
Predictive Clustering Learning Algorithms
for Stroke Patients Discharge Planning
Luigi Lella
1,*
, Luana Gentile
2,†
, Christian Pristipino
3,‡
and Danilo Toni
4,§
1
ASUR Marche, via Oberdan n.2, Ancona, Italy
2
Dept. of Human Neurosciences, Sapienza University, Rome, Italy
3
San Filippo Neri Hospital, ASL1 Roma, Rome, Italy
4
Dept. of Human Neurosciences, Sapienza University, Rome, Italy
Keywords: Pattern Recognition and Machine Learning, Big Data in Healthcare, Data Mining and Data Analysis,
Decision Support Systems.
Abstract: Stroke patients discharge planning is a complex task that could be carried out by the use of a suitable
decision support system. Such a platform should be based on unsupervised machine learning algorithms to
reach the best results. More specifically, in this kind of prediction task clustering learning algorithms seem
to perform better than the other unsupervised models. These algorithms are able to independently subdivide
the treated clinical cases into groups, and they can serve to discover interesting correlations among the
clinical variables taken into account and to improve the prediction accuracy of the treatment outcome. This
work aims to compare the prediction accuracy of a particular clustering learning algorithm, the Growing
Neural Gas, with the prediction accuracy of other supervised and unsupervised algorithms used in stroke
patients discharge planning. This machine learning model is also able to accurately identify the input space
topology. In other words it is characterized by the ability to independently select a subset of attributes to be
taken into consideration in order to correctly perform any predictive task.
* www.linkedin.com/in/luigi-lella
† https://www.neuroscienze.uniroma1.it/
‡ https://www.aslroma1.it/presidi-ospedalieri/presidio-ospedaliero-san-filippo-neri
§ https://www.neuroscienze.uniroma1.it/
1 INTRODUCTION
According to the Italian Ministry of Health website,
approximately 196,000 strokes occur every year in
Italy, of which 20% are relapses. As defined by the
World Health Organization, stroke is a "neurological
deficit of cerebrovascular cause that persists beyond
24 hours or is interrupted by death within 24 hours"
(Italian Ministry of Health website, 2020).
Stroke is caused by an interruption of
oxygenated blood supply due to an occlusion or a
rupture of the arteries supplying the brain. As a
result, brain functions controlled from that area
(limb movement, language, vision, hearing or other)
are partially or totally impaired or lost (Donnan et
al., 2008). About 10-20% of people with stroke die
within a month and another 10% within the first year
after the event. Only 25% of stroke survivors
recover completely, 75% survive with some form of
disability, and half of these suffer from a deficit so
severe that they lose self-sufficiency.
Major risk factors include age, high blood
pressure, tobacco smoking, obesity, high blood
cholesterol, diabetes mellitus, a previous TIA or
stroke, and atrial fibrillation. Diagnosis is performed
by a physical examination and it is supported by
neuroimages (CT and/or MR).
During hospitalization, different pharmacological
and/or interventional treatments are put in place to
preserve vital functions and minimize brain damage.
The National Institutes of Health Stroke Scale
(NIHSS) is used to assess stroke severity (Putra
Pratama et al., 2019; Lyden et al., 2009).
In the discharge phase, it is important to make a
proper plan, not only to enhance individual recovery,
but also to reduce the high social burden and the use
of health system resources (Mess et al., 2016)
296
Lella, L., Gentile, L., Pristipino, C. and Toni, D.
Predictive Clustering Learning Algorithms for Stroke Patients Discharge Planning.
DOI: 10.5220/0010187502960303
In Proceedings of the 14th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2021) - Volume 5: HEALTHINF, pages 296-303
ISBN: 978-989-758-490-9
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

(Pereira et al.,2014). To help in planning, functional
outcome after stroke is evaluated using the modified
Rankin Scale (mRS) which measures the degree of
disability or dependence in activities of daily living.
The lower the score the higher the likelihood of
being able to live at home with a degree of
independence after being discharged from the
hospital or a long-term care ward (Saver et
al.,2010)(Wilson et al.,2002).
Aim of this paper is to present an innovative and
effective prediction model for discharge planning,
based on a machine learning algorithm derived from
data gathered during hospitalisation in the acute
phase.
2 PREVIOUS WORK
A considerable body of literature exists on the use of
machine learning algorithms based on the
assimilation of the data of previously treated clinical
cases. The accuracy of prediction generally tends to
increase over time, as new data become available
(Bishop, 2006). However, there is no algorithm
capable of providing the best predictive accuracy for
each category of problem (Alpaydin, 2020).
Machine learning algorithms can be subdivided
into supervised and unsupervised. In the supervised
learning human experts select the correct answers of
the machine learning model, while unsupervised
learning does not need the intervention of human
experts (Alpaydin, 2020).
Within the unsupervised learning paradigm, it is
possible to operate a further subdivision between
symbolic models that seek to reach a formal
representation of knowledge (using for example
logical representations, inference rules or decision
trees) and sub-symbolic models where the acquired
knowledge is stored in complex representations such
as artificial neural networks. Clustering learning
algorithms (Van Hulle, 1989; Kohonen, 1988;
Kohonen, 1989; Kohonen, 1990) are subsymbolic
unsupervised models that allow to achieve the best
results in an unsupervised manner. If a class attribute
is chosen, such as the length of the hospital stay or
the outcome expressed using a suitable evaluation
scale, these algorithms are able to divide the clinical
cases that can occur in clusters, corresponding to
hospitalizations that end with the same length of
hospital stay or with the same outcome. Even if
these models are not classifiers, after being trained
with a set of clinical cases used as test sets, they are
able to assign a test set record to a correct class,
achieving a considerable high prediction accuracy
when new treated cases are processed. Among the
learning cluster algorithms, Kohonen's Self
Organizing Maps (Kohonen, 1989) have been
widely used in the health sector, but better results
can be achieved by using a more adaptive algorithm
such as Fritzke's Growing Neural Gas (GNG)
(Fritzke,1994). GNG is an incremental network
model based on a simple Hebb-like learning rule.
Unlike previous approaches like the “neural gas”
method of Martinetz and Shulten (Martinetz and
Shulten, 1991) (Martinetz and Shulten,1994) this
model has fixed parameters and it is able to continue
the learning phase, adding other neural units and
connections, until a performance goal is achieved.
By being able to accurately identify the input space
topology, this model is able to identify the variables
to be considered in order to effectively operate the
prediction of a class attribute.
For example, if the mRS is chosen as class
attribute (that is the study variable to be predicted),
the GNG model could predict that a male individual
aged between 40 and 65, with a particular form of
diagnosed stroke and treated with certain
pharmacological therapies, at the end of the hospital
stay, is able to reach a mRS score of 1. This
prediction could be made without taking into
consideration other variables such as risk factors,
results of instrumental and laboratory tests etc. In
other cases the same model could need a greater
number of variables in order to make an accurate
prediction.
The GNG model has already been successfully
used in similar areas, such as in the prediction of the
length of hospital stay (Lella and Licata, 2017)
Functional outcome after stroke is related to
many variables, from biometric data (gender, age,
weight, pressure levels) to risk profiles, from the
results of laboratory tests to the results of
instrumental tests to therapies.
Given this complex interaction of many
variables, using machine learning appears to be the
best solution choosing an unsupervised model that
can improve its predictive accuracy over time. The
purpose of these algorithms is to identify over the
course of time new possible and clinically
meaningful correlations among the available data.
This approach has proved particularly effective
in the clinical setting, especially to predict the
therapeutic outcome of stroke patients (Zdrodowska,
2019; Zdrodowska et al., 2018; Chen et al., 2017)
(Alaiz-Moreton, 2018). The best results were
obtained through the use of the Random Forest
algorithm (Breiman, 2001; Alaiz-Moreton, 2018)
(Tin Kam Ho, 1998; Tin Kam Ho, 1995), an
Predictive Clustering Learning Algorithms for Stroke Patients Discharge Planning
297

ensemble learning method for classification obtained
through the aggregation of decision trees, and the
PART model, a partial decision tree algorithm that
does not need to perform global optimization like
other rule based learners (Zdrodowska et al., 2018;
Ali and Smith, 2006). Excellent results were also
obtained by using supervised models such as the
Support Vector Machine (SVM) (Zdrodowska et al.,
2018), a model based on a binary non-probabilistic
linear classifier (Ben Hur et al.,2001) (Cortes and
Vapnik, 1995).
3 METHODOLOGY
On the basis of the above literature review, it was
decided to use GNG networks to predict the status
of stroke patients one day and seven days after
entering the hospital, as well as at hospital discharge
and after three months, comparing the results with
the ones achieved by the best models used in this
kind of study, i.e. the Random Forest model, the
PART model and the SVM model.
The ZeroR model (Witten et al., 2011), the
OneR (Holte, 1993), the Naive Bayes (John and
Langley, 1995) and the J48 (Witten et al., 2011)
were also taken into consideration.
The ZeroR model is used as a benchmark to
verify that all the other tested algorithms have been
configured and used correctly. ZeroR always
predicts the most frequent class variable in the
presence of any combination of input variables.
Given its simplicity, it has generally a much lower
level of prediction accuracy than the other
algorithms. If this does not occur, the found result
may be due to a bad data selection and coding, or to
a bad configuration of the models.
The OneR, which stands for "one Rule", is a
one-level decision tree. In various areas and
predictive tasks, this model has proved to be much
more efficient than other more complex models, and
it is always advisable to check whether the problem
in question can be effectively treated using this
model which requires a reduced amount of
resources.
The Naive Bayes is a simple probabilistic
classifier based on applying Bayes' theorem with
strong (naive) independence assumptions between
the features.
The J48 is a decision tree based on the "divide
and conquer" strategy used recursively. At each
training step, the node characterized by the highest
amount of information is selected and split into a
series of nodes corresponding to some possible
values that the original node can assume. The
process ends when all the considered instances refer
to the same class attribute value.
The study involved a subset of 20,000 samples
taken from the Italian subset of the SITS registry
(Safe Implementation of Treatments in Stroke
website, 2020), a non-profit, research- driven,
independent and international monitoring initiative
for stroke patients.
Of these, just the data that hold the fields of the
outcome 24 hours after the patient's access to the
hospital (Global Outcome 24), the mRS at 7 days
(Rankin at 7 days), the mRS at hospital discharge
(Rankin at hospital discharge) and the mRS at 3
months (Rankin at 3 months) were taken into
consideration. These three variables were chosen as
class attributes for the tests.
The first class attribute is a qualitative clinical
variable that can take 7 possible values
("muchBetter", "better", "unchanged", "worse",
"muchWorse", "dead"). The other three class
variables can only take the scores 0,1,2,3,4,5 and 6.
The first subgroup of records, with the global
outcome at 24 hours specified, consisted of 13008
records characterized by 69 non class attributes; the
second subgroup, with the mRS at 7 days specified,
was made by 10460 records characterized by 99 non
class attributes; the third subgroup, with the mRS at
hospital discharge specified, was constituted by
4989 records characterized by 129 non class
attributes; the fourth subgroup, with the mRS at 3
months specified, was made by 10777 records
characterized by 152 non class attributes. The
reason why the number of non-class attributes is
different in the four subsets is that an higher length
of hospitalization also increases the number of
available data deriving from further tests performed.
Therefore, the number of non-class variables that
can be considered increases.
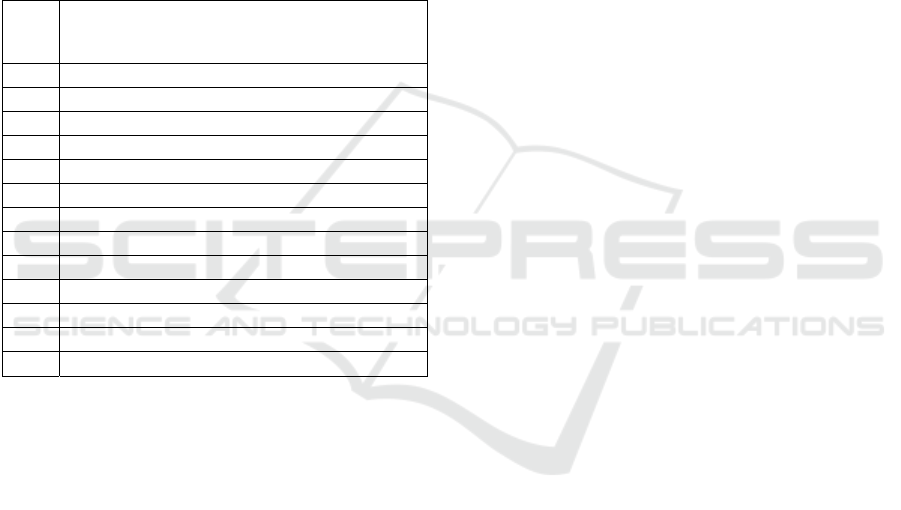
The characteristics of the four subsets of records
are presented in table 1.
Table 1: Features of the considered data sets.
Data set Total no.(male,female); avg age(min,max);
hemorrhagic stroke; ischemic stroke
1–Global
Outcome 24
13008(6974,6034); 71(14,102); 1902;
11106
2–Rankin at
7 days
10460(5491,4969); 71(14,101); 1376;
9084
3–Rankin at
Hospital
Discharge
4989(2780,2209); 68(14,102); 557; 4432
4- Rankin at
3 months
10777(5685,5092); 71(14,104); 755;
10022
HEALTHINF 2021 - 14th International Conference on Health Informatics
298

Part of the patient data was incomplete, but it
was not necessary to perform any type of data
cleaning due to the data entry performed by a
codified online form.
Data were discretized and normalized before
being processed. All predictive machine learning
models taken into consideration were trained with
60% of the samples and tested with the remaining
40% of the samples. The Weka 3.8.4 platform was
used to test ZeroR, OneR, J48, Naive Bayes, SVM
and Random Forest models, while a Java
implementation was used to test the GNG model.
The sequential minimal optimization algorithm
(Platt, 1998) was used to train the SVM model.
The GNG model was tested with the following
parameters:
λ=100, ε
b
=0.2, ε
n
=0.006, α=0.5, α
max
=50, δ=0.995.
The training was stopped when the mean square
error, i.e. the main of the local square error related to
each unit (expected distortion error), dropped below
the threshold of E=0.7.
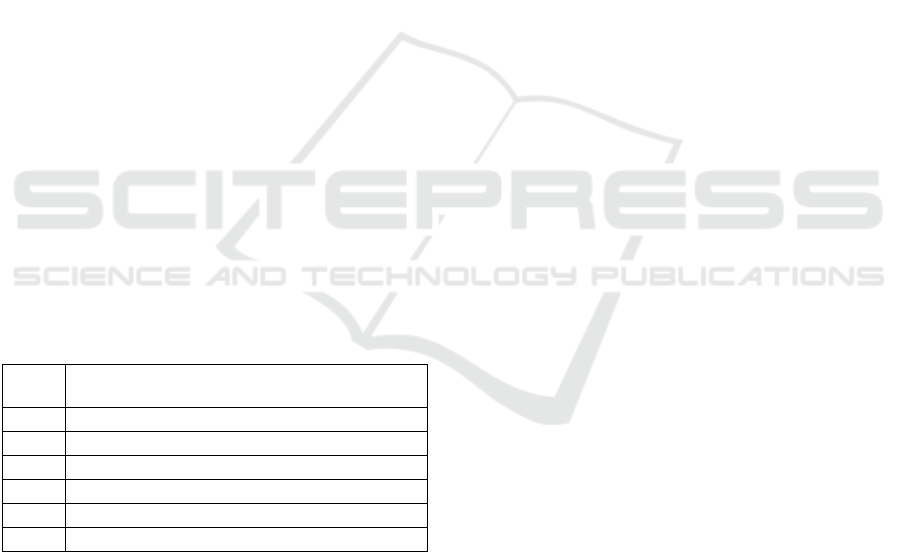
4 RESULTS
The results in terms of prediction accuracy (i.e. the
number of correct predictions over the total number
of predictions) are shown in table 2.
All the tested models reached an higher
prediction accuracy than the ZeroR model, and the
OneR model resulted to be the second worst
algorithm, confirming the complexity of the
prediction task. Naive Bayes, J48, SVM and PART
performed better with a low number of training
records characterized by more non class attributes.
The best results were obtained by the GNG
model and by the Random Forest model, followed
by PART and SVM. The result confirmed the
correctness of the choice of the unsupervised models
over the supervised ones and the chosen clustering
learning model proved to be more performing than
the Random Forest ensemble model.
Once trained, it is also possible to use the GNG
model to identify which non-class attributes are
linked to particular values of the selected class
attribute. For example, it is possible to identify
which clinical variables are linked to the worsening
of patients during the first 24 hours of
hospitalization.
Using the Girvan-Newman algorithm (Girvan
and Newman, 2002) it is possible to identify
communities of nodes starting from the portion of
the trained model of self-organizing neural network
associated with a deterioration of state. In the case of
Table 2: Prediction accuracy of the tested models.
Tested
Models
Prediction Accuracy on data set 1; data
set 2; data set 3; data set 4
ZeroR
30.67; 19.55; 24.05;
27.73
OneR 38.72; 29.96;
37.36;
43.73
Naive
Bayes
29.44; 46.21;
80.36;
56.76
J48
68.9; 71.48;
82.08; 44.88
SVM 41.48; 78.46; 99.19; 82.57
PART 72.26; 76.54; 83.04; 46.89
Random
Forest
97.99; 97.54;
97.25;
84.89
GNG
99.17; 99.64; 99.05; 89.88
the first GlobalOutcome24 subset the selected nodes
are those in which the values of the class attribute
code corresponding to "worse", "muchWorse" and
"dead" exceed a threshold value that has been set
equal to 0.7. Girvan-Newman's algorithm identifies
the communities of nodes by eliminating those
connections characterized by the greatest number of
shorter paths that link each pair of nodes. After
training the first model with the records of the first
subset of input records (GlobalOutcome24) and
selecting the network portion corresponding to the
values of the class attribute "muchWorse" and "dead",
the Girvan-Newman algorithm was used to remove
the first 100 connections characterized by the greatest
number of shorter paths between pairs of nodes.
Table 3: Clinical variables related to death in the first 24
hours of hospitalization.
Cluster
no.
Label (weight)
1
Hypertension(0.99); HighTemperature(0.97)...
2
NIHSS1A=3(1.00); GenderMale(1.00)...
3
NIHSS5A=4(0.99); NIHSS6A=4(0.99)...
4
LowAPTTvalues(1.00); GenderMale(1.00)...
5
NIHSS11=9(1.00); GenderMale(1.00)...
6
GenderMale(1.00);Hypertension(0.96)
7
Hypertension(0.99); NIHSS5B=4(0.98)...
8
Hypertension(0.99); Age>=80(0.96)...
9
Hypertension(0.99); Diabetes(0.95)...
10
Hypertension(0.99); HighTemperature(0.96)...
11
CurrentInfarct(1.00); GenderMale(1.00)...
12
NIHSS5A=4(0.98); Age65-80(0.83)...
13
NIHSS1C=2(0.95); NIHSS6A=4(0.90)...
14
Hyperlipidaemia(1.00);GenderMale(1.00)...
15
NIHSS4=2(1.00); GenderMale(1.00)...
16
PreviousStroke<3months(1.00)...
17
NIHSS8=2(1.00); GenderMale(1.00)...
18
CerebralOedema(1.00); GenderMale(1.00)...
19
NIHSSB=2(0.93); NIHSS1C=2(0.88)...
20
NIHSS7=4(1.00); GenderMale(1.00)...
Predictive Clustering Learning Algorithms for Stroke Patients Discharge Planning
299
Subsequently, the non-class attributes associated
with the nodes of the individual communities were
extracted, that is, those characterized by
corresponding code values higher than the threshold
value of 0.7.
For each node, using a weight function tf-idf
(Baeza, 1999), the attribute most frequent in its own
community and less frequent in the overall set of
extracted communities was chosen. In this way, all
the non-class attributes associated with the
worsening of the clinical picture were identified.
The results of this processing are shown in table 3
and table 4.
Table 4: Clinical variables related to the worsening in the
first 24 hours of hospitalization.
Clus
ter
no.
Label (weight)
1
NIHSS1B=2(1.00); Hypertension(1,00)...
2
Hypertension(1.00); NIHSS5A=4(0.88)...
3
Hypertension(0.97); NIHSS5B=4(0.87)...
4
Hypertension(0.92); NIHSS4=2(0.88)...
5
NIHSS1B=2(1.00); Hypertension(0.94)...
6
Hypertension(0.97); GenderFemale(0.96)...
7
Age65-80(0.98); NIHSS3=2(0.98)...
8
NIHSS5B=4(0.99); NIHSS4=2(0.99)...
9
Hypertension(1,00); LowAPTTvalues(0.93)...
10
NIHSS4=2(0.99); NIHSS11=2(0.88)...
11
Hypertension(0.98); CurrentInfarct(0.92)...
12
NIHSS10=1(0.99); Age18-65(0.87)
13
Hypertension(0.86); GenderMale(0.81); ...
For each cluster of nodes extracted by the use of
Girvan-Newman's algorithm, the non-class attributes
associated to the corresponding nodes are listed. Due
to the GNG model training method, it is reasonable
to assume that each identified cluster is related to a
subset of analysed clinical cases.
The clinical variables associated with the various
clusters which are related to cases of serious
worsening and death patient are displayed in the
results tables 3 and 4. In the first lines the most
important clusters are represented, i.e. those
associated with a greater number of neural units and
therefore with a greater number of clinical cases.
For each cluster the non-class attributes, i.e. the
clinical variables responsible for the worsening or
the death of the patient, are sorted in descending
order by weight associated with the attribute. The
weight is a coefficient between 0 and 1 which
indicates how much the neuronal units associated
with the selected cluster are activated when the
attribute is present in the considered clinical case.
Values close to 0 mean that the attribute is not very
relevant for the worsening or death of the patient,
those close to 1 are instead considered the main
responsible factors.
The obtained results show that the presence of
hypertension, assessed on the basis of the systolic
and diastolic blood pressure values, is considered an
important potential factor for the worsening the
patient's state which can also lead to death. The
presence of hypertension alone, however, is not
sufficient to infer the risk of worsening or death.
Considering for example the first cluster of table 3
related to the death cases, hypertension is an
important factor having a weight equal to 0.99, but it
must also be accompanied by other factors such as
hightemperature, hyperlipidaemia, genderfemale,
NIHSS4 = 2 and age65-80.
Using the tf-idf algorithm, the most
representative clinical variables of the considered
cluster were selected. These are represented in bold
and they allow to highlight which are the attributes
most related to the worsening or death of the patient.
For example, the attributes of table 3 most
related to death cases with the relative weights are
PreviousStroke<3months (1.00), Hyperlipidaemia
(1.00), LowAPTTvalues(1.00), CerebralOedema
(1.00), GenderMale (1.00), NIHSS8 = 2 (1.00),
NIHSS4 = 2 (1.00), NIHSS1A = 3 (1.00), NIHSS7 =
4 (1.00), Hypertension (0.99), NIHSS5A = 4 (0.99),
NIHSS5B = 4 (0.98), HighTemperature (0.96),
Age> = 80 (0.96), Diabetes (0.95), NIHSS6A = 4
(0.90), NIHSS1C = 2 (0.88), Age65-80 (0.83). This
means that the presence of a previous stroke that
occurred no more than three months before,
accompanied by hyperlipidaemia or a cerebral
oedema or a low level of APTT, especially if the
patient is male can be considered a quite worrying
clinical picture. An age greater than 80 is to be
considered a more important risk factor than an age
between 65 and 80.
The clinical variables of table 4 related to the
severe worsening of the patient with the relative
weights are NIHSS1B = 2 (1.00), NIHSS5B = 4
(0.99), NIHSS10 = 1 (0.99), Age65-80 (0.98),
GenderFemale (0.96), Hypertension (0.94),
LowAPTTvalues(0.93), NIHSS11 = 2 (0.88),
NIHSS4 = 2 (0.88), NIHSS5A = 4 (0.88), NIHSS5B
= 4 (0.87), GenderMale (0.81). This means that the
presence of a low sense of orientation, of plegia or
dysarthria especially if the patient is aged between
65 and 80 and hypertensive is to be considered a
potential worsening factor. Female patients are
considered more at risk of serious worsening than
male patients.
HEALTHINF 2021 - 14th International Conference on Health Informatics
300
A similar study was carried out to identify the
clinical variables most correlated with a serious level
of disability after 3 months (corresponding at a mRS
of 3, 4 or 5). The results are shown in table 5.
As it can be seen, high blood pressure levels are
always related to the appearance of a disabling
stroke. The mRS at three months is also strongly
affected by the patient's state 7 days after
hospitalization. Generally there are only slight
differences in outcomes between male and female
patients, although clusters 1, 4 and 6 show a greater
correlation with the male sex while clusters 3 and 5
are more correlated with the female sex.
The first cluster is represented by patients aged
between 65 and 80 characterized by the presence of
occlusions that lead to the appearance of an
ischaemic penumbra (perfusion infarct mismatch).
The second cluster is represented by underweight
patients over the age of 65 characterized by diabetes
and hyperlipidaemia and occlusions and a
hyperdensity of the arteries. The third cluster relates
to underweight patients characterized by a mRS of 4
both after the first 7 days and upon discharge from
the hospital. Such patients are characterized by low
APTT levels. The fourth cluster is made up of
patients aged between 18 and 65, with high blood
cholesterol levels, diabetes and occlusions. The fifth
cluster is represented by patients over eighty
characterized by hyperlipidaemia and low levels of
APTT. The sixth cluster is associated with pre-
diabetic patients aged between 65 and 80 years.
Table 5: Clinical variables related to the worsening in the
first 24 hours of hospitalization.
Cluster
no.
Label (weight)
1
mRS_4_dis(0,90); mRS_3_7d(0,99); ...
2
LowApttValues(0,96); Hypertension(1,00); ...
3
Age65-80(0,85); Hypertension(0,97); ...
4
GenderMale(0,91); Hypertension(0,99); ...
5
Age>=80(0,92); GenderFemale(0,97); ...
6
Prediabetes(0,83); Hypertension(0,97); ...
The age range most at risk of incurring
permanent disabilities at 3 months after treatment is
consistent with the fact that in this cohort 78% of
patients with a 3-month mRS equal to 3, 4 or 5 are
over 65-year-olds.
Analysing the subset of patients with a 3-month
mRS of 3, 4 or 5 aged between 65 and 80, in 72% of
these cases a significant ischaemic penumbra is
detected (perfusion infarct mismatch) and in 44% of
cases also an hyperdense artery sign. This subset of
patients is clearly identifiable with cluster 1.
Considering instead the subset of patients with a
3-month mRS of 3, 4 or 5 aged between 65 and 80
characterized by low APTT levels, in 85% of cases
there are also high serum glucose levels. This subset
of cases can be associated with clusters 2 and 3.
Analysing the subset of patients with a 3-month
mRS equal to 3, 4 or 5 aged between 18 and 65
years it is found that in this case 67% of the patients
are male, 81% have low APTT levels and 80% had
high serum glucose levels. This subset of patients is
clearly identifiable with cluster 4.
The 87% of the subset of patients with a 3-month
mRS equal to 3, 4 or 5 over the age of 80 with
hyperlipidaemia are patients with low APTT levels.
This group can be associated with cluster 5.
5 CONCLUSIONS
The findings of this study suggest that the use of
clustering learning algorithms allows to identify in
an unsupervised way a set of clinical variables
which can be taken into consideration in order to
carry out a good prediction of the clinical outcome.
The Growing Neural Gas model has proved
particularly effective in predicting the patient
outcome compared to other algorithms used in the
same application area. The best result in terms of
predictive accuracy achieved by this model is due to
its ability to exactly identify the input space
topology, which also makes it particularly robust to
noise and lack of data. By analyzing the final
configuration of the trained GNG network, it is also
possible to obtain useful information on the
attributes which are most correlated with certain
outcomes. Statistical analyses carried out on the data
used as training set and test set seem to confirm the
consistency of the extracted knowledge. The
developed model is ready to be tested in prospective
studies in the real world.
REFERENCES
Alaiz-Moreton, H., Fernandez-Roblez L., Alfonso
Cendon, J., Castejon-Limas, M., Sanchez-Gonzalez L.,
Perez H., 2018. Data mining techniques for the
estimation of variables in health-related noisy data.
Advances in intelligent systems and computing, 649,
482-491.
Ali S., Smith K.A., 2006. On learning algorithm selection
for classification. Applied Soft Computing, 6, 119-
138.
Alpaydin E., 2020. Introduction to Machine Learning. 4
th
Predictive Clustering Learning Algorithms for Stroke Patients Discharge Planning
301

Edition. MIT Press.
Baeza Y., 1999. Modern Information Retrieval. Addison-
Wesley Longman Publishing Co., ISBN 0-201-39829-
X.
Ben-Hur, A., Horn, D., Siegelmann, H.T., Vapnik, V.N.,
2001. Support vector clustering. Journal of Machine
Learning Research. 2, 125–137.
Bishop, C. M., 2006. Pattern Recognition and Machine
Learning, Springer.
Breiman L., 2001. Random Forests. Machine Learning.
45(1), 5–32. doi:10.1023/A:1010933404324.
Chen Y.C., Suzuki T., Suzuki M., Takao H., Murayama
Y., Ohwada H., 2017. Building a classifier of onset
stroke prediction using random tree algorithm.
International Journal of Machine Learning and
Computing, 7(4), 61-66.
Cortes, C., Vapnik, V.N., 1995. Support-vector networks.
Machine Learning. 20(3), 273–297.
CiteSeerX10.1.1.15.9362. doi:10.1007/BF00994018.
Donnan, G.A., Fisher M., Macleod M., Davis S.M., 2008.
Stroke. The Lancet. 371(9624), 1612–23.
Fritzke B., 1994. A Growing Neural Gas Network Learns
Topologies. Part of: Advances in Neural Information
Processing Systems 7, NIPS.
Girvan M., Newman M.E.J., 2002. Community structure
in social and biological networks, Proc. Natl. Acad.
Sci. USA 99, 7821–7826.
Holte,R.C., 1993. Very simple classification rules perform
well on most commonly used datasets. Machine
Learning.
Italian Ministry of Health website, 2020. http://www.
salute.gov.it/portale/salute/p1_5.jsp? lingua=italiano&
id=28&area=Malattie_cardiovascolari, last accessed
2020/04/24.
John, G.H.; Langley, P., 1995. Estimating Continuous
Distributions in Bayesian Classifiers. Proc. Eleventh
Conf. on Uncertainty in Artificial Intelligence. Morgan
Kaufmann. 338–345. arXiv:1302.4964
Kohonen T., 1988. An introduction to neural computing.
Neural Networks, 1, 3-16.
Kohonen T., 1989. Self-Organization and Associative
Memory, Berlin: Springer-Verlag.
Kohonen T., 1990. The Self Organizing Map. Proc of the
IEEE, 78(9).
Lella L., Licata I., 2017. Prediction of Length of Hospital
Stay using a Growing Neural Gas Model. In
Proceedings of the 8th International Multi-Conference
on Complexity, Informatics and Cybernetics (IMCIC
2017), 175-178.
Lyden P., Raman R., Liu L., Emr M., Warren M., Marler
J., 2009. National Institutes of Health Stroke scale
certification is reliable across multiple venues. Stroke,
40(7), 2507-2511. doi:10.1161/STROKEAHA.116.
015434.
Martinetz, T. M., Schulten, K J., 1991. A "neural-gas"
network learns topologies. In Kohonen, T., Makisara,
K, Simula, 0., and Kangas, J., editors, Artificial Neural
Networks, North-Holland, Amsterdam, 397-402.
Martinetz, T. M., Schulten, K J., 1994. Topology
representing networks. Neural Networks, 7(3), 507-
522.
Mess M., Klein J., Yperzeele L., Vanacker P., Cras P.,
2016. Predicting discharge destination after stroke: A
systematic review. Clin Neurol Neurosurg. 142(15-
21). doi:10.1016/j.clineuro.2016.01.004.
Pereira S., Foley N., Salter K., McClure J.A., Meyer M.,
Brown J., Speechley M., Teasell R., 2014. Discharge
destination of individuals with severe stroke
undergoing rehabilitation: a predictive model. Disabil
Rehabil. 36(9), 727-731. doi:10.3109/09638288.
2014.902510.
Platt,J., 1998. Sequential Minimal Optimization: A Fast
Algorithm for Training Support Vector Machines.
Technical Report MSR-TR-98-14.
Putra Pratama A., Tresno T., Wahyu Purwanza S., 2019.
Development the national institutes of health stroke
scale (NIHSS) for predicting disability and functional
outcome to support discharge planning after ischemic
stroke. Journal Ners, 14(3).
Saver J.L., Filip B., Hamilton S., Yanes A., Craig S., Cho
M., Conwit R., Starkman S., FAST-MAG
Investigators and Coordinators, 2010. Improving the
reliability of stroke disability grading in clinical trials
and clinical practice: the Rankin Focused Assessment
(RFA). Stroke. 41 (5): 992–
doi:10.1161/STROKEAHA.109.571364. PMC
2930146. PMID 20360551
Safe Implementation of Treatments in Stroke website,
2020. https://sitsinternational.org, last accessed
2020/04/24.
Tin Kam Ho, 1998. The Random Subspace Method for
Constructing Decision Forests. In IEEE Transactions
on Pattern Analysis and Machine Intelligence, 20(8),
832–844, DOI:10.1109/34.709601.
Tin Kam Ho, 1995. Random Decision Forests.
Proceedings of the 3rd International Conference on
Document Analysis and Recognition, Montreal, QC,
278–282.
Van Hulle M. M., 1989. Self Organizing Maps. Handbook
of Natural Computing, 585-622.
Wilson J. L., Hareendran A., Grant M., Baird T., Schulz
U.G., Muir K.W., Bone I., 2002. Improving the
Assessment of Outcomes in Stroke: Use of a
Structured Interview to Assign Grades on the Modified
Rankin Scale. Stroke. 33 (9): 2243–2246.
doi:10.1161/01.STR.0000027437.22450.BD. PMID
12215594
Witten,I. H., Frank,E., Hall,M.A., 2011. Data Mining
Practical Machine Learning Tools and Techniques.
Morgan Kaufmann Publishers.
Zdrodowska M., 2019. Attribute selection for stroke
prediction. Sciendo. Doi 10.2478/ama-2019-0026.
Zdrodowska M., Dardzinska M, Chorazy M., Kulakowska
A., 2018. Data Mining Techniques as a tool in
neurological disorders diagnosis. Acta Mechanica et
Automatica, 12(3), 217-220.
HEALTHINF 2021 - 14th International Conference on Health Informatics
302

APPENDIX
For the input data preprocessing the following coding
rules were used:
The age was codified in four main classes: age>=80;
65<=age<80; 18<=age<65 and 0<=age<18.
The clinical variables “Hypertension” and
“Hyperlipidemia” refer to the risk factors which are
specified in the data entry form. They are not
automatically computed by the use of a codifying
formulas.
If the glucose level is lower than 69 the value is codified
as “Hypoglycemia”, if the glucose level is between 70
and 99 the value is codified as “Normoglycemia”, if
the glucose level is between 100 and 124 the value is
codified as “Prediabetes”, if the glucose level is higher
than 125 the value is codified as “Diabetes”.
If the cholesterol level is lower than 199 the value is
codified as “NormalCholesterol”, if the cholesterol
level is higher than 200 the value is codified as
“HighCholesterol”.
If the temperature level is lower than 98.5 Fahrenheit the
value is codified as “NormalTemperature”, if the
temperature level is higher than 98.6 the value is
codified as “HighTemperature”.
If the APTT is lower than 29 the value is codified as
“LowApttValues”, if the APTT level is between 30
and 39 the value is codified as “NormalApttValues”, if
the APTT level is higher than 40 the value is codified
as “HighApttValues”.
If the BMI is lower than 18.4 the value is codified as
“Underweight”, if the BMI is between 18.5 and 24,9
the value is codified as “Normweight”, if the BMI is
between 25 and 29,9 the value is codified as
“IncreasedOverweight”, if the BMI is between 30 and
34,9 the value is codified as “ModerateOverweight”, if
the BMI is between 35 and 39,9 the value is codified
as “SevereOverweight”, if the BMI is higher than 40
the value is codified as “VerySevereOverweight”.
Predictive Clustering Learning Algorithms for Stroke Patients Discharge Planning
303
