
Data Fusion of Histological and Immunohistochemical Image Data for
Breast Cancer Diagnostics using Transfer Learning
Pranita Pradhan
1,2 a
, Katharina K
¨
ohler
3,4
, Shuxia Guo
1,2 b
, Olga Rosin
3,4
, J
¨
urgen Popp
1,2 c
,
Axel Niendorf
3,4
and Thomas Wilhelm Bocklitz
∗,1,2 d
1
Institute of Physical Chemistry and Abbe Center of Photonics, Friedrich Schiller University,
Helmholtzweg 4, Jena, 07743, Th
¨
uringen, Germany
2
Leibniz Institute of Photonic Technology, Albert-Einstein-Straße 9, Jena, 07745, Th
¨
uringen, Germany
3
MVZ Prof. Dr. med. A. Niendorf Pathologie Hamburg-West GmbH,
Lornsenstraße 4-6, Hamburg, 22767, Hamburg, Germany
4
Institute for Histology, Cytology and Molecular Diagnostics,Lornsenstraße 4, Hamburg, 22767, Hamburg, Germany
Keywords:
Breast Cancer, Transfer Learning, Histology, Immunohistochemistry.
Abstract:
A combination of histological and immunohistochemical tissue features can offer better breast cancer diag-
nosis as compared to histological tissue features alone. However, manual identification of histological and
immunohistochemical tissue features for cancerous and healthy tissue requires an enormous human effort
which delays the breast cancer diagnosis. In this paper, breast cancer detection using the fusion of histolog-
ical (H&E) and immunohistochemical (PR, ER, Her2 and Ki-67) imaging data based on deep convolutional
neural networks (DCNN) was performed. DCNNs, including the VGG network, the residual network and the
inception network were comparatively studied. The three DCNNs were trained using two transfer learning
strategies. In transfer learning strategy 1, a pre-trained DCNN was used to extract features from the images
of five stain types. In transfer learning strategy 2, the images of the five stain types were used as inputs to a
pre-trained multi-input DCNN, and the last layer of the multi-input DCNN was optimized. The results showed
that data fusion of H&E and IHC imaging data could increase the mean sensitivity at least by 2% depending
on the DCNN model and the transfer learning strategy. Specifically, the pre-trained inception and residual
networks with transfer learning strategy 1 achieved the best breast cancer detection.
1 INTRODUCTION
Breast cancer is one of the most prevalent cancers
among women. It is diagnosed by a routine procedure
which is based on morphological tissue features in
hematoxylin and eosin (H&E) stained tissue sections
(figure 1a). The morphological tissue features in-
clude tumour size and type, which are regularly docu-
mented to assess the histological grade of breast can-
cer tissue (Webster et al., 2005). These morphologi-
cal tissue features are also used to prevent recurrence
risk of breast cancer and prescribe personalized ther-
apies. Breast cancer is additionally verified by other
staining technique called the immunohistochemical
a
https://orcid.org/0000-0002-0558-2914
b
https://orcid.org/0000-0001-8237-8936
c
https://orcid.org/0000-0003-4257-593X
d
https://orcid.org/0000-0003-2778-6624
(IHC) staining technique. The IHC staining technique
uses antibodies to highlight specific antigens in the
tissue region (Veta et al., 2014), and includes estro-
gen receptor (ER), progesterone receptor (PR) and
human epidermal growth factor-2 (Her2) (figure 1b-
d). Studies have shown that the IHC examination
with ER, PR, Her2 and Ki-67 can detect five molec-
ular breast cancer sub-types to provide adequate per-
sonalized therapies (Perou et al., 2000; Sørlie et al.,
2001; Cheang et al., 2009). However, none of the
studies report a combination of histology (H&E) and
IHC staining techniques (ER, PR, Her2 and Ki-67)
for breast cancer diagnosis. Therefore, in this work,
an integration of IHC imaging technique i.e. hormone
receptors including ER, PR, Her2 and Ki-67 nuclear
protein stained images with H&E stained images is
proposed to gain new insights into breast cancer bi-
ology (Elledge et al., 2000; Damodaran and Olson,
2012). The combination of histology and IHC stain-
Pradhan, P., Köhler, K., Guo, S., Rosin, O., Popp, J., Niendorf, A. and Bocklitz, T.
Data Fusion of Histological and Immunohistochemical Image Data for Breast Cancer Diagnostics using Transfer Learning.
DOI: 10.5220/0010225504950506
In Proceedings of the 10th International Conference on Pattern Recognition Applications and Methods (ICPRAM 2021), pages 495-506
ISBN: 978-989-758-486-2
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
495
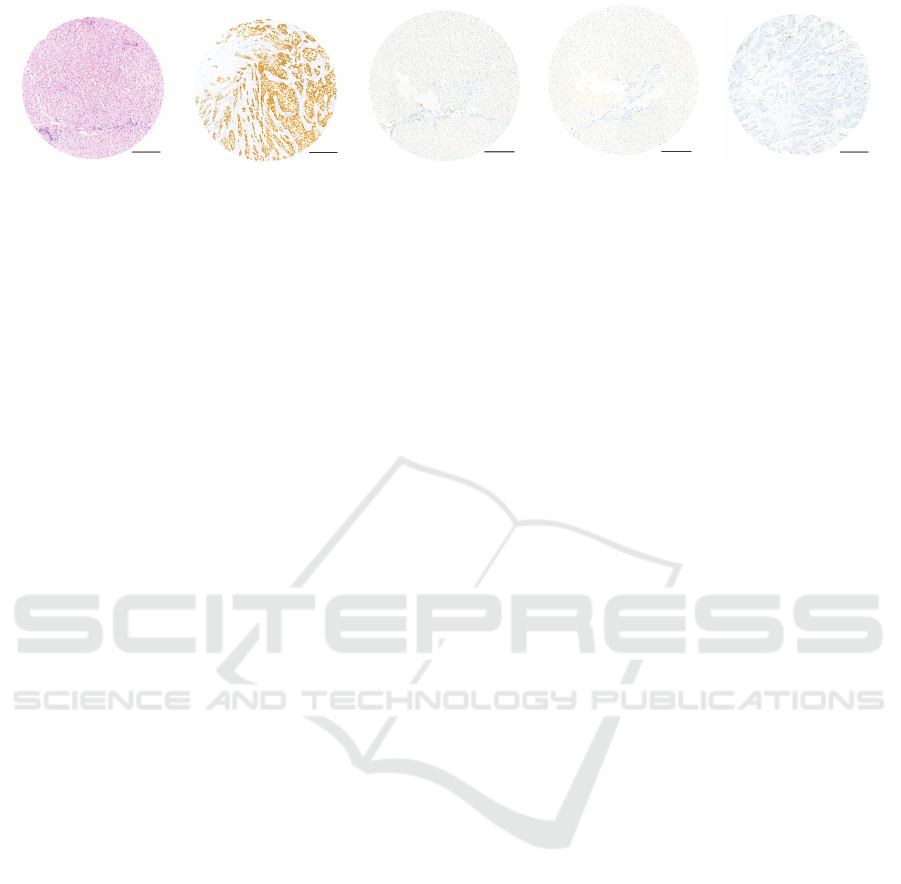
(a) (b) (c) (d) (e)
Figure 1: Five stain type images. (a) Hematoxylin and eosin (H&E), (b) Estrogen receptor (ER), (c) Progesterone receptor
(PR), (d) Human epidermal growth factor-2 (Her2) and (e) Ki-67 protein are shown. Scale bar is 200 µm.
ing technique is referred to as ‘Data fusion’ approach.
Data fusion approach by combining the histologi-
cal and IHC stained images can provide various tissue
features associated with the disease stage and relapse
of breast cancer. However, visual inspection of all five
stained images is a tedious process which can pro-
long the diagnosis. Therefore, automation of breast
cancer detection based on the combination of histo-
logical and IHC imaging data is needed. In this re-
gard, researchers (Pham et al., 2007; Dobson et al.,
2010) used computer-assisted image analysis tech-
niques to automatically monitor changes in the tis-
sue features of histological and IHC stained images
separately. However, computer-assisted image analy-
sis can be limited due to the need for specific soft-
ware systems or the need for user-specific input to
analyze the images. This slows down the process of
analyzing images and providing personalized thera-
pies to the patients. To increase the analysis speed
and reduce human intervention, this work proposes
machine learning (ML) instead of computer-assisted
image analysis techniques.
Conventional ML methods can automatize breast
cancer detection based on the fusion of histological
and IHC imaging data in the following way. First,
the features (e.g. color, shape and texture features)
from the five stain type of imaging data (H&E, ER,
PR, Her2 and Ki-67) can be extracted using image
analysis methods. The feature extraction step in the
conventional ML method is subjective and requires
the effort of an image analyst. Based on the extracted
features, a classification, or a regression model can
be constructed. Subsequently, the classification or the
regression model can be used to make ‘predictions’
(i.e. to predict a class like tumour or normal) on a
new or unseen dataset. Thus, the extracted features
affect the predictions made by the ML model. How-
ever, recently developed ML methods are capable
of performing automatic feature extraction for clas-
sification or regression purpose. These self-learning
methods are categorized into a broad family of ML
called ‘Deep learning’ (DL). The DL models can have
many types of network architectures. Widely used
DL model for images is the deep convolutional neu-
ral network (DCNN) and its numerous applications
are reported in the field of digital pathology (Liu
et al., 2017); for example, cell segmentation or de-
tection (Chen and Chefd’Hotel, 2014), tumour classi-
fication (Cires¸an et al., 2013; Wang et al., 2016) and
carcinoma localization (Janowczyk and Madabhushi,
2016; Coudray et al., 2018; Khosravi et al., 2018;
Sheikhzadeh et al., 2018). Nevertheless, a bottleneck
for DL models is the requirement of huge dataset dur-
ing training, which is difficult to acquire, particularly
in the medical imaging field. In such cases, ‘trans-
fer learning’ methods for DCNNs can be applied for
improving the model performance (Tajbakhsh et al.,
2016).
Transfer learning is the transfer of knowledge
learned on a source task using a source dataset to im-
prove the performance on a target task using the target
dataset (Torrey and Shavlik, 2010). Transfer learning
using any DL model like DCNN can be performed
by three strategies. First, a pre-trained DCNN can be
used as a feature extractor. In this strategy, features
for the target dataset are extracted using a DCNN
trained on different or similar source dataset. The sec-
ond strategy is fine-tuning the weights of the last lay-
ers of a pre-trained DCNN, and the third strategy is
fine-tuning the weights of all layers of a pre-trained
DCNN. In the second and third fine-tuning strategies,
the weights of specific layers of a DCNN trained on a
source dataset are further optimized based on the tar-
get dataset. The three transfer learning strategies like
using a DCNN as a feature extractor or fine-tuning
of a DCNN, requires adequate knowledge of the size
and type of the source and the target dataset (Pan and
Yang, 2010). Transfer learning, if used appropriately,
can improve the initial and final performance of the
DL model on the target dataset. It can also reduce
the total training time of the DL model on the target
dataset. Different transfer learning strategies acquire
different results based on the source and target dataset
which is evident in the next section.
ICPRAM 2021 - 10th International Conference on Pattern Recognition Applications and Methods
496
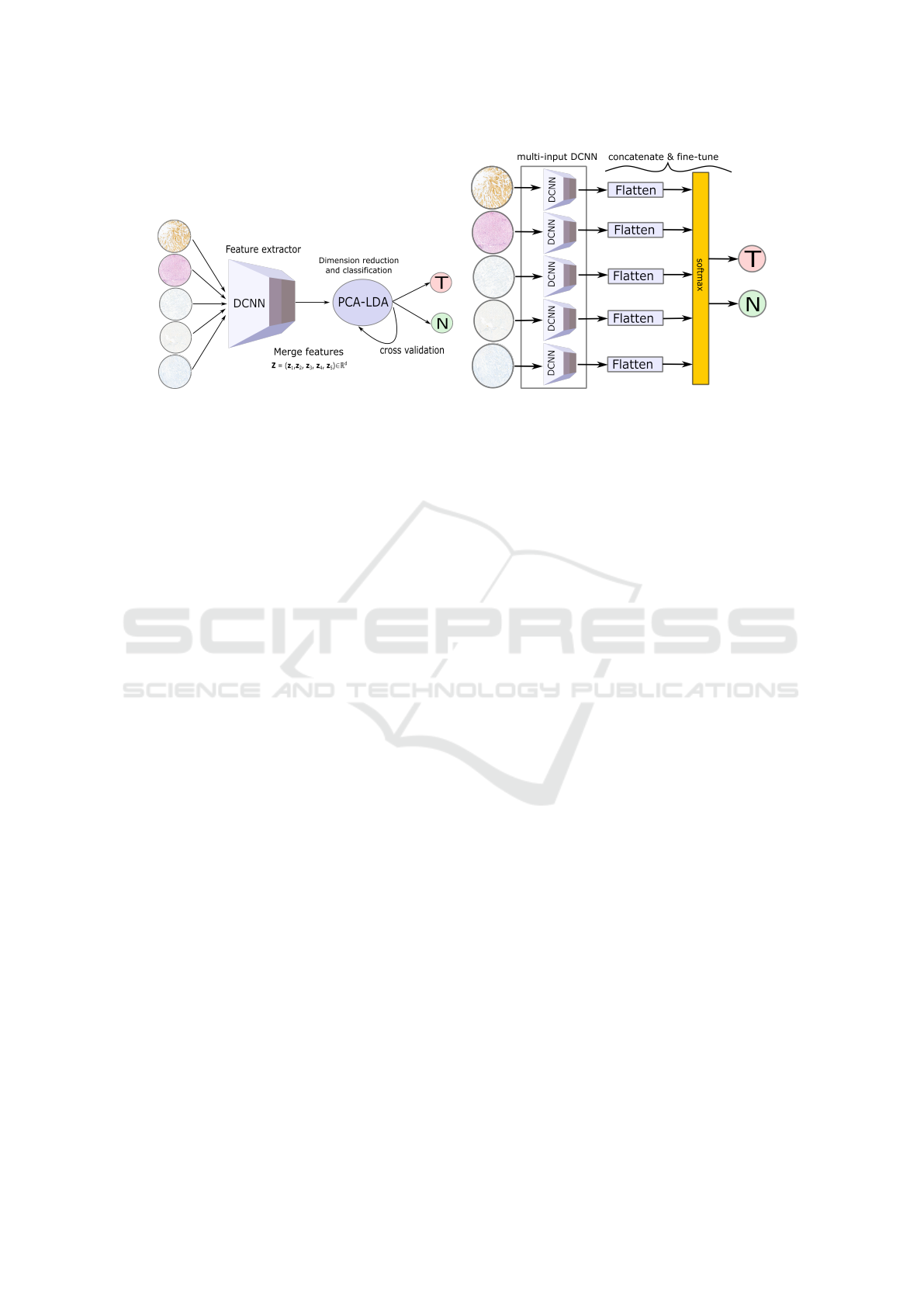
(a) (b)
Figure 2: (a) visualizes transfer learning strategy 1 for data fusion approach where a pre-trained DCNN is used as a feature
extractor. The features extracted from a pre-trained DCNN for all five stain type images are merged and classified into tumour
and normal using the PCA-LDA model. (b) shows transfer learning strategy 2 for data fusion approach where fine-tuning of
the last layer of a pre-trained multi-input DCNN is performed. The five DCNNs are pre-trained models like the VGG16, the
Inceptionv3 or the ResNet50, each having a stain type as its input.
2 RELATED WORK
Transfer learning in medical imaging can be achieved
by training a DCNN on a large medical or non-
medical dataset, and transferring its knowledge to
the target medical dataset (Bayramoglu and Heikkil
¨
a,
2016; Tajbakhsh et al., 2016). A recent study used a
large non-medical dataset like the ImageNet dataset
(Russakovsky et al., 2015) to pre-train a DCNN and
transfer its off-the-shelf features to investigate two
computer-aided detection (CADs) problems namely
thoracoabdominal lymph node detection and intersti-
tial lung disease detection (Shin et al., 2016). In
their work, three different DCNNs including the Ci-
farNet (Krizhevsky and Hinton, 2009), the AlexNet
(Krizhevsky et al., 2012) and the GoogleNet (Szegedy
et al., 2015) were evaluated with three transfer learn-
ing strategies. Similarly, a recent publication (Mor-
mont et al., 2018) compared various transfer learning
strategies based on pre-trained DCNNs using eight
classification datasets in digital pathology. Their re-
sults showed that fine-tuning the ResNet (He et al.,
2016) and the DenseNet (Huang et al., 2017) mod-
els outperformed the other tested models in the mor-
phological classification task. Similar findings were
observed in other references (Antony et al., 2016; Ki-
effer et al., 2017; Ravishankar et al., 2016).
In contrast to the previously mentioned appli-
cations where fine-tuning of a DCNN achieved the
best performance, several other applications using
a DCNN as feature extractor achieved significant
performance on binary and multi-class classification
tasks. These applications included prediction of mor-
phological changes in cells in microscopic images
(Kensert et al., 2018), classification of colon polyps in
endoscopic images (Ribeiro et al., 2016), identifica-
tion of mammographic tumours (Huynh et al., 2016)
and detection of pulmonary nodules in computed to-
mography scans (Van Ginneken et al., 2015). It is
clear from the previous researches that transfer learn-
ing techniques are data-dependent, and a generaliza-
tion of the above-mentioned results is not feasible, es-
pecially in the medical imaging field (Litjens et al.,
2017). Therefore, no consensus of the proper applica-
tion of transfer learning in the medical imaging field
is established. Likewise, the application of transfer
learning, especially for medical imaging data requires
utmost care and further investigations.
In this contribution, data fusion of histological and
immunohistochemical imaging data for classifying
breast cancer is presented for the first time. Due to our
small dataset size, the classification task is performed
using two transfer learning strategies. From previous
experience, the third transfer learning strategy i.e. the
training of a DCNN from scratch is avoided, as it is
computationally expensive and may lead to overfitting
in the absence of large datasets. The performance of
the two transfer learning strategies for the data fusion
approach is compared with histological imaging data.
Moreover, the two transfer learning strategies are per-
formed using three pre-trained DCNN models like the
VGG16 (He et al., 2016), the Inceptionv3 (Szegedy
et al., 2016) and the ResNet50 network (Simonyan
and Zisserman, 2014). The goal of this study was to
verify whether the data fusion approach along with
Data Fusion of Histological and Immunohistochemical Image Data for Breast Cancer Diagnostics using Transfer Learning
497

transfer learning improves the breast cancer diagnosis
based on the sensitivity and F1 score metric.
3 MATERIAL AND METHODS
3.1 Sample Preparation
A Tissue Microarray (TMA) with 97 cores represent-
ing 23 breast cancer cases (78 tumour cores, 18 non-
cancerous tissue cores or the normal breast tissue and
one control core of liver tissue) was produced using
the Manual Tissue Arrayer MTA-1 by Estigen. The
cases were randomly selected out of the daily rou-
tine of MVZ Prof. Dr. med. A. Niendorf Pathologie
Hamburg-West GmbH and anonymized according to
a statement of the ethics committee of the Hamburg
Medical Chamber. Core tissue biopsies (1.0 mm in di-
ameter) were taken from individual FFPE (formalin-
fixed paraffin-embedded) blocks and arranged within
a new recipient block. From the block, 2 µm sections
were cut, placed on glass microscope slides and H&E
staining (figure 1a) following a standard protocol was
performed. Digital images of histology (H&E) slides
were obtained at 40× magnification using the 3DHis-
tech Pannoramic 1000 Flash IV slide scanner with a
spatial resolution of 0.24 µm/pixel (.mrxs image file).
Subsequently, immunohistochemistry staining (ER,
PR, Her2 and Ki-67) (figure 1b-e) was performed on
super frost charged glass slides.
3.2 Image Preprocessing
For the analysis, 96 TMAs or scans (78 tumour
scans and 18 normal scans) from 23 patients were
used, and each TMA had five stain types (H&E,
PR, ER, Her2 and Ki-67). The pixel intensity I of
each TMA was standardized using a min-max scal-
ing (I − I
min
)/(I
max
− I
min
), where I
min
and I
max
is
the minimum and maximum intensity of a pixel in
a TMA. The background pixels were cropped manu-
ally and non-overlapping patches of size 1024×1024
were extracted from a standardized TMA. This led
to 9 patches per TMA (702 tumour and 162 normal
patches). The four corner patches including a large
number of background pixels were removed, leading
to 390 tumour and 90 normal patches. Based on the
480 selected patches, three pre-trained models were
used with two transfer learning strategies.
3.3 DCNN Architectures
To check the robustness of the data fusion approach,
three DCNNs: the VGG network, the Inception net-
work and the residual network, with unique architec-
tures were chosen. The VGG network is a DCNN that
has acquired state-of-the-art performances for image
classification tasks. However, the VGG network can
exhibit the problem of vanishing gradients with an in-
creasing number of layers (Hanin, 2018). Thus, the
residual network which can solve the problem of van-
ishing gradients by adding the ‘shortcut connections’
was explored in this work. Furthermore, the inception
network that provides width in addition to the depth to
a conventional DCNN was utilized. A detailed expla-
nation of the architecture of the three models is given
further.
3.3.1 VGG Network
A VGG network is a DCNN with different configura-
tions from 11 to 16 convolutional layers followed by
three fully connected layers. The number of convo-
lutional layers increases the depth of the VGG net-
work. It is shown that an increase in the depth of
the VGG network decreases the top-5 validation er-
ror (He et al., 2016). However, the decrease in the er-
ror for the VGG network from 16 to 19 convolutional
layers is not significant. Thus, the VGG network
with 16 convolutional layers referred to as VGG16
from Keras was used (Chollet et al., 2015). The in-
put to the VGG16 network was an RGB image of
size 224×224, and each image was preprocessed by
subtracting the mean RGB values computed over the
training dataset.
3.3.2 Inception Network
Deep networks like VGG network require an appro-
priate selection of the number of convolution filters
and filter sizes. For this reason, the inception network
concatenates convolutional layers of different filter
size, including the spatial dimension of 1×1, 3×3
and 5×5. This captures information at various scales
while increasing the computational complexity. In or-
der to reduce the computational cost, a convolutional
layer of 1×1 filter size is applied before each convo-
lutional layer of filter size 3×3 and 5×5. These two
salient features of the Inception network reduce the
dimensionality in the feature space and thereby allows
the network to be deeper and wider. Moreover, the
inception network replaces the fully connected layer
with global averaging layers which reduces the num-
ber of trainable weights, thus reducing over-fitting on
the training dataset (Szegedy et al., 2016). The In-
ceptionv3 implementation from Keras, which has 95
layers and requires an RGB image as input with size
299×299 was used.
ICPRAM 2021 - 10th International Conference on Pattern Recognition Applications and Methods
498
Table 1: This table shows confusion matrices, mean sensitivities and mean F1 scores for the VGG, the Inception and the
residual networks using transfer learning strategy 1. Here, two feature sets extracted from pre-trained models are used; one
feature set is extracted from H&E images only, while the other feature set is extracted from all the five stain types. All metrics
are computed for 96 TMAs by taking majority voting of the predictions acquired for the patches using the PCA-LDA model.
N: normal scans, T: tumour scans.
Data fusion (H&E+IHC imaging data) Only histological imaging data
DCNN
N T
Sens (%) F1 (%) DCNN
N T
Sens (%) F1 (%)
VGG16
N 13 5
79.06 76.24
VGG16
N 14 4
80.56 76.61
T 11 67 T 13 65
Inceptionv3
N 16 2
89.32 85.47
Inceptionv3
N 15 3
88.46 86.97
T 8 70 T 5 75
ResNet50
N 14 4
86.97 87.80
ResNet50
N 14 4
85.68 84.96
T 3 75 T 5 73
Table 2: This table shows confusion matrices, mean sensitivities and mean F1 scores for the VGG, the Inception and the
residual networks using transfer learning strategy 2. Data fusion approach used multi-input DCNN with the five stain type
images as input, whereas a single-input DCNN was used only the H&E image as input. The last layers of both single-input
and multi-input DCNNs were fine-tuned. The mean sensitivities are computed for 96 TMAs by taking majority voting of the
predictions obtained for the patches. N: normal scans, T: tumour scans.
Data fusion (H&E+IHC imaging data) Only histological imaging data
DCNN
N T
Sens (%) F1 (%) DCNN
N T
Sens (%) F1 (%)
VGG16
N 7 11
66.88 70.86
VGG16
N 3 15
55.13 57.57
T 4 74 T 5 73
Inceptionv3
N 0 18
50.00 44.83
Inceptionv3
N 9 9
72.44 75.66
T 0 78 T 4 74
ResNet50
N 0 18
50.00 44.83
ResNet50
N 12 6
81.41 83.78
T 0 78 T 3 75
Table 3: This table shows confusion matrices, mean sensitivities and mean F1 scores for the VGG, the Inception and the
residual network using the two transfer learning strategies. All metrics are computed for 96 TMAs by taking majority voting
of the predictions acquired by the models for patches.
Transfer learning strategy 1 Transfer learning strategy 2
DCNN
N T
Sens (%) F1 (%) DCNN
N T
Sens (%) F1 (%)
VGG16
N 13 5
79.06 76.24
VGG16
N 7 11
66.88 70.86
T 11 67 T 4 74
Inceptionv3
N 16 2
89.32 85.47
Inceptionv3
N 0 18
50.00 44.83
T 8 70 T 0 78
ResNet50
N 14 4
86.97 87.80
ResNet50
N 0 18
50.00 44.83
T 3 75 T 0 78
3.3.3 Residual Network
The configurations of the VGG network show that
deep neural networks achieve good top-5 accuracy
until a certain depth limit (He et al., 2016). An in-
crease in the network depth causes a problem of van-
ishing or exploding gradients (Hanin, 2018) which af-
fects the network convergence and degrades the per-
formance (Simonyan and Zisserman, 2014). There-
fore, the residual networks are built to solve this
degradation problem by adding activations of the top
layers into the deeper layers of the network. For in-
stance, in a deep neural network the activation a of
the (l + 2)
th
layer with weight w and bias b is given as
a
(l+2)
= f [(w
(l+2)
× a
(l+1)
) + b
(l+2)
], (1)
where f is an activation function like linear recti-
fied unit ( f = max (a
(l+2)
,0)). However, in a resid-
ual block the activation a of the l
th
layer (or an iden-
tity mapping) is added via the ‘skip or shortcut con-
nections’ (Bishop et al., 1995; Venables and Ripley,
2013) to the (l +2)
th
layer of the network. Therefore,
the activation of the (l +2)
th
layer in a residual block
can be given a
a
(l+2)
= f [(w
(l+2)
× a
(l+1)
) + b
(l+2)
+ a
(l)
]. (2)
This implies that in worse cases when the network
Data Fusion of Histological and Immunohistochemical Image Data for Breast Cancer Diagnostics using Transfer Learning
499

fails to learn representative features, i.e. w
(l+2)
= 0
and b
(l+2)
= 0, the output still remains an identity
mapping of the input a
l
. In residual networks, a se-
ries of residual blocks along with intermediate nor-
malization layers was used; thus improving the learn-
ing of the deep neural networks. In this work, the
ResNet50 implementation from Keras, which has 152
layers and requires an RGB image as an input with
size 224×224, was used.
The above explained three DCNN models were
trained using two transfer learning strategies which
are discussed in the next section.
3.4 Transfer Learning Strategies
The above-mentioned DCNNs were utilized for two
transfer learning strategies. For the first strategy, a
pre-trained DCNN model to extract off-the-shelf fea-
tures followed by a linear classifier was used. In
the second strategy, a multi-input pre-trained DCNN
model followed by a softmax classifier was used.
Both strategies were performed on a commercially
available PC system intel
R
Core
TM
with NVIDIA
GeForce GTX 1060, 6GB with python packages:
Keras(Chollet et al., 2015), Tensorflow(Abadi et al.,
2015), Scikit-learn (Pedregosa et al., 2011), Scipy
(Jones et al., 2001) and Numpy (Oliphant, 2006).
3.4.1 DCNN as Feature Extractor
In the first strategy (figure 2a), features z
i
∈ R
m
,i =
(1,2,3,4,5) were extracted for patches of each stain
type i using the pre-trained VGG16, Inceptionv3 and
ResNet50 networks. The patches were resized ac-
cording to the model’s input size requirement. For
a patch of a single stain type, 25,088 features were
extracted by the VGG16 (feature shape: 1, 7, 7,
512), 51,200 features were calculated by the Incep-
tionv3 (feature shape: 1, 5, 5, 2048) and 2048 fea-
tures were obtained by the ResNet50 (feature shape:
1, 1, 1, 2048). For data fusion approach, the fea-
tures from all five stain types were concatenated, z =
(z
1
,z
2
,z
3
,z
4
,z
5
) ∈ R
d
(d m) resulting in ∼0.12
million features by the VGG16 model, ∼0.25 mil-
lion features by the Inceptionv3 model and 10,240
features by the ResNet50 model per patch. For his-
tological imaging data, i.e. without the data fusion
approach, the features extracted only from the H&E
images were used. In both cases, the large feature
dimension of each patch was reduced by principal
component analysis (PCA) model, and classified as
normal or tumour using linear discriminant analy-
sis (LDA) model (Hastie et al., 2009). The PCA-
LDA model was evaluated using internal and external
cross-validation scheme explained elsewhere (Guo
et al., 2017). Shortly, the internal cross-validation
was used to optimize the number of PC’s of the PCA-
LDA model. The external cross-validation was used
to predict an independent test dataset based on the
PCA-LDA model. The external cross-validation used
leave-one-patient-out cross-validation, such that the
patches acquired from TMAs of 23 patients were used
at least once as an independent test dataset. The in-
ternal cross-validation used 10 fold cross-validation.
The predictions by the PCA-LDA model acquired for
the patches from the external cross-validation step
were voted to assign each TMA into a tumour or nor-
mal class. Based on the predicted TMA labels (ob-
tained after majority voting of the patches) and true
TMA labels, metrics like confusion matrix, mean sen-
sitivity and mean F1 score were reported. The mean
sensitivity and the mean F1 score were calculated us-
ing an average of the mean sensitivities and the mean
F1 scores for the tumour and normal class, respec-
tively. Lastly, the transfer learning strategy 1 was per-
formed for all the three DCNNs and their classifica-
tion performance based on TMAs was compared.
3.4.2 Fine-tuning of DCNN
In the second strategy (figure 2b), for histologi-
cal imaging data, a single-input DCNN was used;
whereas for the data fusion approach, a multi-input
DCNN was used. The multi-input DCNN model N
was constructed using five pre-trained models of the
same architecture; for instance, five pre-trained VGG
networks each using a stain type image as an in-
put. The input to the multi-input DCNN model was
the five stained images (H&E, ER, Her2, Ki-67 and
PR). The last layer of the multi-input DCNN models
was concatenated and followed by a dense layer with
two outputs (corresponding to the normal and tumour
class) with a softmax activation layer. The softmax
activation layer mapped the non-normalized output of
the model N to the distribution of K probabilities and
is defined as
P(r)
i
=
exp(r
i
)
∑
K
j=1
exp(r
j
)
, (3)
where r = (r
1
,· · ·, r
K
) and K = 2 for a binary clas-
sification task. During the training process, the last
two layers were fine-tuned using Adam optimizer
(Kingma and Ba, 2014) with a learning rate 0.001 and
mini-batch size of 5 patches. To allocate higher class
weight for the minority class (here, the normal class),
the weighted binary cross-entropy loss function
L = −
K
∑
i
α
i
y
i
log(P(r)
i
) (4)
ICPRAM 2021 - 10th International Conference on Pattern Recognition Applications and Methods
500

was used, where α
i
=
1
#K
i
, y
i
, P(r)
i
are the weight,
ground truth and the probability from the softmax ac-
tivation layer of the i
th
class in K, respectively. The
model was evaluated using the mean sensitivity and
the mean F1 score similar to transfer learning strat-
egy 1.
For the evaluation of the single and multi-input
DCNN, the dataset was divided into three parts: train-
ing, validation and testing. In every iteration, patches
of one patient were used as an independent test dataset
and the patches of remaining patients were used as
training and validation dataset. To avoid any train-
ing bias, the training and validation datasets were
randomly split patient-wise such that patches from
30% patients were used as validation dataset and the
rest as the training dataset. In other words, during
each iteration, patches of one patient were used as the
test dataset, patches of 16 patients formed the train-
ing dataset and patches of remaining 6 patients be-
longed to the validation dataset. The combination of
16 and 6 patients in training and validation datasets
were chosen randomly. The iterations were repeated
until all 23 patients were used as an independent test
dataset. Further, every iteration was executed for ten
epochs, and validation sensitivity was monitored for
early stopping of the model training. The model with
best validation sensitivity was used for predicting the
independent test dataset in that iteration. In this way,
the patches of all 23 patients were used individually
as an independent test dataset, and majority voting
of the patches similar to transfer learning strategy 1
was performed. The confusion matrices and aver-
age of the mean sensitivities for the normal and tu-
mour classes were evaluated using the independent
test dataset. Subsequently, transfer learning strategy
2 was performed for all the three pre-trained DCNN
models with the same hyper-parameter setting.
3.4.3 ROC Curve Analysis for TMAs
The results of the two transfer learning strategies were
obtained as ROC curves showing the true and the
false positive rate for the tumour class. The ROC
curves were evaluated for TMAs based on the major-
ity voting of the selected patches. To achieve ROC
curves for TMAs, the model output in the form of
probabilities of each patch for the tumour class was
thresholded using 100 different values in the range
[0, 1]. This led to predictions for patches with dif-
ferent threshold values. Subsequently, the predic-
tions for patches obtained for each threshold value
were majority voted to obtain a prediction for a TMA.
The predictions for TMAs were used to calculate the
true positive rate, the false positive rate and the ROC
curve, as shown in figure 3 and 4. The predictions
for the TMAs obtained with 0.5 threshold were used
to obtain the confusion matrix, mean sensitivities and
mean F1 scores as reported in table 1, 2 and 3.
4 RESULTS
The main aim of this work was to confirm that the
data fusion approach can achieve better breast can-
cer diagnosis than histological imaging data based on
performance metrics. This was confirmed by one of
the two transfer learning strategies. The results are
divided in three parts as shown in table 1, 2 and 3.
Table 1 and 2 report performance metrics obtained
for transfer learning strategy 1 and transfer learning
strategy 2, with and without data fusion approach, re-
spectively. Table 3 shows a comparison of the two
transfer learning strategies using only the data fusion
approach. In table 1, 2 and 3 report values for the
VGG16, the Inceptionv3 and the ResNet50 models.
These values were evaluated for 96 TMAs acquired
by majority voting of the five patches extracted from
each TMA.
The results in table 1 show that the pre-trained
features acquired from the data fusion approach yield
slightly higher mean sensitivities and mean F1 scores
in comparison to the pre-trained features extracted
from the histological imaging data. Higher mean sen-
sitivities using the data fusion approach were seen for
at least two of the three DCNNs. Higher mean F1
score using the data fusion approach was seen only
for the ResNet50 model. Specifically, the pre-trained
features obtained from the data fusion approach us-
ing the Inceptionv3 and the ResNet50 models showed
mean sensitivities 89.32% and 86.97%, respectively.
Similarly, the mean F1 scores for the two models
were 85.47% and 87.80%, respectively. In compari-
son, the pre-trained features from the histological data
using the same DCNN model showed mean sensitiv-
ities 88.46% and 85.68%, respectively. Thus, there
was approximately 2% increase in the model perfor-
mance by data fusion approach based on the mean
sensitivity, which is significant from a clinical per-
spective. However, the VGG16 model showed higher
mean sensitivity (80.56%) using histological imaging
data compared to the mean sensitivity calculated for
the data fusion approach (79.06%). Overall, it can be
seen that transfer learning using pre-trained DCNN
features and a linear classification model (PCA-LDA)
based on data fusion approach show a slight improve-
ment in breast cancer detection in some cases for a
small dataset as in our study.
Contrarily, table 2 obtained by the transfer learn-
ing strategy 2 shows lower mean sensitivities for
Data Fusion of Histological and Immunohistochemical Image Data for Breast Cancer Diagnostics using Transfer Learning
501
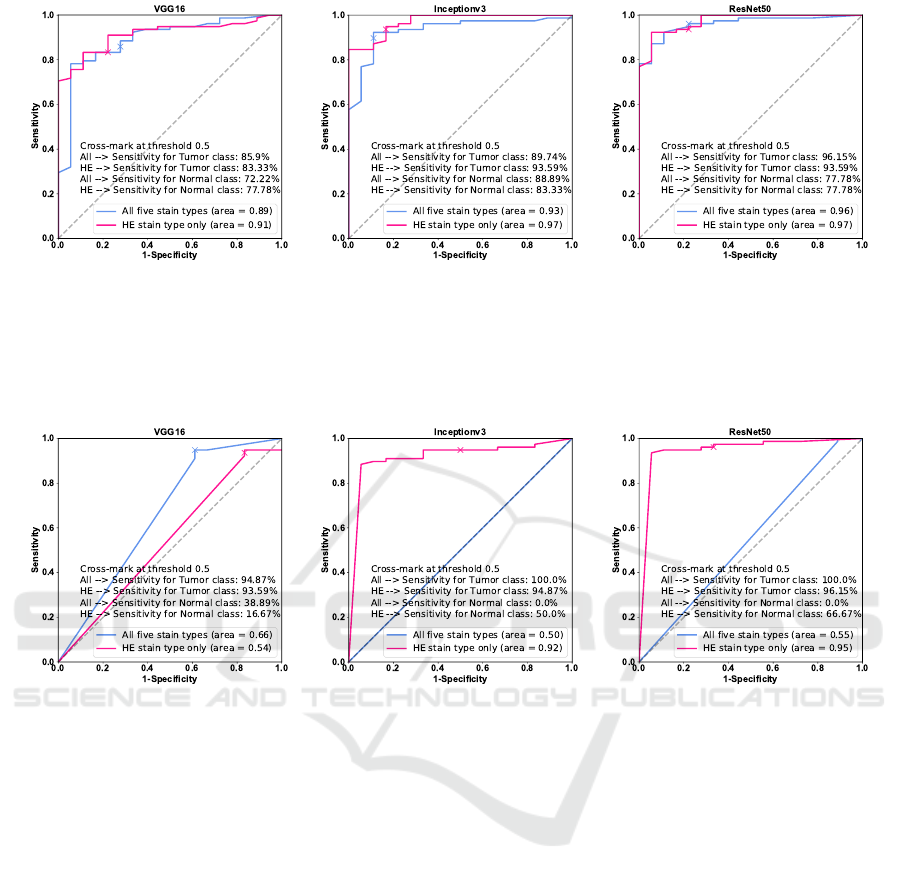
(a) (b) (c)
Figure 3: (a-c) show ROC curves for the VGG16, the Inceptionv3 and the ResNet50 networks using the transfer learning
strategy 1 based on TMAs. The blue line shows ROC curve for the PCA-LDA model trained using the pre-trained DCNN
features obtained from the histological and IHC imaging data, whereas the pink line shows ROC curve for the PCA-LDA
model trained using pre-trained DCNN features extracted from the histological imaging data only. The cross-mark shows the
true and the false positive rate on the ROC curve with 0.5 threshold.
(a) (b) (c)
Figure 4: (a-c) show ROC curves for the VGG16, the Inceptionv3 and the ResNet50 networks using the transfer learning
strategy 2 based on TMAs. The blue line shows ROC curve for the multi-input DCNN model fine-tuned using the histological
and IHC imaging data, whereas the pink line shows the ROC curve for the single-input DCNN model fine-tuned using only
the histological imaging data. The cross-mark shows the true and the false positive rate at 0.5 threshold.
the data fusion approach in comparison to the per-
formance achieved by using histological imaging
data alone. Except for the multi-input VGG16 net-
work, the multi-input Inceptionv3 and the multi-input
ResNet50 network trained with a combination of his-
tological and IHC imaging data predicted all normal
patches as tumour patches. Thus, the multi-input
Inceptionv3 and the multi-input ResNet50 model
achieved mean sensitivity of 50% and mean F1 score
of 44.83%; whereas, the multi-input VGG16 network
showed mean sensitivity of 66.88% and mean F1
score of 70.86% for the data fusion approach. The
mean sensitivity of the single-input VGG16 network
declined to 55.13% when only histological imaging
data was used. On the other hand, the single-input
Inceptionv3 and the single-input ResNet50 models
using histological imaging data showed an opposite
trend with comparatively higher mean sensitivities of
72.44% and 81.41%, and higher mean F1 scores of
75.66% and 83.78%, respectively. Overall, it was ob-
served that transfer learning performed by fine-tuning
the last layer of the pre-trained multi-input DCNNs
result in lower mean sensitivities for the data fusion
approach. This behaviour can be a consequence of
the small sample size. It is clear from the results that
fine-tuning the last layer of DCNNs is not the best ap-
proach for our small breast cancer dataset. Thus, it
is suspected that the fine-tuning of all the layers of a
DCNN will decrease the model performance further.
However, fine-tuning of all layers for large breast can-
cer dataset should be investigated in the future.
Lastly, the performance of the two transfer learn-
ing strategies for the data fusion approach is summa-
rized in table 3, where higher mean sensitivities are
reported for strategy 1, i.e. using pre-trained features
from the VGG16, the Inceptionv3 and the ResNet50
ICPRAM 2021 - 10th International Conference on Pattern Recognition Applications and Methods
502

model. The training of the PCA-LDA model based
on pre-trained features of the Inceptionv3 and the
ResNet50 network yield promising results. The re-
sults from the VGG16 network are lower in compari-
son to the other two models for transfer learning strat-
egy 1, but higher for transfer learning strategy 2.
The performance of the two transfer learning
strategies based on TMAs is summarized in the form
of ROC curves in figure 3 and 4. The ROC curve
calculated for the data fusion approach and histolog-
ical imaging data at various thresholds is depicted in
blue and pink, respectively. The AUC values given in
the figure legend show lower values for the data fu-
sion approach in comparison to the AUC values cal-
culated using histological imaging data. This trend
is observed for both the transfer learning strategies.
From figure 3 and 4, it can be inferred that the over-
all performance of DCNN models trained using an
H&E image is better for both transfer learning strate-
gies. However, the final performance of the models in
terms of mean sensitivities evaluated at 0.50 threshold
is better for the data fusion approach in some cases.
The mean sensitivities cross-marked in each subplot
of figure 3 and 4 are calculated at 0.50 threshold coin-
cide with the values reported in table 1, 2 and 3. These
values are evaluated for TMA’s by performing major-
ity voting of the five patches in each TMA. The ROC
curves at threshold 0.50 which is mostly used to eval-
uate the model performance, show higher mean sensi-
tivities for data fusion approach than using histologi-
cal data, at least for the Inceptionv3 and the ResNet50
model in transfer learning strategy 1 (figure 3). Nev-
ertheless, the AUC derived from the ROC curves for
transfer learning strategy 2 (figure 4) show low mean
sensitivities for all the DCNN networks. The incon-
sistency in the results of two transfer learning strate-
gies can be due to various reasons discussed below.
5 DISCUSSION
Based on the results, three critical findings can be dis-
cussed.
5.1 Data Fusion vs. Histological
Imaging
The results showed that the data fusion approach, i.e.
combining histological and IHC imaging data, in-
creases the model performance by ∼2%. However,
the increase in model performance was achieved only
for transfer learning strategy 1, where features were
extracted from a pre-trained DCNN followed by bi-
nary classification using the PCA-LDA model. It is
important to mention that the analysis was performed
on a limited number of TMAs and it is suspected that
the results can improve with an increasing number of
TMAs, at least for the transfer learning strategy 1.
Furthermore, the data fusion approach can largely in-
crease the feature dimension of the data, thus increas-
ing computational complexity. Nevertheless, these
limitations are the cost of performing reliable and
early breast cancer diagnosis. In future studies, fea-
ture dimension can be reduced by extracting features
from the last layers and a comparative study can be
performed.
5.2 Strategy 1 vs. Strategy 2
From the results shown in table 3 it is clear that
transfer learning strategy 1 outperforms the transfer
learning strategy 2 for our breast cancer dataset. For
transfer learning strategy 2, the misclassification of
the under-represented normal class as tumour class is
higher. This means that transfer learning strategy 2
performed by merging and fine-tuning the last layer
of the pre-trained multi-input model causes ‘negative
transfer learning’ showing lower binary classifica-
tion performance. Although the past studies (Kensert
et al., 2018; Mormont et al., 2018) have shown that
transfer learning strategy 2 for medical imaging data
can provide good classification performances, these
studies used a single-input DCNN for fine-tuning;
whereas, in this study a multi-input DCNN was used.
Thus, training a large multi-input network on a small
dataset can cause the model to overfit and degrade
its performance. Degradation in model performance
can also be a consequence of transferring features
of top layers from two different domains (Yosinski
et al., 2014). Specifically, the transferability of fea-
tures can be negatively affected when the source task
(e.g. classification of the ImageNet dataset) is differ-
ent from the target task (e.g. breast cancer detection).
Thus, transfer learning of features for different do-
mains should be performed cautiously (Yosinski et al.,
2014). Further, merging and fine-tuning only the last
layer and initializing the weights of the whole net-
work based on the ImageNet dataset transferred the
specific features (learned in top layers) of the non-
medical domain to the medical domain, thus decreas-
ing the classification performance in the strategy 2.
To improve the performance of a DCNN model by
the transfer learning strategy 2, initializing and fine-
tuning weights of the top and intermediate layers of
the multi-input DCNN model should be investigated
in future studies.
So far, limitations of the transfer learning strategy
2 were discussed, now it is important to discuss few
Data Fusion of Histological and Immunohistochemical Image Data for Breast Cancer Diagnostics using Transfer Learning
503

limitations of the transfer learning strategy 1. One
of the limitations is the need for an aggressive down-
sampling of the pathological images according to the
input size of the pre-trained DCNN, ignoring the es-
sential information. Although it is also possible to use
a desired input image size by removing the fully con-
nected layers of a pre-trained DCNN, downsampling
our patches of size 1024×1024 to the model’s in-
put size facilitated the best classification performance.
Extracting smaller size patches to increase the num-
ber of patches were also evaluated during the analysis.
However, it was observed that small size patches in-
creased the dataset size but decreased the biologically
significant tissue features in each patch. Irrespective
of our acceptable results using the pre-trained DCNNs
as feature extractors, the interpretability of the trans-
ferred features is questionable. It is difficult to ob-
tain an intuitive understanding of the transferability
of non-medical features obtained from the ImageNet
dataset to the medical domain. Thus, it is important to
investigate transferring features from the medical do-
main to improve the breast cancer classification rate
in future.
5.3 Effect of DCNN Architecture
It was clear from the results that acquiring a good
classification rate using data fusion approach is de-
pendent on the DCNN model. For transfer learn-
ing strategy 1, the Inceptionv3 and the ResNet50
network achieved better classification performances.
While for transfer learning strategy 2, the multi-input
VGG16 network achieved good classification perfor-
mance. Furthermore, for transfer learning strategy
1, the Inceptionv3 and the VGG16 provided a large
number of features (as they were combined from mul-
tiple modalities) in comparison to the ResNet50 net-
work. Large feature dimension not only increased the
dataset size but also increased the memory require-
ment. However, large feature dimension obtained by
large DCNNs like the Inceptionv3 and the ResNet50
proved to be beneficial for training the PCA-LDA
model in transfer learning strategy 1. While for trans-
fer learning strategy 2, it was seen that large DCNN
like the multi-input Inceptionv3 and the multi-input
ResNet50 networks easily overfit and degrade model
performance. It is suspected that large networks
in multi-input fashion like the Inceptionv3 and the
ResNet50 network generates a large number of train-
able parameters which degrades model performance
during fine-tuning. Furthermore, the time required
to fine-tune the last layers of networks increases with
network size.
6 CONCLUSION
The results show that combining histological imaging
data along with IHC imaging data (estrogen recep-
tor, progesterone receptor, human epidermal growth
factor-2 and Ki-67) can improve breast cancer classi-
fication rate as compared to histological imaging data
alone. The improvement in the classification perfor-
mance was approximately 2% when deep convolu-
tional neural networks (DCNN) were used as feature
extractors (i.e. transfer learning strategy 1). However,
the classification performance degraded when fine-
tuning of the last layer of the multi-input DCNN (i.e.
transfer learning strategy 2) was performed. Out of
all three pre-trained networks, the pre-trained resid-
ual network and inception network as feature extrac-
tor outperformed the binary classification task (tu-
mour vs normal), while the pre-trained VGG network
as feature extractor obtained reasonable results. On
the other hand, the VGG network showed better per-
formances than the residual network and the incep-
tion network when fine-tuning of last layers was per-
formed. The increase in performance by 2% for di-
agnosing breast cancer is explainable, because this
task is normally performed using H&E, so the ad-
vancement is limited. Nevertheless, the data fusion
approach can substantially improve differential diag-
nosis, which is important from a clinical perspec-
tive. Therefore, combining histology and IHC stain-
ing technique should be encouraged in future for more
complicated tasks like a differential diagnosis or the
prognosis of breast cancer patients. Overall, this com-
parative study showed that transfer learning could be
utilized to diagnose breast cancer based on the com-
bined histological and IHC imaging data with accept-
able results. However, it is important to perform this
study on a larger dataset in future. On large dataset,
transfer learning strategy 3 i.e. training a DCNN from
scratch can also be investigated. Furthermore, the
data fusion approach can be performed to characterize
stages of breast cancer in future.
ACKNOWLEDGEMENTS
Financial support of the German Science Foundation
(BO 4700/1-1, PO 563/30-1 and STA 295/11-19) and
funding by the BMBF for the project Uro-MDD (FKZ
03ZZ0444J) are highly acknowledged.
ICPRAM 2021 - 10th International Conference on Pattern Recognition Applications and Methods
504

REFERENCES
Abadi, M., Agarwal, A., Barham, P., Brevdo, E., Chen, Z.,
Citro, C., Corrado, G. S., Davis, A., Dean, J., Devin,
M., Ghemawat, S., Goodfellow, I., Harp, A., Irving,
G., Isard, M., Jia, Y., Jozefowicz, R., Kaiser, L., Kud-
lur, M., Levenberg, J., Man
´
e, D., Monga, R., Moore,
S., Murray, D., Olah, C., Schuster, M., Shlens, J.,
Steiner, B., Sutskever, I., Talwar, K., Tucker, P., Van-
houcke, V., Vasudevan, V., Vi
´
egas, F., Vinyals, O.,
Warden, P., Wattenberg, M., Wicke, M., Yu, Y., and
Zheng, X. (2015). TensorFlow: Large-scale machine
learning on heterogeneous systems. Software avail-
able from tensorflow.org.
Antony, J., McGuinness, K., O’Connor, N. E., and Moran,
K. (2016). Quantifying radiographic knee osteoarthri-
tis severity using deep convolutional neural networks.
In 2016 23rd International Conference on Pattern
Recognition (ICPR), pages 1195–1200. IEEE.
Bayramoglu, N. and Heikkil
¨
a, J. (2016). Transfer learning
for cell nuclei classification in histopathology images.
In European Conference on Computer Vision, pages
532–539. Springer.
Bishop, C. M. et al. (1995). Neural networks for pattern
recognition. Oxford university press.
Cheang, M. C., Chia, S. K., Voduc, D., Gao, D., Leung,
S., Snider, J., Watson, M., Davies, S., Bernard, P. S.,
Parker, J. S., et al. (2009). Ki67 index, her2 status,
and prognosis of patients with luminal b breast can-
cer. JNCI: Journal of the National Cancer Institute,
101(10):736–750.
Chen, T. and Chefd’Hotel, C. (2014). Deep learning
based automatic immune cell detection for immuno-
histochemistry images. In International workshop on
machine learning in medical imaging, pages 17–24.
Springer.
Chollet, F. et al. (2015). Keras. https://github.com/fchollet/
keras.
Cires¸an, D. C., Giusti, A., Gambardella, L. M., and Schmid-
huber, J. (2013). Mitosis detection in breast cancer
histology images with deep neural networks. In In-
ternational conference on medical image computing
and computer-assisted intervention, pages 411–418.
Springer.
Coudray, N., Ocampo, P. S., Sakellaropoulos, T., Narula,
N., Snuderl, M., Feny
¨
o, D., Moreira, A. L., Raza-
vian, N., and Tsirigos, A. (2018). Classification and
mutation prediction from non–small cell lung cancer
histopathology images using deep learning. Nature
medicine, 24(10):1559–1567.
Damodaran, S. and Olson, E. M. (2012). Targeting the hu-
man epidermal growth factor receptor 2 pathway in
breast cancer. Hospital Practice, 40(4):7–15.
Dobson, L., Conway, C., Hanley, A., Johnson, A., Costello,
S., O’Grady, A., Connolly, Y., Magee, H., O’Shea, D.,
Jeffers, M., et al. (2010). Image analysis as an adjunct
to manual her-2 immunohistochemical review: a diag-
nostic tool to standardize interpretation. Histopathol-
ogy, 57(1):27–38.
Elledge, R. M., Green, S., Pugh, R., Allred, D. C., Clark,
G. M., Hill, J., Ravdin, P., Martino, S., and Osborne,
C. K. (2000). Estrogen receptor (er) and progesterone
receptor (pgr), by ligand-binding assay compared with
er, pgr and ps2, by immuno-histochemistry in predict-
ing response to tamoxifen in metastatic breast can-
cer: A southwest oncology group study. International
journal of cancer, 89(2):111–117.
Guo, S., Bocklitz, T., Neugebauer, U., and Popp, J. (2017).
Common mistakes in cross-validating classification
models. Analytical Methods, 9(30):4410–4417.
Hanin, B. (2018). Which neural net architectures give rise
to exploding and vanishing gradients? In Advances in
Neural Information Processing Systems, pages 582–
591.
Hastie, T., Tibshirani, R., and Friedman, J. (2009). The el-
ements of statistical learning: data mining, inference,
and prediction. Springer Science & Business Media,
Germany.
He, K., Zhang, X., Ren, S., and Sun, J. (2016). Deep resid-
ual learning for image recognition. In Proceedings of
the IEEE conference on computer vision and pattern
recognition, pages 770–778.
Huang, G., Liu, Z., Van Der Maaten, L., and Weinberger,
K. Q. (2017). Densely connected convolutional net-
works. In Proceedings of the IEEE conference on
computer vision and pattern recognition, pages 4700–
4708.
Huynh, B. Q., Li, H., and Giger, M. L. (2016). Digital mam-
mographic tumor classification using transfer learning
from deep convolutional neural networks. Journal of
Medical Imaging, 3(3):034501.
Janowczyk, A. and Madabhushi, A. (2016). Deep learn-
ing for digital pathology image analysis: A compre-
hensive tutorial with selected use cases. Journal of
pathology informatics, 7.
Jones, E., Oliphant, T., Peterson, P., et al. (2001). SciPy:
Open source scientific tools for Python.
Kensert, A., Harrison, P. J., and Spjuth, O. (2018). Trans-
fer learning with deep convolutional neural networks
for classifying cellular morphological changes. SLAS
DISCOVERY: Advancing Life Sciences R&D, page
2472555218818756.
Khosravi, P., Kazemi, E., Imielinski, M., Elemento, O., and
Hajirasouliha, I. (2018). Deep convolutional neural
networks enable discrimination of heterogeneous dig-
ital pathology images. EBioMedicine, 27:317–328.
Kieffer, B., Babaie, M., Kalra, S., and Tizhoosh,
H. R. (2017). Convolutional neural networks for
histopathology image classification: Training vs. us-
ing pre-trained networks. In 2017 Seventh Interna-
tional Conference on Image Processing Theory, Tools
and Applications (IPTA), pages 1–6. IEEE.
Kingma, D. P. and Ba, J. (2014). Adam: A
method for stochastic optimization. arXiv preprint
arXiv:1412.6980.
Krizhevsky, A. and Hinton, G. (2009). Learning multiple
layers of features from tiny images. Technical report,
Citeseer.
Krizhevsky, A., Sutskever, I., and Hinton, G. E. (2012). Im-
agenet classification with deep convolutional neural
Data Fusion of Histological and Immunohistochemical Image Data for Breast Cancer Diagnostics using Transfer Learning
505

networks. In Advances in neural information process-
ing systems, pages 1097–1105.
Litjens, G., Kooi, T., Bejnordi, B. E., Setio, A. A. A.,
Ciompi, F., Ghafoorian, M., Van Der Laak, J. A.,
Van Ginneken, B., and S
´
anchez, C. I. (2017). A survey
on deep learning in medical image analysis. Medical
image analysis, 42:60–88.
Liu, W., Wang, Z., Liu, X., Zeng, N., Liu, Y., and Alsaadi,
F. E. (2017). A survey of deep neural network ar-
chitectures and their applications. Neurocomputing,
234:11–26.
Mormont, R., Geurts, P., and Mar
´
ee, R. (2018). Com-
parison of deep transfer learning strategies for digital
pathology. In Proceedings of the IEEE Conference on
Computer Vision and Pattern Recognition Workshops,
pages 2262–2271.
Oliphant, T. (2006). NumPy: A guide to NumPy. USA:
Trelgol Publishing.
Pan, S. J. and Yang, Q. (2010). A survey on transfer learn-
ing. IEEE Transactions on knowledge and data engi-
neering, 22(10):1345–1359.
Pedregosa, F., Varoquaux, G., Gramfort, A., Michel, V.,
Thirion, B., Grisel, O., Blondel, M., Prettenhofer,
P., Weiss, R., Dubourg, V., Vanderplas, J., Passos,
A., Cournapeau, D., Brucher, M., Perrot, M., and
Duchesnay, E. (2011). Scikit-learn: Machine learning
in Python. Journal of Machine Learning Research,
12:2825–2830.
Perou, C. M., Sørlie, T., Eisen, M. B., Van De Rijn, M.,
Jeffrey, S. S., Rees, C. A., Pollack, J. R., Ross,
D. T., Johnsen, H., Akslen, L. A., et al. (2000).
Molecular portraits of human breast tumours. nature,
406(6797):747–752.
Pham, N.-A., Morrison, A., Schwock, J., Aviel-Ronen, S.,
Iakovlev, V., Tsao, M.-S., Ho, J., and Hedley, D. W.
(2007). Quantitative image analysis of immunohisto-
chemical stains using a cmyk color model. Diagnostic
pathology, 2(1):1–10.
Ravishankar, H., Sudhakar, P., Venkataramani, R., Thiru-
venkadam, S., Annangi, P., Babu, N., and Vaidya, V.
(2016). Understanding the mechanisms of deep trans-
fer learning for medical images. In Deep Learning
and Data Labeling for Medical Applications, pages
188–196. Springer.
Ribeiro, E., Uhl, A., Wimmer, G., and H
¨
afner, M. (2016).
Exploring deep learning and transfer learning for
colonic polyp classification. Computational and
mathematical methods in medicine, 2016.
Russakovsky, O., Deng, J., Su, H., Krause, J., Satheesh, S.,
Ma, S., Huang, Z., Karpathy, A., Khosla, A., Bern-
stein, M., et al. (2015). Imagenet large scale visual
recognition challenge. International journal of com-
puter vision, 115(3):211–252.
Sheikhzadeh, F., Ward, R. K., van Niekerk, D., and Guil-
laud, M. (2018). Automatic labeling of molec-
ular biomarkers of immunohistochemistry images
using fully convolutional networks. PloS one,
13(1):e0190783.
Shin, H.-C., Roth, H. R., Gao, M., Lu, L., Xu, Z., Nogues,
I., Yao, J., Mollura, D., and Summers, R. M. (2016).
Deep convolutional neural networks for computer-
aided detection: Cnn architectures, dataset charac-
teristics and transfer learning. IEEE transactions on
medical imaging, 35(5):1285–1298.
Simonyan, K. and Zisserman, A. (2014). Very deep con-
volutional networks for large-scale image recognition.
arXiv preprint arXiv:1409.1556.
Sørlie, T., Perou, C. M., Tibshirani, R., Aas, T., Geisler, S.,
Johnsen, H., Hastie, T., Eisen, M. B., Van De Rijn,
M., Jeffrey, S. S., et al. (2001). Gene expression
patterns of breast carcinomas distinguish tumor sub-
classes with clinical implications. Proceedings of the
National Academy of Sciences, 98(19):10869–10874.
Szegedy, C., Liu, W., Jia, Y., Sermanet, P., Reed, S.,
Anguelov, D., Erhan, D., Vanhoucke, V., and Rabi-
novich, A. (2015). Going deeper with convolutions.
In Proceedings of the IEEE conference on computer
vision and pattern recognition, pages 1–9.
Szegedy, C., Vanhoucke, V., Ioffe, S., Shlens, J., and Wo-
jna, Z. (2016). Rethinking the inception architecture
for computer vision. In Proceedings of the IEEE con-
ference on computer vision and pattern recognition,
pages 2818–2826.
Tajbakhsh, N., Shin, J. Y., Gurudu, S. R., Hurst, R. T.,
Kendall, C. B., Gotway, M. B., and Liang, J. (2016).
Convolutional neural networks for medical image
analysis: Full training or fine tuning? IEEE trans-
actions on medical imaging, 35(5):1299–1312.
Torrey, L. and Shavlik, J. (2010). Transfer learning. In
Handbook of research on machine learning appli-
cations and trends: algorithms, methods, and tech-
niques, pages 242–264. IGI Global.
Van Ginneken, B., Setio, A. A., Jacobs, C., and Ciompi,
F. (2015). Off-the-shelf convolutional neural network
features for pulmonary nodule detection in computed
tomography scans. In 2015 IEEE 12th International
symposium on biomedical imaging (ISBI), pages 286–
289. IEEE.
Venables, W. N. and Ripley, B. D. (2013). Modern applied
statistics with S-PLUS. Springer Science & Business
Media.
Veta, M., Pluim, J. P., Van Diest, P. J., and Viergever, M. A.
(2014). Breast cancer histopathology image analysis:
A review. IEEE Transactions on Biomedical Engi-
neering, 61(5):1400–1411.
Wang, D., Khosla, A., Gargeya, R., Irshad, H., and Beck,
A. H. (2016). Deep learning for identifying metastatic
breast cancer. arXiv preprint arXiv:1606.05718.
Webster, L., Bilous, A., Willis, L., Byth, K., Burgemeister,
F., Salisbury, E., Clarke, C., and Balleine, R. (2005).
Histopathologic indicators of breast cancer biology:
insights from population mammographic screening.
British journal of cancer, 92(8):1366–1371.
Yosinski, J., Clune, J., Bengio, Y., and Lipson, H. (2014).
How transferable are features in deep neural net-
works? In Advances in neural information processing
systems, pages 3320–3328.
ICPRAM 2021 - 10th International Conference on Pattern Recognition Applications and Methods
506
