
Overcrowding in the Emergency Department: Could a
Patient-centred Mobile App Change This Paradigm?
Inês Margarido
1
, Ntumba Kasonga Alpha
2
, Nduami Junior
3
and Jan Marin
4
1
Faculty of Medicine of University of Lisbon, Portugal
2
Institut Supérieur d’Ingénieurs de Franche-Comté, Université de Bourgogne, Besançon, France
3
Biomedical Department, Ecole Centrale de Lille, Villeneuve d’Ascq, France
4
School of Design, Zagreb, Crotia
Keywords: Emergency Department, Overcrowding, Self-Referral.
Abstract: Overcrowding in the emergency department has been a growing worldwide problem. Some solutions have
been put forth in the several points of the patient’s path mostly in order to provide a more efficient flow of
patients within the ED. We propose, in this paper, a mobile app that could integrate real-time information of
patients, emergency departments, medical emergency teams and general practitioners. This could help scatter
the non-linear flow of patients before they arrive and ultimately improve not only quality of care but also
better patient outcomes.
1 INTRODUCTION
Emergency Department (ED) overcrowding has been
described as both a patient safety issue and a global
healthcare issue (Pines and Griffey 2015). There is
much debate as to the causes of the phenomenon,
leading to difficulties in developing successful,
targeted solutions. Approximately half of EDs all
over the world report operating near or above
maximum capacity.
Some definitions of ED overcrowding have been
put forth, but in its simplest form, overcrowding
exists when there is no space left to meet the timely
needs of the next patient requiring emergency care
(Salway et al. 2017). If the care of urgent problems is
delayed due to congestion, then overcrowding exists.
This can occur due to the volume of patients
waiting to be seen (input), delays in assessing or
treating patients already in the ED (throughput), or
impediments to patients leaving the ED once their
treatment has been completed (output) (Asplin et al.
2003).
Consequently, there are likely to be many
different causes of overcrowding, depending on when
and where in the patient journey the crowding occurs.
2 WHAT ARE THE CAUSES AND
CONSEQUENCES OF
OVERCROWDING?
2.1 Causes
In order to address this issue and provide the right
solutions, we must see at which point of the cascade
of functioning in the ED is the problem.
In the input of patients, we can point out a non-
linear presentation flow or presentations with more
urgent and complex care needs (Aboagye-Sarfo et al.
2015), increase in presentations by the elderly, high
volume of low-acuity presentations (Bond et al.
2006), limited access to primary care or diagnostic
services in community (Cowling et al. 2013).
During their time in the department, several
causes can be addressed like ED healthcare staff
shortages, presence of junior medical staff, delays in
receiving test results and delayed disposition
decisions (Van Der Linden et al. 2017).
When it comes to the output of patients some of
the reasons pointed out were the slow administrative
procedure to discharge patients and the unavailability
for admission of certain specialities in public
hospitals (Dunn 2003).
Margarido, I., Alpha, N., Junior, N. and Marin, J.
Overcrowding in the Emergency Department: Could a Patient-centred Mobile App Change This Paradigm?.
DOI: 10.5220/0009365303630367
In Proceedings of the 13th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2020) - Volume 1: BIODEVICES, pages 363-367
ISBN: 978-989-758-398-8; ISSN: 2184-4305
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
363

2.2 Consequences
This ED crowding leads to several consequences that
can be divided in whether patient, staff or system
related.
Effects on patients include delays in being
assessed and in receiving required care, increased
frequency of exposure to error, reduced patient
satisfaction, increased inpatient length of stay
(IPLOS) and poorer outcomes such as increased
inpatient mortality and risk of readmission (Jo et al.
2015).
When it comes to the staff, the negative effects
include increased stress and exposure to violence and
non-adherence to best practice guidelines during
times of ED overcrowding, such as increased time to
assessment of pain and/or delays in the administration
of analgesics or delayed administration of antibiotics
during ED crowding (Tsai et al. 2016).
System-level consequences identified were those
that led to `bottle-necks' in the system, namely
increases in length of stay (LOS), both within the ED
itself (EDLOS) and for those patients admitted to the
hospital (IPLOS) and ambulance diversion. Again,
these could also be viewed as consequences for
patients.
3 WHAT HAS BEEN DONE?
Several solutions have been put forward. We can also
divide these solutions according to the point of
journey in the ED.
On the issue of the input of patients some of the
studied and suggested solutions are a co-located
general practitioner (GP) in the ED (Anantharaman
2008), extended GP opening hours, choice of ED
(Sharma and Inder 2011) and social interventions
including education campaigns, financial
disincentives, redirection.
On the question of the throughput of patients there
are shown results in installing a fast-track, bedside
registration, ED nurse flow coordinator, nurse-
initiated protocols, increased ED bed numbers and
staff (Tenbensel et al. 2017), shorter turnaround-
times for laboratory tests, etc.
Solutions looking at output factors include
measurements such as active bed management
(Burley et al. 2007), leadership programs,
implementation of nationally mandated (Sullivan et
al. 2014), timed patient disposition targets, admitting
team prioritising ED admissions and increased
inpatients beds and staff.
Even if all these initiatives could be implanted,
hospitals are not immune to issues of overcrowding
and poor coordination of patient admissions,
transfers, and discharges. None of these has been
proved as the perfect solution.
4 HOW WE GOT HERE
In a systematic review (Morley et al. 2018), there was
a mismatch between proposed solutions and found
causes of ED overcrowding. Most of the solutions
presented are focused on an efficient patient flow
within the ED but a larger part of causes was
associated with the amount and type of people
attending the ED.
To tackle the problem at its origin, we believe that
a greater focus must be given to the upstream part of
the process, this meaning that our focus point are the
incoming patients. Thus, we plan on educating the
patients and reorient them towards sites capable of
hosting them depending on their need by focusing on
patients who direct themselves to the ED by personal
choice.
Indeed, and according to the Panorama des ORU,
activité des structures d’Urgence 2016, from
FEDORU (Fédération des Observatoires Régionaux
des Urgences), about 75% of the arrivals to the
emergency department were made by personal
choice. From 2015 to 2016 there was an increase of
approximately 4% in the visits to the ED. When it
comes to the hospitalizations, only 21% of them are
admitted to the hospital. The age mean of patients
going to the ED is 39 years old and only 13% of the
total of patients are more than 75 years old or less.
Another study group found that between 41.2 to
51.9% of self-referred patients in a Dutch ED visited
the ED inappropriately (Kraaijvanger et al. 2016).
4.1 Self-referrals at the ED
Taking these statistics into consideration, one must
investigate the reasons that motivate patients to visit
the ED directly, especially those with a non-urgent
condition.
A considerable number of studies has been made
in order to characterize these factors. Reasons such as
expecting investigations and wanting to see a doctor
and have tests or further research done in the same
place have been identified. The convenience of ED,
for example, convenience of access, ED nearby or the
idea that the patient could get help earlier at the ED is
also described as a major factor that influences this
kind of behaviour (Kraaijvanger et al. 2017).
ClinMed 2020 - Special Session on Designing Future Health Innovations as Needed
364
5 THE APP
We believe that in order to solve this problem of input
patients the solution that to be put forward must
combine multiple functionalities. Our approach
would put the decisions of the patient in its own
hands.
With the amount of information available online,
it’s difficult to consider only trustworthy information,
especially if one has not got a clear understanding
about the area. Therefore, there is a pressing need to
educate the population with the right knowledge in
order to prevent inappropriate trips to the ED.
By promoting health literacy, we are confident
that perhaps it could decrease the number of
unnecessary trips to the ED that end up causing
congestion on the first steps of the patient pathway
(for example the registration and triage).
Another feature of the app would be the
localization of the nearest emergency departments
and its respective waiting time. This would lead to a
more scattered flow of patients. In this way, the most
central hospitals could decrease their congestion of
ED while the outer hospitals could improve their own
flow.
There is also an urgent need to keep the
emergency medical teams updated in real-time about
the availability of the different EDs. The several ways
that patients can get to the ED must be taken into
account in order to make everything work together
through a better and faster communication with the
common purpose of redirecting correctly them to the
place where they can have the better care provided.
As we mentioned, a lot of the self-referrals on the
ED could simply be treated at a GP. This said, by
providing the availability of the local GPs we believe
that a small part of the flow could be redirected to
primary care.
6 HOW IT WORKS?
We trust that the first step to reduce the number of
non-vital patient visits in EDs, or direct them to a
primary care facility, is through a simple yet
sufficient education of the population. In this way,
they would use a device to educate themselves. The
mobile-app provides simple guidelines and
information about some medical topics that the users
can access to inform themselves about their own
pathologies, to comprehend how urgent is their
problem, if that is the case, or just to keep updated
about hot topics of the world medicine. The
guidelines used would be adapted from NICE
guidelines (National Institute of Health and Care
Excellence) or BMJ Best Practices Medicine
guidelines (British Medical Journal) for different
symptoms.
The patients will also have the possibility to check
the nearest GP and their availability with the option
to book an appointment if desired. This would be a
choice made by the patient if decides to do so.
Besides, the app would provide also the availability
and waiting times of the nearest EDs, if the patient
chooses to truly make use of the department. A map
would then be provided, and the best option of ED
will be recommended based on distance and waiting
times even though the patient can choose another one
that could be more suitable to his situation.
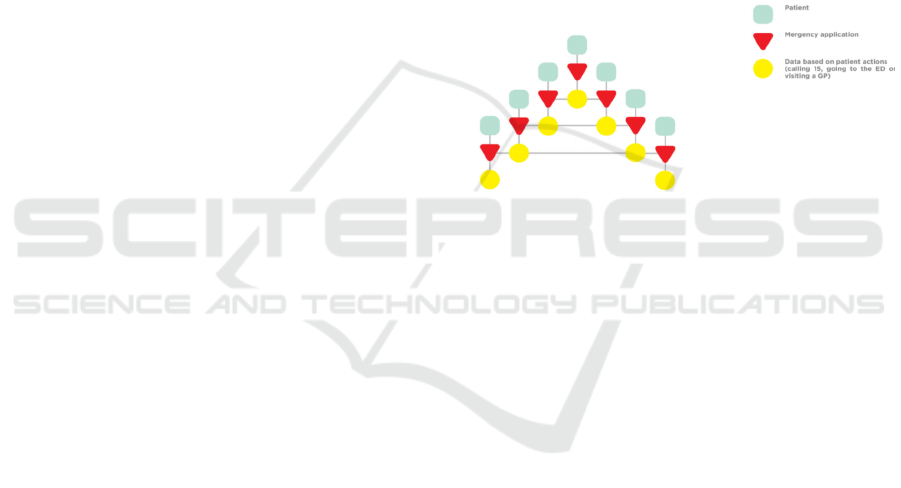
Figure 1: Decision making tree of the patients on our app.
By pressing the start button in the map, patient’s
data would be sent to the choosing ED and real time
updating of the arrival of patient would be done using
GPS tracking of their device. It will be, therefore,
possible to trace the patient and record their data
throughout the whole process. It is necessary to
mention that the data needed here has no other
purpose than tracing so in other words no name or
other type of personal data is needed for our goal.
During registration, already in the ED, patient’s
data will be converted and quantified to number of
patients in the ED and recorded both from the patient
using our app and those coming by their own.
These data will be redirected to emergency
medical teams in order to provide them with real-time
availability of each ED and therefore help by
improving the effectiveness and speed of reallocation
of different patients to different hospitals.
7 IMPLEMENTATION
This software is not a medical device as its intended
purpose is purely informative based on collected data
and international medical guidelines, it is not planned
Overcrowding in the Emergency Department: Could a Patient-centred Mobile App Change This Paradigm?
365

to serve as a diagnostic tool, a therapeutic tool nor a
measuring instrument.
This type of software has many features and each
of them must be clinically tested to validate the safety
of the product and to have more credibility on the
market. A clinical investigation must be done in order
to evaluate not only the effectiveness and efficiency
of the international medical guidelines contained in
the application but also the effectiveness in its
purpose of scattering the flow of the EDs.
A pilot study would have to be performed in the
form of a randomized single-blinded, control trial
with a quantitative and qualitative prospective
evaluation of the effectiveness and efficiency of the
medical guidelines contained in this software on 150
participants for 6 months. Our purpose is to evaluate
the app, if it is useful and if it promotes efficiency but
further work is needed to find the best way to evaluate
this kind of application.
8 CHALLENGES
This idea was thought out in the emergency
department with the insights of experienced doctors
and experts of the medical emergency teams, but it
lacked the patient’s point of view on this subject.
Therefore, a questionnaire or a study must be done
taking into consideration whether the patients would
be interested and make use of an app of this kind.
To make it operational and, since it is built on its
utilization by users, this mobile app must be greatly
diffused in the community, in order to reach a great
number of users. It is crucial that the dissemination of
the app is done in a rightful way.
Also, another drawback of this idea is that the app
needs to be adapted into each city, town or country
individually because the health organisation structure
could be different from one city to the other even in
the same country.
Other possible challenge would be the willingness
of the several hospitals to redirect patients to other
structures. This possibility requires a tough
negotiation with the several directions of the hospitals
of the area.
The most important challenge of this app would
be necessity to ensure that patients with a life-
threatening condition do not make the wrong
decision. Our app would only advise patients and
provide them with the necessary information for them
to make a conscious and informed decision on
whether or which ED to go to. Therefore, the question
of the responsibility of the application information
regarding the risks linked to the medical information
provided must be addressed.
9 CONCLUSIONS
It is undeniable that the problem of overcrowding
must be addressed. According to literature, there’s a
lack of solutions when it comes to the inflow of
patients therefore we strongly believe that this idea
embodies the most economical and most profitable
solution to the issue of overcrowding in the EDs, as it
gives patients the power to regulate their inflow with
the help of emergency medical teams.
We are convinced that if we give the patient the
possibility to make an informed and well-thought
choice, we could somehow manipulate the pathway
of the less-urgent patients.
ACKNOWLEDGEMENTS
This work was developed in the EIT Health ClinMed
2019 Summer School for Innovative Technologies in
Health with the support of many professionals to
whom we would like to present our most thoughtful
thanks.
To Jessica Schiro and Sylvia Pelayo from CIC-IT
Lille, who had an unwearyingly availability to answer
all our questions and guide us throughout the summer
school.
To Dr. François Dubos and Dr. Gregory Smith,
both medical doctors from the Lille Hospital, and Dr.
Facon from Lille Medical Emergency Regulation
Center (S.A.M.U) who shared with us their time and
thoughts on this problem.
Also, we would like to thank the Forum des Living
Lab en Santé et Autonomie for the opportunity to be a
part of such an amazing immersive experience.
REFERENCES
Aboagye-Sarfo, Patrick et al. 2015. “Growth in Western
Australian Emergency Department Demand during
2007-2013 Is Due to People with Urgent and Complex
Care Needs.” EMA - Emergency Medicine Australasia
27(3): 202–9.
Anantharaman, V. 2008. “Impact of Health Care System
Interventions on Emergency Department Utilization
and Overcrowding in Singapore.” International
Journal of Emergency Medicine 1(1): 11–20.
ClinMed 2020 - Special Session on Designing Future Health Innovations as Needed
366

Asplin, Brent R. et al. 2003. “A Conceptual Model of
Emergency Department Crowding.” Annals of
Emergency Medicine 42(2): 173–80.
Bond, Kenneth et al. 2006. Frequency, Determinants, and
Impact of Overcrowding in Emergency Departments in
Canada: A National Survey of Emergency Department
Directors.
Burley, Gwendolyn, Heather Bendyk, and Catherine
Whelchel. 2007. “Managing the Storm: An Emergency
Department Capacity Strategy.” Journal for healthcare
quality : official publication of the National Association
for Healthcare Quality 29(1): 19–28.
Cowling, Thomas E. et al. 2013. “Access to Primary Care
and Visits to Emergency Departments in England: A
Cross-Sectional, Population-Based Study.” PLoS ONE
8(6): 6–11.
Dunn, Robert. 2003. “Reduced Access Block Causes
Shorter Emergency Department Waiting Times: An
Historical Control Observational Study.” Emergency
Medicine 15(3): 232–38.
Jo, Sion et al. 2015. “ED Crowding Is Associated with
Inpatient Mortality among Critically Ill Patients
Admitted via the ED: Post Hoc Analysis from a
Retrospective Study.” American Journal of Emergency
Medicine 33(12): 1725–31. http://dx.doi.org/10.1016/
j.ajem.2015.08.004.
Kraaijvanger, Nicole et al. 2016. “Self-Referrals in a Dutch
Emergency Department: How Appropriate Are They?”
European Journal of Emergency Medicine 23(3): 194–
202.
Kraaijvanger, Nicole, Henk Van Leeuwen, Douwe
Rijpsma, and Michael Edwards. 2017. “Motives for
Self-Referral to the Emergency Department : A
Systematic Review of the Literature.” BMC Health
Services Research (2016): 1–19.
Van Der Linden, M. Christien et al. 2017. “Two Emergency
Departments, 6000 Km Apart: Differences in Patient
Flow and Staff Perceptions about Crowding.”
International Emergency Nursing 35: 30–36.
http://dx.doi.org/10.1016/j.ienj.2017.06.002.
Morley, Claire et al. 2018. “Emergency Department
Crowding : A Systematic Review of Causes ,
Consequences and Solutions.” : 1–42.
Pines, Jesse M., and Richard T. Griffey. 2015. “What We
Have Learned from a Decade of ED Crowding
Research.” Academic Emergency Medicine 22(8): 985–
87.
Salway, RJ et al. 2017. “Emergency Department (ED)
Overcrowding: Evidence-Based Answers to Frequently
Asked Questions.” Revista Clínica Las Condes 28(2):
213–19. http://dx.doi.org/10.1016/j.rmclc.2017.04.008.
Sharma, Anurag, and Brett Inder. 2011. “Impact of Co-
Located General Practitioner (GP) Clinics and Patient
Choice on Duration of Wait in the Emergency
Department.” Emergency Medicine Journal 28(8):
658–61.
Sullivan, Clair M. et al. 2014. “Aiming to Be NEAT: Safely
Improving and Sustaining Access to Emergency Care
in a Tertiary Referral Hospital.” Australian Health
Review 38(5): 564–74.
Tenbensel, Tim et al. 2017. “New Zealand’s Emergency
Department Target - Did It Reduce ED Length of Stay,
and If so, How and When?” BMC Health Services
Research 17(1).
Tsai, Ming Ta et al. 2016. “The Influence of Emergency
Department Crowding on the Efficiency of Care for
Acute Stroke Patients.” International Journal for
Quality in Health Care 28(6): 774–78.
Overcrowding in the Emergency Department: Could a Patient-centred Mobile App Change This Paradigm?
367
