
Digital Innovation in Outpatient Healthcare Delivery Services:
A Common Methodology to Introduce IoT Technologies in Two Use-cases
Salom
´
e Azevedo
1,2 a
and Ana Rita Londral
1 b
1
Value for Health CoLAB, NOVA Medical School, Lisbon, Portugal
2
Department of Engineering and Management, Instituto Superior T
´
ecnico, Lisbon, Portugal
Keywords:
eHealth, Healthcare Pathways, Outpatient, IoT, Patient-centered Design.
Abstract:
The introduction of digital innovation in established healthcare pathways needs collaborative work among
technology providers and clinical teams. Further, the involvement of patients is a key-factor as a highly-impact
resource in the design of effective services and sustainable innovation in Healthcare. This paper presents two
use-cases where a common methodology is being applied in two different hospitals, to digitize outpatient
healthcare pathways using IoT technologies for remote monitoring patients at home. The methodology is
driven by principles of user-centered design and focused on outpatient outcomes measurement. It is described
in three steps: ”as-is” process design, process mapping for the new service and deployment strategy. From
context requirements to results evaluation, clinical teams and patients are actively involved in the service
design.
1 INTRODUCTION
In the last decades, the development of digital tech-
nology innovations brought unprecedented opportuni-
ties to outpatient healthcare delivery and to empower
citizens in managing their own health. Sensors, mo-
bile devices, Internet connection and artificial intelli-
gence algorithms have become more accessible to the
Healthcare systems and to the citizens, and have enor-
mous potential in reducing inpatient costs that have
been continuously increasing, worldwide. However,
these technologies are still a remote reality for most
of the healthcare delivery processes. Among the main
identified reasons for this slow adoption are factors
that influence the acceptance of these technologies
and resistance by medical staff and patients. From
previous research, it is known that the strategy used
for managing change is a key indicator of success or
failure (Safi et al., 2018). Interestingly, recent stud-
ies indicate that the role of patients (demand-side) is
limited and that the healthcare providers (supply side)
play a more important role in driving variation and
growth of healthcare utilization and expenditure in ad-
vanced economies (Kr
¨
amer and Schrey
¨
ogg, 2019). If
that is the case, a shift from a single-disciplinary ap-
a
https://orcid.org/0000-0003-1234-9464
b
https://orcid.org/0000-0002-8002-6790
proach to a multidisciplinary collaboration, that tack-
les real-world medical challenges and considers the
main expectations, capabilities and priorities of pa-
tients and clinical teams, is needed for scaling-up
digital innovations in Healthcare (Kostkova, 2015)
(Spanakis et al., 2016) (Garavand et al., 2016).
In this paper, we present the methodology em-
ployed in two different healthcare services for the
real-time deployment of IoT technologies in outpa-
tient healthcare pathways: (i) follow-up of patients in
the 1st month post-surgery, from the Cardiothoracic
service in a Portuguese public hospital; and (ii) moni-
toring elderly patients that are enrolled in a Homecare
nursing program, delivered by a Portuguese private
hospital. Both use-cases that are reported in this pa-
per are being deployed in real contexts of healthcare
services and include the collaboration of patients and
clinical teams with technology developers, to incor-
porate the IoT technology in the already established
healthcare pathways.
We describe a patient-centered methodology that
is being proposed to evaluate the value of a new ser-
vice for outpatient healthcare with the use of IoT
devices to collect and monitor clinical and patient-
reported outcomes. This work follows the framework
of Value-Based Healthcare, with a focus on the col-
lection of patient-centered outcomes during the out-
patient period (
˚
Akerman and Stowell, 2015).
Azevedo, S. and Londral, A.
Digital Innovation in Outpatient Healthcare Delivery Services: A Common Methodology to Introduce IoT Technologies in Two Use-cases.
DOI: 10.5220/0009394908210826
In Proceedings of the 13th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2020) - Volume 5: HEALTHINF, pages 821-826
ISBN: 978-989-758-398-8; ISSN: 2184-4305
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
821

2 USE CASES
This paper describes the implementation of a service
for outpatient outcomes monitoring in two different
hospital contexts:
2.1 Follow-up Service in Cardiothoracic
Surgery Service in a Public Hospital
A pilot is running to monitor patients from home,
in the first month after cardiothoracic surgery. The
main objective of this telemonitoring service is to
early detect complications and increase patients ex-
perience of safety. Clinical and patient-reported out-
comes are collected daily by the patient and reported
to the clinical staff that contacts the patient in case
of an alarm event is detected. After running a pilot
with two patients that were exposed to cardiothoracic
surgery, the technology and process design were ad-
justed, based on patients and clinical staff feedback.
The pilot moved now to its second-stage: to follow-
up 80 randomly selected patients that are discharged
in this service.
Outcomes that are collected are: blood pressure,
weight, steps, 5 questions in a mobile app and a self-
picture of the surgical wound.
2.2 Homecare Nursing Service for
Elderly Population in a Private
Hospital
This use case relates to the implementation of a pi-
lot from an European project H2020-ACTIVAGE. A
group of 50 elderly patients (age over 65 years old)
and their caregivers, followed in a homecare nursing
service, were selected to use IoT devices to remotely
monitor outcomes and communicate these with the
nursing team. At current stage, the requirements and
process design were already defined to start the pilot.
Outcomes that will be collected are: glucose level,
blood pressure, weight, steps and simple patient-
reported outcomes that are answered through a mobile
app.
3 METHODOLOGY
As both services were deployed in two real-life pi-
lot sites, we followed a case study approach in order
to identify technical, organizational, and sustainabil-
ity perils and to collect the generated knowledge dur-
ing the deployment of the services, according to (Yin,
1994).
In the healthcare context, the process of creat-
ing or re-engineering a healthcare service that meets
the several needs from the different stakeholders in-
volved poses a high risk in guaranteeing that the end-
user (the patient) is the main beneficiary of the ser-
vice. Therefore, we applied the User-centred design
(UCD) methodology to achieve higher levels of ef-
fectiveness, efficiency, and satisfaction (Dabbs et al.,
2009;
˚
Arsand et al., 2008). Some key principles
of UCD were applied, such as an iterative and in-
cremental development process, involvement of end-
users, explained design options, real life context eval-
uation and effective multidisciplinary teams develop-
ment process (Gulliksen et al., 2003).
The UCD process was divided in three main
stages:
1. Environment Analysis: Documentary analysis
to collect the information about the as-is situa-
tion of outpatient services in both hospitals. This
stage comprised several activities, such as: iden-
tification of stakeholder groups profiles, their mo-
tivations and needs, their interests, influence and
importance.
2. Digitizing the Healthcare Outpatient Pathway:
The following step consisted in transforming
stakeholders’ needs into requirements. Firstly,
the real needs and the perceived and expressed
needs were identified through semi-structured in-
terviews. Secondly, the listed requirements were
analysed and negotiated. In this negotiation stage,
for each requirement it was discussed the feasibil-
ity to meet the need, regarding time and complex-
ity, and available resources.
3. Deployment Strategy: In both case studies, we
applied the same deployment strategy. Due to the
lack of literature found in discussion of deploy-
ment effects of health-related IoT-based technol-
ogy in real-life settings, this paper reports the ac-
tivities supporting the implementation of the new
outpatient care services.
4 SERVICE DESIGN OF
OUTPATIENT HEALTHCARE
Digitizing the outpatient healthcare pathway is only
possible through collaborative and multidisciplinary
work, where the assessment of the community and its
members experience plays a crucial role in the adop-
tion and evaluation of a new project or program (Eu-
ropean Commission, 1993) (Vermeulen et al., 2014).
This approach was used to enhance participation and
Scale-IT-up 2020 - Workshop on Best Practices for Scaling-Up Digital Innovations in Healthcare
822
transparency through a logically ordered series of ac-
tions designed to solve problems previously identified
by the involved stakeholders.
The role of the patient in product innovation and
development process has been neglected for most
of the healthcare industry life cycle (Garrido et al.,
2016). However, in the last years, a lot of effort from
academia and patient’s advocates has been conducted
to use the patient as a highly-impact resource in the
design of effective products and services in the health-
care sector. The UCD methodologies are validated
tools to cope with this lapse and empower patients
and their caregivers to be part of this development.
In the context of both use cases described in this pa-
per, the two main characteristics (among the others)
of this systematic methodology are: (i) the participa-
tion of patients, caregivers and the clinical team in the
digitization of the outpatient pathway and (ii) the seek
of consensus among technology providers, healthcare
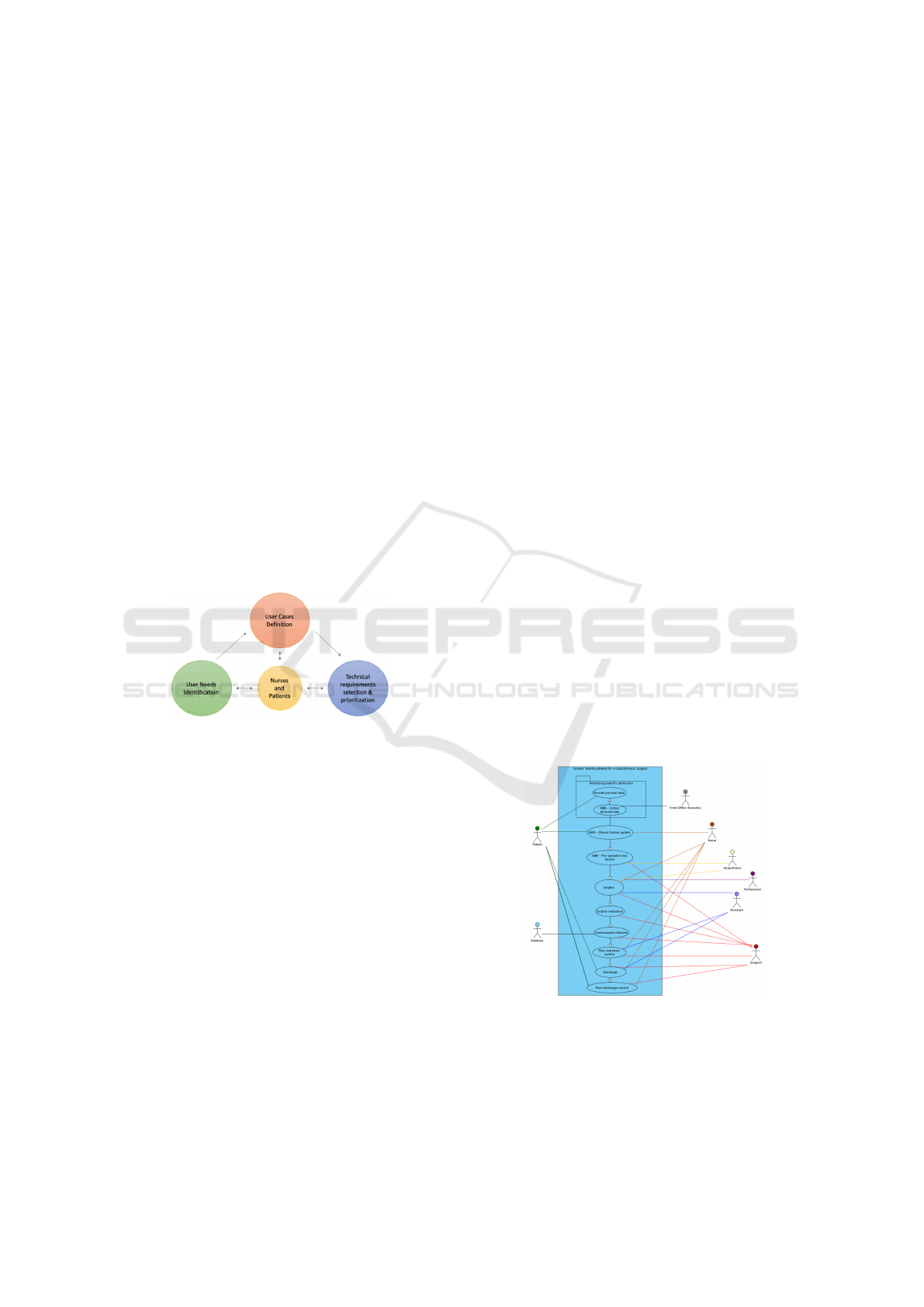
providers and the patients. Figure 1 illustrates the co-
creation framework that was used for this work.
In this section, we briefly describe the three steps
that were developed to implement the deployment
strategy.
Figure 1: The co-creation framework used for the digital
innovation in outpatient healthcare services.
4.1 Step 1: Design the Process as-is
We first selected the following tools to collect enough
information to report the technical requirements:
1. Environmental Analysis through Semi-
structured Individual Interviews. With the
goal of understanding the context of both home
care delivery initiatives, we conducted several
interviews to different stakeholders in order to
understand their needs and motivations, their
relevance and importance in the definition of
the outpatient pathway. The main relevant
stakeholders identified were: assisted persons
(patients), formal caregivers (individuals hired
by the assisted persons to provide assistance at
home), informal caregivers (patient’s relatives),
healthcare professionals (nurses and surgeons),
healthcare providers (hospitals), technology
providers (organizations that develop and pro-
vide solutions), technology transfer supporter
(organizations/institutions that guarantee that
the technological intervention adds value to the
healthcare service, satisfies the most relevant
needs of the different stakeholders, and is cost-
effective). The group profiles were described by
identifying the motivations, goals, and benefits
with the proposed new system. According to
the impact that the solution could have for the
each stakeholder, we classified each in terms of
importance and influence.
2. Previous Experience Analysis through Struc-
tured Individual Interviews. For the most rel-
evant stakeholders identified for each of the use-
cases, we investigated on previous experiences
with technology in their practices (advantages,
disadvantages and opportunities). To gather quali-
tative insights about operational opportunities and
constraints, we interviewed different representa-
tives from each stakeholder group about their atti-
tudes, believes and values of the proposed project.
3. Use Case Scenarios Definition from Visits to
the Real Life Context. To avoid conflicts in de-
sign due to lack of accountability of real-life con-
straints of the system and its actors, the team vis-
ited both hospitals, talked to patients and visited
some homes. The visit to the hospitals enabled
the understanding of the environment in which
the healthcare professionals provide care and how
the interaction with patients occurs. The visit to
patients’ homes enabled the understanding of the
context of how nurses provide care outside hospi-
tal facilities.
Figure 2: Use Case Diagram to identify, clarify, and orga-
nize system requirements.
4. Process Characterization. The output from pre-
vious steps enabled us to create the model of the
current process (”as-is”-model) following existing
best-practice solutions (Im et al., 1997). Visual
Digital Innovation in Outpatient Healthcare Delivery Services: A Common Methodology to Introduce IoT Technologies in Two Use-cases
823
Paradigm software was used to characterize each
step/operation and its dependencies with the rest
of the environment. For each operation, infor-
mation regarding resources, time, cost and clin-
ical constraints was provided by the healthcare
provider and its professionals. Through meeting
with nurses and surgeons several iterations to the
as-is model took place until a consensus to the fi-
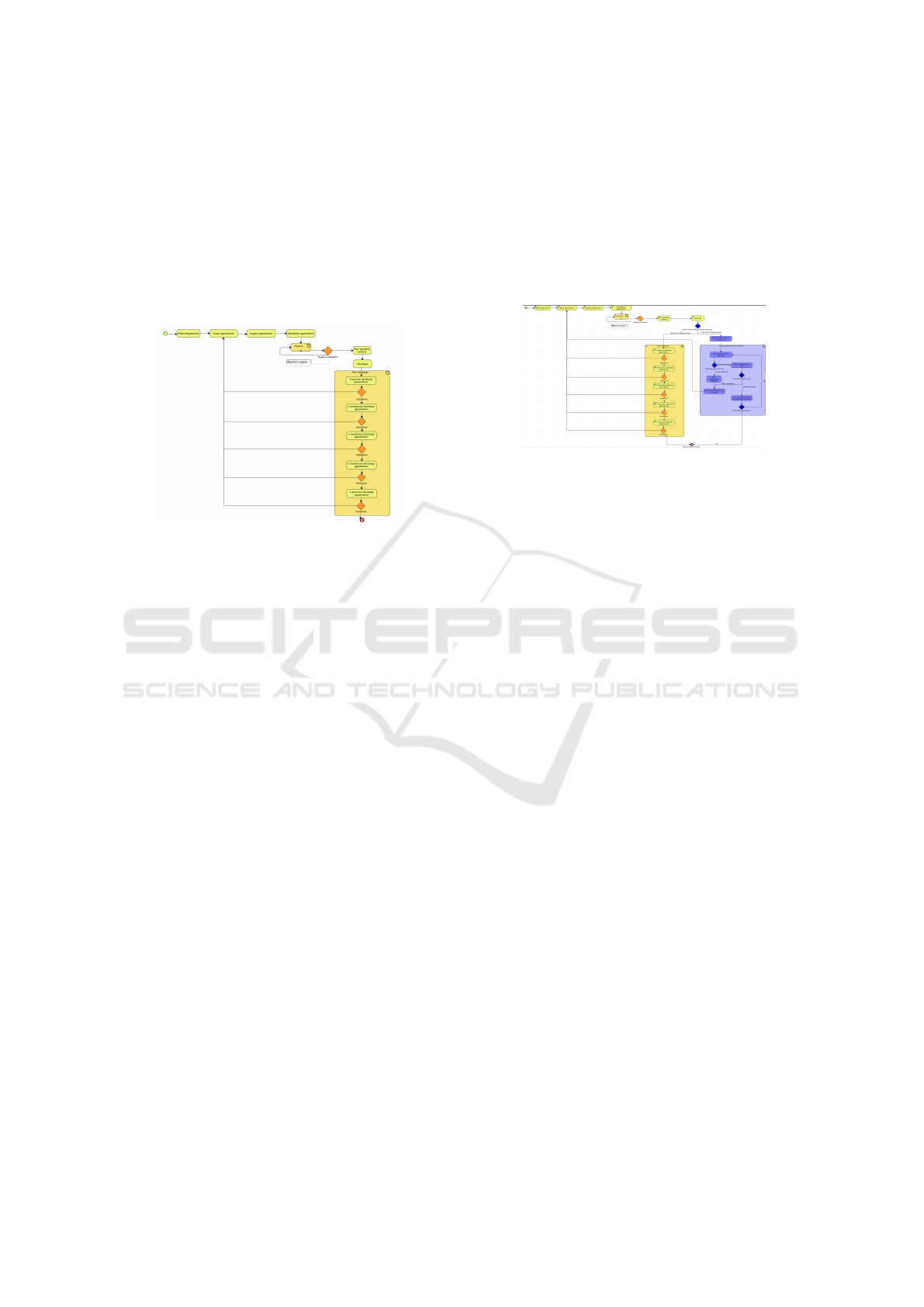
nal process was achieved (Figure 3).
Figure 3: Mapped process of the health pathway of a patient
submitted to cardio-thoracic surgery.
4.2 Step 2: Mapping the Process with a
Focus on Patient-centered Care
The design of the technological solution to be inte-
grated in both home care delivery initiatives was de-
veloped with the contributions from both demand and
supply side were involved. To reach a consensus
in the prioritization of the needs to be coped by the
new system we conducted a focus group with clinical
teams. We presented the general process to the stake-
holders in individual meetings and identified oppor-
tunities to integrate technology that would cope with
the experienced needs.
Transforming the perceived and expressed needs
into retained and specified needs, we conducted sev-
eral meeting to negotiate the requirements that could
be solved by the service and technology proposed, re-
spect the time and the resources available. The list of
requirements was validated by all stakeholders. Five
different types of requirements were identified: func-
tional, security, usability and humanity, maintainabil-
ity and support, and performance. The stakeholders’
list and the real needs identified were used to summa-
rize and describe the different scenarios underlying
the outpatient pathway (Table 1).
The main focus of the ”to-be”-model (Figure 4)
was to enhance the performance of home care service
by improving the patient engagement and experience,
and by informing healthcare professionals with rele-
vant, real-time data on patient’s recovery, health sta-
tus, and quality of life. For this goal, we also worked
on the outcomes reports to provide this information
in an appropriate format so patients and caregivers
get more engaged in the follow-up and recovery pro-
cess. Reporting design is an important issue related to
human-computer interaction that directly affects ac-
ceptance and engagement of both patients and health-
care providers.
Figure 4: Mapped process of the health pathway of a pa-
tient submitted to cardio-thoracic surgery and opportunities
to use IoT-based health-related devices.
4.3 Step 3: Deployment of IoT-based
Technology to Monitor Outpatient
Pathway
The use cases created are being implemented in a pilot
to validate the described methodology. In order to be
able to test the level of adoption of the ”to-be”-model
of outpatient, we selected devices with high usabil-
ity concerns and taking into account the requirements
previously defined. A monitoring web platform al-
lows to control users’ engagement, operational data-
related problems and the outcomes collected by each
monitored patient.
The deployment strategy that is being imple-
mented is iterative: we started to monitor a single pa-
tient with good level of digital literacy for one month,
then incorporated lessons learned and we are now fol-
lowing a group of five randomly selected patients, be-
fore widely running the pilot.
In the cardiothoracic surgery use case, at the day
of discharge from hospital, patients receive instruc-
tions to use the IoT-based kit. For 30 days, the pa-
tient is instructed to follow the same procedure ev-
ery morning: use a mobile app to follow the tasks of
weighting, measuring blood pressure, taking a picture
of the surgical wound, and answering five questions
regarding patient reported outcomes. A report with
the collected outcomes from the patient is digitally
sent to the clinical team who contacts the patient in
case of any abnormality detection.
For the referred first patient, a weekly con-
tact/meeting with nurses and surgeons was followed
to refine the process. After 1 month, the patient re-
Scale-IT-up 2020 - Workshop on Best Practices for Scaling-Up Digital Innovations in Healthcare
824
Table 1: Use Case Scenarios selected for the private Home-
care Nurse Service.
Use Case Scenarios List
Title Description
Daily
activity
monitor-
ing
Nurse needs to monitor activities of
the person’s daily living, such as walk-
ing speed, mobility function, number of
falls and/or risk of fall, fine motor con-
trol, measure hand grip strength, callig-
raphy assessment, ability to speak, and
speech articulation. The nurse evalu-
ates these outcomes when he/she vis-
its the patient. In order to have a
more accurate evaluation of the out-
comes, the nurse asks each stakeholder
(informal and/or formal caregiver and
patient) this information, at different
times throughout the clinical appoint-
ment. Patients usually do not have the
right perception of their level of mobil-
ity function or risk of fall.
Health
parameter
monitor-
ing
Caregivers and patients are told to
register daily different health parame-
ters: blood pressure, pulse/heart rate,
temperature, pain level, weight, gly-
caemia and skin status for preven-
tion and follow-up of disease compli-
cations. When nurse visits the pa-
tient, he/she asks for the records regis-
tered by the informal/formal caregivers
and repeats the record of the patients’
health parameters to validate. When
appropriate, the nurse also takes a pic-
ture of the wound status to have a better
perception of the wound recovery pro-
gression.
Notification
of abnor-
mal
situation
Formal and informal caregivers notice
an abnormal activity, including health
parameters monitored that are outside
of normal range and low activity per-
ceived. They contact nurses and report
the situation. When this happens the
Nurse-Chief makes more questions to
better understand the situation and al-
locates an urgent visit from a nurse to
the patient’s house.
turned to the hospital and delivered the equipment.
System Usability Scale (Martins et al., 2015) and
semi-structured interviews to the patient and nurses
were used to test acceptance and optimize the out-
comes reporting tools.
5 DISCUSSION AND
CONCLUSIONS
In this paper, we propose a methodology to design
outpatient healthcare services, by deployment of IoT
technologies. Due to increasing Elderly population
demands in the Healthcare systems and the increased
treatment options, the sustainability of Healthcare is
threatened in the advanced economies. Digital inno-
vation brings opportunities to empower patients to ac-
tively participate in the process of care, to engage in
the process of collecting and reporting outcomes, in
order to prevent healthcare complications that repre-
sent a burden to the Health systems. These opportuni-
ties are being exploited in various studies focused ei-
ther in technology development and clinical services
(Acheampong and Vimarlund, 2016).
The methodology that we present is based on
UCD and takes into account the real-time imple-
mentation of digital innovation, i.e. a new process
is mapped to be successfully integrated in the ex-
istent running process. This work compares with
other recently published studies (e.g. (Hobson et al.,
2018) (Backman et al., 2018), in the way that the
methodology presented brings an innovative perspec-
tive process mapping and service design that is cen-
tered on the patient and its outcomes collection points
and not on hospital resources or technology design.
This patient-outcomes perspective aims at develop-
ing tools to implement value-based healthcare frame-
works considering the real-life challenges.
The two use-cases described are actually running.
Results from the pilots will be published in future
work. Costs driven from this digital innovation will be
integrated in the overall outcomes analysis, as an im-
portant part for the study of scaling-up requirements.
ACKNOWLEDGEMENTS
The devices and 4G transmission for the pilot in Hos-
pital de Santa Marta (Lisbon, Portugal) was supported
by Fraunhofer Portugal and Vodafone Portugal. The
pilot in the CUF Infante Santo hospital (Lisbon, Por-
tugal) was supported by EU project H2020 ACTI-
VAGE ID732679.
REFERENCES
Acheampong, F. and Vimarlund, V. (2016). Innovating
healthcare through remote monitoring: Effects and
business model. International Journal of Information
System Modeling and Design (IJISMD), 7(1):49–66.
Digital Innovation in Outpatient Healthcare Delivery Services: A Common Methodology to Introduce IoT Technologies in Two Use-cases
825

˚
Akerman, C. and Stowell, C. (2015). Measuring outcomes:
the key to value-based health care. Harvard Business
Webinar.
˚
Arsand, E., Tufano, J. T., Ralston, J. D., and Hjortdahl, P.
(2008). Designing mobile dietary management sup-
port technologies for people with diabetes. Journal of
telemedicine and telecare, 14(7):329–332.
Backman, C., Harley, A., Peyton, L., Kuziemsky, C., Mer-
cer, J., Monahan, M. A., Schmidt, S., Singh, H., and
Gravelle, D. (2018). Development of a path to home
mobile app for the geriatric rehabilitation program at
bruy
`
ere continuing care: Protocol for user-centered
design and feasibility testing studies. JMIR research
protocols, 7(9):e11031.
Dabbs, A. D. V., Myers, B. A., Mc Curry, K. R., Dunbar-
Jacob, J., Hawkins, R. P., Begey, A., and Dew, M. A.
(2009). User-centered design and interactive health
technologies for patients. Computers, informatics,
nursing: CIN, 27(3):175.
European Commission, E. (1993). Cycle Management: In-
tegrated approach and logical framework. Technical
report, European Commission, Brussels.
Garavand, A., Mohseni, M., Asadi, H., Etemadi, M.,
Moradi-Joo, M., and Moosavi, A. (2016). Factors
influencing the adoption of health information tech-
nologies: a systematic review. Electronic physician,
8(8):2713.
Garrido, T., Raymond, B., and Wheatley, B. (2016).
Lessons from more than a decade in patient portals.
Health Affairs Blog, 2016.
Gulliksen, J., G
¨
oransson, B., Boivie, I., Blomkvist, S., Pers-
son, J., and
˚
Asa Cajander (2003). Key principles for
user-centred systems design. Behaviour & Informa-
tion Technology, 22(6):397–409.
Hobson, E. V., Baird, W. O., Partridge, R., Cooper, C. L.,
Mawson, S., Quinn, A., Shaw, P. J., Walsh, T., Wol-
stenholme, D., and Mcdermott, C. J. (2018). The
tim system: developing a novel telehealth service
to improve access to specialist care in motor neu-
rone disease using user-centered design. Amyotrophic
Lateral Sclerosis and Frontotemporal Degeneration,
19(5-6):351–361.
Im, I., El Sawy, O., and Hars, A. (1997). Business process
reengineering: Do software tools matter.
Kostkova, P. (2015). Grand challenges in digital health.
Frontiers in Public Health, 3:134.
Kr
¨
amer, J. and Schrey
¨
ogg, J. (2019). Demand-side deter-
minants of rising hospital admissions in germany: the
role of ageing. The European Journal of Health Eco-
nomics, pages 1–14.
Martins, A. I., Rosa, A. F., Queir
´
os, A., Silva, A., and
Rocha, N. P. (2015). European portuguese validation
of the system usability scale (sus). Procedia Computer
Science, 67:293–300.
Safi, S., Thiessen, T., and Schmailzl, K. J. (2018). Ac-
ceptance and resistance of new digital technologies
in medicine: Qualitative study. JMIR Res Protoc,
7(12):e11072.
Spanakis, E. G., Santana, S., Tsiknakis, M., Marias, K.,
Sakkalis, V., Teixeira, A., Janssen, J. H., de Jong,
H., and Tziraki, C. (2016). Technology-based inno-
vations to foster personalized healthy lifestyles and
well-being: A targeted review. J Med Internet Res,
18(6):e128.
Vermeulen, J., Verwey, R., Hochstenbach, L. M., van der
Weegen, S., Man, Y. P., and de Witte, L. P. (2014).
Experiences of multidisciplinary development team
members during user-centered design of telecare
products and services: A qualitative study. J Med In-
ternet Res, 16(5):e124.
Yin, R. K. (1994). Discovering the future of the case study.
method in evaluation research. Evaluation practice,
15(3):283–290.
Scale-IT-up 2020 - Workshop on Best Practices for Scaling-Up Digital Innovations in Healthcare
826
