
Responding to COVID-19:
Potential Hospital-at-Home Solutions to Re-configure the Healthcare
Service Ecosystem
Nabil Georges Badr
1a
, Luca Carrubbo
2b
and Marguerita Ruberto
2c
1
Higher Institute for Public Health, Saint Joseph University, Beirut, Lebanon
2
Department of Business Sciences, Management and Innovation Systems, Salerno University,
Via Giovanni Paolo II, 132, Fisciano (SA), Italy
Keywords: Hospitalization at Home, Systems Thinking, Viable System, Complex Ecosystems, Healthcare Service
Ecosystems.
Abstract: An effective Healthcare Service Ecosystem must emphasize the notion of well-being co-creation which entails
a dynamic interplay of actors, in face of the challenges, with their ability to use the available resource pools,
at the different system levels. An appropriate response, largely avoiding any crisis, depends on a society's
resilience and the related response of actors in the reconfiguration of resources. Originally considered luxury
and for the fortunate few who could afford the learning curve, Hospitalization-at-Home (HaH) recently
approached a new normal with a positive impact to health outcomes. Nowadays, hospitals have had to
reconfigure their health services to reduce the workload of caregivers during the COVID-19 outbreak. Our
use case can be a lesson for the adaptation of technology for patient empowerment allowing patients to interact
with their care ecosystem while at their home.
1 INTRODUCTION
An effective Healthcare Service Ecosystem (H-SES)
(Frow et al., 2014) must emphasize the notion of well-
being co-creation which entails a dynamic interplay
of actors, in face of the challenges, with their ability
to use the available resource pools, at the different
system levels (Häring et al., 2017).
In pandemics, an essential healthcare disaster per
sort, the social as well as the service-related fabric of
society, supply chains (Bonadio et al., 2020) and even
the complete industry are changed. An appropriate
response, largely avoiding any crisis, depends on a
society's resilience and the related response of actors
in the reconfiguration of resources (Finsterwalder &
Kuppelwieser, 2020). Healthcare systems are no
exception (P2PH, IHI.ORG). “The COVID-19 era is
bringing new attention and urgency to people’s social
needs, the impact of unmet needs on health, and the
a
https://orcid.org/0000-0001-7110-3718
b
https://orcid.org/0000-0002-3530-1298
c
https://orcid.org/0000-0003-2247-5894
importance of partnership among health systems and
community organizations” (P2PH, IHI.ORG).
New behaviours have to be learned for society to
maintain the well-being of its constituents and new
processes put in place and for the survival of the
multiple, and the sustainability of related ecosystems
in support of society. Healthcare Service Ecosystems
have to support new concepts and services;
technology deployment that facilitates telemedicine,
care at home and consultation at a distance must be
accelerated to expand the public’s access to essential
health services during the COVID-19 Pandemic
(CDC.ORG).
1.1 Motivation
Healthcare systems have buckled under the health
emergency in the pandemic, due to insufficient
hospital availability of beds, long waiting times, lack
of adoption of intervention plans for emergencies,
lack of medical and health personnel, of the total
344
Badr, N., Carrubbo, L. and Ruberto, M.
Responding to COVID-19: Potential Hospital-at-Home Solutions to Re-configure the Healthcare Service Ecosystem.
DOI: 10.5220/0010228103440351
In Proceedings of the 14th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2021) - Volume 5: HEALTHINF, pages 344-351
ISBN: 978-989-758-490-9
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

absence of coordination between the different ones’
actors and, above all, the lack of an adequate
assistance territorial network (Grimm, 2020).
Furthermore, the delay in the digitization process and
the presence of IT systems fragmented made it
difficult to exchange information with serious
repercussions on timeliness of the implementation of
all control measures.
For practitioners, the sudden unbalance between
health care needs and available resources has confront-
ed health professionals’ ethical choices with the need
to make decisions in time very short, paying a high toll
also in terms of human lives (Baily et al., 2007).
For patients, the pandemic has confined the
population to their homes. Those ridden with chronic
illnesses must have access to supervised and
continued care. In all, medical healthcare providers
are under an enormous amount of workload pressure,
faced with high risks and shortages of available
services, along with increased total health
expenditure (Moazzami et al., 2020).
This situation sheds the spotlight on the
importance of a reorganization of health services and
can be seen as the perfect storm motivating healthcare
ecosystems to include care at home technologies in
their mainstream. Aside from building responsive
information systems for a timely collection of
information for timely and relevant decision-making,
a paradigm shift in care models must rely on the
empowerment of territorial health care aimed at an
effective taking charge of patients both in terms of
appropriateness of care and clinical governance
(Breslow et al., 1992).
Originally considered luxury and for the fortunate
few who could afford the associated learning curve,
Hospitalization-at-Home (HaH) (Leff, 2001)
approached a new normal with a positive impact to
health outcomes. A recent study found that
substitutive home hospitalization not only reduce cost
by 38%, by improved patient experience. At the
comfort of their home, patients spent a smaller
proportion of the day sedentary and were readmitted
less frequently within 30 days (7% vs. 23%), mainly
due to the lack of potential infections risks, otherwise
extant in traditional hospital settings (Levine et al.,
2020). Clinicians are leading service reconfiguration
to cope with COVID-19. They are learning new
skills, adapting and exploiting new means of
consultations, like the use of video clinics (Thornton,
2020) for example. In other cases, hospitals have had
to reconfigure their health services to reduce the
workload of caregivers during the COVID-19
outbreak, such in the case of the deployment of easy
to use software / devices that allow patients to interact
with their care ecosystem while at their home. In
general, direct-to-consumer telemedicine products,
for instance, can enable patients to connect with their
healthcare provider at a distance. This indicates that
Healthcare ecosystems have had to learn to
reconfigure their resources.
Therefore, “HaH can be viewed as a practical
expression of H-SES adaptive features, re-
configuration ability and modular design on the
grounds of the System Thinking perspective”. The
adaptation of processes and technology can empower
patients to interact with their care ecosystem while at
their home. What HaH Solutions can provide
insight to the potential of re-configuration of
Healthcare Service Ecosystems?
To illustrate our thinking, we formed this
manuscript under the lens of systems thinking applied
to Service Ecosystems (Section 2.1) of healthcare
with the example of HaH as evidence (Section 2.2)
and posturing the value of technology as the central
component (Section 2.3) with a use case that treats the
topic (Section 3) and draws some challenging issues
(Section 4).
2 BACKGROUND
2.1 Healthcare Service Ecosystems
Starting from the recent advance in service research
on H-SES, a number of reflections have been
synthetized in terms of the actors’ engagement and
participation (Frow et al., 2019), including formal and
informal caregiver interactions (Badr et al., 2018).
Special attention has been given to the design and re-
configuration, adaptive processes, and the ability to
face the emergence in the systems (Capunzo et al.,
2013; Carrubbo et al., 2013; 2016; Ciasullo et al.,
2017).
Essentially, Healthcare Service Ecosystems can
be viewed as complex service ecosystems (Ciasullo
et al., 2017), due to the distinctive features and the
ability the re-configure fundamental resources in
reaction or anticipation of external events, where
decision-makers have to manage complex
interactions between several different actors or
entities (e.g., patients, health providers and suppliers,
etc.). Through the lens of system thinking, the
capability of reconfiguration of multiple resources to
deliver value in a different modality requires an
adaptive, cognitive alignment for maintaining the
system’s viability; i.e. the ability of Actors in the
system to 'continue' their actions and survive the
impending events. systems that aim to survive in their
Responding to COVID-19: Potential Hospital-at-Home Solutions to Re-configure the Healthcare Service Ecosystem
345

living context by establishing harmonic relationships
with other entities that own the resources necessary
for their functioning and survival (Barile et al., 2012a;
2012b; 2016). All parts of the system are
interconnected and interact with each other, providing
continuous feedback that serves as a learning cycle
for capability reconfiguration in response to a certain
event. Inherent in these dynamic capabilities of
reconfiguration is a level of complexity (variety,
variability, indeterminacy).
2.2 Hospitalization-at-Home
HaH is one one approach for a H-SES to solve
problems and adapt to evolving contingencies,
transforming the model of care. HaH is based on the
implementation of alternative forms for health
assistance such as healthcare residences, home care,
intermediate care, community mail, and weekend
shipments (Caputo, 2018). From a more general
perspective, the main value proposition of HaH is the
reduction in the number of hospitalizations and the
related reduction of hospital care costs and clinical
risks (Hwang et al., 2008). The changes in care settings
(Al-Balushi et al, 2014), and on the cost reduction for
managing hospital health processes (Bodenheimer et
al, 2020), are also indicative of this transformation. To
achieve this aim, HaH proposes a redefinition (re-
configuration) of the hospital as an advanced place of
care, and it underlines the need for specific
organizational paths directly so as to identify the
procedures for collecting timely and up-to-date data
about health services demand and the resources used
during the health processes. This implies new modes to
intend value, influenced by contextualization (value-
in-context), personal patient’s use (value-in-use) and
their own direct experiences (value-in-experience)
(Polese et al, 2018) as they have been exploited by
service scholars worldwide in last dacades.
Firstly, HaH can be considered as an alternative
approach to consolidated health treatments, because
it aims at organizing in the patient’s home a “care
setting” equivalent to the hospital one, helpful for
chronic illnesses, able to increase patient and
caregiver satisfaction so as to improve patients’
quality of life and to reduce the health processes
costs. Expanding the value to different contexts of the
ecosystem, HaH clinical activities are managed both
at a local (hospitals and districts) and regional level;
the activities of diagnosis, treatment, monitoring, and
rehabilitation are provided within several constraints
in care quality (i.e., waiting time), efficiency (i.e.,
resource utilization), and costs (i.e., fixed annual
savings or budget reduction) (Ignone et al, 2013).
Secondly, thanks to this alternative approach to
healthcare processes, HaH introduces new forms of
responsibility and engagement in the health domain,
offering to patients and their families the opportunity
to acquire the knowledge and competencies useful to
proactively collaborate with health professionals
(Rodríguez et al, 2013).
Thirdly, HaH can positively impact on patients’
quality of life and it can increase efficiency in the use
of the available resource for satisfying the collective
need for health. Considering the multiple potential
contributions provided by HaH for increasing the
efficiency and sustainability of H-SES, several
approaches have been proposed for evaluating its
dynamics, focusing attention on the decrease in
hospitalizations (Cohen et al, 1996), therefore
bolstering the overall value-in-experience of this
extended form of care.
Therefore, through hospitalization at home, H-
SES can re-configure itself and re-organize itself for
increasing the capability of the multiple needs of
patients (Polese, Carrubbo, 2016). In a nutshell,
according to Wilson (2018), the most relevant
advantages provided by HaH practice can be
summarized by provisioning components of
interdisciplinary team-based community care as part
of integrated care with other sectors, bridging
restorative approaches to care with the support for
caregivers as part of home care (Polese et al, 2018).
2.3 The Emergence of Telemedicine
and Assistive Devices
At the centre of the reconfiguration capability of the
H-SES, health technology should be patient centric,
and focus on the interaction between the patient and
the multiple actors and services in the healthcare
ecosystem.
Effective solutions have been developed to manage
the interaction among the care team (Badr et al, 2018),
provide assistive functions (assistive technologies) and
improve the patient’s quality of life (Sofaer &
Firminger, 2005; Moliner, 2009; Sweeney et al, 2015).
Through the deployment of point of use systems and
software based on principles of communication, data
management, patient engagement has become key to
the expansion of the H-SES (Britt et al, 2005; Gruman
et al, 2010; Polese & Carrubbo, 2016). For instance,
telehealth adoption is expanding the accessibility to
healthcare service beyond the traditional setting, with
services such as virtual consultation, allowing access
to cost-effective care. Soon, telepresence physicians
will use robots to help them examine and treat patients
in rural or remote locations (ASME.ORG).
HEALTHINF 2021 - 14th International Conference on Health Informatics
346

The increase of consumerism in remote healthcare
devices is democratizing current healthcare systems.
Consumer-driven care delivery models such as
telehealth, e-pharmacy, retail care, price
transparency, push care closer to the point of the
person, among others. Examples are wearable devices
such as heart monitors that can detect atrial
fibrillation, blood pressure monitors, self-adhesive
biosensor patches that track your temperature, heart
rate, will help consumers proactively get health
support. Drug delivery devices such as insulin pens,
biologic auto injectors, inhalers, and smart packaging
for pills will be commonplace to enhance both
clinical and business operations in healthcare
(https://flex.com/industries/healthcare)
As an emerging technology, it is unrealistic to
expect that solutions as such to be based on
standardizations, given the high degree of
heterogeneity of integrated care practices in place,
and the impossibility of forecasting future demands
for care. However, it is an indication that the H-SES
is attempting to reconfigure itself through the use
technology among others.
3 HAH EXPERIMENTAL USE
CASE
Here, we introduce an interesting use case
exemplifying reconfigurable Healthcare Ecosystems.
The setting of our example is in South of Italy, in
Salerno City (Campania Region).
3.1 The ‘ADD-Protection’ Co-financed
R&D Project
The Project was named ‘ADD-Protection’ to mean
the increase of care provision to defend the health of
the community, additional to the traditional protocol
already existing. This attempt was before COVID-19
situation, but still represent a best practice to
efficiently respond to uncertain and unpredictable
conditions that can occur over time. Results explain
how the innovative solution proposed can effectively
support a new organization and design of healthcare
service (seen as a whole) when needed, and today
give us (scholars, practitioners, medical employees,
managers and politicians) a very relevant suggestion
to perform a continuative care in the unusual and we
are living now.
The Project was about 1 year long and gave lots
of insightful information about the problems and the
opportunities to improve the performance level and
quality by offering modular technology solutions
with a high potential to enable evolutions in the global
Healthcare Service Ecosystem as a whole.
The experiments involve 50 persons (40-85 years
old) affected by 3 special pathologies: diabetes in
adults, heart difficulties, breath chronical problems.
3.2 The ‘ADD-Protection’ Research
Activities
Prior to the COVID-19 pandemic, The Hospital of
Salerno, named San Giovanni di Dio Ruggi
d’Aragona in San Leonard – launched an experiment
in collaboration with SIMAS Intedept., a research
Centre of Salerno University and a local firm Magaldi
Life Ltd. The attempt was to develop a new protocol
to evaluate specific cases of chronic disease of long-
term patient, in the aim to provide care to their homes.
The project included multiple milestones (Figure
1) incorporating the expansion of the definition of a
multimode medical service protocol and communica-
tion plan, the development and implementation of an
information system for remote medical examination
and the supporting infrastructure. The technology
implemented allowed for the monitoring of vital signs
and the detection of early warning. The project also
accounted for cost reduction measures, changes in the
related processes, the diffusion of training to the
actors in the service, including informal caregivers.
The following project plan was laid out to manage
and monitor the activities in the following milestones:
• MIL_1 - Development of an election procedure
for the definition of the perimeter of
"appropriateness of protected discharge" in a
logic that may include, alongside the dual option:
HOSPITAL - HOME; a multipolar option:
HOSPITAL - HOME and / or local RSA and / or
HOSPICE.
• MIL_2 - Development of a systemic and
multichannel communication plan through which
the hospital structure informs its context around
the value of the Protected Discharge model. The
aim was to calibrate the awareness to improve the
positive reception of the service and also
removing all the elements of disinformation that
it could reduce the effectiveness of the project to
the extreme of its failure.
• MIL_3 - Development of a REMOTE
MEDICAL EXAMINATION system aimed at
activating a direct communication channel
between patients and operators - in particular
hospital doctors - which allows a level of
continuity of care that is truly accessible by the
Responding to COVID-19: Potential Hospital-at-Home Solutions to Re-configure the Healthcare Service Ecosystem
347
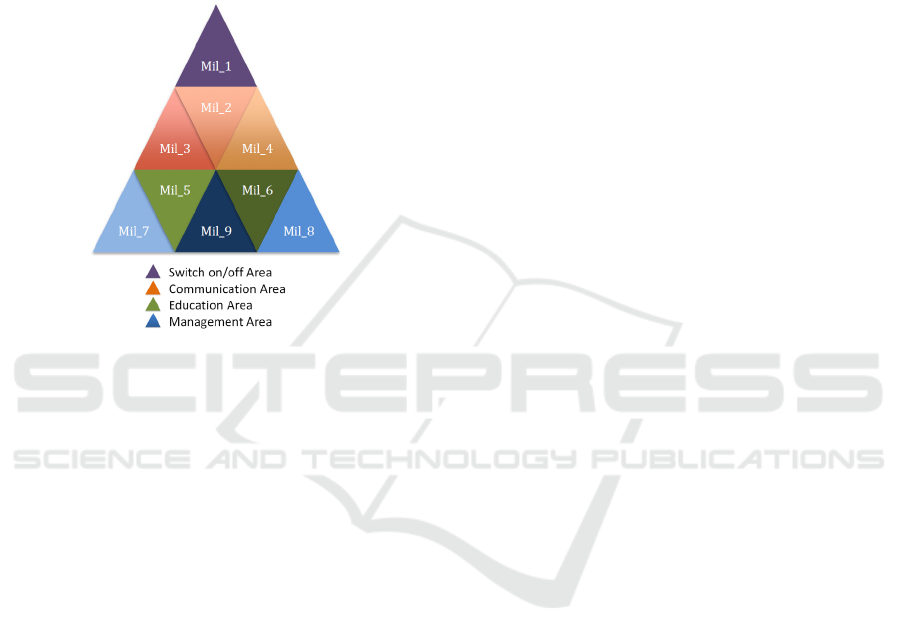
patient, especially assessment of clinical
conditions, functional and cognitive status.
• MIL_4 - Development of a dedicated IT platform
for sharing information (knowledge management)
between the parties involved in the service, with
particular reference to: progress of the treatment
plan, list of open problems, status of achievement
of objectives, and improve level of satisfaction of
the patient and family (process management
information).
Figure 1: Milestone Project Areas - From
(www.magaldilife.it).
• MIL_5 - Development of new staff training
(doctors and nurses) and any other actor involved
in the service.
• MIL_6 - Development of a new approach to
communication, involvement and active
participation of discharged subjects and their
families (informal care giver).
• MIL_7 - Development of an alert procedure that
allows you to collect weak signals and weigh the
risk factors that can lead to an early return to
hospital, not limited to health factors related to
the patient but also to those of family
sustainability.
• MIL_8 - Development of a cost logic that goes
towards the concept of "care budget", for the
elaboration of an individual Care Plan ad hoc for
the de-hospitalized patient.
• MIL_9 - Development of a renewed coordination
of activities in accordance with the principles of
Project Management, by virtue of the lower level
of standardization of each intervention.
3.3 The Technologies Used
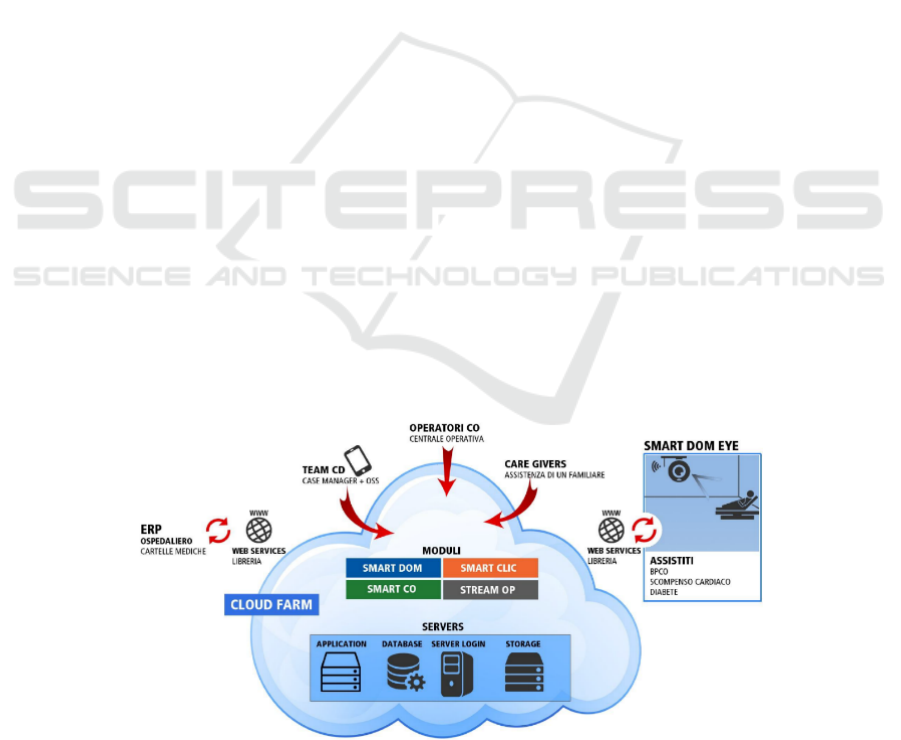
This HaH project was enabled by technologies such
as electronic medical records, real-time diagnosis
with go-pro cam, Big Data Analytics special tool,
including the provisioning of infrastructures services
required for the collection and treatment of data
generated by the experiment.
Smart home and assistive devices integrated with
a software interface. The interface at the patient’s was
modular, timely, easy-to-use, and compatible with all
main existing information systems in Healthcare.
The supporting infrastructure relied on a cost
effective cloud architecture with a multi-channel
access (web, tablet, mobile) by all project
stakeholders (OSS team, case manager, caregivers,
project manager, etc.) to the structured and
unstructured data of the platform. Interconnections
with third parties (ERP HOSPITAL) and FSE
(Electronic Health Record) allowed the possibility, in
addition to reporting, to develop business intelligence
algorithms, when operational, to obtain data and
knowledge on a single practice.
For further reference, we have included, in the
Appendix, Figure 2 depicting the overall set of
components of the technology system used.
3.4 Outcome
The implementation of HaH services reduced the
demand on the resources of the hospitals providing
the same treatment to HaH patients at a lower cost,
availing the resources of the hospital for inpatient
care. Cost savings reported were to the scale of 870 €
per bed per day (for 1 year).
Additionally, patients who participated in the
ADD Protocol have reported better care and better
experience (lessened need to visit the hospital) and
practitioners have expressed better satisfaction due
principally to reduction of their workload. Patients
were empowered to address their issues and in the
comfort of their environment; during the 1-year
timeframe, 89% have reported better access to expert
advice and punctuality in receiving care assistance
and 95% had better hygiene. On the other hand, 93%
of patients reported courteous and pleasant
interaction with their care provider Patients reported
with a higher quality experience overall. Though
initially apprehensive about the use of sophisticated
technologies for care at home, the participants in the
project viewed technology integration as an
unalloyed benefit, as they cherish opportunities to be
with loved ones at home rather than in a hospital, with
the ability to quickly resume a normal life. The
project was deemed a success as it has bolstered the
value of HaH as a viable model of care. As a result,
the ADD project was sanctioned and the local level,
into a set of HaH services.
HEALTHINF 2021 - 14th International Conference on Health Informatics
348

4 REFLECTIONS
As a complex system, the H-SES must be dynamic,
allowing for constant change but minimizing
disruption in the outcome of the services. The
robustness of the system must balance its flexibility
to adapt, reconfigure in the face of changes in the
environment, conditions and constraints.
This is a use case of exploiting technology to re-
configure the Healthcare Service Ecosystem with
structured coordination activities, patient and
caregiver involvement, training of practitioners.
While we can detect the contribution of the usual
suspects in a technology implementation, this study
underscores the importance of aligning to the
quadruple aim of care, health, cost and meaning in
work (Sikka et al, 2015). Patients can progress their
treatment plans outside the hospices of a hospital,
reducing the care burden on the hospital staff,
lowering the risk on the patient’s health and
significantly curbing the cost of care. Our use case
has shown that HaH, when done right, can (1)
Improve effectiveness of care (e.g., lower
readmission rates for heart failure patients); (2)
Reduce the threat of complications, for improved care
outcome; (3) Provide timeliness of care – improving
patient access to care; (4) Increase the satisfaction of
the variety of actors in the system (Patients,
providers, etc.); and (5) Reduce burden and cost on
the Hospitals.
In general, systems thinking studies have
considered variety, variability and uncertainty as
pillars for defining actions and interconnections
among actors. Our use case reinforces this thinking
by introducing examples of adaptation, and re-
configurability.
From the perspective of adaptation, we make
evident how healthcare entities need to change and
update protocols, procedures, operations, by
following local needs, and adapting to physical,
technological and infrastructural constraints. In our
case, the use of technology underscored the
advantage of integrating clinical actions with existing
technical trends and tools. Lessons can be drawn for
the implementation of a wider component of this
ecosystem that solves for the crowding hospitals, in
the seasonal peak of particular diseases, outside the
structural limits of such a traditional hospital
department, in the absence of doctors, medical teams
or other personnel for any reasons.
Another perspective is how the healthcare
ecosystem was reconfigured to deal with the variety,
variability and uncertainty of the conditions in
settings outside the perimeter of the traditional
hospital, taking into account the sustainability of
service provision, the lean management of resources
(including people efforts), and the self-learning
actions to implement the specialized know-how and
skills/competences in care giving.
5 CONTRIBUTION
Grounded in the works of contemporary scholars, this
paper offers valuable insights for future
implementation of similar HaH solutions that align
with the quadruple aim principles. The modular
design of the HaH technical solution was an
important element in its success, demonstrating a real
capacity to solve patient’s problems and chronical
difficulties. The system could be used by patients
with different health conditions, in different setting,
with or without the assistance of caregivers, with
exchangeable modes to make an efficient and high
quality healthcare service. Yet, such
implementations bring forth a set of adoption and
ethical issues to deal with, as addressed hereafter.
Historically, HaH has had faced a number of
ethical, legal and clinical practice issues, at the levels
of data-protection, patients’ privacy, training of
family caregiver, discharge planning, etc. (Arras &
ubler, 1994; Budd et al, 2020). The complexity of the
phenomenon of high-tech home care has exposed
patient data to be available to the occasional user of
the devices at a distance from potential governance
measures, otherwise available inside the hospital
systems. Medical teams have to include in their
decisions patients’ preferences, the agreed upon free
choice paradigm can contrast with hospital proposals,
the digital divide can introduce troubles in terms of
distant treatments, there can be such a problem of
infrastructure constraints, like the accessibility, or
difficulties in sensitization and informed consent.
Other frictions could occur when the service is
experienced effectively, as in the case when the care
at home comes too late as a consequence of previous
errors in diagnosis, or when rapid readmissions are
not possible/practicable.
6 CONCLUSION
In closing, this paper has presented a HaH
implementation use case, testimonial to the fact that,
notwithstanding issues of ethics, politics and policy
ramifications, HaH is a viable system component in a
H-SES. As in the case of any other complex system
Responding to COVID-19: Potential Hospital-at-Home Solutions to Re-configure the Healthcare Service Ecosystem
349

implementation, there has to be a clear definition for
fit for use and fit for purpose.
Our use case was timely and effective in
upholding the principles of the Quadruple Aim. The
unwavering focus on patient experience, improving
their outcome, lowering their risk and creating a
service ecosystem where all actors are satisfied, costs
are controlled and services are rendered effectively.
The project was deemed a success as it has bolstered
the value of HaH as a viable model of care. As a
result, the ADD project was sanctioned and the local
level, into a set of HaH services.
Nowadays, clinicians are leading service
reconfiguration to cope with COVID-19, through
learning new skills, adapting and exploiting new
means of consultations. In other cases, hospitals have
had to reconfigure their health services to reduce the
workload of caregivers during the COVID-19
outbreak. Our use case can be a lesson for the
adaptation of technology for patient empowerment
allowing patients to interact with their care ecosystem
while at their home.
REFERENCES
Al-Balushi, S.; Sohal, A.S.; Singh, J.; Al Hajri, A.; Al Farsi,
Y.M.; Al Abri, R. Readiness factors for lean
implementation in healthcare settings—A literature
review. J. Health Organ. Manag. 2014, 28, 135–153.
Arras, J. D., & Dubler, N. N. (1994). Bringing the hospital
home ethical and social implications of high-tech home
care. The Hastings Center Report, 24(5), S19-S28.
ASME.ORG https://aabme.asme.org/posts/top-6-robotic-
applications-in-medicine
Badr, N. G., Sorrentino, M., & De Marco, M. (2018,
September). Health Information Technology and
Caregiver Interaction: Building Healthy Ecosystems. In
International Conference on Exploring Service Science
(pp. 316-329). Springer, Cham.
Baily, M. A., Bottrell, M., & Lynn, J. (2007). Health care
quality improvement: ethical and regulatory issues. B.
Jennings (Ed.). Hastings Center.
Barile, S., Polese, F., Carrubbo L., “Il cambiamento quale
fattore strategico per la sopravvivenza delle
organizzazioni imprenditoriali”, in S. Barile, F. Polese,
M.Saviano (eds), Immaginare l’Innovazione, pp.1-35,
2012a.
Barile, S., Polese, F., Saviano, M., Carrubbo L. (2016),
“Service Innovation in Translational Medicine”, in
Russo Spena T., Mele C., Nuutinen M. (Eds.),
Innovation in Practices, Perspectives and Experiences,
ed. Springer, pp.417-438, 2016.
Barile, S., Polese, F., Saviano, M., Carrubbo, L., Clarizia,
F. (2012b), “Service Research Contribution to
Healthcare Networks’ Understanding”, in Mickelsson,
J., Helkkulla, A. (eds.), Innovative Service
Perspectives, Hanken School of Economics, Hanken.
Bodenheimer, T.; Lorig, K.; Holman, H.; Grumbach, K.
Patient self-management of chronic disease in primary
care. JAMA 2002, 288, 2469–2475.
Bonadio, B., Huo, Z., Levchenko, A. A., & Pandalai-Nayar,
N. (2020). Global supply chains in the pandemic (No.
w27224). National Bureau of Economic Research.
Breslow, L., “Empowerment, not outreach: serving the
health promotion needs of the inner city”, American
journal of health promotion, vol.7, n.1, p.7, 1992.
Britt, T.W., Castro, C.A., Adler, A.B., “Self-engagement,
stressors, and health: A longitudinal study”, Pers Soc
Psychol Bull, vol.31, n.11, pp.1475-1486, 2005.
Budd, J., Miller, B. S., Manning, E. M., Lampos, V.,
Zhuang, M., Edelstein, M., ... & Short, M. J. (2020).
Digital technologies in the public-health response to
COVID-19. Nature medicine, 1-10.
Sikka, R., Morath, J. M., & Leape, L. (2015). The quadruple
aim: care, health, cost and meaning in work.
Capunzo, M., F. Polese, G. Boccia, L. Carrubbo, F.
Clarizia, and F. De Caro, “Advances in service research
for the understanding and the management of service in
healthcare networks,” Gummesson, E., Mele, C.,
Polese, F. (eds), System Theory and Service Science:
Integrating three perspectives in a new service agenda,
Giannini, Napoli, pp. 14–17, 2013.
Caputo, F. Approccio Sistemico e Co-Creazione di Valore
in Sanità; Edizioni Nuova Cultura: Roma, Italy, 2018.
Carrubbo, L, F. Clarizia, X. Hysa, and A. Bilotta, “New
“smarter” solutions for the healthcare complex service
system,” Gummesson, E., Mele, C., Polese, F.(eds),
System Theory and Service Science: Integrating Three
Perspectives In a New Service Agenda, Giannini,
Napoli, pp. 14–17, 2013.
Carrubbo, L., Bruni, R., Cavacece, Y., Moretta Tartaglione,
A., "Service System Platforms to improve value co-
creation: insights for Translational Medicine", in
Gummesson, E., Mele, C., Polese, F. (eds), System
Theory and Service Science: Integrating three
perspectives in a new service agenda, Napoli, 09-12.
2015.
CDC.ORG - https://cdc.gov/coronavirus/2019-
ncov/hcp/telehealth.html
Ciasullo, M. V., Cosimato, S., & Pellicano, M. (2017).
Service innovations in the healthcare service
ecosystem: a case study. Systems, 5(2), 37.
Cohen, S.R.; Hassan, S.A.; Lapointe, B.J.; Mount, B.M.
Quality of life in HIV disease as measured by the
McGill quality of life questionnaire. Aids 1996, 12,
1421–1427.
Finsterwalder, J., & Kuppelwieser, V. G. (2020).
Equilibrating resources and challenges during crises: a
framework for service ecosystem well-being. Journal
of Service Management.
Frow, P., J. R. McColl-Kennedy, T. Hilton, A. Davidson,
A. Payne, and D. Brozovic, “Value propositions: A
service ecosystems perspective,” Marketing Theory,
vol. 14, no. 3, pp. 327–351, 2014
HEALTHINF 2021 - 14th International Conference on Health Informatics
350
Frow, P., McColl-Kennedy, J. R., Payne, A., & Govind, R.
(2019). Service ecosystem well-being:
conceptualization and implications for theory and
practice. European Journal of Marketing
Grimm CA. Hospital Experiences Responding to the
COVID-19 Pandemic: Results of a National Pulse
Survey March 23–27, 2020. U.S. HHS. OIG.
Gruman, J., Rovner, M.H., French, M.E., Jeffress, D.,
Sofaer, S., Shaller, D., Prager, D.J., “From patient
education to patient engagement: implications for the
field of patient education”, in Patient education and
counseling, vol.78, n.3, pp.350-356, 2010.
Häring, I., Sansavini, G., Bellini, E., Martyn, N.,
Kovalenko, T., Kitsak, M., ... & Linkov, I. (2017).
Towards a generic resilience management,
quantification and development process: general
definitions, requirements, methods, techniques and
measures, and case studies. In Resilience and risk (pp.
21-80). Springer, Dordrecht.
Hwang, J.; Christensen, C.M. Disruptive innovation in
health care delivery: A framework for business-model
innovation. Health Aff. 2008, 27, 1329–1335.
Ignone, G.; Mossa, G.; Mummolo, G.; Pilolli, R.; Ranieri,
L. Increasing public healthcare network performance
by de-hospitalization: A patient pathway perspective,
Strateg. Outsourc. Int. J. 2013, 6, 85–107.
Leff, B. Acute? Care at home. The health and cost effects
of substituting home care for inpatient acute care: A
review of the evidence. J. Am. Geriatr. Soc. 2001, 49,
1123–1125.
Levine, D. M., Ouchi, K., Blanchfield, B., Saenz, A.,
Burke, K., Paz, M., & Schnipper, J. L. (2020). Hospital-
level care at home for acutely ill adults: a randomized
controlled trial. Ann. Intern. Med., 172(2), 77-85.
Moazzami, B., Razavi-Khorasani, N., Moghadam, A. D.,
Farokhi, E., & Rezaei, N. (2020). COVID-19 and
telemedicine: Immediate action required for
maintaining healthcare providers well-being. Journal of
Clinical Virology, 104345.
Moliner, M.A., “Loyalty, perceived value and relationship
quality in healthcare services”, Journal of Service
Management, vol.20, n.1, pp.76-97, 2009.
P2PH, IHI.ORG; Pathways to Population Health (P2PH) -
http://www.ihi.org/
Polese, F.; Carrubbo, L. Eco-Sistemi di Servizio in Sanità;
G. Giappichelli Editore: Torino, Italy, 2016.
Polese, F.; Carrubbo, L.; Caputo, F.; Sarno, D., “Managing
Healthcare Service Ecosystems: Abstracting a
Sustainability-Based View from Hospitalization at
Home (HaH) Practices”, in Sustainability, pp.1-15.
2018.
Rodríguez Verjan, C.; Augusto, V.; Xie, X.; Buthion, V.
Economic comparison between Hospital at Home and
traditional hospitalization using a simulation-based
approach. J. Enterp. Inf. Manag. 2013, 26, 135–153.
Sofaer, S., Firminger, K., “Patient perceptions of the quality
of health services”, in Annual Review of Public Health,
vol.26, pp.513-559, 2005.
Sweeney, J.C., Danaher, T.S., Mccoll-Kennedy, J.R.,
“Customer effort in value cocreation activities
improving quality of life and behavioral intentions of
health care customers”, in Journal of Service Research,
vol.18, n.3, pp.318-335, 2015.
Thornton, J. (2020). Clinicians are leading service
reconfiguration to cope with covid-19. bmj, 369.
Wilson, M.G. Rapid Synthesis: Identifying the Effects of
Home Care on Improving Health Outcomes, Client
Satisfaction and Health System Sustainability;
McMaster Health Forum: Hamilton, ON, Canada,
2018; 9.
APPENDIX
Figure 2: The new ‘ADD’ flow - From (www.magaldilife.it).
Responding to COVID-19: Potential Hospital-at-Home Solutions to Re-configure the Healthcare Service Ecosystem
351
