
Trust Profile based Trust Negotiation for the FHIR Standard
Eugene Sanzi and Steven A. Demurjian
Department of Computer Science & Engineering, University of Connecticut, 371 Fairfield Way, Storrs, U.S.A.
Keywords: Trust Negotiation, Trust Profile, FHIR, Authorization, Healthcare.
Abstract: Sensitive healthcare data within Electronic Healthcare Records (EHRs) is traditionally protected through an
authentication and authorization process. The user is authenticated based on a username/password
combination which requires a pre-registration process. Trust profile based trust negotiation replaces the
required human intervention during the traditional pre-registration process with an automated approach of
verifying that the user owns the trust profile with digital signatures. To accomplish this, the negotiation
process gradually exchanges the credentials within the trust profile to build trust and automatically assign
authorization rules to previously unknown users. In this paper, we propose a new model for attaching trust
profile authorization data to Fast Healthcare Interoperability Resources (FHIR), a standard created by HL7,
in order to integrate the process of trust profile based trust negotiation into FHIR.
1 INTRODUCTION
The healthcare industry is increasingly adopting new
techniques for sharing secure healthcare data through
Health Information Exchange (HIE) (De Pietro &
Francetic, 2018). While integration between
electronic healthcare records (EHRs) stored at
multiple providers has been hampered due to the
difficulty in implementing interoperability standards,
the exchange of patient healthcare data between
providers is shown to positively affect patient
treatment and patient satisfaction (Yasnoff, 2015).
However, the authorization to healthcare data
between healthcare providers is still attached to the
slow username/password combination authentication
process which requires explicit pre-registration. This
pre-registration slows the dissemination of
potentially time-critical sensitive healthcare data by
requiring a system administrator to remotely
determine a potential user’s identity and explicitly
assign authorization to the user.
Despite the difficulties in coordinating the
exchange of health data, healthcare providers are
adopting new technologies that facilitate its
exchange. The Fast Healthcare Interoperability
Resources (FHIR) (HL7 International, 2020) is a
healthcare interoperability standard whose goal is to
facilitate the retrieval of healthcare data by providing
a common API to locate and exchange healthcare
records. FHIR’s data exchange structure is built on
the concept of a resource, which provides a
meaningful set of healthcare related data for transfer.
FHIR provides over 125 different resources for:
patients, observations, medications, patient consent,
etc. Requests for a specific resource are available
through a REST API that supports instance level
interactions such as: read, vread (version read),
update, patch (update a portion of a resource), delete,
and history interactions. FHIR has emerged as a
popular choice (Posnack & Barker, 2018) for
supporting HIE. Microsoft has an azure API for FHIR
(https://azure.microsoft.com/en-us/services/azure-
api-for-fhir/), and Google has created a cloud
healthcare API using FHIR (https://cloud.google.
com/healthcare). Large EHR providers such as Epic
(Epic Systems Corporation, 2020) and Cerner
(Cerner, 2020) have leveraged FHIR to facilitate HIE
for patient use.
Trust negotiation (Winsborough et al., 2000) was
introduced as a method of building trust between two
parties whose identities were previously unknown to
each other. In this context, trust is defined as the
ability to ascertain that the other party is authorized
to obtain the requested sensitive data and will handle
the data appropriately. During trust negotiation, each
participant possesses a set of credentials capable of
describing whether the other participant should
consider them trustworthy. The credentials are
exchanged between participants throughout several
rounds of trust negotiation until there is a
242
Sanzi, E. and Demurjian, S.
Trust Profile based Trust Negotiation for the FHIR Standard.
DOI: 10.5220/0009830502420251
In Proceedings of the 9th International Conference on Data Science, Technology and Applications (DATA 2020), pages 242-251
ISBN: 978-989-758-440-4
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

determination that: each participant possesses the set
of credentials necessary to obtain trust; or, at least one
participant does not possess a trustworthy set of
credentials meaning trust cannot be established. One
effort (Ryutov et al., 2005) extended trust negotiation
by creating an adaptive framework, allowing online
business to determine customer trustworthiness based
on past purchase value. This adaptive framework has
been expanded to include our controller’s adaptation
to the requestor’s role and the specific resource being
accessed. In (Vawdrey et al., 2003), trust negotiation
was adapted to healthcare by describing a trust
negotiation process for obtaining a patient’s EHR, but
provides only a healthcare license as a credential. In
(Elkhodr et al., 2011), a three step trust negotiation
process is used for determining the authenticity of a
request for healthcare data, but still requires that the
identity of the requestor is previously known.
Our prior work proposed and defined a trust
profile (Sanzi et al., November 2016) as an extension
to trust negotiation that defines a set of credentials
based on the trust profile owner’s history of
successful access to sensitive data via trust
negotiation. A trust profile is a collection of access
history credentials that describe a particular user (the
owner) and are digitally signed by a controller, an
entity responsible for the secure dissemination of
sensitive data. Trust profiles utilize X.509 identity
certificates (Cooper et al., 2008), attribute certificates
(Farrell & Housley, 2002), and certificate chaining to
build trust between controllers in the credentials they
have digitally signed (Sanzi & Demurjian, May
2016). The users send a request for data with a subset
of their personal trust profile to a controller, which
then reads the access history provided, determines
whether the credentials are sufficient to establish
trust, and releases the data if sufficient trust has been
established (Sanzi et al., 2017). If trust negotiation is
successful, the controller creates new credentials
detailing the new access to sensitive data and sends
them to the user with the requested data. These new
credentials are then added to the user’s personal trust
profile to be presented to other controllers during
future trust negotiation attempts. This improves upon
previous works by providing a standardized set of
credentials describing an entire access history,
allowing complex requirements to be formulated on
the controller side, and new credentials to be obtained
during the course of a user’s career.
Our work in this paper is part of an ongoing effort
to integrate trust profile based trust negotiation into
the authorization process of modern EHRs across all
of the healthcare stakeholders (e.g., physicians,
nurses, insurance billing agents, patients, patient
families, etc.). The decentralization of healthcare
information has spread across multiple EHRs as
patients increasingly are being treated by teams of
healthcare specialists in geographically separated
locations. Our new proposed method of authorization
for the release of sensitive healthcare data is required
and replaces the time intensive pre-registration
process. The FHIR security model is enhanced by
integrating a new capability that incorporates the
option for trust profile based trust negotiation during
a resource request if the requestor is unknown to the
healthcare organization providing FHIR based HIE.
In support of this work, we propose a new model that:
details trust profile metadata integrated into FHIR
resources; and, describes the trust profile credentials
needed to obtain access utilizing a combination of
role-based access control (RBAC) (Ferraiolo et al.,
2001) and mandatory access control (MAC) (Bell &
La Padula, 1976). Successful access to FHIR data
results in requestors obtaining needed healthcare data
quickly and includes dynamic additions to their trust
profiles detailing access to the requested resources
that can be presented to other FHIR systems during
future trust negotiation attempts.
The remainder of this paper is organized into five
sections. Section 2 presents background on FHIR,
access control models, trust negotiation, trust profiles,
and the process of obtaining authorization via trust
negotiation supported by trust profiles. Section 3
introduces extensions to our existing trust profile
model (Sanzi et al., 2017) for intercepting resource
requests to provide trust profile based authorization
by annotating FHIR concepts and resource objects
with trust profile data, and resolving authorization to
the requested resources. Section 4 presents an
example of the model applied to the healthcare
domain. Section 5 has a conclusion for the paper.
2 BACKGROUND
2.1 Access Control
The Role-based access control (RBAC) (Ferraiolo et
al., 2001) model binds a set of permissions to operate
on data (create, read, update, delete) to roles (e.g.,
physician, nurse, front desk secretary, etc.). These
roles are then assigned to users. When a user is
assigned a role, the user may perform any action
allowed in that role’s permission set. RBAC is a
popular access control model in healthcare as a result
of its ability to simplify the assignment of complex
permissions through role assignment, allowing
consistent permissions across each type of job.
Trust Profile based Trust Negotiation for the FHIR Standard
243
During trust negotiation, the user’s assumed role
allows our controller to map a set of required trust
profile credentials to the specific resource requested.
The Mandatory access control (MAC) (Bell & La
Padula, 1976) model defines a set of sensitivity levels
on subjects (users) and objects (data) and allows
access to the data if the user meets the required
sensitivity level. MAC is generally modeled with
levels: top secret (TS) < secret (S) < classified (C) <
unclassified (U). If a user wishes to read data, they
must meet or exceed the sensitivity level assigned to
the data they wish to access. MAC in healthcare can
be implemented as a method where the sensitivity
level of the data corresponds with the potential for
damage if released.
2.2 Trust Profiles
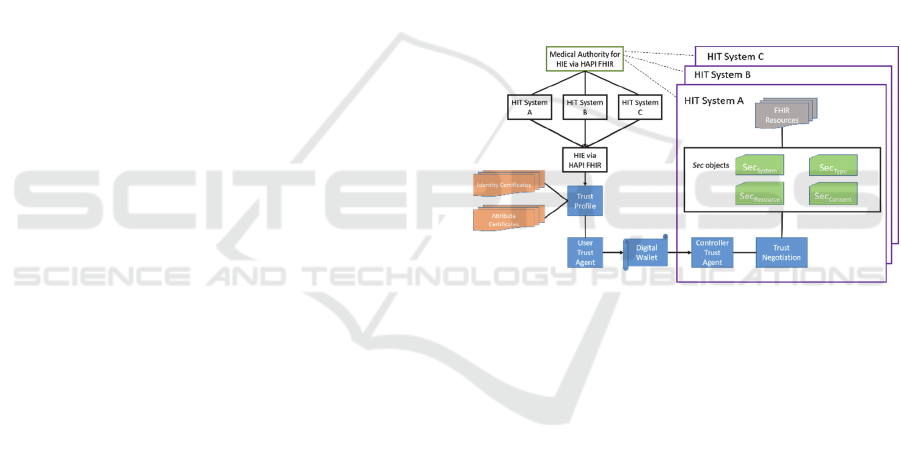
To facilitate the discussion of trust profile concepts,
Fig. 1 displays a generalized overview of trust
negotiation extended with trust negotiation. The
medical authority in the upper left corner establishes
trust between HIT Systems A, B, and C below by
digitally signing its CA certificates, allowing each of
them to trust any certificates signed by the other two.
A user’s trust profile, consisting of the identity and
attribute certificates appearing on the left side of Fig.
1, is endorsed through the digital signatures provided
by HIT Systems A, B, and C. A user constructs a
digital wallet, which is sent to the controller of an HIT
system. The controller utilizes the four Sec objects to
be introduced in Section 3 to build a credential
expression that describes the entries in the trust
profile necessary to release the FHIR resources that
they protect.
In Fig. 1, a trust profile is a complete collection
of a user’s entire history of access to sensitive data. In
the healthcare field, a trust profile would describe
each successful access a healthcare professional is
granted to sensitive healthcare data. A trust profile is
encoded in a series of X.509 encoded identity
(Cooper et al., 2008) and attribute certificates (Farrell
& Housley, 2002). Healthcare controllers issue one
identity certificate per user the first time a user
successfully accesses healthcare data from the
controller. The accesses are described in sets of
attribute certificates attached to the identity
certificates. An attribute certificate is attached to an
identity certificate by including the identity
certificate’s serial number and issuer, which is a
combination that must be unique to that identity
certificate. The attribute certificate is digitally signed
by the controller to prevent subsequent modification.
The identity certificates describe a user’s public
key, and the user proves ownership of the trust profile
data by proving ownership of the private key
associated with the public key listed in the identity
certificates. This also allows the user to claim
ownership of any attribute certificate attached to the
identity certificate. A healthcare provider must obtain
his/her own certificate to allow a controller to act as a
certificate authority (CA), allowing them to digitally
sign trust profile certificates. The trust profile
certificates digitally signed by a healthcare provider
are only trusted by another provider during trust
negotiation if: the other provider has decided to trust
the controller’s certificate by adding it directly to a
local trust store; or, the other provider trusts the entity
that signed the controller’s certificate by adding the
entity’s certificate to a local trust store. A healthcare
organization promotes trust by performing as a
trusted entity signing the requestor’s trust profile
entries.
Figure 1: Overview of trust profile based trust negotiation.
Each user may obtain multiple identity
certificates (left side of Fig. 1), one from each
controller that has granted sensitive data access. Each
identity certificate may have one or more attached
attribute certificates and the access described within
the attribute certificate must refer to data accessed
from the controller that signed the attached identity
certificate. A controller may only describe accesses
that occurred within the EHR it controls. When a user
with a trust profile discovers healthcare data, the user
first initiates a request for trust negotiation by
specifying: the resource being requested, the role the
user possesses, and an initial subset of the trust profile
referred to as a digital wallet (bottom portion of Fig.
1). The controller receives the request, retrieves
security metadata for the resource, and builds a
credential expression (ψ) during trust negotiation
located at the bottom of HIT System A’s purple box
(right side of Fig. 1). The credential expression
represents credentials that must be present in the
digital wallet to grant the requestor access to the
DATA 2020 - 9th International Conference on Data Science, Technology and Applications
244

resource. The controller retrieves the four Sec objects
(inner box of HIT System A) that describe the
security constraints on the FHIR resource being
requested (top of HIT System A). The controller may
generate a set of release actions that depend on the
credentials the requestor presents, such as: redacting
sensitive data if the credentials are insufficient to
release more sensitive data, logging the transaction in
different severity logs, or dispatching audit
notifications to the local system administrator.
If the credentials passed to the controller within
the digital wallet are insufficient, the controller builds
a server governance policy (SGP) (Winsborough et
al., 2000) that describes the missing requirements.
Trust negotiation may occur over several rounds, as
the requestor and controller negotiate the release of
potentially sensitive trust profile credentials. If the
presented credentials are insufficient, negotiation
fails and the connection is terminated. If the requestor
has presented sufficient credentials to obtain access to
the resource, the controller generates new certificates
to describe the current data access and sends the
certificates and health data back to the requestor. If a
new identity certificate is required, the controller asks
the requestor for a new public key for the new identity
certificate. The controller then performs its release
actions depending on the credentials matched to the
credential expression and terminates the connection.
The requestor receives the healthcare data and trust
profile certificates and adds the new certificates to the
trust profile. These new certificates may be used
during trust negotiation with any controller.
Trust negotiation failures may be caused by a lack
of required credentials or by deadlock during the trust
negotiation process, where both the requestor and
controller require a credential from the other before
their own required credential can be released. Our
integration of release actions improves the success
rate by allowing controllers to relax requirements on
the requestor in exchange for a lower rated trust
transaction, which may result in data redaction or
notes for manual auditing. Oblivious attribute
certificates (Li & Li, 2006) can be used to eliminate
deadlock by creating certificates that can only be read
if the receiver possesses the attributes necessary to
read them. With oblivious attribute certificates, data
can be exchanged without the possibility of it being
readable if the receiver is not authorized to view it.
2.3 FHIR
Fast Healthcare Interoperability Resources (FHIR)
(HL7 International, 2020) provides structures for
sharing EHR data between healthcare providers. Data
is accessed through resources. Resources are
accessed utilizing a location URL as part of a REST
API in conjunction with a logical ID. This allows data
that resources describe to sync between separate
FHIR systems.
FHIR resources are organized in categories:
foundation resources, base resources, clinical
resources, financial resources, and specialized
resources. We highlight only a subset relevant for the
paper. The base resources describe: patients,
practitioners, and family relationships; organizations,
services, appointments, and encounters. The clinical
resources are for a patient’s health history, including:
diagnostic data, medications, care provision, and
request/response communication. HAPI FHIR
(HAPI FHIR, 2020) is a Java implementation of the
FHIR resources Patient, FamilyMemberHistory,
Condition, Observation, Diagnostic Report,
Medication, Immunization, AllergyIntolerance,
Coverage, EligibilityRequest, Claim,
PaymentNotice, etc. The resources are available
through the FHIR standard's REST API.
3 TRUST PROFILE AND FHIR
INTEGRATION
In this section, we describe our method for integrating
FHIR with a trust profile based trust negotiation
approach for dynamic and automatic authorization to
requested FHIR resources that extends our prior work
on a trust profile model (Sanzi et al., 2017) that
encodes several different properties of access to a
healthcare system within four types of attribute
certificates. The remainder has seven subsections.
Section 3.1 explores the interaction between the data
encoded in trust profile attribute certificates and a
description of the type of security metadata tracked
within four different types of Sec objects. Each of the
four different types of Sec object metadata is
elaborated on in Sections 3.2, 3.3, 3.4, and 3.5
respectively. Section 3.6 describes the internal
structure of the security objects. Section 3.7 describes
the way that the security constraints of each of the
four Sec objects are combined to resolve a request.
3.1 Sec Object Interaction
The trust profile’s attribute certificate types track: the
associated identity certificate, the attribute certificate
issuer, and a timestamp. The attribute certificate types
are: affiliation certificates (AC
Affiliation
), data resource
access certificates (AC
DataResourceAccess
), data resource
Trust Profile based Trust Negotiation for the FHIR Standard
245

confidentiality certificates (AC
DataResourceConfidentiality
),
and system confidentiality certificates
(AC
SystemConfidentiality
). Affiliation certificates denote
current employment with a trusted healthcare
provider and signify a thorough manual background
check as part of the pre-employment process. Data
resource access certificates provide metadata on the
role the user possessed during the access, FHIR
resource ID, and the system ID representing the FHIR
server that serviced the originating request. The data
resource confidentiality certificate provides: the
confidentiality level of the resource accessed, the
FHIR resource ID, and the system ID. The system
confidentiality certificate describes the highest level
of confidentiality that the certificate subject has
accessed on the FHIR server and the system’s ID.
In support of trust profile integration, we have
modified the HAPI FHIR implementation to enable
the creation of a credential expression whose access
rules are created based on a configuration. This
metadata describes the properties needed in the
requestor’s trust profile to gain authorization to the
resource. The modifications support the creation of
multiple credential expressions based on any set of
properties specified within the trust profile.
Security metadata for our extension is divided
into one of four levels, whose various access rules are
combined utilizing the process described in this
section to form one credential expression for the
entire trust negotiation process. These four levels are:
system security refers to the requirements that
the controller must observe in the requestor’s
trust profile to gain access to any resources
resource type security refers to the
protections of an individual type of resource
resource security refers to the actual
protection of an individual resource instance
on the FHIR server and data within the object
patient consent refers to the ability of a
patient to describe which healthcare
providers may access each resource, at either
the resource type or individual resource level
3.2 System Security Metadata
System security (Sec
System
) refers to the requirements
the controller must observe in the requestor’s trust
profile to gain access to any resources. This may
include a valid affiliation certificate denoting current
employment at a trusted healthcare provider and at
least one data resource access certificate describing
access to a resource under the role requested for the
current trust negotiation. System security also
encompasses the overall highest security clearance
the user has been granted on a specific system. As
specified in the trust profile model, an identity
certificate in a trust profile may have a system
confidentiality attribute certificate attached to it that
records the highest security clearance previously
granted to the trust profile owner by the specific
healthcare system that signed it. This certificate is
replaced with a newer certificate listing a higher
clearance in the event that the controller grants the
requestor access to a resource with a higher listed
security clearance than the clearance listed in the
requestor’s system confidentiality attribute
certificate. The requestor may be assigned higher
security clearances by the FHIR server depending on
which trust profile entries the requestor sends to
satisfy the generated credential expression. An
AC
SystemConfidentiality
certificate previously digitally
signed by the controller may be provided during
negotiation to claim a previous confidentiality level
assigned by the controller. A system confidentiality
level may be assigned based on the perceived damage
caused by a potential unauthorized leak of the
requested data, and a requestor that meets the
confidentiality requirements for portions of the
requested resource, but not the entire resource, may
result in a release action (RA) (Sanzi et al., 2017) that
causes the controller to filter data of higher sensitivity
from the resource before sending it to the requestor.
3.3 Resource Type Security Metadata
Resource type security (Sec
Type
) refers to the
protection of all of the resources of a given type.
Resource types are further divided into base, clinical,
and financial resource types (HL7 International,
2019). Each resource type possesses an associated
security object that describes the credentials that must
be presented by the requestor for the controller to
release a resource of the given type. The required
credentials are described by a series of Access History
Properties (AHP), each describes a single property of
access to a sensitive FHIR resource. These credentials
are also organized within the security object by the
role the requestor assumes for the given trust
negotiation transaction. Recall that (Sanzi et al.,
2017) specifies that in the initial request for trust
profile based trust negotiation, the requestor specifies
the role (e.g., family physician, emergency room
physician, nurse, billing agent, front desk secretary,
etc…) to be assumed for the purposes of negotiation.
The controller filters the resources a requestor of a
given role accesses based on the perceived needs of a
DATA 2020 - 9th International Conference on Data Science, Technology and Applications
246

role. For example, a physician role will be allowed to
access clinical resources (e.g., summary, diagnostics,
medications, care provisions, request and responses)
whereas a front desk secretary may be limited to the
patient resource (describing the patient’s
demographic data) under the base category. The role
specified by the requestor will also affect the proof
the controller requests for assurance of the requestor’s
membership of the specified role. A family physician
requesting a patient’s clinical resources may be asked
to provide credentials from the trust profile indicating
a historical access to the patient’s clinical resources
whereas a front desk secretary may only have to
provide proof of employment (affiliation) via a desk
secretary role to access a patient’s demographic data.
3.4 Resource Security Metadata
Resource security (Sec
Resource
) protects an individual
resource object on the FHIR server and the data
within the object. The resource Sec
Resource
provides
security data for is identified within the Sec
Resource
by
a matching identifier. Sec
Resource
is similar to Sec
Type
with the exception that it protects an individual
resource instance as contrasted to an entire collection
of resources of a certain type, increasing the
granularity with which a resource is protected. When
the request for a FHIR object through trust
negotiation is first received, the Sec
Resource
object
attached to the requested FHIR object is retrieved by
matching the FHIR ID.
3.5 Patient Consent Security Metadata
Patient consent security (Sec
Consent
) allows the patient
described by the FHIR object to provide input as to
which healthcare providers may access each resource,
at either the resource type or individual resource
level. Our Sec
Consent
security object is based on the
principles of patient consent (The Office of the
National Coordinator for Health Information
Technology, 2019) outlined by The Office of the
National Coordinator for Health Information
Technology (ONC). Patient consent methods allow
patients to consent to HIE among multiple healthcare
providers by allowing patients to note when and how
their health data is shared whether their health data is
shared for treatment, bill payment, or general
healthcare operations. Our patient consent object
overrides other security objects when present,
allowing the patient to have final authority over the
disclosure of the health record. The Sec
Consent
object is
built by the patient and attached to the patient’s
records within a FHIR system, allowing the patient to
provide input as to which trust profile credentials are
necessary during trust negotiation for the release of
different types of FHIR data and FHIR resources.
The patient interacts with the Sec
Consent
object via
a patient portal provided by the healthcare
organization maintaining the FHIR server. The
patient portal follows the ONC’s meaningful consent
guidelines (The Office of the National Coordinator
for Health Information Technology, 2018) and
describes the patient’s choices as well as the
implication of their options regarding what data will
be released to which types of providers under
different circumstances. The patient portal interface
provided by the healthcare organization presents
multiple options that cover different use cases along
with descriptions for which healthcare providers have
access to the patient’s FHIR resources depending on
the options chosen. This simplifies the selection
process for a patient, allowing the patient to fully
comprehend the implications of each choice without
needing a deep understanding of trust profiles or trust
negotiation. At the healthcare provider’s discretion,
more granular interfaces can be made available to the
patient should the patient have the knowledge to
construct more detailed Sec
Consent
objects. The
Sec
Consent
object contains the same format as the
Sec
Resource
and Sec
Type
objects with the restriction that
a Sec
Consent
object is only attached to a FHIR resource
via ID if the resource ID’s patient identifier matches
the identifier of the patient creating the Sec
Consent
object. Additionally, the patient may include multiple
instances of a healthcare professional’s public key
from a trust profile identity certificate. This allows the
patient to identify a healthcare professional as being
able to access a portion of the patient’s healthcare
records if the patient has a pre-existing relationship.
If a public key is listed as a potential credential to gain
access to a FHIR resource, the healthcare professional
attempting to access the resource proves ownership of
the public key by proving ownership of the associated
private key. This is done by digitally signing a
message with the private key during trust negotiation
in accordance with public key infrastructure.
3.6 Security Object Structure
Each Sec object contains a tree structure as illustrated
with the Sec
Type
example in Fig. 2 detailing the
specific credentials that must be presented to the
controller on a per role basis, as well as release
actions required for the release of the resource based
on which parts of the credential expression are
satisfied. A Sec object is organized into a tree
structure. The root of the tree contains an identifier
Trust Profile based Trust Negotiation for the FHIR Standard
247
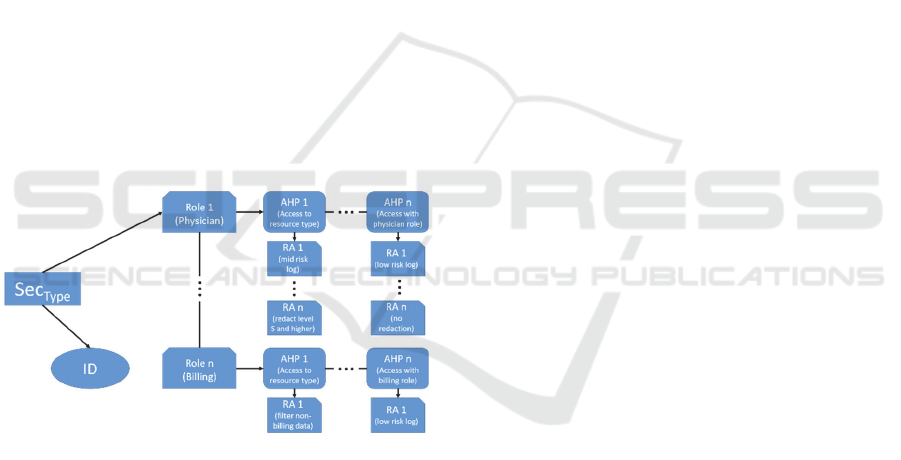
that defines the type of Sec object. The Sec
System
,
Sec
Type
, Sec
Resource
, and Sec
Consent
objects also provide
the system ID, resource type ID, resource ID, or
patient ID, respectively, that they are responsible for
protecting. The next level of the tree represented by
the top branch in Fig. 2, which provides a supported
list of roles capable of retrieving data of the requested
Sec object. For example, a Sec
System
object contains a
complete listing of all of the roles that are able to
access any sensitive data protected by the controller,
whereas Sec
Type
for an Observation will only contain
the roles that are capable of accessing an Observation.
Each role contains subtrees representing the AHPs
that the controller must request from the requestor’s
trust profile to grant access if the requestor is
assuming that role. An AHP is noted as required, in
which case its absence in the credentials during trust
negotiation causes trust negotiation to fail; or
optional, which allows the FHIR object to be released
even if not present. The existence of required or
optional AHPs allows more flexibility in the ability to
build trust between the requestor and controller by
requesting the presence of an AHP without requiring
it, while still providing a baseline for AHPs that must
be present for the controller to trust the requestor with
the release of the requested FHIR object.
Figure 2: An example Sec object structure.
Each AHP has an optional set of release actions,
RAs, attached to it that describes ancillary actions the
controller must take to approve the satisfaction of the
AHP requirement by a credential in the requestor’s
trust profile. The RA for an AHP optionally has:
potential additions, modifications, or redactions of
the resource before release to the requestor; or
specifies side effect actions such as noting the release
of the resource at certain risk levels in a multi-level
audit log and dispatching audit notifications to the
healthcare organization’s local security auditor for
immediate review. Additions to the resource include
contextual data not requested but necessary to
understand the resource, e.g., a program for reading
X-Ray scans. Modifications to the resource include
changes such as translating embedded data into a
standard format. Redactions may occur if the
requestor’s credentials meet a trust level sufficient to
access parts of a resource, but not the entire resource.
In this case, the sensitive data is redacted, allowing
the requestor to obtain the subset of useful data that
the requestor is authorized to access. Integrating an
RA into a resource is a method that the controller uses
to increase the rate of trust negotiation success and
disseminate requested PHI without compromising
patient security.
Conceptually, each AHP listed in a Sec object
represents an entry in the requestor’s trust profile that
proves successful, secure handling of the type of Sec
object by the role. The healthcare organization that
shares the PHI is responsible for determining the
AHPs necessary as to whether a requestor is
trustworthy. A requestor making a request under a
family physician role for their patient’s EHR data
located at a remote healthcare organization could
result in the following requested AHPs and RAs:
Sec
System
: Affiliation with any healthcare
provider (RA: log as high risk)
Sec
Type
: Past access to a resource of the same
type within the last year (RA: reduce log level
to medium risk, redact resource data with
sensitivity: S or higher)
Sec
Resource
: Optional: Past access to a resource
belonging to the patient within the last two
years (RA: reduce log level to low risk, audit
notification not required, no redaction
required)
Sec
Consent
: Affiliation with a listed healthcare
provider (RA: notify patient of access
through a healthcare portal)
3.7 Request Resolution
When a request for trust negotiation is initially
received, the controller first retrieves each of the four
Sec objects that will be associated with the request:
the system object for the FHIR installation as a whole,
the type object for the type of resource being
requested, the resource object for the individual
FHIR resource by ID, and, the consent object
associated with the patient. Each Sec object must be
satisfied by one or more credentials sent by the
requestor to determine the requestor’s
trustworthiness. When the controller receives a
requestor’s trust profile credential and has finished
verifying the credentials authenticity, an attempt is
DATA 2020 - 9th International Conference on Data Science, Technology and Applications
248

made to match it against the AHPs in each of the four
retrieved Sec objects. The controller records which of
the AHPs has been satisfied, and creates an SGP
based on which AHPs remain unsatisfied to send back
to the requestor. All of the four Sec objects must be
satisfied for the trust negotiation to be successful. A
Sec object may specify that a particular AHP is
optional, thereby increasing trust in the requestor and
modifying the release actions accordingly.
Additionally, the Sec object may define a set of AHPs
as optional, but require that at least one be met for the
Sec object to be satisfied. A single trust profile
credential is potentially capable of satisfying multiple
AHPs across multiple Sec objects. During credential
exchange, the controller is continually checking the
requestor’s credentials and matching them to the Sec
objects until all of the AHPs are satisfied or the
requestor chooses not to send another credential. If
the requestor chooses not to send another credential,
the controller checks whether all of the four Sec
objects are satisfied, executes the release actions, and
provides the resource and new trust profile
credentials. The controller’s final set of release
actions are resolved hierarchically from Sec
System
to
Sec
Resource
by beginning with the Sec
System
’s set of
release actions and combining with Sec
Type
’s release
actions, then Sec
Resource
’s release actions. When two
RAs conflict at different levels, the RA at the lowest
level (closest to the individual resource) takes
precedence. The Sec
Consent
’s release actions are
separated from the other three Sec objects and are
always executed as specified by the patient. The
consent object concerns patient notifications but may
also filter access to the patient’s resources more
strictly or release resources more freely to specific
healthcare providers and thus override the other three
Sec objects. Within a single Sec object, each AHP
contains a ranking, with higher ranking determining
which RA is executed if there is a conflict between
two RAs in two satisfied AHPs.
4 HEALTHCARE EXAMPLE
In this section, we demonstrate the operation of a trust
profile enhanced FHIR installation by providing an
example of an implementation in a healthcare setting
in Greater Hartford, Connecticut. Jane is a physician
working at Family Medicine Center (FMC) as a
family physician. Fig. 3 shows the different
interactions of Dr. Jane as she proceeds through the
trust profiling process to request permission to access
a new FHIR resource at another location that she has
not been authorized to. During her career, she has
gradually built a trust profile containing an access
history that describes access to sensitive data from
both her local EHR as displayed in the lower left of
Fig. 3 and remote access to EHRs maintained by other
healthcare providers in the area. While retrieving her
patient’s EHR, she discovers that the patient has
recently been seen at Hartford Hospital (HH) and a
new healthcare record of the FHIR Observation
resource was generated, represented by the Patient
Observation in the top middle of Fig 3. Dr. Jane is
unknown to HH and HH has no record of her, but
maintains a FHIR installation that supports trust
profile based trust negotiation.
Dr. Jane begins by initiating a request for trust
negotiation to HH under her family physician role for
the patient’s FHIR resource, which includes a trust
profile credential indicating current affiliation with
FMC, and sends it to HH. Dr. Jane is now the
requestor. The controller at HH receives the request
for trust negotiation, identifies the resource being
requested, and extracts the trust profile credentials.
The controller must now build the credential
expression that defines which trust profile credentials
are necessary to release the requested resource to Dr.
Jane and the release actions it must perform. The
controller identifies the four Sec objects represented
with ovals along the right side and upper left corner
of Fig. 3 that describe the credentials Dr. Jane will
need to present. These objects are: HH’s Sec
System
object that describes the credentials necessary to
access any FHIR resource from HH, the Sec
Type
object
that describes the credentials necessary to access any
Observation resource, the Sec
Resource
object that
describes the credentials necessary to access the
specific Observation, and, the Sec
Consent
object that
describes the credentials the patient requires to access
a resource they own. The Sec objects, AHPs, and RAs
represented to the right of Fig. 3 retrieved are:
Sec
System
: Current affiliation with any
healthcare provider (RA: log as high risk,
send audit notification to local auditor)
Sec
Type
: Past access to a resource of the same
type within the last year (RA: log as medium
risk, redact resource data with sensitivity: S
or higher)
Sec
Resource
: Optional: Past access to a resource
belonging to the patient within the last two
years (RA: log as low risk, audit notification
not required, no redaction required)
Sec
Consent
: Current affiliation (RA: patient
notification) or optionally: affiliation with a
listed healthcare provider
Trust Profile based Trust Negotiation for the FHIR Standard
249
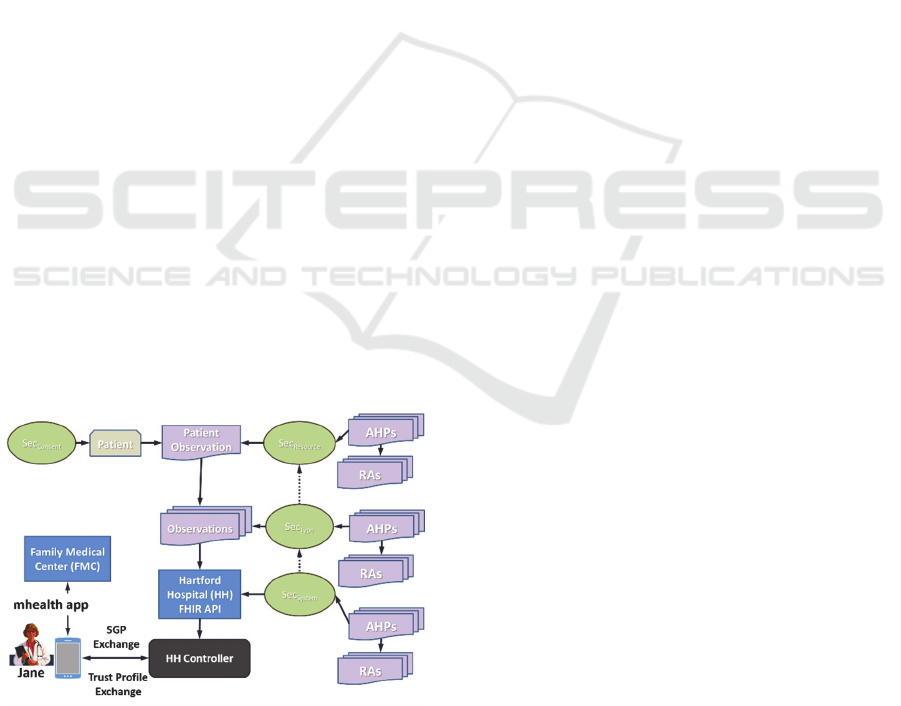
The controller matches the initial trust profile
credential, affiliation with FMC, against each of the
four Sec objects (green ovals in Fig. 3). The credential
satisfies both the Sec
System
object and the optional
Sec
Consent
requirement since the patient regularly sees
Dr. Jane at FMC. Since not all of the objects are fully
satisfied, the controller sends a server governance
policy (SGP) to Dr. Jane listing the missing AHPs.
Dr. Jane receives the request and sends a trust profile
entry describing access to one of the patient’s
Observation resources at FMC occurring three
months in the past. The controller receives this
request and matches it against each of the four Sec
objects. This new credential satisfies both the Sec
Type
and optional Sec
Resource
since the access to the
Observation resource matches both the Sec
Type
requirement of access to an Observation resource and
the Sec
Resource
requirement of access to an Observation
resource belonging to the patient, identified by a
patient ID. Having satisfied all of the credentials, the
controller processes the release actions of each Sec
object starting with Sec
System
and ending with
Sec
Consent
. Sec
Resource
’s log requirements override the
Sec
System
and Sec
Type
log requirements, logging the
access as low risk, no redaction being performed, and
overriding the audit notification requirement. The
affiliation with a listed healthcare provider AHP of
the Sec
Consent
object was the AHP that was satisfied
and carries no release action. The controller notifies
Dr. Jane that the trust negotiation was successful,
retrieves the requested Observation resource, and
generates new trust profile credentials describing Dr.
Jane’s access to the resource. The requested resource
and new credentials are sent to Dr. Jane, who can now
examine the patient’s observations from HH and add
the new credentials to her trust profile.
Figure 3: Trust negotiation example.
5 CONCLUSION AND ONGOING
RESEARCH
In this paper, we have outlined a methodology for
integrating trust profile based trust negotiation into
the FHIR environment supported by an example of its
operation in a real world healthcare scenario that
extends our prior work on trust profiles (Sanzi et al.,
2017). The methodology involves applying security
constraints for the specific resource requested by the
requestor. The security objects request access history
properties to allow access at the system level,
resource type level, individual resource level, and the
patient consent level. The trust profile credentials are
composed into a single credential expression by the
controller utilizing the requirements listed at each
level to provide a complete list of trust profile
requirements and to describe release actions for the
controller to execute to ensure a valid, secure
transaction. Combining the security objects allows
the healthcare organization operating a FHIR
installation to provide granular permissions for
accessing sensitive health data while acknowledging
the patient’s right to provide guidance towards the
dissemination of the patient’s EHR. Release actions
provide alternatives for trust profile requirements,
allowing for proper release of PHI when required.
This increased ability to share healthcare data among
providers increases patient recovery and satisfaction.
In support of our trust profile effort, we have
modified a mobile health application created in
support of a Connecticut bill (Connecticut General
Assembly, 2015) that is used for concussion
management of students in grades kindergarten
through high school by school nurses, athletic
trainers, parents, etc., to include the integrated trust
profile process as described in Section 3 with FHIR.
This mobile health application for concussion
management is integrated through the HAPI FHIR
server to the OpenEMR electronic medical record
(https://www.open-emr.org/) with the ability to take
information out of OpenEMR using its PHP API and
return observation and patient objects for the students
that have concussions. Our current research is
transitioning our model ideas in Section 3 in order to
fully realize the ability to access FHIR resources for
doing the trust management as described in Section 3
and illustrated in the healthcare example in Section 4.
DATA 2020 - 9th International Conference on Data Science, Technology and Applications
250

REFERENCES
Bell, D. E., & La Padula, L. J. (1976). Secure Computer
Systems: Unified Exposition and Multics
Interpretation. Bedford, Mass.: MITRE Corp.
Cerner. (2020, January 4). Home. Retrieved from
https://www.cerner.com/
Connecticut General Assembly. (2015). Substitute for
Raised H.B. No. 6722. Retrieved from https://www.
cga.ct.gov/asp/cgabillstatus/cgabillstatus.asp?selBillTy
pe=Bill&which_year=2015&bill_num=6722
Cooper et al. (2008, May). Internet X.509 Public Key
Infrastructure Certificate. Retrieved from
https://tools.ietf.org/html/rfc5280
De Pietro, C., & Francetic, I. (2018). E-health in
Switzerland: The laborious adoption of the federal law
on electronic health records (EHR) and health
information exchange (HIE) networks. Health Policy,
122(2), 69-74. doi:10.1016/j.healthpol.2017.11.005
Elkhodr et al. (2011). Enhancing the security of mobile
health monitoring systems through trust negotiations.
Local Computer Networks (LCN), 2011 IEEE 36th
Converence on (pp. 754-757). Bonn: IEEE.
Epic Systems Corporation. (2020, January 4). Epic.
Retrieved from https://www.epic.com/
Farrell, S., & Housley, R. (2002, April). An Internet
Attribute Certificate Profile for Authorization.
Retrieved from The Internet Engineering Task Force
(IETF®): https://www.ietf.org/rfc/rfc3281.txt
Ferraiolo et al. (2001). Proposed NIST standard for role-
based access control. ACM Transactions on Informa-
tion and System Security (TISSEC), 4(3), 224–274.
HAPI FHIR. (2016). Server Interceptors. Retrieved
January 10 2020, from https://web.archive.org/web/
20190512185820/http://hapifhir.io/doc_rest_server_int
erceptor.html
HAPI FHIR. (2020). HAPI FHIR - The Open Source FHIR
API for Java. Retrieved January 10, 2020, from
https://hapifhir.io/
Health Level 7 International. (2013). Confidentiality.
Retrieved January 19, 2020, from http://www.
hl7.org/documentcenter/public/standards/vocabulary/v
ocabulary_tables/infrastructure/vocabulary/Confidenti
ality.html
Health Level Seven International. (2013). Unique ID, R1 -
3. HCS Guide Final 2013 0322 JMD.pdf. Retrieved
January 16, 2020, from https://www.hl7.org/document
center/public/wg/secure/3.%20HCS%20Guide%20Fin
al%202013%200322%20JMD.pdf
HL7 International. (2019, January 4). Health Level Seven
International. Retrieved from https://www.hl7.org/
HL7 International. (2019, November 1). Resourcelist -
FHIR v4.0.1. Retrieved January 19, 2020, from
https://www.hl7.org/fhir/resourcelist.html
HL7 International. (2020). Index - FHIR v4.0.1. Retrieved
January 10, 2020, from http://hl7.org/fhir/
Li, J., & Li, N. (2006, Oct.-Dec.). OACerts: Oblivious
Attribute Certificates. IEEE Transactions on
Dependable and Secure Computing, 3(4), 340-352.
Posnack, S., & Barker, W. (2018, October 1). Health IT
Buzz. Retrieved January 4, 2019, from https://www.
healthit.gov/buzz-blog/interoperability/heat-wave-the-
u-s-is-poised-to-catch-fhir-in-2019
Ryutov et al. (2005). Adaptive Trust Negotiation and
Access Control. SACMAT '05 Proceedings of the tenth
ACM symposium on Access control models and
technologies (pp. 139-146). New York City: ACM New
York, NY, USA ©2005.
Sanzi et al. (2017). Integrating Trust Profiles, Trust
Negotiation, and Attribute Based Access Control. 2017
5th IEEE International Conference on Mobile Cloud
Computing, Services, and Engineering (MobileCloud)
(pp. 177-184). San Francisco: IEEE. doi:10.1109/
MobileCloud.2017.30
Sanzi et al. (November 2016). Trust Profiling to Enable
Adaptive Trust Negotiation in Mobile Devices. In S.
Mukherja (Ed.), Mobile Application Development,
Usability, and Security (pp. 95-116). IGI Global.
Sanzi, E., & Demurjian, S. (May 2016). Identification and
Adaptive Trust Negotiation in Interconnected Systems.
In A. Malik, A. Anjum, & B. Raza (Eds.), Innovative
Solutions for Access Control Management (pp. 33-65).
IGI Global.
The Office of the National Coordinator for Health
Information Technology. (2018, September 19).
Meaningful Consent Overview | HealthIT.gov.
Retrieved January 24, 2020, from https://www.
healthit.gov/topic/meaningful-consent-overview
The Office of the National Coordinator for Health
Information Technology. (2019, April 17). Patient
Consent for Electronic Health Information Exchange |
HealthIT.gov. Retrieved January 24, 2020, from
https://www.healthit.gov/topic/patient-consent-
electronic-health-information-exchange
U.S. Department of Veterans Affairs - Office of Public and
Intergovernmental Affairs. (2019, July 29). VA
achieves critical milestone in its Electronic Health
Record Modernization Program. Retrieved January 4,
2020, from https://www.va.gov/opa/pressrel/press
release.cfm?id=5286
Vawdrey et al. (2003). Trust Negotiation for Authentication
and Authorization in Healthcare Information Systems.
Engineering in Medicine and Biology Society, 2003.
Proceedings of the 25th Annual International
Conference of the IEEE (pp. 1406-1409). IEEE.
Winsborough et al. (2000). Automated trust negotiation.
DARPA Information Survivability Conference and
Exposition, 2000. DISCEX '00. Proceedings. 1, pp. 88
- 102. Hilton Head, SC: IEEE. doi:10.1109/
DISCEX.2000.824965
Yasnoff, W. A. (2015). A Feasible and Sustainable
Approach to Health Information Infrastructure Via
Mobile Devices. Retrieved Oct. 23, 2015, from
http://mediasite.uchc.edu/mediasite41/Play/b409b6fea
70b4ec5b3fc34355340ac521d
Trust Profile based Trust Negotiation for the FHIR Standard
251
