
Prediction of Local Abnormal Ventricular Myocardial Electrical
Activation on Surface ECG in Patients with Structural Heart Disease
Zafar M. Yuldashev
1a
, Anatoli P. Nemirko
1b
, Evgeny N. Mikhaylov
2c
, Dmitry S. Lebedev
2d
,
Aleksei A. Anisimov
1e
, Alena I. Skorobogatova
1f
and Darina S. Ripka
1g
1
Saint Petersburg Electrotechnical University, Professor Popov Street 5, Saint-Petersburg, Russia
2
Almazov National Medical Research Centre, Akkuratov Street 2, Saint-Petersburg, Russia
Keywords: Endo- and Epicardial Electrograms, Surface ECG, Synchronous Registration, Signal Processing and Analysis,
Ventricular Late Potentials, Correlation, Life-threatening Heart Disorders.
Abstract: The problems of processing and analysis synchronous records endo- and epicardial electrograms and surface
ECG signals, detection of ventricular late potentials of patients with ventricular tachyarrhythmia and coronary
heart disease by using spatial and temporal signal accumulation algorithms, correlation of temporal and
spectral characteristics of late potentials with the dynamics and localization of dangerous heart disorders are
considered.
1 INTRODUCTION
The surface ECG signal is the result of the spatio-
temporal summation of the electric potential, which
is formed as a result of the excitation of myocardial
fibres by the action potential when it spreads along
the conduction pathways of the heart and the
contractile myocardium. Normally, the action
potential is first generated by the sinoatrial node and
sets the heart rate. A cardiac electrogram is an
electrical signal recorded by a pair of electrodes of a
special catheter when the action potential passes by
this pair of electrodes. The temporal characteristics
and form of intracardiac electrograms on paired
catheter electrodes represent the nature of the
propagation of the action potential along the
myocardium. There is a relation between the
characteristics of intracardiac electrograms and the
waves and segments of the surface ECG signal. Endo-
and epicardial electrogram registration is of
paramount importance in diagnosis and treatment of
heart rhythm disorders, since they allow establishing
a
https://orcid.org/0000-0003-1075-3420
b
https://orcid.org/0000-0001-6459-626X
c
https://orcid.org/0000-0002-6553-9141
d
https://orcid.org/0000-0002-2334-1663
e
https://orcid.org/0000-0003-1363-1971
f
https://orcid.org/0000-0002-5490-6217
g
https://orcid.org/0000-0002-0244-4487
the localization and mechanism of tachyarrhythmias
and conduction abnormalities. Ventricular late
potentials and fragmented QRS complexes have
significant diagnostic value. A large number of
publications that have become classics of clinical
cardiology (Breithardt, Borggrefe, Martinez-Rubio,
et al, 1988; Simson, Euter, Michelson et al, 1981;
Simson, 1983; Breithardt, Cain, El-Sherif et al., 1991)
show that these potentials are reliable predictors of a
number of life-threatening heart disorders and sudden
death. However, the registration and analysis of endo-
and epicardial electrograms is carried out only for
certain indications, in contrast to the registration and
analysis of the surface ECG signal, the identification
and evaluation of the characteristics of ventricular
late potentials and fragmented potentials is difficult
due to their short duration (less than 180 ms), low
amplitude (less than 40 μV), significant frequency
variability (up to 700 Hz), amplitude and duration.
Since in the majority cases ventricular fragmented
and late potentials are not detected on surface ECG
using simle analysis, special methods and algorithms
Yuldashev, Z., Nemirko, A., Mikhaylov, E., Lebedev, D., Anisimov, A., Skorobogatova, A. and Ripka, D.
Prediction of Local Abnormal Ventricular Myocardial Electrical Activation on Surface ECG in Patients with Structural Heart Disease.
DOI: 10.5220/0009374103950401
In Proceedings of the 13th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2020) - Volume 1: BIODEVICES, pages 395-401
ISBN: 978-989-758-398-8; ISSN: 2184-4305
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
395

for processing and analyzing multi-channel
recordings of a surface ECG signal are required.
In patients with structural heart diseases
inhomogeneous and delayed electrical activation is
associated with re-entrant and triggered life-
threatening ventricular tachyarrhythmias, as it had
been shown in many scientific researches (Kreiner,
Gottlieb, Furukawa et al., 1992; Wong and Windle,
1994; Teptin, Latfullin, Kоnturov, Mamedova, 2004;
Ohisa, Ohira, Mizonobe et al., 2002). Usually, local
abnormal electrical activation of ventricular
myocardium can be recorded invasively only, when a
mapping catheter is placed at endocardial or
epicardial surface in close proximity to the diseased
area. In clinical practice, invasive mapping of
ventricular tachycardia substrate is aimed at detection
of areas with low amplitude and abnormal local
activity. Although the presence and location of
abnormal activity can be predicted according to
patient clinical characteristics (for instance, in
patients with known localization of post-myocardial
infarction scar), there is a need in prediction models
of the presence and extent of abnormal activity areas
in patients with other cardiac diseases. Pre-procedure
knowledge of localization of the target area for
mapping and further catheter ablation (in order to
terminate and render VTs non-inducibleis of
paramount importance, since it helps to plan the
required access and needed extent of tissue ablation.
The purpose of this study is to develop a
processing algorithm for detecting ventricular late
potentials and fragmented signals from synchronous
recordings of surface ECG and invasively registered
signals, and to improve the accuracy of estimation the
presence of local abnormal electrograms and their
spectral characteristics using the analysis of surface
ECG.
To achieve this goal, we have solved the
following research tasks:
1. Formation of a database of synchronous recordings
of endo- and epicardial electrograms and 12-channel
surface ECG signals reflecting the presence and
absence ventricular late potentials and fragmented
electrograms for various heart rhythm disorders.
2. Detection, analysis and classification of ventricular
late potentials and fragmented QRS complexes using
algorithms for synchronous accumulation and spatial
averaging over surface ECG signals, comparison of
the accuracy of detection of ventricular late and
fragmented potentials and assessment of their
characteristics taking into account synchronous
recordings of intracardiac electrograms.
3. Formation of a complex of indicators of surface
ECG signals correlating with intracardiac ventricular
fragmented and late potentials.
4. Development of an algorithm for identifying late
and fragmented ventricular potentials and evaluating
their temporal, spectral and dynamic characteristics.
5. Formation of a complex of indicators of
fragmented QRS complexes and ventricular late
potentials, reflecting dangerous heart rhythm
disorders.
2 METHODS
2.1
Patient Population
Patients with known structural heart disease and
documented ventricular tachycardia (VT) were
referred for electrophysiological study and catheter
ablation of VT substrate. Inclusion criteria were the
following: the presence of structural myocardial
disease diagnosed using transthoracic
echocardiography, magnetic resonance tomography,
and/or endomyocardial biopsy; VT detected on
surface ECG or by interrogation of an existent cardiac
implantable electronic device (mainly, implantable
cardioverter-defibrillator); signed informed consent
to undergo an invasive electrophysiological study.
Exclusion criteria were the following: the presence of
a reversible VT cause, acute systemic inflammatory
disease, intracardiac thrombosis, the need for
coronary revascularization according to the clinical
and angiographic evaluation.
2.2
Electrophysiological Study
The electrophysiological procedure was performed in
an electrophysiological laboratory; patients were
evaluated in a fasting state under general anesthesia
with propofol, fentanyl and arduan. A femoral access
was performed via the common femoral vein (a
transseptal 8F Multipurpose sheath (Cordis, Johnson
and Johnson, USA) and a 6F vascular sheath (Avanti,
Cordis, Johnson and Johnson, USA) were
introduced), and via the common femoral artery (an
8F vascular sheath was used).
A combined endocardial left ventricular access
was performed retrogradely via the arterial sheath and
using the transseptal access. Puncture of the
interatrial septum was performed using the
Brockenbrough BRK-1 needle (Abbott, USA) with a
small amount of contrast media used to confirm
appropriate access to the left atrium (Optiray 300,
Mallickrodt, Germany).
After successful transseptal puncture the
transseptal sheath was advanced into the left
NDNSNT 2020 - Special Session on Non-invasive Diagnosis and Neuro-stimulation in Neurorehabilitation Tasks
396

ventricle. Following left-sided access intravenous
heparin was administered (100 IU* kg-1) to prevent
thrombosis. A 6F quadripolar diagnostic catheter
(Webster, Johnson and Johnson, USA) was placed
into the right ventricle apex for stimulation and/or
time annotation of the bipolar intracardiac signals.
Electrogram mapping was performed using both a
duodecapolar Pentaray catheter (Biosense Webster,
USA) and a 3.5-mm tip quadripolar irrigated mapping
and ablation catheter NaviStar ThermoCool
(Biosense Webster, USA). Electrophysiological
mapping was performed under the non-fluoroscopic
three-dimensional mapping system CARTO 3
(Biosense Webster, USA).
Three-dimensional shells were created using the
“FAM (Fast Anatomical Model)” module and
automatic point acquirement using the “Confidense”
module with a maximum 2 mm distance between
points. Electrophysiological signals from mapping
catheters were recorded and stored simultaneously
with surface ECG signals on the CardioLab (GE,
USA) system.
When epicardial mapping was indicated and
planned, fluoroscopically-guided subxyphoid
puncture was performed first; the technique was
previously described in details (Simonova, Lebedev,
Mikhaylov, 2017; Simonova, Mikhaylov, Tatarskiy
et al., 2019). The non-steerable 8F multipurpose
sheath was inserted into pericardial space for
introducing and manipulating a mapping catheter.
Endo- and epicardial mapping was performed
during sinus rhythm or during right ventricle
stimulation at a rate 600 ms per min. Normal bipolar
signals were characterized by two high-frequency
deflections (a positive and a negative consecutive
deflections). Abnormal signals were characterized by
splitting, notching, slurring, fragmentation, doubling
(the presence of an isoline between two components),
and by the late activity (signals widely separated from
the main signals and located after the end of QRS on
the surface ECG).
2.3
Electrophysiological Signals’
Extraction
Tracings with normal and abnormal bipolar signals
were manually annotated on the electrophysiological
system, and tracings containing the ECG and
intracardiac/epicardial bipolar signals were extracted
from the electrophysiological system in .txt format.
The extraction was performed using an integrated
module which allowed marking the cut-off timings on
the whole registration. The raw signal was recorded
at 1000 Hz sampling rate.
3 PROBLEMS SOLVING
3.1
Forming of the Synchronous
Records Base of Endocardial
Electrograms and Surface ECG
Signal
After selecting the most informative segments of the
signals and storing them, the logic of constructing a
database of synchronous records was formulated: a
hierarchical structure of the presentation was chosen.
Its use makes it easy to find records of interest by type
of heart rhythm disturbance and to reveal the
dynamics of the parameters before and after invasive
treatment (radiofrequency catheter ablation of a
tachycardia critical isthmus and/or areas with local
abnormal electrical potentials).
The first level of division is the type of observed
ventricular disturbance: fibrillation, flutter,
tachycardia, bradycardia, extrasystole and late
potentials (Yuldashev, Nemirko, Manilo et al., 2019).
After dividing the recordings by type of
disturbance, the signals were divided into 3 additional
levels: recordings before RF ablation, during and
after the ablation. Using this division allows to track
the change in the characteristics of the electrical heart
activity throughout the operation.
Surface ECG signals were recorded in three or
twelve leads. Signal record database contains 3
channels of surface ECG: I, II and III. For disorders
associated with the ventricles, all 12 ECG channels
were used. Intracardiac activity is represented by the
following leads:
1) dABL – distal lead of the ablation catheter
electrode;
2) ABL – proximal lead of the ablation catheter
electrode;
3) CS12, CS34, CS 56, CS78, CS910 – leads of the
catheter electrode located in the coronary sinus;
4) RV – signals from distal bipoles of the diagnostic
catheter placed in the right ventricle apex;
5) Pentaray – bipolar signals recorded from the
duodecapolar steerable mapping catheter roving in
and on the ventricles.
The database of records consists of 296 records
lasting from 10 to 20 minutes, including records of
the norm and atrial pathology – 128 records, various
ventricular pathologies – 168 records.
Prediction of Local Abnormal Ventricular Myocardial Electrical Activation on Surface ECG in Patients with Structural Heart Disease
397
3.2
FQRS Complex and Ventricular
Late Potentials Detection
Algorithms
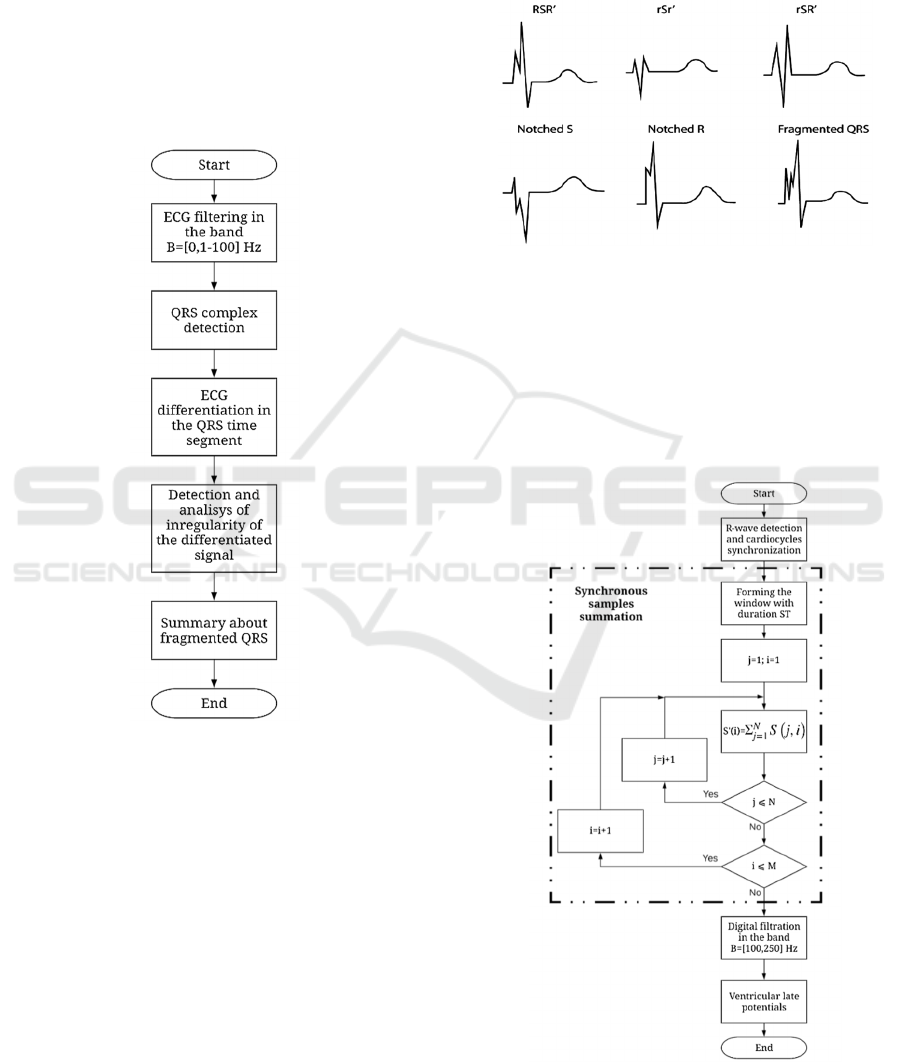
The following algorithm was proposed to detect
fragmented QRS (FQRS) complexes (figure 1). At
the first stage, the surface ECG signal was subjected
to low-pass filtering with a cutoff frequency of the
filter fCH = 100 Hz to reduce the influence of high-
frequency noise during the extraction of QRS
complexes.
Figure 1: Fragmented QRS detection algorithm.
In the reason of the fragmented QRS complex is
characterized by the presence of notches, patterns in
the areas of Q, R and S waves (figure 2), to detect
them, the initial ECG signal in the segment of the
selected QRS complex undergoes differentiation.
Next, the irregularity of the differentiated signal is
established and its analysis. A smooth change in the
differentiated signal from a negative value to a
positive value means the absence of fragmented QRS
complexes. Its stepwise change reflects the presence
of fragmented complexes.
Methods of temporal or spatial summation are
used to detect ventricular late potentials. It should be
noted that the ventricular late potentials appear on the
ST segment and are characterized by a very low
amplitude (tens of μV), high frequency (up to
hundreds of Hz), short duration (up to 150 ms) and
significant variability of characteristics from one
cardiocycle to another. This fact makes it difficult to
detect and analyze ventricular late potentials (VLP).
Figure 2: Types of fragmented QRS complex.
Methods of temporal or spatial summation are
used to detect ventricular late potentials (figure 3). It
should be noted that the ventricular late potentials
appear on the ST segment and are characterized by a
very low amplitude (tens of μV), high frequency (up
to hundreds of Hz), short duration (up to 150 ms) and
significant variability of characteristics from one
Figure 3: Temporal summation VLP detection method.
NDNSNT 2020 - Special Session on Non-invasive Diagnosis and Neuro-stimulation in Neurorehabilitation Tasks
398
cardiocycle to another. This fact makes it difficult to
detect and analyze ventricular late potentials (VLP).
When using temporary summation (figure 3), R
prongs are first allocated on the ECG signal, relative
to which a window that coincides with the ST
segment is formed. Within this window, for all N
(usually up to 150) cardiocycles, synchronous
accumulation (summation) of discrete ECG signal
counts is performed.
For one cardiocycle, the number of samples can
reach m = 200. With synchronous accumulation, the
amplitude of the late ventricular potential increases N
times and reaches a level of tens of mV. It is filtered
by a band-pass filter in the range from 100 to 250 Hz
in order to eliminate the low-frequency components
of the ST segment. The rest of the signal represents
the ventricular late potential. The considered method
of synchronous signal accumulation for detecting the
ventricular late potential has advantages and
disadvantages. The advantage is the simplicity and
using only one channel of the surface ECG signal.
Disadvantages exceed advantages. The presence of
noise fluctuations in the ECG signal leads to the
detection of R prongs and the formation of a window
within which synchronous accumulation is
performed, with an error of up to 2-3 reports of the
sampling signal at a sampling frequency of 1,0 kHz,
which in turn smears the ventricular late potential and
distorts the high-frequency components. Another
disadvantage is the inability to assess the dynamics of
the characteristics of the VLP and their duration due
to the long stage of accumulation (up to 150
cardiocycles).
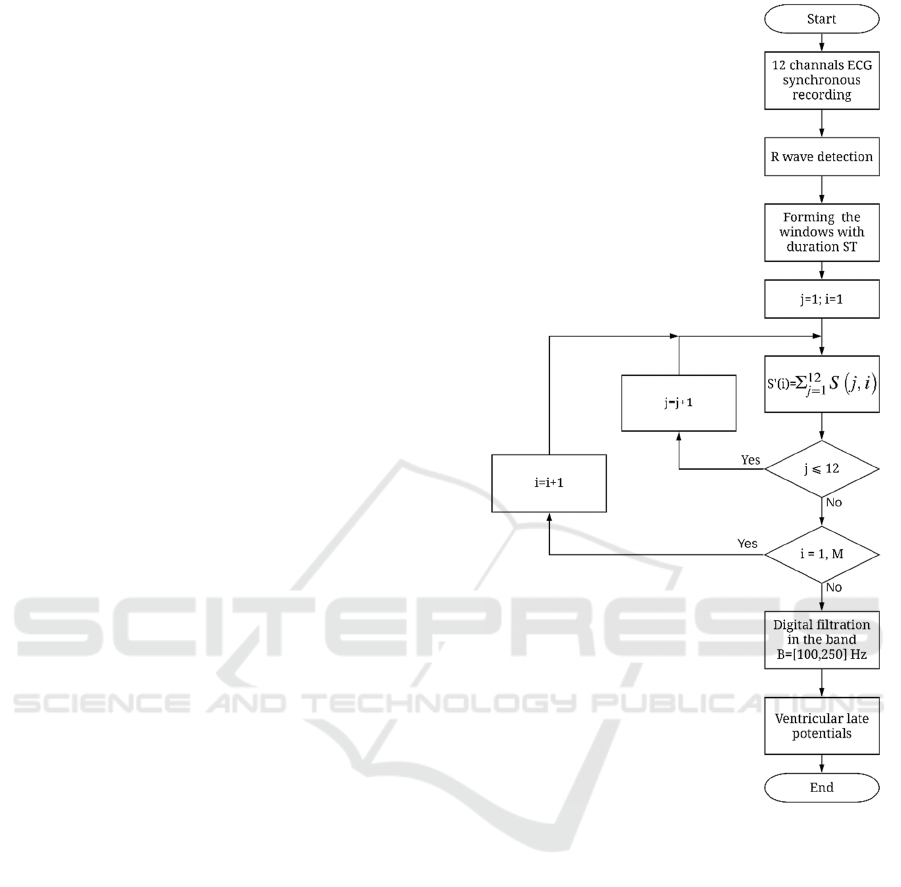
The spatial accumulation method (figure 4) is
devoid of these disadvantages. However, it requires
performing synchronous recordings of surface ECG
signals over 12 channels, detecting R prongs, forming
the window for detecting the samples of ECG signals
on ST segment, summing up identical discrete
samples across all channels, band-pass filtering of the
resulting signal in the range from 100 to 250 Hz.
The resulting signal represents the ventricular late
potential obtained from the spatial summation of
multichannel ECG signals. The advantage of the
considered method is that it allows reflecting the
dynamics of the characteristics of the VLP signal, and
is less sensitive to fluctuation noise, because the
formation of the window and synchronization of the
summation of the samples is carried out
simultaneously on all channels. However, this
method has a drawback. It does not allow to
significantly increase the amplitude of the VLP
signal, the gain does not exceed 12.
Figure 4: Spatial accumulation VLP detection method.
3.3 Fragmented QRS and VLP Research
Studies of ventricular late potentials were performed
on 16 patients using synchronous recording of
intracardiac ventricular electrograms and 12 leads of
surface ECG (Yuldashev, Anisimov, Nemirko et al.,
2019). The ventricular late potentials were detected
on intracardiac electrograms in all cases, while
surface ECGs did not visually reveal these
abnormalities due to very low levels of late potentials
amplitude, short duration, and high frequency of
electrical vibrations (figures 5 -7).
The ventricular late potentials detected by
intracardiac electrograms almost in most cases
correlate well with various ventricular myocardial
disorders. As the results of studies [1, 4, 6, 7, 8] show,
the accuracy and sensitivity of the diagnosis of both
Prediction of Local Abnormal Ventricular Myocardial Electrical Activation on Surface ECG in Patients with Structural Heart Disease
399

Figure 5: Example of VLP detection.
Figure 6: Example of VLP detection.
Figure 7: Example of VLP detection.
dangerous cardiac arrhythmias due to cardiac
conduction disorders and myocardial cell
morphology using ventricular late potentials is at least
92%.
The results of these studies confirm the need for
further improvement of methods and technologies for
identifying fragmented and late potentials using
surface ECGs and verifying their results using
intracardiac electrograms.
3.4 Clinical and Development
Perspective
To the best of our knowledge, the signal database
created within the scope of this work is one of the first
of its kind and will be used in future research.
Processing algorithms for automatic local
electrical abnormal potentials detection are under
development in this project, and, once developed, will
be useful with potential future implementation into
invasive electrophysiological diagnostic systems.
The prediction algorithms based on surface ECG
analysis could be useful in estimation of the presence
and localization of local abnormal electrical activity
and will be of clinical importance, since might be
implemented into pre-procedure planning of the
access and extent of catheter ablation.
4 CONCLUSIONS
The results of the studies confirm the conclusions
about the need and feasibility of using the ventricular
late potentials and fragmented potentials for the
diagnosis of dangerous heart disorders. Of course, in
a clinical setting, the results of recording intracardiac
electrograms can be used to diagnose that disorders.
However, often there is a need for the diagnosis of
cardiac abnormalities outside the clinic, in particular
at home using a wide range of electrocardiographs.
To diagnose heart disorders that pose a threat to the
patient’s life, at home it is necessary to use tools and
software that will record surface ECG signals and
identify fragmented and late heart potentials hidden
in surface ECG signals. Given that the accuracy of the
diagnosis of such heart disorders using methods of
pre-processing and synchronous signal accumulation
is quite high, such devices will significantly improve
the quality of medical care for cardiac patients.
ACKNOWLEDGEMENTS
This research was supported by Russian Foundation
for Basic Research (RFBR), research projects 18-29-
02036, 19-29-01009.
REFERENCES
Breithardt, G., Borggrefe, M., Martinez-Rubio, A. et al,
1988. Prognostic significance of ventricular late
NDNSNT 2020 - Special Session on Non-invasive Diagnosis and Neuro-stimulation in Neurorehabilitation Tasks
400

potentials in the postmyocardial infarction period. In
Herz. Bd 13, №3, pp.180-187.
Simson, М. В., Euter, D. E., Michelson E. L., et al, 1981.
Detection of delayed ventricular activation on the body
surface in dogs. In Amer. J. Physiol. Vol. 241, pp.
H363-H369.
Simson, M. B., 1983. Clinical application of signal
averaging. In Cardiol. Clin. Vol. 1, pp. 109-190.
Breithardt, G., Cain, M. E., El-Sherif, N. et al., 1991.
Standards for analysis of ventricular late potentials
using high resolution or signal-averaged
electrocardiography. A statement by a Task Force
Committee between the European Society of
Cardiology, the American Heart Association and the
American College of Cardiology. In Eur. Heart.
Journal. Vol. 12(4), pp. 473-480.
Kreiner, G., Gottlieb, C. D., Furukawa, S. et al., 1992. Late
potentials in an ovine model of acute transmural
myocardial infarction. In J. Appl. Physiol. Vol. 73(3),
pp. 841-846.
Wong, C. B., Windle, J. R., 1994. Clinical applications of
signal averaged electrocardiography in patients after
myo cardial infarction. In Nebraska Medical Journal.
Vol. 79(2), pp. 28-31.
Teptin, G. M., Latfullin, I. A., Kоnturov, S. W., Mamedova,
L. E., 2004. Analysis of low amplitude cardiac signals
and its interpretation. In Environmental Radioecology
and applied ecology. Vol. 10, №1, pp. 3-7.
Ohisa, N., Ohira, M., Mizonobe, K. et al., 2002.
Comparative study of T-wave alternans, QT c
dispersion and late potential for predicting ventricular
tachycardia in patients with ischemic heart disease. In
Rinsho Byori. Vol. 50(2), pp.191-195.
Simonova, K. A, Lebedev, D. S, Mikhaylov, E. N., 2017.
Epicardial mapping and ablation in management of
ventricular tachycardia. In Complex Issues of
Cardiovascular Diseases. Vol 6(4), pp. 138-145.
Simonova, K. A, Mikhaylov, E. N, Tatarskiy, R. B et al.,
2019. Epicardial arrhythmogenic substrate in patients
with postinfarction ventricular tachycardia: a pilot
study. In Journal of Arrhythmology. Vol 1(95), pp. 38-
46.
Yuldashev, Z., Nemirko, A., Manilo, L. et al., 2019.
Processing of Synchronous Recordings of Surface ECG
and Intracardiac Potentials for Diagnostics of
Dangerous Heart Rate Disturbances. In Proceedings
Ural Symposium on Biomedical Engineering,
Radioelectronics and Information Technology
(USBEREIT). PP. 102-105.
Yuldashev, Z., Anisimov, A., Nemirko, A. et al., 2019.
Heart rate disorders identification using superficial
ECG and invasive electrogram. In AIP Conference
Proceedings.
Prediction of Local Abnormal Ventricular Myocardial Electrical Activation on Surface ECG in Patients with Structural Heart Disease
401
