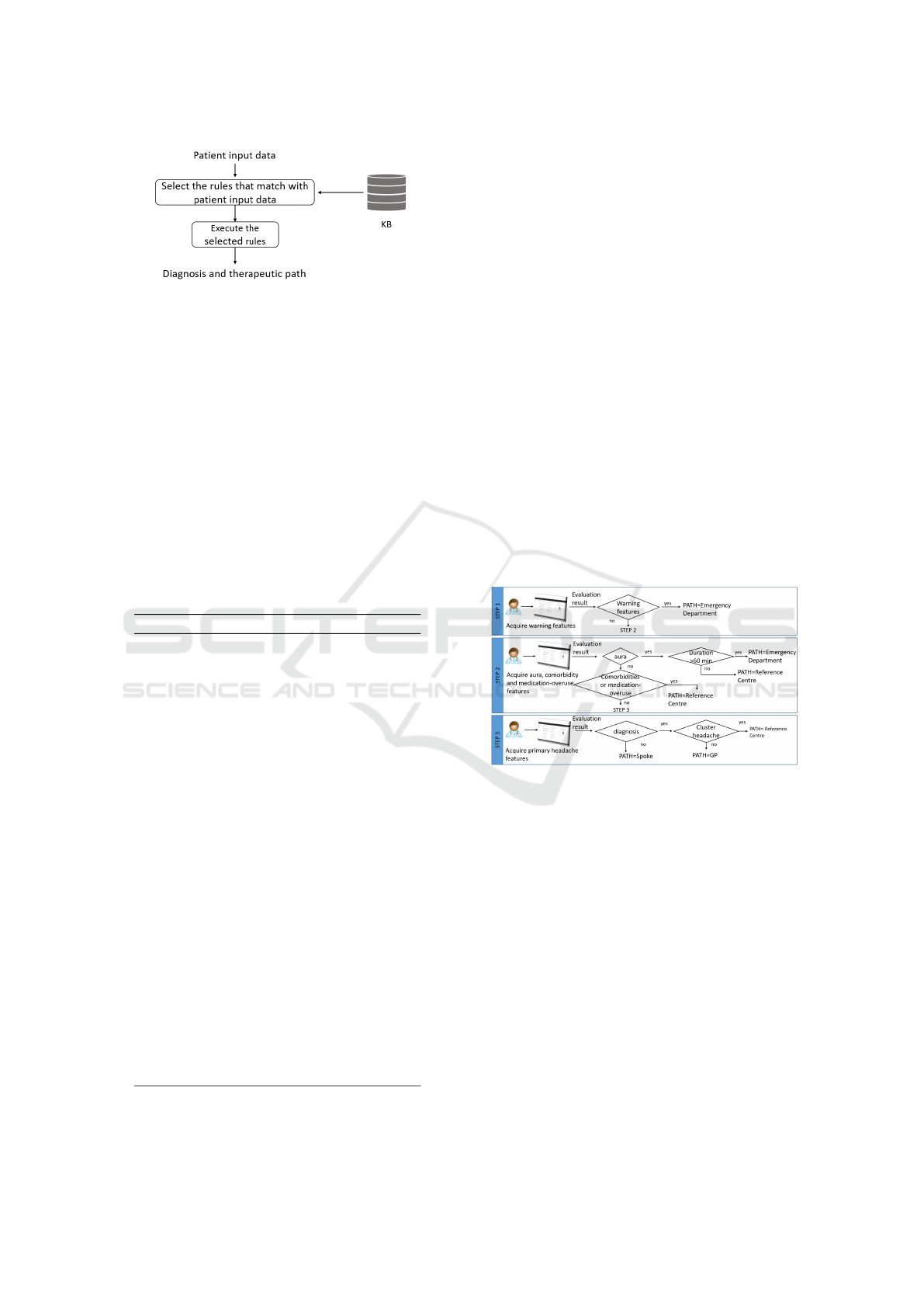
Figure 5: Workflow of the Inference Engine.
rules starts. It returns the patient-specific diag-
nosis and therapeutic path on the basis of satisfied
rules.
4.3 Communication Interface
The CDSS communication interface was developed
as SOAP web service compliant with the HL7 DSS
international standard (HL7DSS, 2017). It defines a
standard interface for decision support applications,
regardless of data format, inference mechanisms and
implementation technology. The HL7 DSS stan-
dard guarantees the interoperability of the CDSS with
other applications in the healthcare environment.
Table 3: Primary headache categorical values.
Variable Allowed values
Pain Location Bilateral, Unilateral,
Mono/Bilateral
Pain Quality Pulsating, Variable,
Pressing/tightening
(non-pulsating)
Pain Intensity Mild, Moderate,
Severe, Very severe
Effect on
activities
Not aggravated
by routine activities,
Aggravated
by routine activities,
Restlessness, Agitation
Other
symptoms
Photophobia, Phonophobia,
Nausea, Vomiting,
Red eye, Watery eye,
Nasal congestion, Runny nose,
Swollen eyelid,
Forehead and facial sweating,
Constricted pupil,
Drooping eyelid
Duration of
headache
30 minutes-continuous,
4-72 hours, 15-180 minutes
Frequency of
headache
< 15 days per month,
> 15 days per month,
1 every other day to 8 per day
4.4 Graphical User Interface
The GUI has three main parts including warning
symptoms questions page, aura, comorbidity and
medication-overuse symptoms question page, pri-
mary headache symptoms question page. A decision
page where patient-specific diagnosis and therapeutic
path are explained, have been implemented. The first
diagnostic web page is the warning symptoms ques-
tion page. The GP inserts patient data in appropriate
fields. The data are thus evaluated by the CDSS. If no
alert is detected, the GP can continue the diagnostic
process and the second question page is shown; other-
wise, the decision page is presented with the patient-
specific diagnostic path. The second diagnostic page
concerns aura, comorbidity and medication-overuse
symptoms question page. The GP fills in the fields
with patients’ clinical characteristics, which are eval-
uated by the CDSS. If no clinical condition is de-
tected, the GP can continue the diagnostic process.
The third page is the primary headache symptoms
question page. After the evaluation of the CDSS, the
final decision page is presented to the GP. Figure 6
shows the three diagnostic steps. The web pages are
Figure 6: Diagnostic steps.
both Italian and English language. Figure 7 shows the
primary headache symptoms question page.
4.5 Functional Specifications
When a patient assessment is required, the GP sends a
request message to the CDSS, via GUI, to activate the
clinical decision support. The requested data are for-
warded to the inference engine through the CDSS’s
interface. The inference engine, based on the submit-
ted data, identifies the more appropriate rules set in
the knowledge base and performs it. The CDSS re-
turns the diagnostic and the patient care path sugges-
tions to the GUI.
The proposed CDSS is a plug and play system
based on the Service Oriented Architecture paradigm
(Erl, 2005); it has been modelled following the Model
Driven Architecture methodology (MDA, 2012).
HEALTHINF 2021 - 14th International Conference on Health Informatics
406

Figure 7: GUI for the diagnosis of primary headache type.
As regards privacy and data protection, the CDSS
does not use patient identification data and bidirec-
tional communication data is encrypted.
5 RESULTS AND DISCUSSION
To investigate the performance of the proposed
CDSS, we firstly performed an assessment of the sys-
tem on available datasets. In order to measure the
effectiveness of the proposed CDSS in the primary
headache diagnosis, we used a publicly available
dataset hosted on http://www.migbase.com/migbase_
dataset.xls. The dataset contains answers to question-
naires of 850 patients with headache problems. A
neurologist labelled each sample in migraine, tension-
type headache, and cluster headache; only one sam-
ple has been labelled as no headache. The pro-
posed CDSS correctly recognized 609/609 (100%)
patients with migraine, 155/184 (84.23%) patients
with tension-type headache, and 55/56 (98.21%) pa-
tients with cluster headache. Overall, the CDSS cor-
rectly recognized 816 (96%) patients; suggested di-
agnostic uncertainty and further clinical investigation
for 25 (2.94%) patients, whereas only 9 (1.06%) pa-
tients were misclassified. Because no real data was
available, we produced realistic test data for different
types of secondary headaches and warning symptoms.
Although the use of real data was clearly preferable,
the use of this data allowed us to test all rule sets im-
plemented under the supervision of a clinical expert.
The dataset consists of 10 cases. The CDSS classified
correctly all the cases.
We further explored the use of the CDSS in a real
healthcare setting. The CDSS has been deployed in
the Calabria Cephalalgic Network and experimentally
evaluated in daily practice by the GPs during a period
of 5 months. The real case study involved 10 GPs, 1
Reference Centre, 3 Spokes, and 80 patients. Before
the practical evaluation, the CDSS was presented at
GPs during several training events. The GPs were in-
terviewed during the evaluation period and at the end,
in order to judge the performance of the CDSS and its
impact in a daily practice. Interviews were also con-
ducted with the Spoke and the Reference Centre to
evaluate how neurologists and GPs managed patients.
GPs considered the CDSS useful and were satisfied
by its performance: the CDSS is easy to use, patients
data is collected in a short time, the given support
in diagnosis is fundamental especially for complex
cases. Compared to the previous 5 months, the neu-
rologists of the Reference Centre recorded a reduction
of accesses for episodic migraine diagnosis during the
evaluation period, i.e., 12.5% vs 5%. This result sug-
gests an improvement in management of patients with
headache for the GP and therefore, a reduced demand
for unnecessary and expensive instrumental examina-
tions. The proposed CDSS really supports GPs to
manage patients with headaches. As a consequence, a
more appropriate use of healthcare resources there is.
6 CONCLUSIONS
This paper has presented a knowledge-based CDSS to
support GPs for the integrated clinical management
A Knowledge-based Clinical Decision Support System for Headache Disorders Management
407

of headache patients. The knowledge base codes the
NICE Clinical Guideline for headache disorders, the
GP clinical workflow and the clinical best practices
from the Calabria Cephalalgic Network. Communi-
cation interfaces are compliant with HL7 DSS inter-
national standard in order to guarantee interoperabil-
ity with other healthcare applications.
The CDSS has been assessed in the GPs’ daily
practice of the Calabria Cephalalgic Network. The
preliminary results are promising. They confirm an
improvement in the management of patients with
headache within primary care facilities. The CDSS
effectively supports GPs in dealing with a patients
headache diagnosis by reducing diagnosis time on the
one hand, even during the anamnesis phase, inappro-
priate accesses to the Spokes and Reference Centre,
and patient’s expenses on the other hand for headache
treatments.
REFERENCES
Aljaaf, A. J., Mallucci, C., Al-Jumeily, D., Hussain, A.,
Alloghani, M., and Mustafina, J. (2018). A study
of data classification and selection techniques to di-
agnose headache patients. Applications of Big Data
Analytics, page 121.
Carville, S., Padhi, S., Reason, T., Underwood, M., Group,
G. D., et al. (2012). Diagnosis and management of
headaches in young people and adults: summary of
NICE guidance. BMJ, 345:e5765.
Celik, U. and Yurtay, N. (2017). An ant colony optimization
algorithm-based classification for the diagnosis of pri-
mary headaches using a website questionnaire expert
system. Turkish Journal of Electrical Engineering &
Computer Sciences, 25(5):4200–4210.
Çelik, U., Yurtay, N., Koç, E. R., Tepe, N., Güllüo
˘
glu,
H., and Erta¸s, M. (2015). Diagnostic accuracy com-
parison of artificial immune algorithms for primary
headaches. Computational and mathematical meth-
ods in medicine, 2015.
Dong, Z., Yin, Z., He, M., Chen, X., Lv, X., and Yu, S.
(2014). Validation of a guideline-based decision sup-
port system for the diagnosis of primary headache
disorders based on ICHD-3 beta. The journal of
headache and pain, 15(1):40.
Elkind, A. H. (1991). Drug abuse and headache. The Med-
ical clinics of North America, 75(3):717–732.
Erl, T. (2005). Service-oriented architecture: concepts,
technology, and design. Prentice Hall.
Eslami, V., Rouhani-Esfahani, S., Hafezi-Nejad, N., Re-
faeian, F., Abdi, S., and Togha, M. (2013). A comput-
erized expert system for diagnosing primary headache
based on international classification of headache dis-
order (ICHD-II). SpringerPlus, 2(1):199.
Hasan, M. R., Hasan, M. S., and Siraj, F. (2012). An ex-
pert system based headache solution. In Computer Ap-
plications and Industrial Electronics (ISCAIE), 2012
IEEE Symposium on, pages 287–292. IEEE.
HL7DSS (2017). http://www.hl7.org/implement/standards/
product_brief.cfm?product_id=12.
IHS (2018). http://www.ihs-headache.org/ichd-guidelines.
Istat (2015). http://www.istat.it/it/files/2015/09/
Dimensioni-salute.pdf?title=Le+dimensioni+della+
salute+in+Italia+-+16%2Fset%2F2015+-+Volume.
pdf.
Keight, R., Aljaaf, A. J., Al-Jumeily, D., Hussain, A. J.,
Özge, A., and Mallucci, C. (2017). An intelligent
systems approach to primary headache diagnosis. In
International Conference on Intelligent Computing,
pages 61–72. Springer.
Kopec, D., Shagas, G., Selman, J., Reinharth, D., and
Tamang, S. (2004). Development of an expert sys-
tem for aiding migraine diagnosis. J Inform Technol
Healthcare, 200:355.
Krawczyk, B., Simi
´
c, D., Simi
´
c, S., and Wo´zniak, M.
(2013). Automatic diagnosis of primary headaches by
machine learning methods. Open Medicine, 8(2):157–
165.
MDA (2012). http://www.omg.org/mda/.
Potter, R., Probyn, K., Bernstein, C., Pincus, T., Un-
derwood, M., and Matharu, M. (2018). Diagnos-
tic and classification tools for chronic headache dis-
orders: a systematic review. Cephalalgia, page
0333102418806864.
Simi
´
c, S., Simi
´
c, D., Slankamenac, P., and Simi
´
c-Ivkov, M.
(2008). Rule-based fuzzy logic system for diagnosing
migraine. In Hellenic Conference on Artificial Intelli-
gence, pages 383–388. Springer.
Steiner, T. J., Jensen, R., Katsarava, Z., Linde, M., MacGre-
gor, E. A., Osipova, V., Paemeleire, K., Olesen, J., Pe-
ters, M., and Martelletti, P. (2007). Aids for manage-
ment of common headache disorders in primary care.
The online Journal of Headache and Pain, 8.
Vandewiele, G., De Backere, F., Lannoye, K., Berghe,
M. V., Janssens, O., Van Hoecke, S., Keereman, V.,
Paemeleire, K., Ongenae, F., and De Turck, F. (2018).
A decision support system to follow up and diag-
nose primary headache patients using semantically en-
riched data. BMC medical informatics and decision
making, 18(1):98.
World-Health-Organization (2016). http://www.who.int/
mediacentre/factsheets/fs277/en/.
Yin, Z., Dong, Z., Lu, X., Yu, S., Chen, X., and Duan,
H. (2015). A clinical decision support system for the
diagnosis of probable migraine and probable tension-
type headache based on case-based reasoning. The
journal of headache and pain, 16(1):29.
Yin, Z., Min, L., Lu, X., and Duan, H. (2014). A clinical de-
cision support system for primary headache disorder
based on hybrid intelligent reasoning. In Biomedical
Engineering and Informatics (BMEI), 2014 7th Inter-
national Conference on, pages 683–687. IEEE.
Zafar, K., Anwar, Z., Anwar, M., Ahmed, W., Khan, A.,
Rehman, S., and Halim, Z. (2013). Clinical deci-
sion support system for the diagnosis of migraine and
headache. Journal of Basic and Applied Scientific Re-
search, 3(10).
HEALTHINF 2021 - 14th International Conference on Health Informatics
408
