
On the Involvement of Mental Healthcare Professionals in the Co-design
of Highly-rated Anxiety Apps
Nidal Drissi
a
and Sofia Ouhbi
b
Dept. Computer Science & Software Engineering, CIT, U.A.E. University, Al Ain, U.A.E.
Keywords:
m-Health, Requirements Engineering, Mental Health, Anxiety, Cognitive Behavioral Therapy.
Abstract:
Mobile applications (apps) have the potential to assist people with their mental health issues. They have
shown promising results in mitigating many mental health disorders and symptoms, including issues related
to anxiety. Mental health apps are based on different approaches, one of which is cognitive behavioral therapy
(CBT). However, these solutions still face many concerns and challenges, such as the lack of involvement
and inputs of mental healthcare professionals (MHP) in their design and evaluation. This paper focuses on
highly-rated CBT-based apps for anxiety and investigates the involvement of MHP in their co-design. Based
on the obvious importance of inclusion of mental health professionals in the creation of mental care apps, the
following hypothesis was formed: MHP are involved in the design and creation of CBT-based apps for anxiety.
To investigate this hypothesis, 23 apps were selected and analysed. Results showed that contrarily to the initial
hypothesis, about half of the selected CBT-based apps for anxiety did not involve MHP in their design. Results
also showed that the number of installs of the selected apps might be impacted by the involvement of MHP.
The average of installs of apps which involved MHP was significantly higher than the average of installs of
apps that did not. This might indicate that users tend to trust apps that involve MHP more, which might
have impacted their decision to install them. Findings of this study might be of interest to people suffering
from anxiety, to help them find apps for anxiety that are based on MHP input, as well as to developers and
researchers targeting similar apps.
1 INTRODUCTION
Requirements engineering (RE) is critical for the suc-
cess of software projects (Pohl, 2010). There are four
main phases in the requirements development pro-
cess: (1) requirements elicitation, (2) requirements
analysis, (3) requirements specification, and (4) re-
quirements validation (Bourque et al., 2014). The
requirements elicitation phase can be viewed as the
most important step in any software project, includ-
ing the development of mobile applications (apps). It
is the base for all the steps that follow in the creation
process (Stephens, 2015). In this phase, the require-
ments engineer or the software engineer works to col-
lect the needs of different stakeholders that have inter-
est in the software product. The stakeholders that can
be involved include, among others, the customer, the
user, and the developers. It should be noted that the
customers are not always the users. The customers are
the ones paying for the creation of the software prod-
a
https://orcid.org/0000-0001-9667-5931
b
https://orcid.org/0000-0001-7614-9731
uct, while the users are the ones that will be using
the product. End-users are very important stakehold-
ers that are very often overlooked and not included in
the design process (Costabile et al., 2009). Many de-
sign approaches such as user-centred design stress on
the importance to understand the expectations of end-
users and to capture their needs (Van Leersum et al.,
2020). Several studies have also shown the impor-
tance of including end users in the co-design and co-
creation of the software product, particularly in con-
nected health solutions (Ouhbi et al., 2019; Dey et al.,
2019).
In the case of connected mental health solutions
(Drissi et al., 2020a), RE process is crucial and critical
as it will produce functionalities that are supposed to
help end-users with their mental health issues. Mental
health in general and anxiety in particular should be
approached and treated carefully. Which is why it is
not enough to opt for including only end-users in the
co-design of related apps, as in many cases the end-
users do not know what treatment approaches are suit-
able to assist them with their anxiety. Therefore men-
Drissi, N. and Ouhbi, S.
On the Involvement of Mental Healthcare Professionals in the Co-design of Highly-rated Anxiety Apps.
DOI: 10.5220/0010183102810287
In Proceedings of the 14th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2021) - Volume 5: HEALTHINF, pages 281-287
ISBN: 978-989-758-490-9
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
281

tal health professionals (MHP) should be involved in
the co-design of these apps, especially that the end-
users with anxiety are vulnerable users. Anxiety is
a “psychological and physiological state (mind and
body) associated with feelings of fear, worry, uneasi-
ness, dread, or nervousness” (Cortman et al., 2015).
It can be manged with several treatment approaches
such as cognitive behavioral therapy (CBT) (Loerinc
et al., 2015). CBT is a common type of psychother-
apy, based on helping patients becoming aware of
inaccurate or negative thinking, in order to be able
to deal with challenging situations in a more effec-
tive way (Mayo Clinic Staff, 2020). CBT has been
proven to be effective for anxiety (Norton and Bar-
rera, 2012; Lyneham and Rapee, 2006), and can help
with other issues like depression and sleep disorders
(Mayo Clinic Staff, 2020).
Mobile mental health is one of the most adopted
forms of use of technology for mental care (Drissi
et al., 2020a). The number of mobile mental health
apps is increasingly growing in app repositories (Hol-
lis et al., 2015; Olff, 2015), especially due to the cur-
rent COVID-19 pandemic, which has increased the
interest in digital mental health (Torous and Kesha-
van, 2020). In fact, COVID-19 has resulted in the
surge of several psychological issues, including anx-
iety, in the general population (Salari et al., 2020).
There is a wide range of apps that offer different func-
tionalities targeting anxiety self-treatment and man-
agement, such as breathing exercises, meditation,
yoga, games, and online therapy (Drissi et al., 2020b;
Drissi et al., 2019). The use of apps for mental health
has been reported to be effective for many psycholog-
ical issues, including stress, anxiety, and depression
(Harrison et al., 2011; Loo Gee et al., 2016). But the
majority of the available apps lack evidence on their
efficiency and only few have been thoroughly tested
(Larsen et al., 2019; Anthes, 2016). Involvement of
MHP in the co-design, testing and evaluation of such
apps, might help overcome those problems, as well as
help insuring users’ trust, and improving clinical out-
comes (Hollis et al., 2015).
This paper investigates the involvement of MHP
in the co-design of anxiety apps. To do so, 23 highly-
rated CBT-based apps for anxiety were selected and
analyzed. Highly-rated apps are considered to pro-
vide a certain level of satisfaction to end users. Users’
satisfaction is related to the quality of the app, partic-
ularly to its usability. For this reason, we included
only highly-rated apps. To the best of our knowledge,
there are no similar studies that address the involve-
ment of MHP in the co-design of mental care apps.
Since the involvement of MHP in mobile mental care
apps is important on many levels, our hypothesis is as
follows: CBT-based mental care apps for anxiety do
include MHP in their co-design.
2 METHODOLOGY
This study mainly focuses on answering this research
question (RQ): Do CBT-based apps for anxiety in-
volve MHP in their design?
This section presents the methodology followed to
answer the RQ and select the apps to be analysed in
this paper. The search conducted in this study fol-
lowed the guidelines of the Preferred Reporting Items
for Systematic reviews and Meta-Analysis (PRISMA)
group (Liberati et al., 2009).
2.1 Sources and Eligibility Criteria
A general search string composed with only the term
“Anxiety” was used, and it was automatically applied
to the names and descriptions of the apps. Each app
identified from the search result was analyzed to de-
termine whether to be included or excluded from the
selection.
The following Inclusion criteria (IC) were used:
• IC1: anxiety-related apps in Google Play Store
• IC2: apps that have a free version
• IC3: apps rated 4+ stars
IC1 focuses on apps available in Google Play
Store as, in contract with Apple App Store, it pro-
vides the number of installs of each app. Google Play
is a very popular app repository, with a wide range
of health apps, it includes over 41,377 app (Statista,
2019).
IC2 focuses the selection on free apps, as many
people can use them without payment. Moreover,
recent statistics in March 2020 showed that 96.3%
of Android apps were freely available worldwide
(Clement, 2020).
IC3 includes only apps that provide high user sat-
isfaction as the app’s user ratings reflect a certain level
of the app’s user satisfaction.
The apps identified from the search results that
met at least one of the following exclusion criteria
(EC) were excluded:
• EC1: apps that do not include the CBT approach
• EC2: apps that could not be installed
EC1 includes only anxiety app based on the CBT
approach, which are the focus of this study. EC2 ex-
cludes apps that could not be installed, therefore could
not be examined.
HEALTHINF 2021 - 14th International Conference on Health Informatics
282
2.2 Apps Analysis
The description of each app selected available in the
Google Play was examined. Each selected app was
installed in OPPO A9 (Android 9) and analyzed. Ex-
tracted data included:
• Name of the app
• Rating
• Number of raters
• MHP involved (e.g. therapists, counselors, re-
searchers, advisors, and others with a mental
health background), this information was re-
trieved from the app’s description
• Number of downloads
• Release date, which was retrieved from the App
Annie platform (https://www.appannie.com/en/)
3 RESULTS AND DISCUSSION
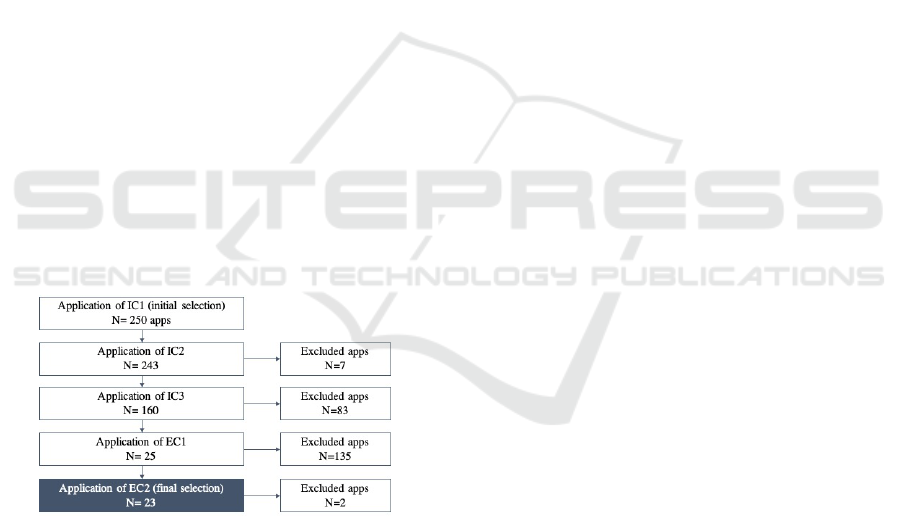
A total of 23 apps were included in the final selec-
tion as shown in Fig. 1. Table 1 presents information
on the included apps, and Table 2 presents apps that
involve MHP and information on the latest. It must
be noted that for some apps, the stated involvement
of MHP in the app was general, and did not provide
specific names. Twelve selected apps included MHP
in their design, while the rest did not.
Figure 1: Selection process.
One way to conduct requirements gathering is by
looking for answers to these questions: Who, What,
When, Where, Why and How (Stephens, 2015). In
the case of CBT-based apps for anxiety, the answer
to the “who” question is users suffering from anxiety;
the answer to the “what” is functionalities that will
help with anxiety; the answer to the “why” is to help
people suffering from anxiety to deal with it; and the
answer to the “how” can be any method able to de-
liver the functionalities identified in the “what” ques-
tion. Looking for answers of these questions from
end-users is not enough to create an app able to help
users deal with anxiety, even if they suffer from it.
They should not be considered as experienced in the
field of anxiety as they cannot provide a clear insight
on how to deal with it. Therefore, incorporating MHP
in mental health apps is necessary as they can provide
science- and evidence-based answers to the aforemen-
tioned questions. However, only half of the selected
apps involved MHP in their design. Inclusion of MHP
in the creation and design of apps for mental health,
is crucial to insure the safety of the end-user.
Many mental treatment approaches can be used
in a wrong way if not under supervision of a pro-
fessional. This is also the case of CBT, as it has
many disadvantages that should be acknowledged
(The Healthy CBT-Clinic, 2020), and in many cases
it works only under certain circumstances (Institute,
2020). MHP are knowledgeable of approaches used
for anxiety, like the CBT approach, and can present
methods to manage and treat anxiety, that can be
transformed to app functionalities, and can also pro-
vide directions on how to best implement those func-
tionalities in apps.
According to the U.S. Food and Drug Adminis-
tration (FDA), an app is considered of a “minimal
risk” to the user, if it helps users self-manage their
condition, provides tools to help users organize or
track their health information, or provide easy ac-
cess to information about a health condition or a
treatments, among others (FTC, 2016). Apps se-
lected in this study provide functionalities that fall un-
der the aforementioned characteristics, such as self-
assessment tests, guided relaxation audios, breathing
exercises, providing educational content, journaling
and mood tracking. This “minimal risk” can be miti-
gated by the involvement of MHP.
For an app to keep its health claims healthy
according to the Federal Trade Commission (FTC)
(Lesley Fair, 2015), it should first respect this prin-
ciple: “Claims about serious medical conditions call
for serious science”. The perfect way to ensure that a
mental care app respects this principle is by involving
MHP in the co-design of m-health apps in general and
mental health apps in particular. This would insure
that all implemented treatment-related functionalities
are based on well comprehended and previously prac-
ticed science, that have proof of being effective on
previous patients.
There is also a lack of research evidence on the
efficacy and effectiveness of health apps (Giota and
Kleftaras, 2014), including mental health apps, which
despite their potential effectiveness and ability to im-
prove treatment access, and improve the monitoring
and management of many mental health symptoms
and disorders, the majority of available ones still lack
On the Involvement of Mental Healthcare Professionals in the Co-design of Highly-rated Anxiety Apps
283
Table 1: Results.
ID App name Link Rating #Raters Latest
Update
Initial
release date
#Installs
A1 Youper - Emotional Health https://bit.ly/32AAnKq 4.7 46,031 22-May-20 27-Aug-15 1,000,000
A2 Wysa: stress, depression & anxiety ther-
apy chatbot
https://bit.ly/2Q3NAss 4.7 36,225 21-May-20 6-Oct-16 1,000,000
A3 Moodpath - Depression & Anxiety Test https://bit.ly/2X6FelC 4.6 23,980 15-Apr-20 1-Jun-17 1,000,000
A4 Sanvello (ex Pacifica) https://bit.ly/2rmJGAG 4.6 14,106 5-May-20 25-Jan-15 1,000,000
A5 InnerHour: Calm,Sleep,Depression &
Anxiety Therapy
https://bit.ly/2pNLOBn 4.5 4,109 9-May-20 22-Aug-17 500,000
A6 What’s Up? - A Mental Health App https://bit.ly/2Q2Hzwj 4.4 3,126 20-Apr-20 10-Mar-15 500,000
A7 BetterHelp: Online Counseling & Ther-
apy
https://bit.ly/32svl2A 4.3 7,392 15-Apr-20 17-Nov-14 500,000
A8 Stop Panic & Anxiety Self-Help https://bit.ly/2K5YaeS 4.7 2,353 15-Apr-20 21-Jan-12 100,000
A9 CBT Thought Record Diary https://bit.ly/2NyGHxH 4.7 671 22-May-20 28-Jun-14 100,000
A10 Woebot: Your Self-Care Expert https://bit.ly/33ySl1g 4.5 6,223 15-Apr-20 6-Mar-18 100,000
A11 Clear Fear shorturl.at/lsOUX 4.4 173 15-Apr-20 3-Dec-18 100,000
A12 Depression CBT Self-Help Guide https://bit.ly/36OIfvh 4.2 1,446 15-Apr-20 26-Feb-12 100,000
A13 feel better - Mood & CBT therapy to
manifest goals
shorturl.at/eowKP 4.6 539 15-Apr-20 24-Jul-17 50,000
A14 FearTools - Anxiety Aid shorturl.at/mnwY9 4.4 96 20-Apr-20 6-Dec-16 50,000
A15 UP! - Mood Tracker for Burnout and
Bipolar
shorturl.at/lFOQ6 4.3 1,859 30-Jul-19 50,000
A16 Moodfit - Tools & Insight to Shape Up
Your Mood
shorturl.at/rvHQR 4.6 280 2-May-20 19-Jan-17 10,000
A17 GG Relationship Doubt & Obsessions
(ROCD)
shorturl.at/cyF16 4.5 163 15-Apr-20 4-Jun-16 10,000
A18 OCD Daily Exercise by GG (GGOC) shorturl.at/joFIV 4.5 153 15-Apr-20 7-Sep-16 10,000
A19 Psychiatry Pro-Diagnosis, Info, Treat-
ment, CBT & DBT
shorturl.at/vwIV2 4.4 185 10-May-20 19-Mar-19 10,000
A20 Stress & Anxiety Companion https://bit.ly/2Vs9OXp 4.1 14 2-May-20 15-Oct-18 10,000
A21 Pocketcoach - Anxiety Helper https://bit.ly/2XmrLql 4.6 63 20-May-20 8-Aug-19 5,000
A22 De-StressMe: CBT Tools to Manage
Stress
shorturl.at/lsuPY 4.3 42 15-Apr-20 21-Jun-18 5,000
A23 Self-manage Depression: Daily exercise
(GGDE)
shorturl.at/czWZ2 4.3 33 11-May-20 24-Jul-18 1,000
Table 2: Mental health professionals involved.
ID Mental health professional involved
A1 Team of doctors and scientists led by Dr. Jose Hamilton (a psychiatrist)
A2 Advisors with a mental health background
A3 Experienced therapists and doctors.
A4 Psychologists
A5 Psychiatrists and therapists
A7 Counselors and therapists
A9 Licensed mental health professionals at Duke university
A10 Dr. Alison Darcy (a clinical research psychologist) and Dr. Athena Robinson (a psychologist and expert clinician).
A11 Developed by a clinician
A17, A18, A23 Dr. Guy Doron (IDC) (a clinical psychologist and researcher)
scientific evidence about their efficacy (Donker et al.,
2013; Wang et al., 2018). The majority of studies in-
vestigating health apps were found to test basic mo-
bile features like text messaging, and only few as-
sessed the impact of the apps based on their outcome
(Fiordelli et al., 2013).
CBT-based mental care apps are an example of
that, as even though CBT is an effective approach
when used face to face (Hofmann et al., 2012), the
evidence on its impact when implemented in an app
environment is limited (Giota and Kleftaras, 2014),
especially over a long time periods of use (Rathbone
et al., 2017). Inclusion of MHP in the design as
well as in the evaluation can help solve this issue.
When this is the case, apps will be based on scientific,
proven mental care approaches since the first stages of
their design, and their outcome regarding treatment
results can be properly investigated and tested based
on scientific evidence. An example of that, is the
selected app A3, which in its description, the devel-
HEALTHINF 2021 - 14th International Conference on Health Informatics
284
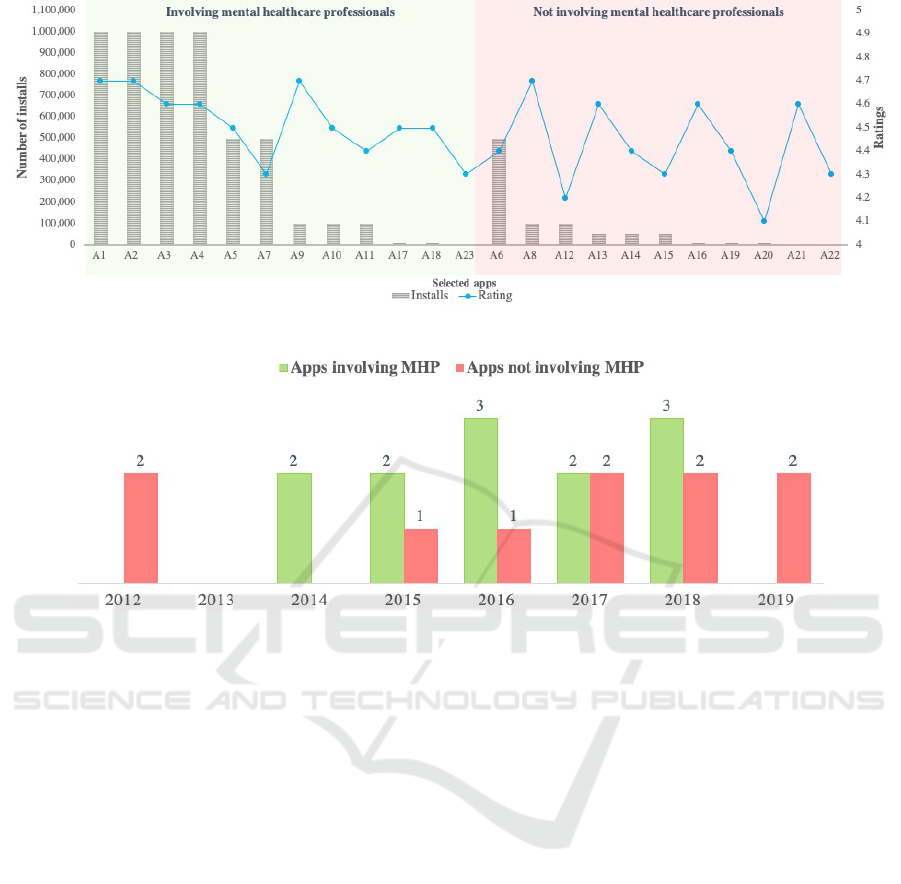
Figure 2: Number of installs and ratings of the selected apps.
Figure 3: Initial release years of selected apps. Acronym: Mental Healthcare Professionals (MHP).
opers specified the inclusion of researchers from the
fields of psychology and psychotherapy to conduct
clinical studies on the app. A recent study (Burchert
et al., 2019), compared the results of A3’s assess-
ment of mood dynamics with results from the Patient
Health Questionnaire (PHQ-9) depression screening,
Another recent study (Mulansky, 2020) analysed the
geodata of the A3’s users to determine its connection
to their state of mind.
After a careful analysis of the selected apps, we
found that 48% did not include MHP in their creation
process. If we project the aforementioned insights, we
can assume that many existing mental care apps were
not co-created with MHP. Such apps might jeopardize
the safety of end-users, and provide misguided infor-
mation or harmful practices. Results presented in Fig
2 also show that the involvement of MHP might in-
fluence the number of installs of a CBT-based anxiety
app. The average of installs of apps that mention in
their description the involvement of MHP is 443,417
installs, while the average of installs of the apps that
do not is 80,909 installs. Having MHP involved in the
design of an app might increase its chance of instal-
lation by five times. This big difference shows that
involvement of MHP might increase the trust of the
users in the app, and encourages them to install the
app and use it. It should be noted that on average both
categories of apps were released 4 years ago as shown
in Fig. 3. Note that the A15’ initial release date was
not available.
This study might have some limitations such as:
(i) including paid apps in the selection might have al-
lowed us to identify additional findings. However, the
majority of Android apps (96.3% of Android apps),
according to recent statistics, are available freely in
app repositories (Clement, 2020); and (ii) analyzing
low-rated apps might have allowed us to identify ad-
ditional findings as well. However, we investigated
highly-rated apps to remove concerns about the us-
ability of the studied apps.
4 CONCLUSIONS
This study investigated the involvement of MHP in
the co-design of CBT-based apps for anxiety. A to-
tal of 23 Android highly-rated apps were selected and
analyzed. Contrarily to our hypothesis, not all in-
vestigated apps included input from MHP, as nearly
half of the selected apps did not report any involve-
On the Involvement of Mental Healthcare Professionals in the Co-design of Highly-rated Anxiety Apps
285

ment of MHP in their design or evaluation. A sig-
nificant difference in numbers of installs in the se-
lected apps was identified. Results suggested that the
fact of mentioning the involvement of MPH in the
description of a CBT-based anxiety app, might im-
pact potential users trust, and increase its installation
chances by five times. This study further confirms the
existing concerns of existence of non-evidence-based
apps, that are neither co-designed, nor evaluated in
collaboration with MHP, which might influence the
apps’ safety and effectiveness.
For future work, we intend to work with psychia-
trists and other MHP to co-create a connected health
application for anxiety treatment in UAE.
ACKNOWLEDGMENTS
This work is part of the Abu Dhabi Young Investiga-
tor Award (AYIA) 2019 (#AYIA19-001) awarded by
the Abu Dhabi Research and Development Authority
(ADRDA).
REFERENCES
Anthes, E. (2016). Pocket psychiatry: mobile mental-health
apps have exploded onto the market, but few have
been thoroughly tested. Nature, 532(7597):20–24.
Bourque, P., Fairley, R. E., et al. (2014). Guide to the soft-
ware engineering body of knowledge (SWEBOK (R)):
Version 3.0. IEEE Computer Society Press.
Burchert, S., Kerber, A., Zimmermann, J., and Knaevel-
srud, C. (2019). 14-day smartphone ambulatory as-
sessment of depression symptoms and mood dynam-
ics in a general population sample: comparison with
the PHQ-9 depression screening. Frontiers in Psy-
chology, 10:704.
Clement, J. (2020). Statista. Free and paid app distribution
for Android and iOS 2020.
Cortman, C., Shinitzky, H., and O’Connor, L.-A. (2015).
Take Control of Your Anxiety: A Drug-free Approach
to Living a Happy, Healthy Life. Red Wheel/Weiser.
Costabile, M. F., Mussio, P., Provenza, L. P., and Piccinno,
A. (2009). Supporting end users to be co-designers of
their tools. In International Symposium on End User
Development, pages 70–85. Springer.
Dey, N., Rautray, P., and Soni, M. (2019). Patient-centered
design in a connected healthcare world: A case study.
In Research into Design for a Connected World, pages
967–976. Springer.
Donker, T., Petrie, K., Proudfoot, J., Clarke, J., Birch,
M.-R., and Christensen, H. (2013). Smartphones for
smarter delivery of mental health programs: a system-
atic review. Journal of Medical Internet Research,
15(11):e247.
Drissi, N., Ouhbi, S., Idrissi, M. A. J., Fernandez-Luque, L.,
and Ghogho, M. (2020a). Connected mental health:
Systematic mapping study. Journal of Medical Inter-
net Research, 22(8):e19950.
Drissi, N., Ouhbi, S., Idrissi, M. A. J., and Ghogho,
M. (2020b). An analysis on self-management and
treatment-related functionality and characteristics of
highly rated anxiety apps. International Journal of
Medical Informatics, page 104243.
Drissi, N., Ouhbi, S., Idtissi, M. A. J., and Ghogho, M.
(2019). Mobile apps for post traumatic stress disor-
der. In 2019 41st Annual International Conference of
the IEEE Engineering in Medicine and Biology Soci-
ety (EMBC), pages 4279–4282. IEEE.
Fiordelli, M., Diviani, N., and Schulz, P. J. (2013). Mapping
mhealth research: a decade of evolution. Journal of
Medical Internet Research, 15(5):e95.
FTC (2016). Mobile health apps interactive
tool. URL: www.ftc.gov/tips-advice/business-
center/guidance/mobile-health-apps-interactive-tool.
Giota, K. G. and Kleftaras, G. (2014). Mental health
apps: innovations, risks and ethical considerations.
E-Health Telecommunication Systems and Networks,
2014.
Harrison, V., Proudfoot, J., Wee, P. P., Parker, G., Pavlovic,
D. H., and Manicavasagar, V. (2011). Mobile mental
health: review of the emerging field and proof of con-
cept study. Journal of Mental Health, 20(6):509–524.
Hofmann, S. G., Asnaani, A., Vonk, I. J., Sawyer, A. T.,
and Fang, A. (2012). The efficacy of cognitive behav-
ioral therapy: A review of meta-analyses. Cognitive
Therapy and Research, 36(5):427–440.
Hollis, C., Morriss, R., Martin, J., Amani, S., Cotton, R.,
Denis, M., and Lewis, S. (2015). Technological in-
novations in mental healthcare: harnessing the dig-
ital revolution. The British Journal of Psychiatry,
206(4):263–265.
Institute, S. (Accessed on Sep 2020). What’s wrong with
CBT? URL: www.sweetinstitute.com/sweet-institute-
blog-and-news/2018/7/3/whats-wrong-with-cbt.
Larsen, M. E., Huckvale, K., Nicholas, J., Torous, J., Bir-
rell, L., Li, E., and Reda, B. (2019). Using science to
sell apps: evaluation of mental health app store quality
claims. NPJ Digital Medicine, 2(1):1–6.
Lesley Fair (2015). 5 principles to help keep your
health claims healthy. URL: www.ftc.gov/news-
events/blogs/business-blog/2015/12/5-principles-
help-keep-your-health-claims-healthy.
Liberati, A., Altman, D. G., Tetzlaff, J., Mulrow, C.,
Gøtzsche, P. C., Ioannidis, J. P., Clarke, M., Dev-
ereaux, P. J., Kleijnen, J., and Moher, D. (2009). The
PRISMA statement for reporting systematic reviews
and meta-analyses of studies that evaluate health care
interventions: explanation and elaboration. PLoS
Medicine, 6(7):e1000100.
Loerinc, A. G., Meuret, A. E., Twohig, M. P., Rosenfield,
D., Bluett, E. J., and Craske, M. G. (2015). Response
rates for CBT for anxiety disorders: Need for stan-
dardized criteria. Clinical Psychology Review, 42:72–
82.
HEALTHINF 2021 - 14th International Conference on Health Informatics
286

Loo Gee, B., Griffiths, K. M., and Gulliver, A. (2016). Ef-
fectiveness of mobile technologies delivering ecolog-
ical momentary interventions for stress and anxiety: a
systematic review. Journal of the American Medical
Informatics Association, 23(1):221–229.
Lyneham, H. J. and Rapee, R. M. (2006). Evaluation of
therapist-supported parent-implemented CBT for anx-
iety disorders in rural children. Behaviour Research
and Therapy, 44(9):1287–1300.
Mayo Clinic Staff (Accessed on Sep 2020). Cognitive
Behavioral Therapy. URL: www.mayoclinic.org/tests-
procedures/cognitive-behavioral-therapy/about/pac-
20384610.
Mulansky, L. (2020). Untersuchung der Geodaten von
Benutzern der Moodpath mHealth App mithilfe von
Methoden des Maschinellen Lernens. PhD thesis, Ulm
University.
Norton, P. J. and Barrera, T. L. (2012). Transdiagnostic
versus diagnosis-specific CBT for anxiety disorders:
A preliminary randomized controlled noninferiority
trial. Depression and Anxiety, 29(10):874–882.
Olff, M. (2015). Mobile mental health: a challenging re-
search agenda. European Journal of Psychotrauma-
tology, 6(1):27882.
Ouhbi, S., Karampela, M., and Isomursu, M. (2019). Inte-
grating users logic into requirements engineering for
connected healthcare co-design. In In Proceedings
of the 14th International Conference on Evaluation
of Novel Approaches To Software Engineering (enase
2019), pages 480–485. SCITEPRESS Digital Library.
Pohl, K. (2010). Requirements engineering: fundamentals,
principles, and techniques. Springer Publishing Com-
pany, Incorporated.
Rathbone, A. L., Clarry, L., and Prescott, J. (2017). As-
sessing the efficacy of mobile health apps using the
basic principles of cognitive behavioral therapy: sys-
tematic review. Journal of Medical Internet Research,
19(11):e399.
Salari, N., Hosseinian-Far, A., Jalali, R., Vaisi-Raygani, A.,
Rasoulpoor, S., Mohammadi, M., Rasoulpoor, S., and
Khaledi-Paveh, B. (2020). Prevalence of stress, anxi-
ety, depression among the general population during
the COVID-19 pandemic: a systematic review and
meta-analysis. Globalization and Health, 16(1):1–11.
Statista (2019). Number of mhealth apps available in the
Apple App Store from 1st quarter 2015 to 3rd quarter
2019.
Stephens, R. (2015). Beginning software engineering. John
Wiley & Sons.
The Healthy CBT-Clinic (Accessed on Sep 2020).
Pros & Cons of CBT Therapy. URL =
http://www.thecbtclinic.com/pros-cons-of-cbt-
therapy.
Torous, J. and Keshavan, M. (2020). COVID-19, mobile
health and serious mental illness. Schizophrenia Re-
search.
Van Leersum, C. M., Moser, A., van Steenkiste, B.,
Reinartz, M., Stoffers, E., Wolf, J. R., and van der
Weijden, T. (2020). What matters to me–a web-
based preference elicitation tool for clients in long-
term care: a user-centred design. BMC Medical Infor-
matics and Decision Making, 20(1):1–12.
Wang, K., Varma, D. S., and Prosperi, M. (2018). A sys-
tematic review of the effectiveness of mobile apps for
monitoring and management of mental health symp-
toms or disorders. Journal of Psychiatric Research,
107:73–78.
On the Involvement of Mental Healthcare Professionals in the Co-design of Highly-rated Anxiety Apps
287
