
Sociotechnical Challenges of eHealth Technology for Patient
Self-management: A Systematic Review
Stefan Hochwarter
a
Department of Computer Science, Norwegian University for Science and Technology, Trondheim, Norway
Keywords:
eHealth, mHealth, Welfare Technology, Assistive Technology, Collaboration, Cooperative Work, STS,
Review, Challenges.
Abstract:
Ageing of society and increase of time spent with chronic conditions challenge the traditional long-term care
model. Assistive technology and eHealth are seen to play an important role when addressing these challenges.
One prominent example are patient self-management systems. These systems not only transform the way
patients with chronic conditions interact with the healthcare system, but also change work practices of care
providers. This literature review addresses sociotechnical challenges of eHealth technologies with a strong
collaborative component. As a result, four themes are identified and discussed.
1 INTRODUCTION
Population projections indicate a worldwide popula-
tion ageing, with high-income countries leading the
list (UN, 2017). This poses a challenge for the de-
livery of healthcare services, both at a societal and
economic dimension. The financial crisis in Europe
(European debt crisis) since 2009 and the popula-
tion ageing forces the countries to rethink their long-
term care (LTC) policies (Swartz, 2013). The rise of
life expectancy comes in hand with the increase of
disability-adjusted life years (DALYs), whereas non-
communicable diseases are leading the list (OECD,
2017). A shift in primary care for patients with
chronic illnesses to address this demographic change
is proposed and the use of technology is seen as a
powerful mean (Bodenheimer et al., 2002a; Boden-
heimer et al., 2002b).
Welfare Technology (WT), or assistive technol-
ogy as commonly known outside Scandinavia, is
one prominent example of such technology in (pri-
mary) healthcare
1
. The aim of WT is to in-
crease the life quality and independence of peo-
ple with physical, psychological or social impair-
ments (Departementenes servicesenter, Informasjons-
forvaltning, 2011). The landscape of WT consists of a
wide range of different technologies, such as sensors,
a
https://orcid.org/0000-0003-2652-135X
1
In this paper we stick to term Welfare Technology to avoid
ambiguity.
Internet of Things (IoT) or GPS. Even though WT of-
ten introduces and relies on innovative technical solu-
tions, previous research in the field of WT states that
challenges are only 20 % of technical and 80 % of or-
ganizational nature (Helsedirektoratet, 2012). Hence,
the introduction of WT and in turn the digital trans-
formation of healthcare raises challenges of socio-
technical nature. This has also an effect on the work
of care providers and the communication and collab-
oration with their patients (Meskó et al., 2017).
WT involves numerous types of actors which are
highly heterogeneous. Platforms are seen as an in-
termediate between the use of ICT and societal out-
comes. They also support communication across the
different users of the platform, each with their own,
often very specific, requirements to the system. When
designing such a platform, the values and needs of
these different actors need to be carefully considered
and taken into account (Ann Majchrzak et al., 2016).
The platformization can also lead to a disruption of
existing channels for communication between the par-
ticipating actors of the platform. This can result to
uncertainty about where to find information or who is
responsible when new information occurs.
The digital transformation also affects the work
practices of care providers. In some cases this
could also mean the need to perform additional or
different work than before the introduction of e.g.
WT solutions. New skills are developed by both
the care providers and receivers and different forms
of communication challenge the traditional form of
394
Hochwarter, S.
Sociotechnical Challenges of eHealth Technology for Patient Self-management: A Systematic Review.
DOI: 10.5220/0010237603940400
In Proceedings of the 14th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2021) - Volume 5: HEALTHINF, pages 394-400
ISBN: 978-989-758-490-9
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
care (Grisot et al., 2018).
These challenges are common themes within
the field of Computer-Supported Cooperative Work
(CSCW). The umbrella term CSCW was coined in
1984 during a workshop by Irene Greif and Paul M.
Cashman. The terms used to describe this field were
not strictly defined, also to allow broader discussions
and invite researchers from various fields to partici-
pate. Schmidt and Bannon made an effort to describe
those terms in more detail, looking at the meaning
of CS (“computer-supported”) and CW (“cooperative
work”). They argue that one first needs to understand
the underlying mechanisms and nature of cooperative
work in order to design computer systems that sup-
port cooperative work (Schmidt and Bannon, 1992).
Two prominent challenges in the field of CSCW are
common themes when implementing welfare tech-
nology that changes the “traditional” way of work-
ing in healthcare, namely the challenge of dispar-
ity in work and benefit and disruption of social pro-
cesses (Grudin, 1994).
The aim of this study to investigate sociotechnical
challenges of eHealth technology with a focus on its
collaborative nature. Welfare technology poses new
challenges to the healthcare system and the way work
is organized around the patient, similar to the chal-
lenges described in CSCW literature, as stated above.
This is especially visible for patient self-monitoring
and reporting, as it creates new ways of communica-
tion and challenges the traditional division of work of
care providers and receivers.
2 METHODS
As the eHealth landscape is rapidly changing, and
new eHealth solutions and national strategies arise
under the umbrella of welfare technology, there is the
need for an updated review on the current challenges
and opportunities. Even though there have been some
systematic literature reviews identified (see for exam-
ple (Vassli and Farshchian, 2018)), no review was
found to understand the collaborative nature of this
emerging, and indeed cooperative technology. Hence,
concepts were chosen in accordance with the theme,
choosing examples of welfare technology that have a
high degree of collaboration.
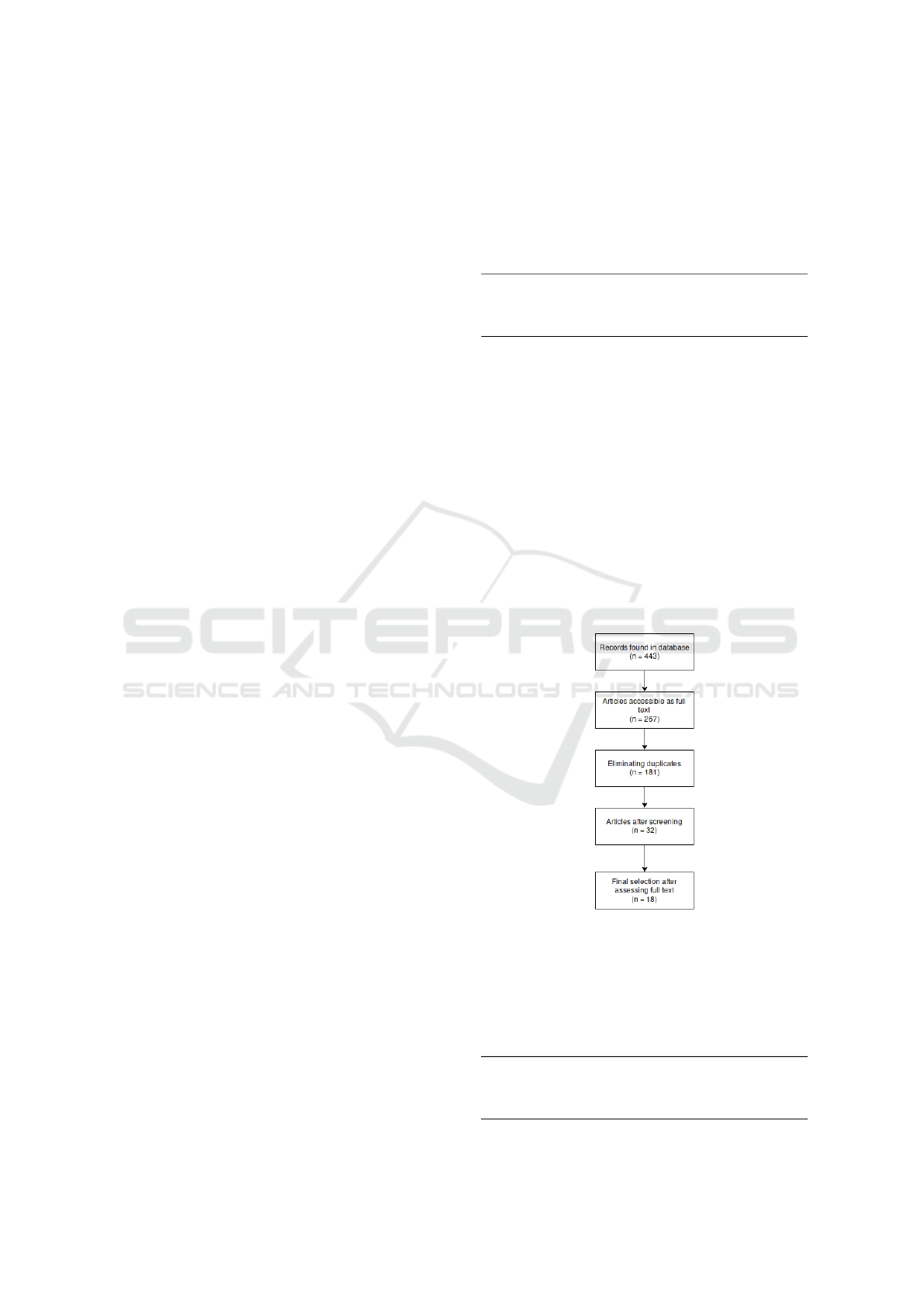
A systematic literature review was conducted in
five steps to investigate the study objective to inves-
tigate the sociotechnical challenges of eHealth tech-
nology for patient self-management. The review was
designed according to Cruzes and Dyba (Cruzes and
Dyba, 2011). In a first step a first unstructured search
to explore the field and get an understanding of com-
mon terms and phrases in this field was conducted.
Following, the objective was split up into three con-
cepts, and for each concept similar terms were identi-
fies (see Table 1).
Table 1: Mapping the objective to concepts.
Concept 1 Concept 2 Concept 3
motivation welfare technology self-monitoring
pitfalls ehealth patient reporting
challenges mhealth remote monitoring
telemedicine self-management
Based on these concepts, papers for review were
identified searching the Scopus database. Scopus
was selected as a primary source as it also includes
records from the MEDLINE and EMBASE databases.
A complete search history including the number of
found and accessible papers can be seen in table 3.
Accessible papers were selected based on predefined
inclusion and exclusion criteria (Table 2). In a next
steps, duplicates where removed and an initial screen-
ing to assess if the paper is relevant to this objective by
reading the title and abstract, and evaluating the jour-
nal type and research field. After reading the full-text
version of the articles identified in the first screening,
the final selection of articles for the literature review
were selected (see figure 1).
Figure 1: The study selection process.
Finally, the selected articles were analyzed and
concepts were identified and mapped using the ref-
erence management system Zotero with the extension
ZotFile to extract annotations.
Table 2: Inclusion and exclusion criteria.
original articles published in peer-reviewed journal
articles published in 2009 until 2019
written in English, German or a Scandinavian language
no study protocols
Sociotechnical Challenges of eHealth Technology for Patient Self-management: A Systematic Review
395
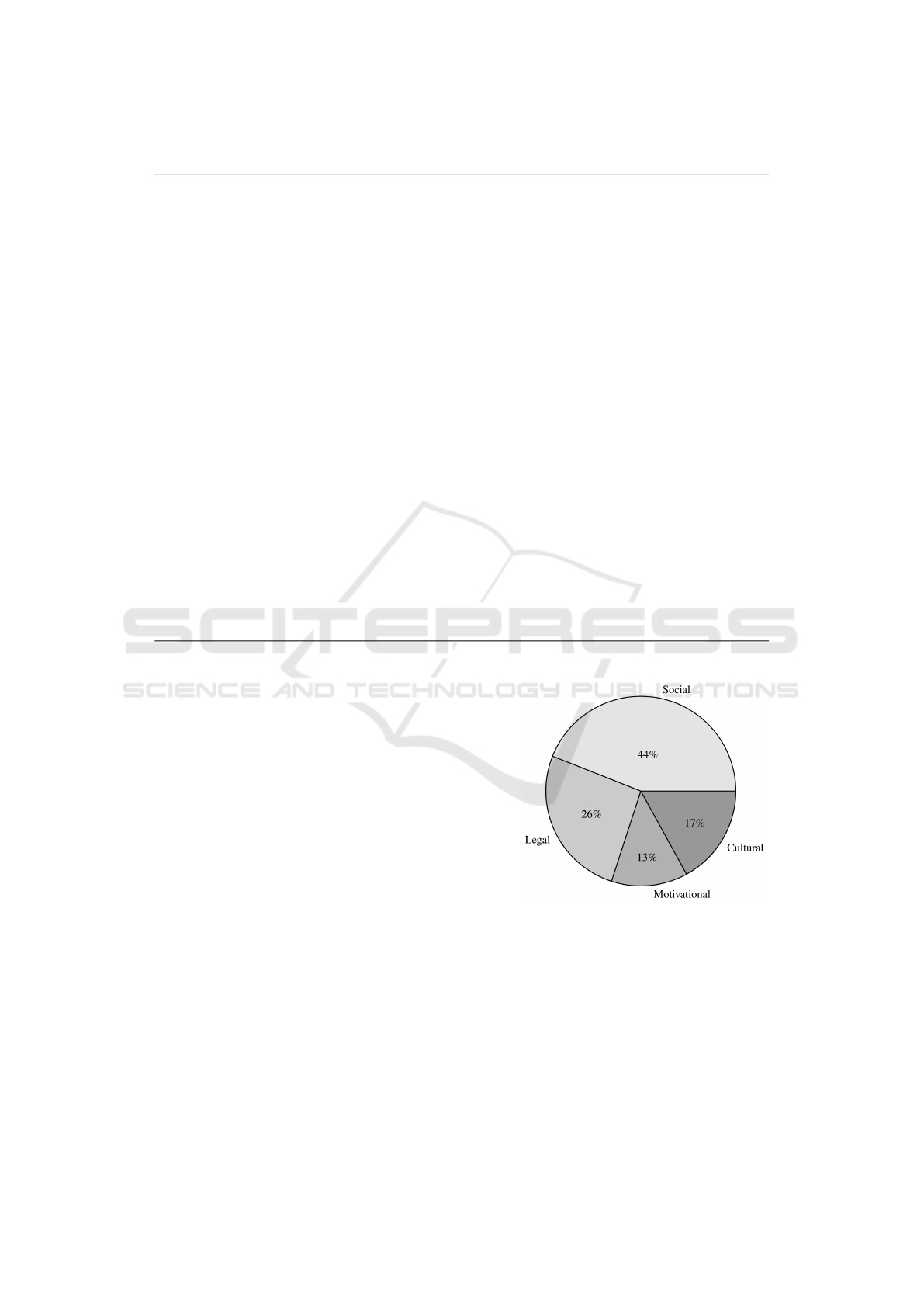
Table 3: The search history of the literature review.
Search Found Accessible
TITLE-ABS-KEY ( "welfare technology" self-monitoring ) AND DOCTYPE ( ar ) AND PUBYEAR > 2008 0 0
TITLE-ABS-KEY ( "welfare technology" patient reporting ) AND DOCTYPE ( ar ) AND PUBYEAR > 2008 0 0
TITLE-ABS-KEY ( "welfare technology" remote monitoring ) AND DOCTYPE ( ar ) AND PUBYEAR > 2008 1 0
TITLE-ABS-KEY ( "welfare technology" self-management ) AND DOCTYPE ( ar ) AND PUBYEAR > 2008 0 0
TITLE-ABS-KEY ( "welfare technology" motivation ) AND DOCTYPE ( ar ) AND PUBYEAR > 2008 1 1
TITLE-ABS-KEY ( "welfare technology" pitfalls ) AND DOCTYPE ( ar ) AND PUBYEAR > 2008 0 0
TITLE-ABS-KEY ( "welfare technology" challenges ) AND DOCTYPE ( ar ) AND PUBYEAR > 2008 6 5
TITLE-ABS-KEY ( ehealth AND self-monitoring AND motivation ) AND DOCTYPE ( ar ) AND PUBYEAR > 2008 3 2
TITLE-ABS-KEY ( ehealth AND self-monitoring AND pitfalls ) AND DOCTYPE ( ar ) AND PUBYEAR > 2008 0 0
TITLE-ABS-KEY ( ehealth AND self-monitoring AND challenges ) AND DOCTYPE ( ar ) AND PUBYEAR > 2008 11 8
TITLE-ABS-KEY ( ehealth AND patient AND reporting AND motivation ) AND DOCTYPE ( ar ) AND PUBYEAR > 2008 1 1
TITLE-ABS-KEY ( ehealth AND patient AND reporting AND pitfalls ) AND DOCTYPE ( ar ) AND PUBYEAR > 2008 0 0
TITLE-ABS-KEY ( ehealth AND patient AND reporting AND challenges ) AND DOCTYPE ( ar ) AND PUBYEAR > 2008 8 4
TITLE-ABS-KEY ( ehealth AND remote AND monitoring AND motivation ) AND DOCTYPE ( ar ) AND PUBYEAR > 2008 2 0
TITLE-ABS-KEY ( ehealth AND remote AND monitoring AND pitfalls ) AND DOCTYPE ( ar ) AND PUBYEAR > 2008 0 0
TITLE-ABS-KEY ( ehealth AND remote AND monitoring AND challenges ) AND DOCTYPE ( ar ) AND PUBYEAR > 2008 17 8
TITLE-ABS-KEY ( ehealth AND self-management AND motivation ) AND DOCTYPE ( ar ) AND PUBYEAR > 2008 14 8
TITLE-ABS-KEY ( ehealth AND self-management AND pitfalls ) AND DOCTYPE ( ar ) AND PUBYEAR > 2008 0 0
TITLE-ABS-KEY ( ehealth AND self-management AND challenges ) AND DOCTYPE ( ar ) AND PUBYEAR > 2008 21 12
TITLE-ABS-KEY ( mhealth AND self-monitoring AND motivation ) AND DOCTYPE ( ar ) AND PUBYEAR > 2008 27 16
TITLE-ABS-KEY ( mhealth AND self-monitoring AND pitfalls ) AND DOCTYPE ( ar ) AND PUBYEAR > 2008 0 0
TITLE-ABS-KEY ( mhealth AND self-monitoring AND challenges ) AND DOCTYPE ( ar ) AND PUBYEAR > 2008 11 6
TITLE-ABS-KEY ( mhealth AND patient AND reporting AND motivation ) AND DOCTYPE ( ar ) AND PUBYEAR > 2008 4 3
TITLE-ABS-KEY ( mhealth AND patient AND reporting AND pitfalls ) AND DOCTYPE ( ar ) AND PUBYEAR > 2008 0 0
TITLE-ABS-KEY ( mhealth AND patient AND reporting AND challenges ) AND DOCTYPE ( ar ) AND PUBYEAR > 2008 13 11
TITLE-ABS-KEY ( mhealth AND remote AND monitoring AND motivation ) AND DOCTYPE ( ar ) AND PUBYEAR > 2008 3 1
TITLE-ABS-KEY ( mhealth AND remote AND monitoring AND pitfalls ) AND DOCTYPE ( ar ) AND PUBYEAR > 2008 0 0
TITLE-ABS-KEY ( mhealth AND remote AND monitoring AND challenges ) AND DOCTYPE ( ar ) AND PUBYEAR > 2008 24 15
TITLE-ABS-KEY ( mhealth AND self-management AND motivation ) AND DOCTYPE ( ar ) AND PUBYEAR > 2008 19 10
TITLE-ABS-KEY ( mhealth AND self-management AND pitfalls ) AND DOCTYPE ( ar ) AND PUBYEAR > 2008 1 1
TITLE-ABS-KEY ( mhealth AND self-management AND challenges ) AND DOCTYPE ( ar ) AND PUBYEAR > 2008 35 22
TITLE-ABS-KEY ( telemedicine AND self-monitoring AND motivation ) AND DOCTYPE ( ar ) AND PUBYEAR > 2008 25 14
TITLE-ABS-KEY ( telemedicine AND self-monitoring AND pitfalls ) AND DOCTYPE ( ar ) AND PUBYEAR > 2008 1 1
TITLE-ABS-KEY ( telemedicine AND self-monitoring AND challenges ) AND DOCTYPE ( ar ) AND PUBYEAR > 2008 28 18
TITLE-ABS-KEY ( telemedicine AND patient AND reporting AND motivation ) AND DOCTYPE ( ar ) AND PUBYEAR > 2008 9 6
TITLE-ABS-KEY ( telemedicine AND patient AND reporting AND pitfalls ) AND DOCTYPE ( ar ) AND PUBYEAR > 2008 0 0
TITLE-ABS-KEY ( telemedicine AND patient AND reporting AND challenges ) AND DOCTYPE ( ar ) AND PUBYEAR > 2008 23 13
TITLE-ABS-KEY ( telemedicine AND remote AND monitoring AND motivation ) AND DOCTYPE ( ar ) AND PUBYEAR > 2008 15 7
TITLE-ABS-KEY ( telemedicine AND remote AND monitoring AND pitfalls ) AND DOCTYPE ( ar ) AND PUBYEAR > 2008 0 0
TITLE-ABS-KEY ( telemedicine "remote monitoring" challenges ) AND DOCTYPE ( ar ) AND PUBYEAR > 2008 31 13
TITLE-ABS-KEY ( telemedicine AND self-management AND motivation ) AND DOCTYPE ( ar ) AND PUBYEAR > 2008 49 32
TITLE-ABS-KEY ( telemedicine AND self-management AND pitfalls ) AND DOCTYPE ( ar ) AND PUBYEAR > 2008 0 0
TITLE-ABS-KEY ( telemedicine "self-management" challenges ) AND DOCTYPE ( ar ) AND PUBYEAR > 2008 40 29
3 RESULTS
Of the initial 443 records found, 18 articles were se-
lected to be included in the literature review. From the
181 accessible articles without duplicates, 159 were
excluded mainly because they were not addressing the
defined study objective, they were purely focusing on
the effect of interventions, or were study protocols for
future studies.
Common themes related to the study objective
were identified and mapped. The most common
theme was related to social pitfalls, followed by moti-
vational and legal challenges. Figure 2 visualizes the
distribution of the themes. Table 4 describes the in-
cluded papers, their subject of study and the themes
identified.
3.1 Social
Social challenges and pitfalls are the most common
theme. The lack of social support for the patients
when using self-management solutions is seen as a
major challenge by many articles. Solutions are re-
ceived as impersonal and complicated by the end-
users (Rollo et al., 2016; Hoaas et al., 2016). Missing
Figure 2: Identified themes related to study objective.
personal contact with the care personnel and hence
the absent of physical meetings are reported for long-
term care of patients with chronic conditions. Adher-
ence is suffering from this shortcomings (Hoaas et al.,
2016; Moyano et al., 2019). The lack of personal con-
tact and personal support is the most mentioned chal-
lenge (Rollo et al., 2016; Hoaas et al., 2016; Rollo
et al., 2016; Firet et al., 2019; Wake et al., 2016;
Östlund et al., 2015). Stand-alone interventions with-
out personal support are reported to have low usage
HEALTHINF 2021 - 14th International Conference on Health Informatics
396

Table 4: Details of reviewed literature and identified themes.
Reference Subject of study Theme(s)
(Bossuyt et al., 2017) disease management and monitoring for pa-
tients with inflammatory bowel disease
legal; social
(Dhillon et al., 2016) patient-centered health management system cultural
(Early et al., 2017) IT-based self-management of COPD coupled
with nurse-coach support
social; motivational
(Firet et al., 2019) eHealth with pelvic floor muscle training to
support self-management of stress urinary in-
continence
social
(Henkemans et al., 2018) pilot implementation of app for self-
management
social
(Hoaas et al., 2016) exercise training at home, telemonitoring and
self-management, weekly videoconferencing
sessions
social
(Legido-Quigley et al., 2014) teleradiology across borders in the European
Union
legal
(Martin et al., 2012) adoption, readiness, and implementation of
telemedicine in rural hospitals and primary
care providers
legal
(Moyano et al., 2019) perception and acceptability of text messag-
ing intervention for diabetes care
social
(Nilsen et al., 2016) case study of welfare technology describing
resistance of implementation
cultural
(Odnoletkova et al., 2016) perception of tele-coaching in type 2 diabetes motivational; legal
(Rollo et al., 2016) eHealth systems for supporting diabetes self-
management
cultural; social
(Ross et al., 2018) self-management program for people with
type 2 diabetes
motivational
(Saner and van der Velde, 2016) eHealth and telemedicine challenges and op-
portunities in cardiology services
legal
(Slettebø et al., 2018) ethical challenges perceived by leaders of
community health services for older people
legal; social
(Wake et al., 2016) evaluation of national electronic personal
health record and self-management platform
for people with diabetes
social
(Zibrik et al., 2015) uptake of eHealth for chronic disease self-
management among immigrants and seniors
cultural
(Östlund et al., 2015) design of welfare technology solutions and
addressing the needs of its users - STS-
inspired design
social
and acceptance, especially with the older population
or minorities (Wake et al., 2016).
The role of relatives in a healthcare system that
is designed around medical conditions rather than the
patient’s need is another factor for the use of self-
management systems, and hence challenges the eq-
uitable use and distribution of these systems (Slettebø
et al., 2018). For children, the role of the parent and
their education level is crucial for receiving and effec-
tively using self-management solutions (Henkemans
et al., 2018).
3.2 Legal
Several articles explicitly mention legal barriers for
the use of welfare technology. The use of self-
management systems challenges the responsibilities
of the involved actors. This is reflected by the ques-
tion of who is responsible in certain situations and
how much trust one can put into reports generated
by others through self-reporting systems (Legido-
Quigley et al., 2014). Further, the tension between
following the minimum legal requirements and the
additional care through digital health services chal-
Sociotechnical Challenges of eHealth Technology for Patient Self-management: A Systematic Review
397

lenges the work of care professionals (Slettebø et al.,
2018). Generally, the lack of a legal framework or
the fragmentation of legal frameworks is considered
an issue when care providers implement and use wel-
fare technology solutions (Martin et al., 2012; Saner
and van der Velde, 2016; Odnoletkova et al., 2016).
Finally, legal issues related to privacy, information se-
curity and the right to be forgotten hinder the diffusion
of WT. These challenges are also linked to social pit-
falls (Bossuyt et al., 2017; Odnoletkova et al., 2016).
3.3 Cultural
Cultural differences influence the usefulness of differ-
ent features of eHealth solutions. Different require-
ments to the workflow and user interface are reported,
based on different cultural background. Features that
are of use in one region might not be of use in an-
other region, or culture so to speak (Dhillon et al.,
2016). The role of cultural practices, language bar-
riers, and the clash of different professional cultures
are stated as inhibited factors. Resistance against the
role of co-creators arises out of these factors. Fur-
ther, poor eHealth literacy is mentioned as a common
problem linked to the user’s background (Rollo et al.,
2016; Nilsen et al., 2016; Zibrik et al., 2015).
3.4 Motivational
Finally, pitfalls related to motivational factors were
mentioned in three papers. The lack of motivation to
use IT rather than poor IT skills is stated as a barrier
for patients (Early et al., 2017). One paper mentions
that the motivation of patients with chronic diseases
is the biggest issue to overcome when implementing
self-management systems. (Odnoletkova et al., 2016).
On the other side, lack of motivation is also reported
for care providers who are unwilling to support the
system by providing resources (Ross et al., 2018).
4 DISCUSSION
The objective of this paper was to investigate the so-
ciotechnical challenges of eHealth technology for pa-
tient self-management. Particularly of interest was
the collaborative nature of eHealth technology, hence
systems for patient self-management were chosen as
a good and timely case to investigate this objective.
The major theme found in this literature review,
is the one of social pitfalls. When designing and im-
plementing welfare technology that disrupts existing
channels, it has strong social effects. Communication
and personal contact between the care providers and
patients are subject to change. The shift from care
activities from a well-defined and known (at least for
the healthcare professionals) environment affects the
way care is delivered and experienced. The private
homes of the patient play a central role and its percep-
tion changes. Also, the way cooperative work is done
in the healthcare sector receives an additional com-
ponent to the already manifold system. Finally, the
importance of a peer-network (e.g. relatives, neigh-
bors) is illustrated to ensure personal support. Infor-
mal caregivers gain more attention and importance in
this setting.
The lack of a legal framework is also mentioned
repeatedly as an obstacle to implement WT. In or-
der to avoid additional work without compensation,
or work where responsibilities are not clearly defined,
a legal framework needs to be established. This also
includes GDPR (General Data Protection Regulation)
and clear reimbursement systems. Leading the way in
the European north, Denmark has established a Digi-
tal Health Strategy and an eHealth reference architec-
ture.
Further, it is essential to understand the users
and actors involved. The actors can generally not
be divided in homogenous groups, rather very het-
erogenous groups that have distinctive characteristics
within the group. Elderly patients often have more
than one disorder, and the management of comorbid-
ity is in-turn very individual. This has also been un-
derlined in articles reporting cultural challenges, and
calls for a holistic approach that takes this diversity
into account when designing WT systems.
Finally, another common theme is the one of moti-
vational challenges. For the care-receivers, in the role
of co-creators, motivation can stagnate for chronic
conditions where they should self-report even in the
absent of symptoms, and this in turn reminds the pa-
tients that they are living with a chronic disease. For
care providers, on the other hand, poor motivation can
be traced back to new work routines, new required
skills, and lack of clearly established boundaries for
their responsibilities (cf. legal challenges).
The importance of addressing challenges of col-
laboration can be seen throughout all four identified
themes and their descriptions, although most common
within the identified social challenges. The impli-
cations of moving care into the home have been ad-
dressed by many scholars in the field of CSCW. The
lack of personal contact and personal support, as de-
scribed in section 3.1, can be a consequence of mov-
ing care to a different setting. At home, the (invis-
ible) work of relatives for healthcare plays a major
role, while their work might not be recognized, or sys-
tems and workflows were not designed with them in
HEALTHINF 2021 - 14th International Conference on Health Informatics
398

mind. At the same time, power relations change when
healthcare worker visit the patients physically at their
homes. So moving care to a new environment chal-
lenges the traditional coordination of it (Fitzpatrick
and Ellingsen, 2013).
These challenges have been discussed in detail in
the field of CSCW, but it aims to go beyond barely
describing the context at hand. It is a constructive
research domain, it is design oriented and aims to im-
plement better CSCW systems (Schmidt and Bannon,
1992). To do so, one must first understand the do-
main that shall be changed - in our case the coop-
erative work systems to treat and manage long-term
diseases. As Welfare Technology is a rather new um-
brella term, which though attracts much attention, the
identified challenges are of relevance for the design of
new and improved solutions.
5 CONCLUSION
This paper focused on the sociotechnical challenges
of eHealth technology, and it aims to support the un-
derstanding of the complex systems involved. Hence,
it can not cover all the aspects that are relevant. The
scope of this paper was on the system as a whole, in-
cluding all actors involved and using self-monitoring
or self-management systems as a proxy for systems
with high collaborative nature. This is still a very
broad perspective, and this makes it easy to miss im-
portant details. Future research is recommended to
look at a specific group of actors (e.g. patients, policy-
makers, nurses), at a specific condition (e.g. asthma,
dementia) or systems using technologies with unique
characteristics (e.g. fall detectors, medicine dis-
pensers). Further, I encourage researchers to become
active and uncover what works and what doesn’t by
using for example action design research or participa-
tory design.
This work has several limitations, mainly due to
its scope. First, it uses strict inclusion and exclusion
criteria. Only peer-reviewed journal articles are in-
cluded. To have access to more recent and up-to-date
findings, conference papers can further be of interest.
Also, only one database was used to retrieve our arti-
cles (Scopus). Including other databases which cover
a different audience would increase the range of cov-
ered topics and perspectives.
Finally, to fully understand this complex and fast-
moving field, a different approach, such as a realist
review, might bring up more insight into this field.
ACKNOWLEDGEMENTS
I would like to thank Babak A. Farshchian and Elena
Parmiggiani for their constructive feedback. Further,
I’d like to thank the three anonymous reviewers for
their input that helped to improve this paper.
REFERENCES
Ann Majchrzak, M. Lynne Markus, and Jonathan Ware-
ham (2016). Designing for Digital Transformation:
Lessons for Information Systems Research from the
Study of ICT and Societal Challenges. MIS Quarterly,
40(2):267–277.
Bodenheimer, T., Wagner, E. H., and Grumbach, K.
(2002a). Improving Primary Care for Patients With
Chronic Illness. Journal of the American Medical As-
sociation, page 5.
Bodenheimer, T., Wagner, E. H., and Grumbach, K.
(2002b). Improving Primary Care for Patients With
Chronic IllnessThe Chronic Care Model, Part 2. Jour-
nal of the American Medical Association.
Bossuyt, P., Pouillon, L., Bonnaud, G., Danese, S., and
Peyrin-Biroulet, L. (2017). E-health in inflammatory
bowel diseases: More challenges than opportunities?
Digestive and Liver Disease, 49(12):1320–1326.
Cruzes, D. S. and Dyba, T. (2011). Recommended Steps for
Thematic Synthesis in Software Engineering. In 2011
International Symposium on Empirical Software En-
gineering and Measurement, pages 275–284, Banff,
AB. IEEE.
Departementenes servicesenter, Informasjonsforvaltning,
editor (2011). Innovasjon i omsorg ; utredning fra
et utvalg oppnevnt ved kongelig resolusjon 26. juni
2009. Number 2011,11 in Norges offentlige utred-
ninger. Departementenes Servicesenter, Informasjons-
forvaltning, Oslo.
Dhillon, J. S., Wünsche, B., and Lutteroth, C. (2016). De-
signing and evaluating a patient-centred health man-
agement system for seniors. Journal of Telemedicine
and Telecare, 22(2):96–104.
Early, F., Young, J., Robinshaw, E., Mi, E., Mi, E., and
Fuld, J. (2017). A case series of an off-the-shelf online
health resource with integrated nurse coaching to sup-
port self-management in COPD. International Jour-
nal of Chronic Obstructive Pulmonary Disease, Vol-
ume 12:2955–2967.
Firet, L., de Bree, C., Verhoeks, C. M., Teunissen, D. A. M.,
and Lagro-Janssen, A. L. M. (2019). Mixed feelings:
General practitioners’ attitudes towards eHealth for
stress urinary incontinence - a qualitative study. BMC
Family Practice, 20(1).
Fitzpatrick, G. and Ellingsen, G. (2013). A Review of 25
Years of CSCW Research in Healthcare: Contribu-
tions, Challenges and Future Agendas. Computer Sup-
ported Cooperative Work (CSCW), 22(4-6):609–665.
Grisot, M., Hagen, L., Kempton, A. M., and Aanestad,
M. (2018). Supporting Patient Self-Care: Examining
Sociotechnical Challenges of eHealth Technology for Patient Self-management: A Systematic Review
399

Nurses’ Practices in a Remote Care Setting. Studies in
Health Technology and Informatics, pages 601–605.
Grudin, J. (1994). Groupware and social dynamics: Eight
challenges for developers. Communications of the
ACM, 37(1):92–105.
Helsedirektoratet (2012). Velferdsteknologi. Fagrapport om
implementering av velferdsteknologi i de kommunale
helse- og omsorgstjenestene 2013-2030. Technical
Report IS-1990.
Henkemans, O. A. B., Keij, M., Grootjen, M., Kamphuis,
M., and Dijkshoorn, A. (2018). Design and evaluation
of the StartingTogether App for home visits in preven-
tive child health care. BMC Nursing, 17(1).
Hoaas, H., Andreassen, H. K., Lien, L. A., Hjalmarsen, A.,
and Zanaboni, P. (2016). Adherence and factors af-
fecting satisfaction in long-term telerehabilitation for
patients with chronic obstructive pulmonary disease:
A mixed methods study. BMC Medical Informatics
and Decision Making, 16(1).
Legido-Quigley, H., Doering, N., and McKee, M. (2014).
Challenges facing teleradiology services across bor-
ders in the European union: A qualitative study.
Health Policy and Technology, 3(3):160–166.
Martin, A. B., Probst, J. C., Shah, K., Chen, Z., and
Garr, D. (2012). Differences in Readiness Be-
tween Rural Hospitals and Primary Care Providers for
Telemedicine Adoption and Implementation: Find-
ings From a Statewide Telemedicine Survey: Differ-
ences in Telemedicine Readiness. The Journal of Ru-
ral Health, 28(1):8–15.
Meskó, B., Drobni, Z., Bényei, É., Gergely, B., and Gy
˝
orffy,
Z. (2017). Digital health is a cultural transformation
of traditional healthcare. mHealth, 3:38–38.
Moyano, D., Morelli, D., Santero, M., Belizan, M., Irazola,
V., and Beratarrechea, A. (2019). Perceptions and Ac-
ceptability of Text Messaging for Diabetes Care in Pri-
mary Care in Argentina: Exploratory Study. JMIR
Diabetes, 4(1):e10350.
Nilsen, E. R., Dugstad, J., Eide, H., Gullslett, M. K., and
Eide, T. (2016). Exploring resistance to implemen-
tation of welfare technology in municipal healthcare
services – a longitudinal case study. BMC Health Ser-
vices Research, 16(1).
Odnoletkova, I., Buysse, H., Nobels, F., Goderis, G., Aert-
geerts, B., Annemans, L., and Ramaekers, D. (2016).
Patient and provider acceptance of telecoaching in
type 2 diabetes: A mixed-method study embedded in
a randomised clinical trial. BMC Medical Informatics
and Decision Making, 16(1).
OECD (2017). Health at a Glance 2017: OECD Indicators.
OECD, Paris.
Östlund, B., Olander, E., Jonsson, O., and Frennert, S.
(2015). STS-inspired design to meet the challenges
of modern aging. Welfare technology as a tool to pro-
mote user driven innovations or another way to keep
older users hostage? Technological Forecasting and
Social Change, 93:82–90.
Rollo, M. E., Aguiar, E. J., Williams, R. L., Wynne, K.,
Kriss, M., Callister, R., and Collins, C. E. (2016).
eHealth technologies to support nutrition and physical
activity behaviors in diabetes self-management. Dia-
betes, Metabolic Syndrome and Obesity: Targets and
Therapy, Volume 9:381–390.
Ross, J., Stevenson, F., Dack, C., Pal, K., May, C., Michie,
S., Barnard, M., and Murray, E. (2018). Develop-
ing an implementation strategy for a digital health in-
tervention: An example in routine healthcare. BMC
Health Services Research, 18(1).
Saner, H. and van der Velde, E. (2016). eHealth in car-
diovascular medicine: A clinical update. European
Journal of Preventive Cardiology, 23(2_suppl):5–12.
Schmidt, K. and Bannon, L. (1992). Taking CSCW
seriously. Computer Supported Cooperative Work
(CSCW), 1(1):7–40.
Slettebø, Å., Skaar, R., Brodtkorb, K., and Skisland, A.
(2018). Conflicting rationales: Leader’s experienced
ethical challenges in community health care for older
people. Scandinavian Journal of Caring Sciences,
32(2):645–653.
Swartz, K. (2013). Searching for a Balance of Responsibil-
ities: OECD Countries’ Changing Elderly Assistance
Policies. Annual Review of Public Health, 34(1):397–
412.
UN (2017). World Population Ageing 2017 - Highlights.
Technical report, United Nations, Department of Eco-
nomics and Social Affairs, Population Division.
Vassli, L. T. and Farshchian, B. A. (2018). Acceptance of
Health-Related ICT among Elderly People Living in
the Community: A Systematic Review of Qualitative
Evidence. International Journal of Human–Computer
Interaction, 34(2):99–116.
Wake, D. J., He, J., Czesak, A. M., Mughal, F., and
Cunningham, S. G. (2016). MyDiabetesMyWay:
An Evolving National Data Driven Diabetes Self-
Management Platform. Journal of Diabetes Science
and Technology, 10(5):1050–1058.
Zibrik, L., Khan, S., Bangar, N., Stacy, E., Novak Lauscher,
H., and Ho, K. (2015). Patient and community cen-
tered eHealth: Exploring eHealth barriers and facil-
itators for chronic disease self-management within
British Columbia’s immigrant Chinese and Punjabi
seniors. Health Policy and Technology, 4(4):348–356.
HEALTHINF 2021 - 14th International Conference on Health Informatics
400
