
The Doctor Will See Yourself Now: Review and Discussion of a
Mass-market Self-service Technology for Medical Advice
Joseph Ollier
1a
and Tobias Kowatsch
2,3 b
1
Center for Digital Health Interventions, Chair of Technology Marketing, ETH Zurich, Zurich, Switzerland
2
Center for Digital Health Interventions, Chair of Information Management, ETH Zurich, Zurich, Switzerland
3
Center for Digital Health Interventions, Institute of Technology Management, St. Gallen, Switzerland
Keywords: Self-service Technology, Digital Health, Data Privacy.
Abstract: Leveraging new technological tools in medical service delivery has been shown as important factor adding
scalability and/or value to patient care. However, as of yet, relatively little research has focused on the
implementation of mass-market digital health products to address population needs. The current paper
examines one such tool; a browser-optimized smartphone app developed by a major Swiss health insurance,
offering validated medical information for patients to identify the optimal care path of action (i.e. self-care,
pharmacy visit, general practitioner visit, hospital visit). Summary statistics of usage data from 149 922 users
over 6 months are outlined, overviewing; (i) key usage cases for the service over time, (ii) for whom the app
was used, (iii) dropout rates and potential design pitfalls. Possible themes are identified such as the importance
of additional information regarding privacy or service/usage experience information, and some considerations
for both the research, design and implementation communities.
1 INTRODUCTION
Never before in human history has so much
information been available at a few taps of the finger
(Acquisti, Brandimarte, & Loewenstein, 2015), yet
finding trustworthy and legitimate sources of medical
information remains a challenge (Soldaini & Goharian,
2017). At one end of the spectrum, digital platforms
have enabled the recycling of long disputed
information to new audiences, for example, the rise of
“anti-vaxxer” campaigns (Kennedy, 2019), whereas at
the other end of the spectrum, digital artefacts have
enabled health information to connect with new
audiences in a meaningful and engaging manner
(Barello et al., 2015). Somewhere between these two
extremes resides the average individual, searching for
information online and making health decisions for
themselves or their family. With over 1 billion health
related searches globally on Google, equating to 70
000 queries a minute, the consumer desire for health
information is clear (M. Murphy, 2019).
For policy makers and firms alike, addressing this
desire for health information is both an opportunity
and a challenge. Opportunities lie in reducing the
a
https://orcid.org/0000-0001-8603-0793
b
https://orcid.org/0000-0001-5939-4145
burden for healthcare systems; for example within
Switzerland, despite rising hospital admissions, only
2.4% of the national healthcare budget (equating to
19 CHF per month) is spent on preventative measures
such as the dissemination of healthcare information
(FSO, 2019). For firms, creating trustworthy health
services through self-service technologies can
address this state of consumer confusion; forging a
meaningful connection with patients/customers and
delivering medical services that add value (Sweeney,
Danaher, & McColl-Kennedy, 2015; W.-T. Wang,
Cheng, & Huang, 2013). For all parties, addressing
these needs solves the long-standing issue of
individuals entering the health system at the wrong
point in time (Mayer, Villaire, & Connell, 2005);
either too early (before adequate self-care steps have
been taken) or too late (when the danger of serious
complications has increased).
In seeking to address these challenges a number
of mass-market digital tools have been developed by
organizations, offering information on medical
symptoms, check-ups, diagnosis or other information
(Lupton, 2016), such as Ada, a digital app health
companion (Ada, 2020) or the Health A-Z website
798
Ollier, J. and Kowatsch, T.
The Doctor Will See Yourself Now: Review and Discussion of a Mass-market Self-service Technology for Medical Advice.
DOI: 10.5220/0009373607980807
In Proceedings of the 13th Inter national Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2020) - Volume 5: HEALTHINF, pages 798-807
ISBN: 978-989-758-398-8; ISSN: 2184-4305
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

(NHS, 2020). However, as of yet, consumer reception
to such medical self-service technologies is relatively
little understood due to a lack of usage data released
by the implementers of such services to the general
public. The current paper therefore overviews some
first insights based on six months usage data with one
such tool developed and offered starting 2018 by a
major health insurer in Switzerland.
The remainder of this paper is structured as
follows: first, we review the conceptual background
of digital health information tools, including the
justification for both policy makers and firms that
enact them. Next, we overview the self-service
technology in use (a smartphone-optimized browser
app), and then we examine the highlighted results
from available usage data. Finally, findings are
reviewed in light of relevant academic work and
useful future research streams are addressed.
2 CONCEPTUAL BACKGROUND
In making health choices, it has long been known that
individuals face difficulties in making suitable deci-
sions within a complex healthcare system (Paasche-
Orlow, Parker, Gazmararian, Nielsen-Bohlman, &
Rudd, 2005). Individuals require easily available,
accurate and timely information (Hibbard & Peters,
2003), however the abundance of information does not
always translate into more informed choices. Visits to
the emergency department for minor complaints
(Mayer et al., 2005; S. M. Murphy & Neven, 2014;
Rieffe, Oosterveld, Wijkel, & Wiefferink, 1999) or
unnecessary general practitioner visits when a
pharmacy could provide better self-care information
and medication (Hassell, Rogers, & Noyce, 2000)
have long been established as contributing to
increased healthcare system costs (Hewner, Sullivan,
& Yu, 2018; Mayer et al., 2005; Rieffe et al., 1999).
Free healthcare services providing health
information have been touted as potentially useful
solutions, preventing individuals entering the
healthcare system at the wrong entry point (Hwang,
Liao, Griffin, & Foley, 2012). This has included
phone consultations (Hallfors, Saku, Makinen, &
Madanat, 2018), and more recently the utilization of
digital platforms (Bahadori, Teymourzadeh, &
Mousavi, 2018) such as email and smartphone
communications (Chua et al., 2017). These free
services have the added benefit of being a potentially
useful way to reach non-insured and/or low income
groups which may benefit in particular with a trusted
health information source (Hwang et al., 2012).
For patients, use of digital tools have been shown
to lead to higher health literacy (Xie, 2011) and by
consequence, less unnecessary emergency room or
general practitioner visits, which contribute to reducing
overcrowding in healthcare systems (FSO, 2019).
From a business perspective, for private enterprises
creating digital tools, services research has shown the
ability to work well with healthcare resources enables
a “co-creation” of value, with positive downstream
consequences for both customer and firm (McColl-
Kennedy, Vargo, Dagger, Sweeney, & van Kasteren,
2012; Sweeney et al., 2015). However, to date,
relatively little commercial data has been available
examining consumer reception to the introduction to
such digital products at a mass-market / population
level. Yet this is vital, for policy makers, practitioners
and academics to push the development of such digital
tools to their next steps of development.
3 METHOD
The current paper outlines data from a browser-based
smartphone app created by a major Swiss health
insurance firm, available on any device without
requiring the app’s download. The app was developed
based on a verified medical framework created
independently by doctors and adapted by the
insurance firm into a dialogue/survey like format.
Individuals could input their main and secondary
complaints and answer a variety of questions to
receive medical advice. The medical advice consisted
of a recommendation of a course of action, rather than
a medical diagnosis per se, as the apps purpose was
to direct individuals to the correct healthcare system
entry point for further evaluation. Upon completion
of the dialogue, individuals would be recommended
to; (i) take self-care steps, (ii) visit a pharmacy, (iii)
visit their general practitioner, (iv) visit emergency
department, for example. See figures 1-4 for
screenshots of the tool in English.
In total, 149 222 app uses were recorded during 6
months of field use in German-speaking Switzerland,
from the product launch in September 2018 to the end
of the data collection period in February 2019. The
tool was not widely marketed or available to the
general public, but current customers of the health
insurance firm were emailed a link stating that the
product was live and that they could access and use
the tool. A selection of data was made available by
our partner company for the purposes of
disseminating knowledge of healthcare innovations
in the field. Data made available includes; (i) for
whom the tool was used (age and gender), (ii) the
primary symptom (main usage reason), (iii) changes
The Doctor Will See Yourself Now: Review and Discussion of a Mass-market Self-service Technology for Medical Advice
799
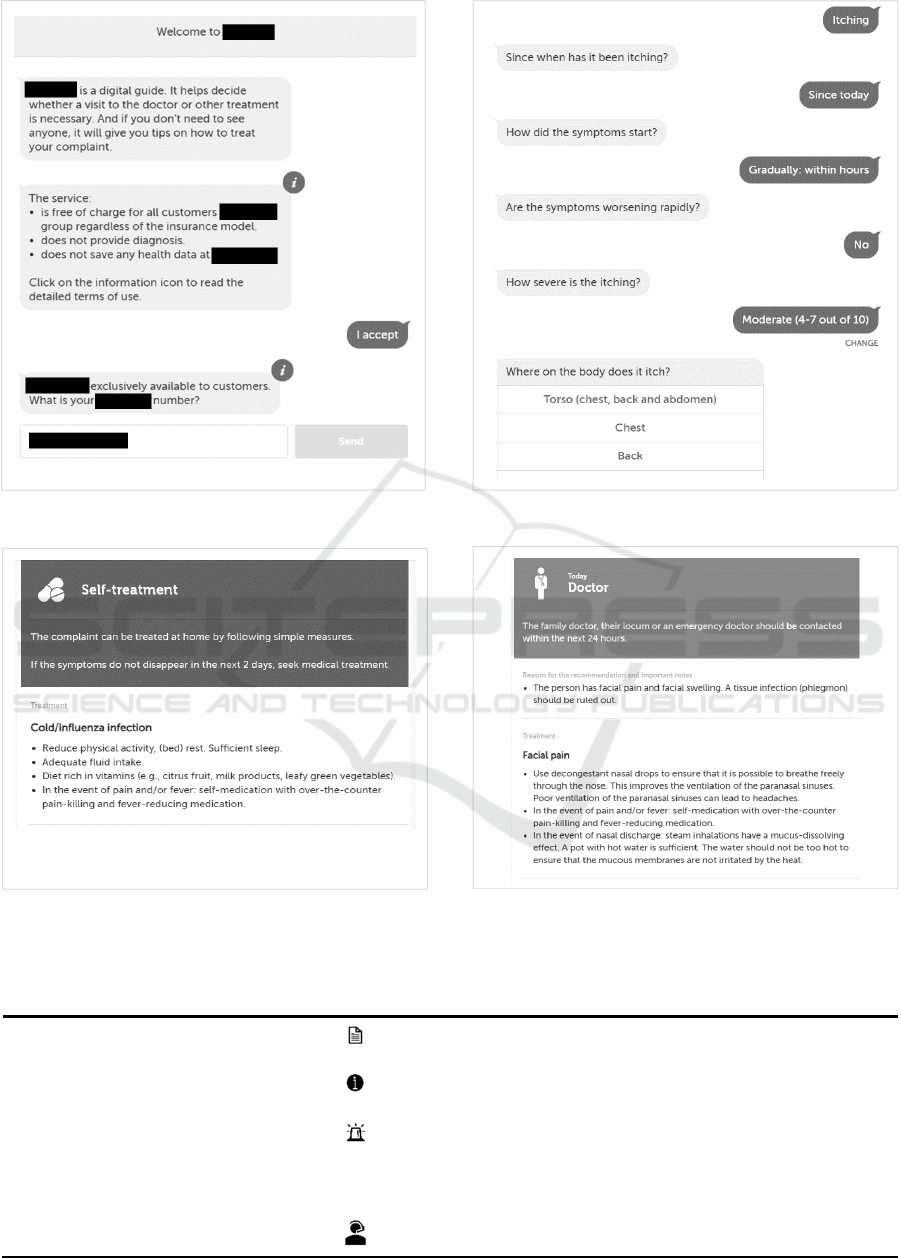
Figure 1: Dialogue start.
Figure 3: Self-care recommendation.
Figure 2: Dialogue symptom selection.
Figure 4: Doctor-visit recommendation.
Table 1: Buttons leading out of optimal usage path.
Use Button Description
Terms and conditions as PDF
Receive terms and conditions as a PDF document
Info Icons
Explain in more detail (e.g. about symptoms, the meaning of
statements)
Emergency
Emergency contact numbers given (911 equivalent)
Frequently asked questions
FAQ
Further information about the app, service information and
data and security
Contact center
Contact numbers for call center staff
Scale-IT-up 2020 - Workshop on Best Practices for Scaling-Up Digital Innovations in Healthcare
800
in disease ranking, showing most common symptoms
selected between 1-3 (first three months) and 4-6
months (latter three months) respectively, (iv) users
continuing/drop outs (per section of the app, where
section consists of a completed dialogue section
around symptoms and/or a separate page of
information) and buttons leading out of the optimal
usage path (i.e. clicking to view FAQs, or further
information buttons etc.) as summarized in table 1.
4 RESULTS
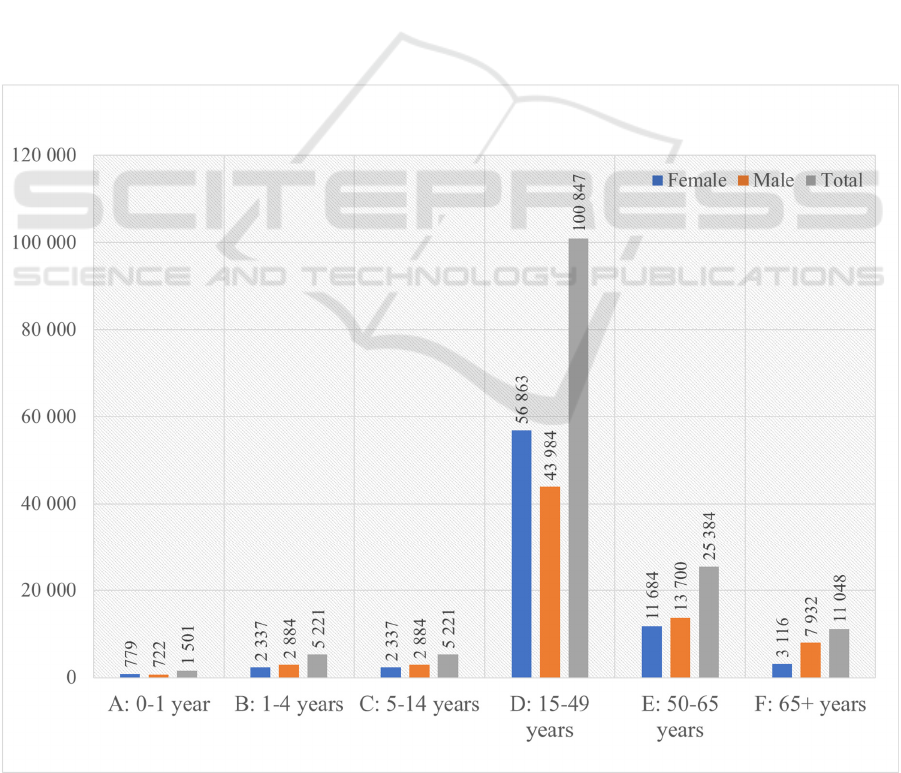
Figure 5 shows a breakdown of the use cases by age
and gender, whereby these figures reflect the intended
recipient of the medical information. Overall cases
were recorded for all age groups, however,
individuals aged 15+ reflect the bulk of intended
recipients of information. This is potentially as users
still exhibit a lack of trust and/or preference for
human support for cases of the very young or elderly.
Figure 6 outlines primary symptoms selected by
users. As likely to be expected, the primary use case
for the app is for common acute illnesses. “Other
complaints” (not included in figure) include
conditions such as insect stings/bites, heart
palpitations, joint problems etc. which occur less
frequently but require more specialist knowledge.
Table 2 further elucidates symptom choices by
showing the ranking of main symptom selected in
November 2018, in the first 3 months, as well as in
February 2019, in the latter 3 months. Rank 1
indicates the most selected symptom, with
descending scores equating to decreased frequency of
selection. Symptom changes over time outlined in the
table indicate that there could be some seasonality in
symptom prevalence; for example, with vomit/nausea
and fever changing dramatically in ranking. This
could also point to the usefulness of digital tools in
predicting population level healthcare trends, for
example, the spread of illnesses as outlined in the
discussion later.
Figure 5: For whom the tool was used (by age and gender, total N=149 222).
The Doctor Will See Yourself Now: Review and Discussion of a Mass-market Self-service Technology for Medical Advice
801
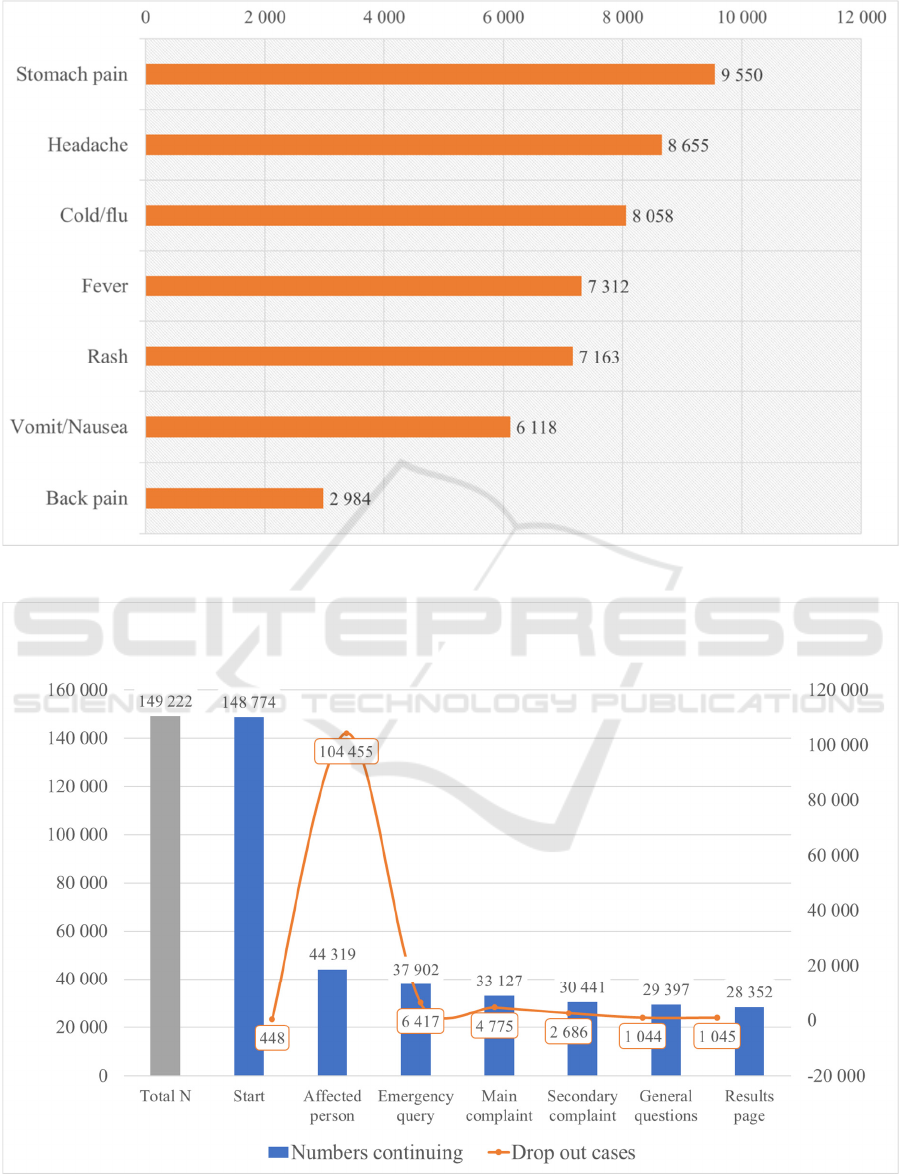
Figure 6: Primary symptoms selected (total N=149 222, other symptoms N=99 382).
Figure 7: App dialogue section / page visited.
Scale-IT-up 2020 - Workshop on Best Practices for Scaling-Up Digital Innovations in Healthcare
802
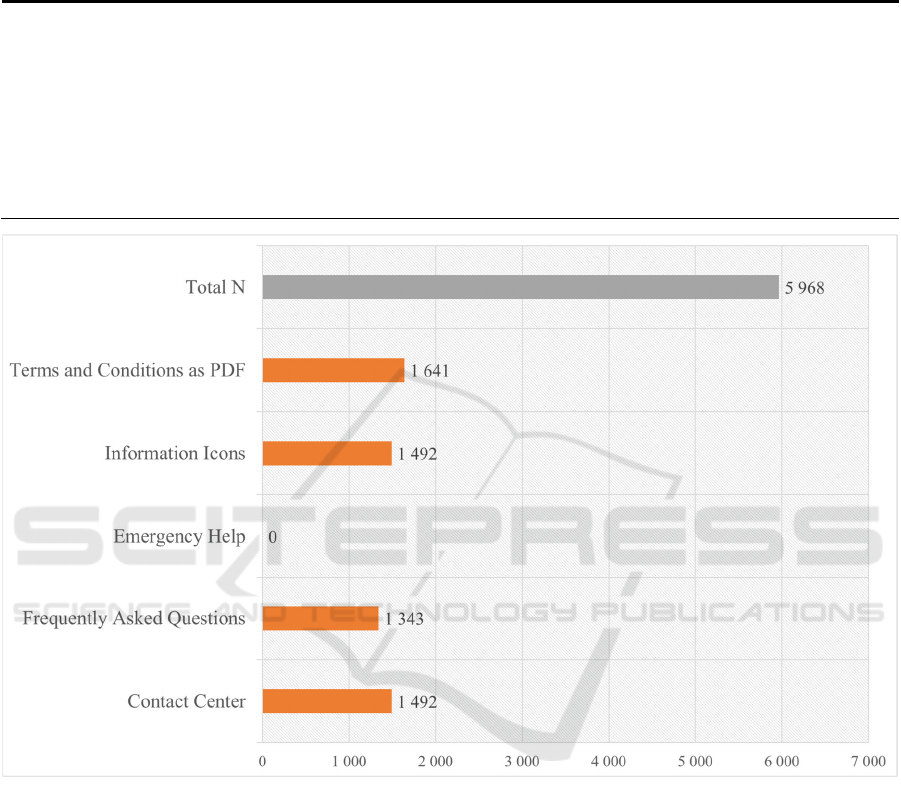
Table 2: Symptom ranking for 3 months usage (1 is highest rank).
Symptom
Ranking between Sept 2018 to
Nov 2018
Ranking between Dec 2018 to
Feb 2019
Ranking
change
Stomach pain 1 1 0
Headache 3 2 +1
Cold/flu 6 3 +3
Fever 14 4 +10
Rash 2 5 -3
Vomit/Nausea 18 6 +12
Back pain 5 12 -7
Figure 8: Buttons out of the optimal usage path.
Figure 7 shows the number of remaining
users/dropouts through each page/section of the app.
As can be evidenced, once users have begun the main
dialogue (i.e. talking about the affected person), the
majority continue through to the results page.
However, a large number of individuals drop out
between the start page and the affected person page.
This is possibly due to the request of the customer
insurance number, and subsequent fears around data
privacy, as explored further in the discussion.
Figure 8 outlines buttons clicked upon by the user,
removing them from the “optimal” usage path (i.e. the
most direct path to results, buttons that mayrequire
navigating back to main usage path). Buttons clicked
include; requiring terms and conditions as a PDF,
information icons (explaining medical
symptoms/jargon), frequently asked questions, and
contact center (i.e. how to contact a human for help).
Interestingly, there were no uses of the emergency
contact button; perhaps as individuals feared
requesting an ambulance by using the button, or
perhaps as users would prefer to use more traditional
channels in case of emergency. As also overviewed in
the discussion, these results hint at the importance of
including sufficient information within the main app
usage path, so as to not derail customers from the
intended usage/service experience.
The Doctor Will See Yourself Now: Review and Discussion of a Mass-market Self-service Technology for Medical Advice
803
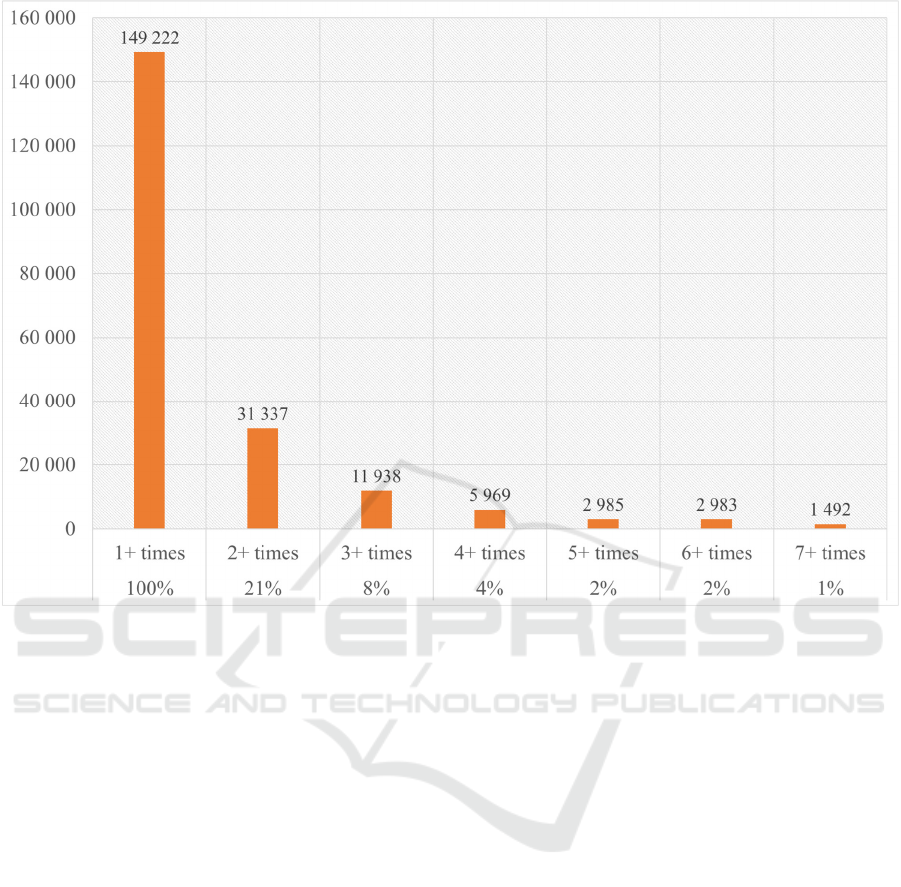
Figure 9: Buttons out of the optimal usage path
Finally figure 9 highlights the number of users
returning to use the medical tool again, with the
majority of users using the app only once. Figures
show that some individuals did return to use the app
again over the six-month period; 21% of users
(n=31 337) used the app two or more times, 8% three
or more times (n=11 938) and so on.
5 DISCUSSION AND FUTURE
RESEARCH
Trust in novel digital medical platforms and medical
services has been identified as of importance
previously (Mackert, Mabry-Flynn, Champlin,
Donovan, & Pounders, 2016; Moreira & Silva, 2015),
and for digital platforms more generally, trusting
preferences have been linked to both consumer and
platform characteristics (Komiak & Benbasat, 2006;
Metzger, 2006, 2007; W. Q. Wang & Benbasat,
2007). Usage statistics indicate that the app was
primarily used for older teenagers and adults, with
relatively fewer cases for more at-risk groups (i.e. the
young and elderly) where consequences of
misdiagnosis are more severe. In addition, primary
symptoms selected in the app were for common
complaints which typically consumers already have
an adequate level of health knowledge about (i.e.
cold, fever, rash). Thusly it appears that although
consumers welcome using these apps, they still
exhibit a degree of caution and mistrust about relying
on them for more serious medical queries, as also
further evidenced by no use of the emergency button
within the app. It would therefore be interesting to
examine how consumers react to using such digital
platforms, when the intended medical enquiry is more
severe, and something for future researchers to
investigate.
The number of app dialogue sections/pages
visited and the dropout rate is also interesting
considering heightened privacy concerns amongst the
general populace after recent well publicized scandals
(Isaak & Hanna, 2018; Zhang et al., 2018). Despite
attracting a large number of customers to the app
launch site, many dropped out when asked to provide
their customer insurance number and date of birth for
validation purposes, even though they were informed
no health data would be saved by the firm. Previous
research has identified the timing of consent is of
importance in disclosure decisions (Anderson &
Scale-IT-up 2020 - Workshop on Best Practices for Scaling-Up Digital Innovations in Healthcare
804

Agarwal, 2011), and one explanation therefore may
be that individuals were not significantly engaged
with the service offering before being asked to
provide information and thusly many left the app.
Alternatively, as user “emotions and resistances” may
stand in the way of successful digital health tools
(Lupton, 2013), it may be that individuals simply did
not believe the company when they stated no health
data would be saved yet also asked health insurance
customer number. As privacy disclosures are both a
legal requirement, and evidently of importance for
users, future research may wish to consider
alternative methods of framing privacy related
information which connects with individuals on a
meaningful level (Zhang et al., 2018).
In addition to privacy related information, further
service/usage experience information may also be of
benefit, as evidenced from the utilization of buttons
out of the main interaction path. Users selected to
receive further information related to privacy (e.g.
terms and conditions) or service matters (e.g.
frequently asked questions) indicating that service
roles were unclear (Solomon, Surprenant, Czepiel, &
Gutman, 1985). Expectation setting has been known
as importance in service evaluations (Ofir &
Simonson, 2007), and including extra information
within the main section of the app (particularly if it is
a dialogue based format as the current service) may
serve to “onboard” individuals to the service
experience (Rawson, Duncan, & Jones, 2013). This
has been found as particularly important in extant
research where service literacy is important
(Voorhees et al., 2017), which is likely the case with
novel digital products such as those employed in
healthcare.
The potential of use of such apps for health care
providers is also outlined when examining symptom
changes from 3 months and 6 months which show
changes in the ranking of symptoms, for example,
fever changing from ranked 14
th
to 4
th
. Previously
tracking symptom web searches and social media
posts has been used to predict influenza spread at both
population and sub-population levels (Santos &
Matos, 2014; Volkova, Ayton, Porterfield, & Corley,
2017). Thusly one could suppose that providing the
provision of these new tools was widespread enough,
and relevant permissions were given to healthcare
bodies to access the data, they may provide a highly
accurate data source for making predictions. This
may resolve some of the issues around inaccurate
information used for predictions, for example with
Google Flu (Kandula & Shaman, 2019). Future
research should also consider how such tools can be
monitored in terms of whether they successfully
prevent unnecessary emergency room or general
practitioner visits (Bahadori et al., 2018), or
successfully refer individuals to the correct healthcare
entry point.
Finally, repeat usage numbers show that there
exists some interest amongst the populace in
exploring digital healthcare tools. The current self-
service technology utilized a dialogue-type
interaction, guiding individuals through a linear path
to their results, in a dyadic manager mimicking
regular clinician-patient communication (McColl-
Kennedy et al., 2012; Sweeney et al., 2015). Virtual
agents such as text-based chatbots have been widely
applied to medical contexts to act as digital coaches
(Kowatsch et al., 2017), for example, the cognitive-
behavioral therapy chatbot “WoeBot” (Fitzpatrick,
Darcy, & Vierhile, 2017). It would be interesting to
discern whether making such self-services more
anthropomorphized would bring any benefits in terms
of repeat usage and minimizing drop outs in future
research, as anthropomorphism has been touted as a
key satisfaction driving mechanism for “service
robots” placed in the frontline (Wirtz et al., 2018).
For future practitioners seeking to implement
such digital tools, the authors would firstly note that
the number of total uses indicates a good appetite
amongst consumers to try such tools. Important
however, as noted earlier in the discussion, is to find
ways to successfully onboard users to the service
experience through use of supplementary
information. In particular, privacy concerns seem to
dominate, and a key recommendation for
practitioners wishing to roll out such digital self-
service technologies is to find ways to reduce user
privacy concern. This could be through the use of
additional privacy assurance disclosures, for
example, or not requesting customer details (e.g.
login information) immediately upon starting the
interaction.
6 SUMMARY AND NEXT STEPS
In summary results show that such digital self-service
technologies hold great potential with large numbers
of customers visiting the app site within a relatively
short time frame. However, the results also show that
trust in such digital services is not entirely established
yet, as evidenced by the large number of drop outs
after requesting the potentially sensitive customer
insurance number. In addition, the use cases for the
product seem to be for relatively benign complaints,
rarely for at-risk groups (young, elderly) and never in
the case of emergency. Future research should
The Doctor Will See Yourself Now: Review and Discussion of a Mass-market Self-service Technology for Medical Advice
805

examine how information relating to privacy and
service/usage experience can be made more
meaningful and/or clear to users, and whether this is
evidenced in changing use cases and usage patterns.
REFERENCES
Acquisti, A., Brandimarte, L., & Loewenstein, G. (2015).
Privacy and human behavior in the age of information.
Science, 347(6221), 509-514. doi:10.1126/science.
aaa1465
Ada. (2020). Ada: Your Digital Health Companion.
Retrieved from https://ada.com/
Anderson, C. L., & Agarwal, R. (2011). The Digitization of
Healthcare: Boundary Risks, Emotion, and Consumer
Willingness to Disclose Personal Health Information.
Information Systems Research, 22(3), 469-490.
doi:10.1287/isre.1100.0335
Bahadori, M., Teymourzadeh, E., & Mousavi, S. M. (2018).
eHealth solutions and nonurgent visits in emergency
departments. Technol Health Care, 26(3), 571-572.
doi:10.3233/THC-181290
Barello, S., Triberti, S., Graffigna, G., Libreri, C., Serino,
S., Hibbard, J., & Riva, G. (2015). eHealth for Patient
Engagement: A Systematic Review. Front Psychol, 6,
2013. doi:10.3389/fpsyg.2015.02013
Chua, M. E., Saunders, M. A., Bowlin, P. R., Ming, J. M.,
Lopes, R. I., Farhat, W. A., & Dos Santos, J. (2017).
Impact of smartphone digital photography, email, and
media communication on emergency room visits post-
hypospadias repair. Can Urol Assoc J, 11(3-4), E134-
E137. doi:10.5489/cuaj.4170
Fitzpatrick, K. K., Darcy, A., & Vierhile, M. (2017).
Delivering Cognitive Behavior Therapy to Young
Adults With Symptoms of Depression and Anxiety
Using a Fully Automated Conversational Agent
(Woebot): A Randomized Controlled Trial. JMIR Ment
Health, 4(2), e19. doi:10.2196/mental.7785
FSO. (2019). Health Pocket Statistics 2018. Switzerland:
Federal Statistics Office Retrieved from
https://www.bfs.admin.ch/bfs/en/home/statistics/health
/health-system.assetdetail.7347549.html
Hallfors, E., Saku, S. A., Makinen, T. J., & Madanat, R.
(2018). A Consultation Phone Service for Patients With
Total Joint Arthroplasty May Reduce Unnecessary
Emergency Department Visits. J Arthroplasty, 33(3),
650-654. doi:10.1016/j.arth.2017.10.040
Hassell, K., Rogers, A., & Noyce, P. (2000). Community
pharmacy as a primary health and self-care resource: a
framework for understanding pharmacy utilization.
Health Soc Care Community, 8(1), 40-49.
doi:10.1046/j.1365-2524.2000.00222.x
Hewner, S., Sullivan, S. S., & Yu, G. (2018). Reducing
Emergency Room Visits and In-Hospitalizations by
Implementing Best Practice for Transitional Care Using
Innovative Technology and Big Data. Worldviews Evid
Based Nurs, 15(3), 170-177. doi:10.1111/wvn.12286
Hibbard, J. H., & Peters, E. (2003). Supporting informed
consumer health care decisions: data presentation
approaches that facilitate the use of information in
choice. Annu Rev Public Health, 24, 413-433.
doi:10.1146/annurev.publhealth.24.100901.141005
Hwang, W., Liao, K., Griffin, L., & Foley, K. L. (2012). Do
free clinics reduce unnecessary emergency department
visits? The Virginian experience. J Health Care Poor
Underserved, 23(3), 1189-1204. doi:10.1353/hpu.
2012.0121
Isaak, J., & Hanna, M. J. (2018). User Data Privacy:
Facebook, Cambridge Analytica, and Privacy
Protection. Computer, 51(8), 56-59. doi:10.1109/mc.
2018.3191268
Kandula, S., & Shaman, J. (2019). Reappraising the utility
of Google Flu Trends. PLoS Comput Biol, 15(8),
e1007258. doi:10.1371/journal.pcbi.1007258
Kennedy, J. (2019). Populist politics and vaccine hesitancy
in Western Europe: an analysis of national-level data.
Eur J Public Health, 29(3), 512-516.
doi:10.1093/eurpub/ckz004
Komiak, & Benbasat. (2006). The Effects of
Personalization and Familiarity on Trust and Adoption
of Recommendation Agents. Mis Quarterly, 30(4).
doi:10.2307/25148760
Kowatsch, T., Nißen, M., Shih, C.-H. I., Rüegger, D.,
Volland, D., Filler, A., . . . Büchter, D. (2017). Text-
based Healthcare Chatbots Supporting Patient and
Health Professional Teams: Preliminary Results of a
Randomized Controlled Trial on Childhood Obesity.
Paper presented at the Persuasive Embodied Agents for
Behavior Change (PEACH2017) Workshop at the 17th
International Conference on Intelligent Virtual Agents.
Lupton, D. (2013). The digitally engaged patient: Self-
monitoring and self-care in the digital health era. Social
Theory & Health, 11(3), 256-270. doi:10.1057/
sth.2013.10
Lupton, D. (2016). Digital health technologies and digital
data: new ways of monitoring, measuring and
commodifying human bodies. Research handbook on
digital transformations, 85.
Mackert, M., Mabry-Flynn, A., Champlin, S., Donovan, E.
E., & Pounders, K. (2016). Health Literacy and Health
Information Technology Adoption: The Potential for a
New Digital Divide. J Med Internet Res, 18(10), e264.
doi:10.2196/jmir.6349
Mayer, G. G., Villaire, M., & Connell, J. (2005). Ten
recommendations for reducing unnecessary emergency
department visits. J Nurs Adm, 35(10), 428-430.
doi:10.1097/00005110-200510000-00003
McColl-Kennedy, J. R., Vargo, S. L., Dagger, T. S.,
Sweeney, J. C., & van Kasteren, Y. (2012). Health Care
Customer Value Cocreation Practice Styles. Journal of
Service Research, 15(4), 370-389. doi:10.1177/
1094670512442806
Metzger, M. J. (2006). Effects of Site, Vendor, and
Consumer Characteristics on Web Site Trust and
Disclosure. Communication Research, 33(3), 155-179.
doi:10.1177/0093650206287076
Scale-IT-up 2020 - Workshop on Best Practices for Scaling-Up Digital Innovations in Healthcare
806

Metzger, M. J. (2007). Communication Privacy
Management in Electronic Commerce. Journal of
Computer-Mediated Communication, 12(2), 335-361.
doi:10.1111/j.1083-6101.2007.00328.x
Moreira, A. C., & Silva, P. M. (2015). The trust-
commitment challenge in service quality-loyalty
relationships. Int J Health Care Qual Assur, 28(3), 253-
266. doi:10.1108/IJHCQA-02-2014-0017
Murphy, M. (2019). Dr Google will see you now: Search
giant wants to cash in on your medical queries.
Retrieved from https://www.telegraph.co.uk/techno
logy/2019/03/10/google-sifting-one-billion-health-
questions-day/
Murphy, S. M., & Neven, D. (2014). Cost-effective:
emergency department care coordination with a
regional hospital information system. J Emerg Med,
47(2), 223-231. doi:10.1016/j.jemermed.2013.11.073
NHS. (2020). Health A-Z. Retrieved from
https://www.nhs.uk/conditions/
Ofir, C., & Simonson, I. (2007). The effect of stating
expectations on customer satisfaction and shopping
experience. Journal of Marketing Research, 44(1), 164-
174. doi:DOI 10.1509/jmkr.44.1.164
Paasche-Orlow, M. K., Parker, R. M., Gazmararian, J. A.,
Nielsen-Bohlman, L. T., & Rudd, R. R. (2005). The
prevalence of limited health literacy. J Gen Intern Med,
20(2), 175-184. doi:10.1111/j.1525-1497.2005.
40245.x
Rawson, A., Duncan, E., & Jones, C. (2013). The truth
about customer experience. Harvard Business Review,
91(9), 90-98.
Rieffe, C., Oosterveld, P., Wijkel, D., & Wiefferink, C.
(1999). Reasons why patients bypass their GP to visit a
hospital emergency department. Accident and
Emergency Nursing, 7(4), 217-225. doi:10.1016/s0965-
2302(99)80054-x
Santos, J. C., & Matos, S. (2014). Analysing Twitter and
web queries for flu trend prediction. Theor Biol Med
Model, 11 Suppl 1, S6. doi:10.1186/1742-4682-11-S1-
S6
Soldaini, L., & Goharian, N. (2017). Learning to rank for
consumer health search: a semantic approach. Paper
presented at the European conference on information
retrieval.
Solomon, M. R., Surprenant, C., Czepiel, J. A., & Gutman,
E. G. (1985). A Role Theory Perspective on Dyadic
Interactions: The Service Encounter. Journal of
Marketing, 49(1). doi:10.2307/1251180
Sweeney, J. C., Danaher, T. S., & McColl-Kennedy, J. R.
(2015). Customer Effort in Value Cocreation Activities:
Improving Quality of Life and Behavioral Intentions of
Health Care Customers. Journal of Service Research,
18(3), 318-335. doi:10.1177/1094670515572128
Volkova, S., Ayton, E., Porterfield, K., & Corley, C. D.
(2017). Forecasting influenza-like illness dynamics for
military populations using neural networks and social
media. PLoS One, 12(12), e0188941.
doi:10.1371/journal.pone.0188941
Voorhees, C. M., Fombelle, P. W., Gregoire, Y., Bone, S.,
Gustafsson, A., Sousa, R., & Walkowiak, T. (2017).
Service encounters, experiences and the customer
journey: Defining the field and a call to expand our lens.
Journal of Business Research, 79, 269-280.
doi:10.1016/j.jbusres.2017.04.014
Wang, W.-T., Cheng, S.-Y., & Huang, L.-Y. (2013).
Technology-Based Service Encounters Using Self-
Service Technologies in the Healthcare Industry.
International Journal of Human-Computer Interaction,
29(3), 139-155. doi:10.1080/10447318.2012.695728
Wang, W. Q., & Benbasat, I. (2007). Recommendation
agents for electronic commerce: Effects of explanation
facilities on trusting beliefs. Journal of Management
Information Systems, 23(4), 217-246.
doi:10.2753/Mis0742-122230410
Wirtz, J., Patterson, P. G., Kunz, W. H., Gruber, T., Lu, V.
N., Paluch, S., & Martins, A. (2018). Brave new world:
service robots in the frontline. Journal of Service
Management, 29(5), 907-931. doi:10.1108/josm-04-
2018-0119
Xie, B. (2011). Effects of an eHealth literacy intervention
for older adults. J Med Internet Res, 13(4), e90.
doi:10.2196/jmir.1880
Zhang, X., Liu, S., Chen, X., Wang, L., Gao, B., & Zhu, Q.
(2018). Health information privacy concerns,
antecedents, and information disclosure intention in
online health communities. Information &
Management, 55(4), 482-493. doi:10.1016/j.im.2017.
11.003
The Doctor Will See Yourself Now: Review and Discussion of a Mass-market Self-service Technology for Medical Advice
807
