
Xtrace: Novel Bioresorbable Device for Patent Foramen Ovale
Closure
Sara Abu Ajamieh
1
, Diana Mindroc-Filimon
2
, Irene Mozo
3
and Isabel Rocha
4
1
Karolinska Institutet, Stockholm, Sweden
2
German Cancer Research Center, Heidelberg, Germany
3
Faculty of Physics, University of Barcelona, Barcelona, Spain
4
Santa Maria Hospital, Lisbon, Portugal
Keywords: Patent Foramen Ovale, Cryptogenic Stroke, PFO Closure, Bioabsorbable Occluder.
Abstract: Patent foramen ovale (PFO) is a congenital cardiac lesion, affecting about 25% to 30% of the adult
population. It is associated with several serious complications, including cryptogenic strokes, transient
ischemic attacks, and migraine. The prevalence of PFO has significantly increased in patients with
cryptogenic stroke; up to 40% of ischemic strokes with an unknown cause have a PFO. Recently, technical
advancements in medical engineering have made the percutaneous transcatheter closure of PFO a feasible
treatment option. However, current PFO closure devices may lead to complications such as the need for
replacing the device after several years, sudden migration of the implant, erosion, infection, or arrhythmias.
Attempts are needed to produce a safer and more effective closure devices. Here, we propose an innovative
medical device called Xtrace. It consists of a biodegradable material that will be partially degraded by the
host body while substituted by autologous host tissue. This innovative device will potentially fulfill the
essential unmet clinical need, as well as provide a safe and effective delivery of therapy for the general
population.
1 INTRODUCTION
The foramen ovale is a compulsory channel between
the two atria during fetal development. It provides
placental oxygenated blood to reach the arterial
circulation of the fetus. Naturally, the hole is
completely sealed at birth, as it can be seen in Figure
1. However, closure does not occur for approximately
a quarter of the general population (Hagen, 1984).
This is due to a defect in the postnatal fusion of the
septum primum and secundum, forming tunnel-like
gap called patent foramen ovale (PFO). Although the
reason behind PFO is unknown, studies suggest that
it may be genetic. PFO has been implicated in several
serious complications, including cryptogenic strokes,
transient ischemic attacks, and migraine. The primary
cause of stroke is still unknown in about 40% of
patients with a stroke diagnosis (Giblett, 2019). The
occurrence of a PFO with either transient or
continuous right to left shunt can potentially lead to
paradoxical embolism (Belkin, 1990). Over the past
three decades, technical advancements in medical
engineering have made the percutaneous
transcatheter closure of PFO a feasible treatment
option. Several percutaneous PFO closure devices
have various advantages and are expected to work
equally well if placed in their most suitable anatomy
(Ko, 2010). However, PFO closure devices may lead
to some complications such as the need for replacing
the device after several years, sudden migration of the
implant, erosion, infection, thrombogenicity, or
arrhythmias. Attempts to produce safer and more
effective closure devices are underway.
Figure 1: Representation image of a human heart. (A)
Normal heart with a closed foramen ovale. (B) Heart with
an open foramen ovale.
344
Ajamieh, S., Mindroc-Filimon, D., Mozo, I. and Rocha, I.
Xtrace: Novel Bioresorbable Device for Patent Foramen Ovale Closure.
DOI: 10.5220/0009374603440349
In Proceedings of the 13th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2020) - Volume 1: BIODEVICES, pages 344-349
ISBN: 978-989-758-398-8; ISSN: 2184-4305
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
2 STATE OF THE ART
Currently, there are different varieties of therapeutic
approaches that can be adopted for the treatment of PFO.
2.1 Pharmacological Treatment
Anticoagulant or antiplatelet therapies can be used to
treat PFO. However, drug treatment is only
symptomatic, and may be contraindicated in some
cases and requires life lasting engagement. Cross-
sectional multicenter studies have shown that PFO
closure is associated with a significant risk reduction
when compared with pharmacological treatment
(Saver, 2017).
2.2 Implantation of Occluders
Percutaneous PFO closure procedures have been
originated from well-established atrial septal defect
(ASD) closure techniques. In experienced centers,
this is a very low-risk procedure that can be carried
out in a short time (Meier, 2005). Therefore,
catheterization laboratories worldwide have seen a
substantial rise in the number of trans-catheter PFO
closures being performed (Opotowsky, 2008). In
some practices, a submissive sizing balloon together
with periprocedural echocardiographic guidance
(either trans-esophageal or intra- cardiac) is used in
patients during PFO device closure (Ko, 2010). From
the design features perspective, several types of
devices can be distinguished:
Self Expanding Double Disk Occluders: These
devices consist of commonly used PFO closure
devices; they include two metallic opposing discs
covered by fabric and attached by a thin waist. A
combination of oppositional mechanical forces
formed by the 2 opposing discs and fibrous tissue
encapsulation seal the PFO. The GORE
R
CARDIOFORM Septal Occluder and the Abbott
Amplatzer
TM
PFO Occluder, both using a nitinol
framework, are the only devices of this nature
currently permitted by the US Food and Drug
Administration (FDA) for PFO closure in the United
States.
Occluders with PFO Tunnel: These devices are
placed on the PFO tunnel and stabilized by adjustable
atrial anchors. This technique brings the septum
primum and secundum in close apposition, reducing
the amount of material exposed to blood circulation.
The Coherex FlatStent
TM
occluder (Coherex Medical,
Inc) is the most popular device of this family.
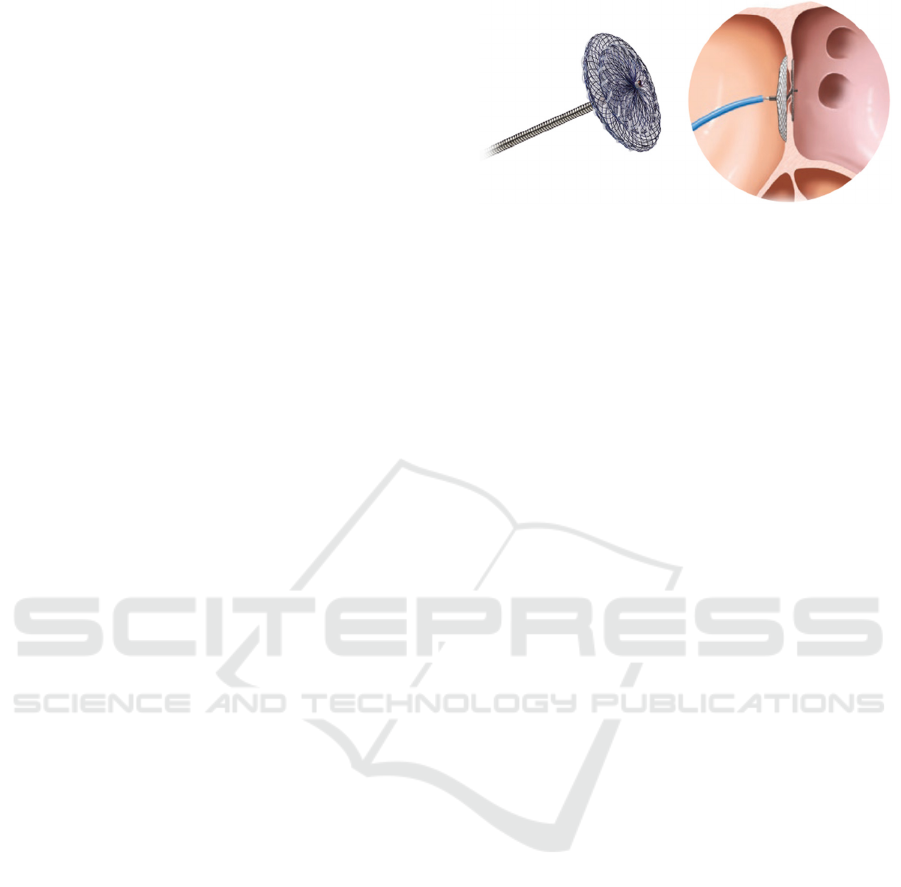
Figure 2: Amplatzer device and respective intervention.
(Amplatzer, 2019).
Bioabsorbable PFO Occluders: Bioabsorbable
occluders follow the same deploying technique as
metallic occluders. However, they substitute the
metallic material constituting the disk with resorbable
polymers, which are expected to be replaced by native
tissue upon reabsorption. The risk of thrombosis is
reduced, as well as arrhythmia and device migration.
However, bioabsorbable devices are still ongoing
clinical evaluation phases
HeartStitch
R
Occluder (Sutura, Inc): The
HeartStitch occluder utilizes complex suture
technology to seal the septum primum and secundum.
However, this technique requires greater surgeon
proficiency and is still not available for clinical use.
The current solutions present a series of
disadvantages. The pharmacological treatment
represents just a symptomatic solution and does not
actually solve the problem. On the other hand, the
metallic disk occluders can be refused by the patient’s
body, cause inflammation, migrate from the foramen
ovale or require a replacement after a specific time.
Plus, these devices are composed of metallic
materials, and can cause long term inflammatory
response as well as magnetic resonance artifacts. The
bioabsorbable occluders are not available anymore,
since a higher risk of shunts was associated to their
use. Moreover, the available devices were still
leaving a metallic framework behind in the body
(Meier, 2005).
3 PROPOSAL OF THE PRODUCT
3.1 Design of the X-trace Device
The proposed device will be composed by two
opposed disks of an acellular porcine collagen type I
matrix, each of which will be supported by two arms
of the biodegradable JDBM-2 Mg alloy (Mao, 2017).
Each of the arms will account with 3 interposed
spring hinges that will serve to attach the device to the
host tissue.
Xtrace: Novel Bioresorbable Device for Patent Foramen Ovale Closure
345

3.1.1 Disks Design
The disks will be composed of porcine collagen type
I matrix. This material offers full guarantees as it has
already been used in PFO closure procedures
(Morgan, 2010). Full growth of autologous tissue has
been shown six months after implantation of this type
of collagen matrix. This suggests that the material
induces a sufficient host tissue response to repair the
size of the defect.
3.1.2 Framework Design
The framework will be composed by a Mg alloy, Mg-
2.2Nd-0.1Zn-0.4Zr, denoted JDBM-2, that has
already shown promising results upon application on
vascular stents (Morgan, 2010). Magnesium is one of
the most promising metals used on bioabsorbable
devices, as the corrosion products of Mg alloys can
be absorbed or excreted by the human metabolic
system (Staiger, 2006). Mg alloys also show excellent
anti-platelet deposition (Gu, 2009) and low
thrombogenicity (Staiger, 2006). After being exposed
to a double extrusion procedure, the JDBM-2 alloy
shows excellent mechanical properties (YS = 66 +- 3
Mpa, UTS = 181 +- 5 MPa, elongation = 10.2 +-
1.3%), which makes it a promising candidate for
cardiovascular intervention. Moreover, the treatment
applied to the JDBM-2 alloy implies a great
improvement of its corrosion properties, which are
often a problem in Mg alloys.
Classically, the galvanic corrosion rates of Mg
alloys are too high compared with those of other
metals, which derives on device failure between the
tissue has completely healed. However, the JDBM-2
alloy corrosion properties (0.37 mm/year) make it
suitable for this kind of applications, as complete
structural and mechanical integrity of stents
manufactured with this alloy has been shown after 6
months of implantation (Mao, 2017).
3.2 Delivery System and Deployment of
the Device
The delivery and deployment of the device will be
done following the same techniques and principles
used on metallic devices implantation. As usual, the
whole process will be guided through fluoroscopy
and intracardiac echocardiography (ICE), and
patients will be under general sedation. The delivery
system, based on the AMPLATZER Delivery system,
will be composed of:
Loader: Used to introduce the device intro the
catheter
Hemostasis Valve: This part accounts with an
extension tube and stopcock that controls bleeding
Delivery Sheat: Used to deliver the device itself
Dilator: Used to allow tissue penetration
Delivery Cable: This cable is used for delivery of the
device, which is screwed to the distal tip of the cable.
To hydrate the collagen disks, the device will have to
be exposed to a soaked saline solution during
approximately 5 minutes. The device will be then
collapsed and loaded into the delivery system thanks
to the loader cable. The device will be administered
together with heparin and antibiotics to prevent
coagulation and infections.
3.3 Follow-up
The follow up of the procedure will consist of
periodic transthoracic echocardiography and chest
RX at 24 hours, three months, six months, and one
year after implantation, as done with similar devices.
It is also important to perform blood marker control
in order to check for any possible complications such
as coagulation and infections.
3.4 Benefit and Concerns
The use of 100% bioabsorbable materials translate
into multiple potential benefits of our device, X-
Trace. Those include decreased long-term
thrombogenicity, lower inflammatory response,
lower erosion potential and reduced
arrhythmogenicity. Plus, as the device will be
substituted by fibrous endothelialized tissue, the risks
of lifespan and chronic mechanical stress are almost
avoided. Moreover, the X-Trace device will increase
eligibility for PFO closure treatment: until now, all
the devices being used contain metallic materials that
have a long life inside the body which are not
compatible with the treatment of atrial fibrillation
(echocardiographic ablation). The proposed device,
which does not leave any metallic residues behind,
will enhance a better treatment of comorbidities. The
most significant concern is resorption or mechanical
failure of the device before its replacement by
autologous endocardial tissue, which could lead to a
recurrent device over it.
4 RISK ANALYSIS AND
ESSENTIAL REQUIREMENTS
According to 21 CFR 860, our product classifies as
Class III Medical Product. This translates into a high
ClinMed 2020 - Special Session on Designing Future Health Innovations as Needed
346
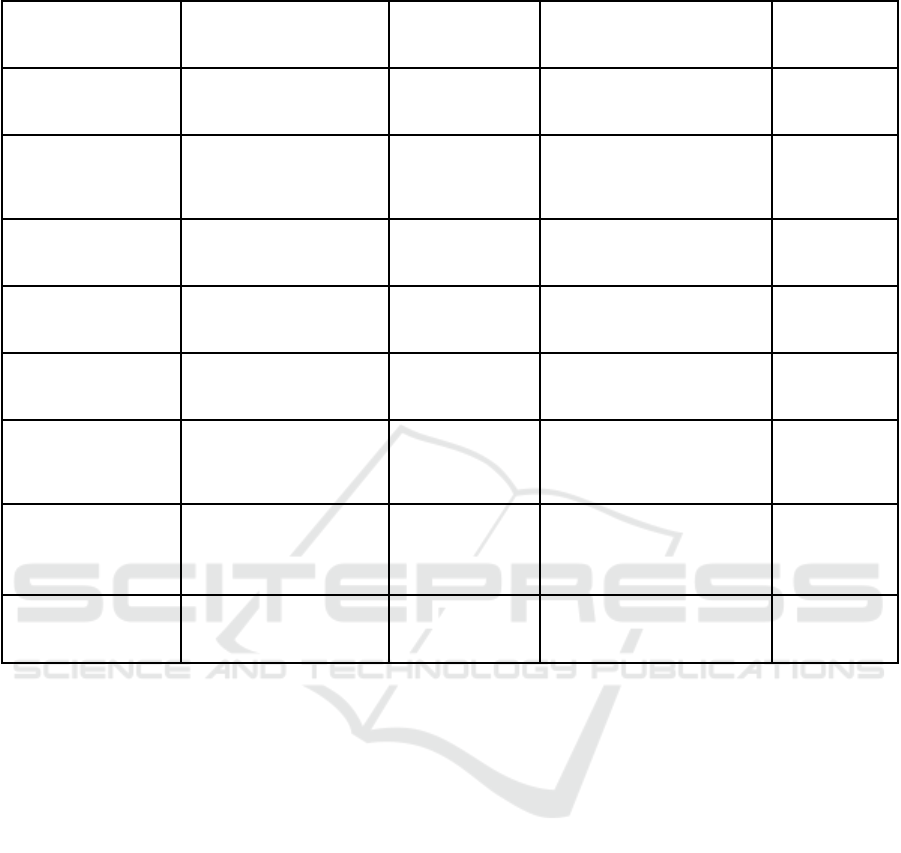
Table 1: Risk Assessment.
Hazardous situation Hazard Initial risk level Safety control measures
Final risk
level
Wrong insertion of
catheter
Bruising, damage to
artery
Acceptable
Experienced medical staff,
trainings
Acceptable
Forgetting to
assembly parts of the
intervention set
Incomplete intervention
set, necessity of removal
and reinsertion
Unacceptable
Trainings, intuitive design of
the product, warnings, clear
instructions of use
Acceptable
Use of contrast agent
for imaging
Allergic reaction Acceptable
Thorough pre-examination
of the patient record
Acceptable
Misplacement of the
product in situ
Migration of the device,
incomplete closure
Unacceptable Training, accurate imaging Acceptable
Device does not open
in situ
Tissue harm by removal
and reinsertion
Unacceptable
Testing, training, clear
instructions of use
Acceptable
Shape of collagen
matrix is
compromise
d
Tissue harm by removal
and reinsertion
Unacceptable
Testing, training, clear
instructions of use
Acceptable
Different
absorption rate of
the materials
Incomplete closure of
the ovale
Unacceptable
Thorough preclinical and
clinical trials
Acceptable
Migration of the
device
Artery, blockage,
tissue har
m
Unacceptable
Thorough preclinical and
clinical trials
Acceptable
risk medical device, which poses numerous risks and
its design requires a thorough risk analysis .Our work
follows the requirements from 21 CFR 820 in terms
of this risk analysis. Some of the identified risks are
presented in Table 1.
5 DEVELOPMENT PLAN
5.1 Timeline
The development plan will include the following
steps:
1. Initiation opportunity and risk analysis: During this
phase, the minimum requirements in terms of
mechanical properties, performance and
bioabsorbability for the device will be assessed
through literature review and advice from
professionals and key opinion leaders (KOL).
Moreover, basic financial, regulatory and legal
aspects will be evaluated, in conjunction with early
risk assessment and regulatory and clinical path.
Furthermore, a market and competence analysis will
be performed. Funding opportunities will be assessed.
2. Formulation of concept and feasibility: The initial
project plan will be elaborated and responsibilities
will be allocated to individual team members. Plus,
considering the needs and problem specification –
mechanical properties, self-deployability,
bioabsorbability, etc- and the professional’s opinion,
an early prototype will be selected. The extended risk
analysis will be initiated; all the possible risks, as well
as alternatives to avoid and minimize them, will be
listed. The preliminary economic, financial and
regulatory strategies will be further defined. Pre-
clinical studies to prove the non-toxicity and to
characterize the mechanical properties of the
materials to be used will be also performed.
Moreover, basic prototypes to sustain proof of
concept will be elaborated.
3. Design and development: At this phase, the product
design will be implemented and evaluated, ensuring
that the basic essential requirements are satisfied.
Moreover, the risk management, in which design, use
and process will have to be considered, and regulatory
Xtrace: Novel Bioresorbable Device for Patent Foramen Ovale Closure
347

strategies will be defined and implemented,
considering the specific device design. Furthermore,
the clinical validation plan will be designed
considering the applicable legislation as well as the
particularities of the designed device.
4. Final validation and product launch preparation: At
this phase, approval from the competent authorities
(in this case, FDA) will be required to commercialize
the product. Hence, all the applicable documentation
(clinical studies, safety, etc) will have to be presented.
Moreover, a market launch plan must be prepared:
direct contact with professionals and health provider
must be made to make them aware of our product.
5. Product launch and post-launch assessment:
During this phase, physicians must be trained in the
use of our product and sales strategies must be set in
practice. Moreover, to ensure safety, post-market
surveillance and follow up studies must be done.
Follow up is fundamental to identify and correct any
potential mistakes appearing on the process.
5.2 Tests and Experiments
During the product development phase, a series of
tests and studies is necessary in order to be able to
finally access the market. These tests are the
recommended endpoints by ISO 10993-1:2009 and
FDA. Firstly, cytotoxicity and cytocompatibility in-
vitro tests will have to be performed to evaluate the
toxic potential of the materials used in our product
and their biological acceptance by human tissue.
Permanent lineage cells will be used to classify the
modifications from non-cytotoxic to severe
cytotoxicity, while human differentiated cells will be
used to evaluate the cytocompatibility. For both tests,
it is afterwards intended to use small animal models
as rats for initial in-vivo testing of the bioresorbable
materials. A mechanical analysis in silico would be
necessary to test the material properties.
Secondly, a large animal model as a sheep is
necessary to validate in vivo biocompatibility and the
whole intervention process. Preferably, interventional
cardiologists would perform PFO closure on created
defects in the atrial septum of 10-20 animals.
Irritation, acute systemic toxicity, genotoxicity,
implantation and hemocompatibility can be evaluated
through these experiments. The collected data will be
used for further modifications of the device.
After successful experiments on animal models, a
pilot clinical study with 5-10 patients would have to
be performed to evaluate the device in terms of
biological reaction and the intervention process in
humans. This study will be a long term study with
follow-up of the patients to assess the degradation
rate of the materials, potential inflammations or other
complications. The collected data will be used for
further modifications of the device. The following
trials would be clinical trials on a bigger number of
patients to collect the necessary data for clinical
approval. Inclusion criteria, the choice of the
comparator, blinding, the duration of the study and
follow-up are all matters which will be taken into
consideration when creating the protocol. After
successful entry on the market, post-market follow-
up studies will have to be performed to collect
complaints and mitigate emerging risks.
6 DISCUSSION
Previous studies have tried to develop effective
solutions that prevent the adverse side effects and
complications of the current FDA approved PFO
occluders but without a successful outcome (Giblett,
2019 and Schwerzmann, 2005). The use of metallics
materials (mainly nitinol) can lead to late erosion.
Moreover, the bioabsorbable occluders are not
available in clinic due to higher risk of shunts.
Evidence suggests that the closure of PFO using the
bioabsorbable device is correlated with a low
complication rate and a low recurrence rate of
embolic events. Nevertheless, a high percentage of
mild or moderate residual shunting is present in the
following 6-months after the procedure. We analysed
previous clinical studies (Van den Branden, 2010),
performed literature review, as well as gained
feedback from professionals and key opinion leaders
(KOL) on designing the novel medical device in order
to solve these complications.
In order not to leave any foreign material behind,
the used material must be bioabsorbable, i.e., capable
of being absorbed into living tissue. To prevent
complete failure of the device before complete tissue
replacement, the service lifetime of the device must
be between 6 and 12 months. As the material will be
in direct contact with living tissue, it must be bio- and
hemocompatible. The used material must prevent
platelet aggregation and thrombogenesis. Moreover,
it must not cause excessive tissue inflammation.
Therefore, it is essential to assess the mechanical
properties, performance and bio-absorbability of our
proposed device to achieve a safe treatment. We find
ourselves in the very early stages of the project at the
moment of this communication, therefore the
majority of the research has been done only at a
theoretical level.
ClinMed 2020 - Special Session on Designing Future Health Innovations as Needed
348

7 CONCLUSION
Although our aim is initially to target the adult
population who suffer from cryptogenic strokes and
other complications, our prospects do include
expanding our target audience and tacking pediatric
treatment too. Moreover, skills are certainly needed
to be learned for the PFO closure procedure with the
help of an experienced interventional cardiologist
performing interventions with our device. The
availability of the product for different categories of
patients will fulfill the essential unmet clinical need,
as well as provide a safe and effective delivery of
therapy for the whole population. On the technical
side, there is the possibility to include a bioactive
coating capable of releasing anticoagulant drugs
directly into the framework of the device, thus
removing the necessity of administering the drugs
after the intervention separately.
ACKNOWLEDGEMENTS
We want to give a special thanks to the organisers of
EIT Health Clinmed 2019 summer school, as well as
the mentors for giving us advice and feedback on our
project during the workshop days. We also thank the
Faculty of Medicine of the University of Lisbon and
the Cardiology Imaging Unit at the Santa Maria
Hospital (Lisbon, Portugal) for arranging the
immersive experience.
REFERENCES
AMPLATZER PFO Occluder: PFO Closure Device.
Retrieved from https://www.cardiovascular.abbott/us/
en/hcp/products/structural-heart/amplatzer-pfo.html
Belkin, R. N., & Kisslo, J. (1990). Atrial septal aneurysm:
Recognition and clinical relevance. American Heart
Journal, 120(4), 948–957. doi: 10.1016/0002-
8703(90)90214-i
Branden, B. J. V. D., Post, M. C., Plokker, H. W., Berg, J.
M. T., & Suttorp, M. J. (2010). Patent Foramen Ovale
Closure Using a Bioabsorbable Closure Device. JACC:
Cardiovascular Interventions, 3(9), 968–973. doi:
10.1016/j.jcin.2010.06.012
Collado, F. M. S., Poulin, M. F., Murphy, J. J., Jneid, H., &
Kavinsky, C. J. (2018). Patent Foramen Ovale Closure
for Stroke Prevention and Other Disorders. Journal of
the American Heart Association, 7(12). doi:
10.1161/jaha.117.007146
Giblett, J. P., Abdul-Samad, O., Shapiro, L. M., Rana, B.
S., & Calvert, P. A. (2019). Patent Foramen Ovale
Closure in 2019. Interventional cardiology (London,
England), 14(1), 34–41. doi:10.15420/icr.2018.33.2
Gu, X., Zheng, Y., Cheng, Y., Zhong, S., & Xi, T. (2009).
In vitro corrosion and biocompatibility of binary
magnesium alloys. Biomaterials, 30(4), 484–498.
https://doi.org/10.1016/j.biomaterials.2008.10.021
Hagen, P. T., Scholz, D. G., & Edwards, W. D. (1984).
Incidence and Size of Patent Foramen Ovale During the
First 10 Decades of Life: An Autopsy Study of 965
Normal Hearts. Mayo Clinic Proceedings, 59(1), 17–
20. doi: 10.1016/s0025-6196(12)60336-x
Ko, R., Walker, N. E., & Mullen, M. J. (2010). Different
patent foramen ovale closure techniques in varying
anatomies. Interventional Cardiology, 2(1), 85–95. doi:
10.2217/ica.09.36
Mao, L., Shen, L., Chen, J., Zhang, X., Kwak, M., Wu, Y.,
Ding, W. (2017). A promising biodegradable
magnesium alloy suitable for clinical vascular stent
application. Scientific Reports, 7(1). doi:
10.1038/srep46343
Meier, B. (2005). Closure of patent foramen ovale:
technique, pitfalls, complications, and follow up. Heart,
91(4), 444–448. doi: 10.1136/hrt.2004.052258
Morgan, G., Lee, K.-J., Chaturvedi, R., & Benson, L.
(2010). A biodegradable device (BioSTAR™) for atrial
septal defect closure in children. Catheterization and
Cardiovascular Interventions, 76(2), 241–245. doi:
10.1002/ccd.22517
Opotowsky, A.R., Landzberg, M.J., Kimmel, S.E., Webb,
G.D., Trends in the Use of Percutaneous Closure of
Patent Foramen Ovale and Atrial Septal Defect in
Adults, 1998-2004. (2008). JAMA, 299(5), 521–522.
https://doi.org/10.1001/jama.299.5.521
Rhodes, J. (2008) PFO Closure for Prevention of Recurrent
Cryptogenic Stroke. Cardiac Interventions Today, 72.
Saver, J. L., Carroll, J. D., Thaler, D. E., Smalling, R. W.,
MacDonald, L. A., Marks, D. S., & Tirschwell, D. L.
(2017). Long-Term Outcomes of Patent Foramen Ovale
Closure or Medical Therapy after Stroke. The New
England Journal of Medicine, 377(11), 1022–1032.
https://doi.org/10.1056/NEJMoa1610057
Schwerzmann, M., & Salehian, O. (2005). Hazards of
percutaneous PFO closure. European Journal of
Echocardiography : the Journal of the Working Group
on Echocardiography of the European Society of
Cardiology, 6(6), 393–395. https://doi.org/10.1016/j.
euje.2005.09.007
Staiger, M. P., Pietak, A. M., Huadmai, J., & Dias, G.
(2006). Magnesium and its alloys as orthopedic
biomaterials: A review. Biomaterials, 27(9), 1728–
1734. doi: 10.1016/j.biomaterials.2005.10.003
Xtrace: Novel Bioresorbable Device for Patent Foramen Ovale Closure
349
