
The Use of Virtual Reality Applications in Stroke Rehabilitation for
Older Adults: Technology Enhanced Relearning
Peter Mozelius, Awais Ahmad and Karin Ahlin
Department of Computer and System Science, Mid Sweden University, Östersund, Sweden
Keywords: Stroke Rehabilitation, Virtual Reality, e-Health, Technology Enhanced Relearning, Older Adults.
Abstract: After stroke rehabilitation is a long-term relearning process that can be divided into cognitive relearning,
speech relearning and motoric relearning. Today with an aging population it it interesting to look at technology
enhanced and game-based solutions that can facilitate independent living for older adults. The aim of the
study was to identify and categorise recently conducted research in the field of virtual reality applications for
older adults' relearning after stroke. This study was conducted as a systematic literature review with results
categorised in a pre-defined framework. Findings indicate that virtual reality-based stroke rehabilitation is an
emerging field that can renew after stroke rehabilitation. Most found studies were on stroke patients' motoric
and game-based relearning, and with less studies on speech rehabilitation. The conclusion is that virtual reality
systems should not replace the existing stroke rehabilitation, but rather to have the idea of combining and
extending the traditional relearning process where human-to-human interaction is essential. Finally, there are
no virtual reality applications that can fit all stroke patients' needs, but a thoughtful selection of exercises that
matches each individual user would have a potential to enhance the current relearning therapy for older adults
after stroke.
1 INTRODUCTION
Stroke is a serious and global health-care problem
that has been identified as the most common reason
for disability worldwide (Hoffmann, 2001;
Langhorne, Bernhardt & Kwakkel, 2011; Gamito et
al., 2017). For stroke survivors, rehabilitation is a
crucial and long-term challenge that requires
motivation and hard work from the patients and also
extensive resources from the health care providers
(Broeren et al., 2008). The way back to an
independent and joyful life after stroke is often a long
journey where patients as well as relatives together
have to struggle for a successful relearning (Greveson
& James, 1991; (Broeren et al., 2008). A stroke
patient’s disability could be divided into the
categories of motor, speech and cognitive injuries,
where the cognitive part of the rehabilitation is related
to the motoric and speech aspects of a patient’s
relearning after stroke.
The motoric rehabilitation deals with problems
using the body, while speech rehabilitation is related
to problems with language and communication. Both
impairments drastically reduce the ability to read,
write, communicate and interact (Seniów, Litwin &
Lesniak, 2009, Langhorne et al., 2011, Veerbeek et
al., 2014, Pollock et al., 2014, Toussignant et al.,
2018). Effective rehabilitation should be built around
an everyday treatment, which is challenging to
provide due to the high amount of human resources
and running costs that are involved. On the other
hand, several technology-enhanced alternatives have
emerged that have a potential to complement the
traditional long-term rehabilitation. This study had a
focus on identifying and discussing virtual reality
applications that have been part of post stroke
rehabilitation.
1.1 Aim and Research Question
The aim of this study was to identify and categorise
recently conducted research in the field of virtual
reality applications for older adults’ relearning after
stroke. The main research question to answer was:
“Which are the lessons learnt in technology enhanced
stroke rehabilitation for older adults using virtual
reality applications?”.
Mozelius, P., Ahmad, A. and Ahlin, K.
The Use of Virtual Reality Applications in Stroke Rehabilitation for Older Adults: Technology Enhanced Relearning.
DOI: 10.5220/0009354201450155
In Proceedings of the 6th International Conference on Information and Communication Technologies for Ageing Well and e-Health (ICT4AWE 2020), pages 145-155
ISBN: 978-989-758-420-6
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
145

2 EXTENDED BACKGROUND
Virtual reality has been an emerging trend in the 21st
century, and the technical level is today far better than
it was in the previous century. In tandem with the
technical development, virtual reality systems have
been implemented and tested in a huge number of
areas, and quite frequently in health care.
2.1 Virtual Reality
Virtual reality has generally been defined as a
computer-generated three-dimensional artificial
environment that creates imitated reality (Pesonen et
al., 2017). That imitated reality generates a feeling of
a real-looking world which allows the user interaction
as well; a user can interact by performing different
kind of actions such as verbal commands, and
different kind of physical and facial gestures
(Glännfjord et al., 2017). Furthermore, virtual reality
could be divided into several types of environments
that can be immersive, semi-immersive and non-
immersive. The full immersive could be a cave
environment, whilst the semi-immersive type could
be exemplified by a flight simulator. Finally, the non-
immersive type consists of applications using the
desktop system for viewing. Non-Immersive systems
are the most basic ones offering a less powerful
experience of being present than that the immersive
virtual world systems can afford (Peters et al., 2016).
Virtual reality is considered an alternative for
different types of physical and cognitive
rehabilitation following stroke (Yamato et al., 2016).
The use of virtual reality provides the possibility of
strictly controlled user interaction (Brahnam & Jain,
2011), that might be used for different types of post
stoke therapies such as cognitive training for re-
learning of daily routine tasks (Gamito et al., 2017)
and upper limb dysfunction therapy following stroke
(Yates et al., 2016). Many of the stroke rehabilitation
interventions involve intensive and highly repetitive
exercises and the treatments involving virtual reality
can be useful not only for the patients but it may also
decrease the treatment costs and human resources for
medical caregivers (Yamato et al., 2016).
2.2 Theoretical Framework
Stroke rehabilitation could primarily be divided into
the categories of: cognitive relearning, speech
relearning and motoric relearning (Ahmad, Mozelius
& Ahlin, 2019). Furthermore, technology enhanced
stroke rehabilitation might be sub-classed into a
category of game-based relearning (Mozelius, Ahlin
& Ahmad, 2019). These four categories described
below, was used as a theoretical framework for the
deductive thematic analysis in this study.
2.2.1 Cognitive Relearning
A fundamental part of the rehabilitation after stroke
is the cognitive relearning, therefore, it is important
to carefully examine the patient’s cognition status
before the rehabilitation starts (Skidmore et al., 2010,
Heruti et al., 2002). The vast majority of stroke
rehabilitation exercises need basic cognitive abilities
for a successful memorising and relearning. Various
cognitive deficiency can make it difficult to perform
the rehabilitation exercises (Heruti et al., 2002).
Therefore, a patient's cognitive skills determine the
overall strategy of different types of rehabilitation and
relearning following a stroke. The vast majority of
stroke survivors are reported to have some kind of
cognitive impairment that can have a negative impact
on the patients' daily life activities (Palmcrantz et al.,
2017).
Most stroke patients are depending on long-term
cognitive rehabilitation process to recover (Cogollor
et al., 2018). Even mild cognitive impairments after
stroke can affect things such as a patient’s
independent living, the quality of life and the
occupational effectiveness (Jokinen et al., 2015). Due
to brain damage, the cognitive impairments can also
cause issues such as attention deficits, memory loss,
spatial neglect and perceptual disorders. There exist
various exercises that can improve the attention and
alertness for patients with attention deficiencies
(Langhorne et al., 2011, Jokinen et al., 2015), and
several types of therapies can be suggested for
relearning and cognitive improvements. However,
the type of rehabilitation is always depending on each
patient’s specific impairments.
2.2.2 Speech Relearning
Language and speech related dysfunctions have been
classified as a condition called aphasia. Aphasia is a
common stroke impairment phenomenon where
patients’ cognitive ability might not be decreased, but
that parts of their speaking, reading and/or writing
skills are damaged (Tousignant et al. 2018). Close to
a third of stroke patients suffer from some kind of
aphasia (Tousignant et al. 2018; Greener, Enderby &
Whurr, 1999) In the first weeks after a stroke, many
speech and language impairments recover, but the
rest of the relearning can take years of repeated
training with speech and language therapy as an
important part of the recovery process (Gerstenecker
& Lazar, 2019). Several research studies indicate that
ICT4AWE 2020 - 6th International Conference on Information and Communication Technologies for Ageing Well and e-Health
146

the quality of life for aphasia patients is severely
affected, and linked to emotional suffering,
communication disorders and social limitations
(Hilari et al., 2003; Ross & Wertz, 2003; Øra et al.,
2018).
Moreover, aphasia patients often suffer from
anomia, where the word retrieval fails and the person
cannot express what they want they want to say. This
creates major problems in a patient’s daily life with
misunderstandings and a reduced social life
(Tousignant et al. 2018). Due to the speech and
language issues suffer from to not be able to express
emotions and to share thoughts and knowledge. A
constant lack of expressions that can lead to isolation
and to states of deep frustration (Johansson, Carlsson
& Sonnander, 2012). Another consequence of speech
inability the increased uncertainty, where patients
become uncertain about what has been said and what
has been understood. This also leading to doubts
about what was planned, which also affects the
patient’s relatives and friends (Øra et al., 2018).’
2.2.3 Motoric Relearning
Almost all stroke patients experience some motor
impairments that limit their physical activity and the
ability to carry out daily routine tasks (Langhorne et
al., 2009, Palmcrantz et al., 2017). To support
motoric relearning and to increase the quality of
patient's life, intense and long-term physical training
is required. This is a long-term process that should be
started as early as possible after a stroke (Ehn et al.,
2015). Many of the currently most used treatments for
motoric relearning involve physiotherapy and guided
physical exercises, and the perceived benefits are
obvious (Veerbeek et al., 2014).
In the 21st century, several types of technology-
enhanced systems have been tested in motoric
rehabilitation of stroke patients. The various systems
have their various identified benefits, drawbacks and
limitations (Rizzo & Kim, 2005, Broeren et al., 2008,
Palmcrantz et al., 2017). In the rich number of novel
relearning therapies that has been developed and
tested there are also many examples that use virtual
reality techniques. Some early 21st century examples
using ankle and wrist devices for stroke rehabilitation
have been described by Deutsch et al. (2001) and Jack
et al. (2001). Finally, as pointed out by Porras et al.
(2018), motor rehabilitation techniques involving
virtual reality is an emerging field that has had a rapid
and promising development during the last decade.
2.2.4 Game-based Relearning
At the same time as the variety of digital games has
increased and reached a wider audience (Juul, 2010),
games have been frequently involved in several
aspects of learning. A game-based learning approach
has been tested in a wide range of areas such as
computer programming (Malliarakis, Satratzemi &
Xinogalos, S. (2014), history education (Mozelius et
al., 2017) and melanoma recognition (Maganty et al.,
2018). The combination of virtual reality and games
has been found to increase patients’ interest and
enthusiasm in the rehabilitation process (Brahnam &
Jain, 2011).
Different types of VR based gaming systems such
as Xbox Kinect and Wii seem to have some potential
benefits in terms of accessibility, usability, and
affordability (Yates et al., 2016). Deutsch et al.
(2011) studied how exergames were used on the
Nintendo Wii platform to improve balance and
mobility for post-stroke patients. An interesting
setup, but a lesson learnt was that a game-based setup
for stroke patients also requires a careful pre-
evaluation of the involved games (Deutsch et al.,
2011). Finally, an interesting and more specalised
approach to rehabilitation after stroke, could be to
develop and use task-specific game-based virtual
reality systems (Shin, Ryu & Jang, 2014).
3 METHOD
This study was carried out as a systematic literature
review according to the step-by-step approach for
health science research presented by Parahoo (2006)
and Cronin, Ryan and Coughlan (2008). First step
was to select a topic and to formulate the research
question that is presented in the end of the
introduction. Second step was to define inclusion and
exclusion criteria for a set of articles that represent the
status quo of the chosen field. The second step is
closely aligned to the third step of selecting and
accessing the literature, where the recommendation is
to combine pre-defined keywords in a search string
(Ely & Scott, 2007). Fourth step then is to assess the
quality in the found articles and select the ones that
contain appropriate and related information. Finally,
the fifth step of analysing and synthetisising the
findings was conducted following the preview,
question, read, summarise (PQRS) system that is
recommended by Cronin, Ryan and Coughlan (2008).
To retrieve a result set that represents the-state-of-
the-art of the chosen field the selection criterion was
to exclude articles that are older than 2018, and that
The Use of Virtual Reality Applications in Stroke Rehabilitation for Older Adults: Technology Enhanced Relearning
147

articles should preferably have been published in
peer-reviewed research journals. The rationale for
building on articles no older than 2018 was to look at
state-of-the art solutions in this field. However, some
articles were selected in a backward search, a
technique that has been defined as "reviewing older
literature cited in the articles yielded from the
keyword search" (Vom Brocke et al., 2009). The pre-
defined search string for retrieving a relevant result
set was "stroke rehabilitation" AND "virtual reality"
AND "older adults", where AND is the Boolean
operator for combining keywords to a search criterion
to find articles that must include all the chosen
keywords (Ely & Scott, 2007; Cronin, Ryan and
Coughlan, 2008). Finally, the review was framed with
the frequently used approach of dividing the literature
into categories. An approach that allows an
integration of themes and patterns from both
theoretical and empirical studies in the answering of
the research question (Carnwell and Daly, 2001). In
the fourth step an assessment of the chosen research
methods was an important part of the quality
assessment, and research methods for the selected
articles are briefly described below in Table 1.
Articles without a detailed description of a sound
research method were excluded. Out of the initial 594
articles that were retrieved with the search string and
the exclusion criteria the articles listed below in Table
1 were selected for further analysis after the quality
assessment step where articles were skimmed with a
focus on abstracts, method chapters, findings and
conclusions. The two main criteria in the quality
assessment were firstly to examine the used research
methods, and secondly to look for findings that could
answer the research question.
4 FINDINGS AND DISCUSSIONS
Several studies recommend that technology enhanced
solutions involving virtual reality should be more
frequently used in after stroke rehabilitation to
increase motivation and to better meet the needs of
the patient (Hashim et al., 2018; Langan et al., 2018,
Yeh, Pai & Jeng, 2019). The largest part of the
selected articles had studied motoric relearning
(Langan et al., 2018; Zafar, Malik & Masood, 2018;
Howes et al, 2019), and surprisingly many studies
involved the concept of game-based learning (Zafar,
Malik & Masood, 2018; Sheehy et al, 2019; Yeh, Pai
& Jeng, 2019). There are also several interesting
studies on cognitive relearning (Gamito et al., 2017;
(Yeh, Pai & Jeng, 2019), while there were few
findings of speech rehabilitation studies. The four
categories are presented one by one here below.
4.1 Motoric Relearning
A promising area of motoric relearning seems to be
balance and gait exercises where a virtual reality
application also can eliminate the risk of falling
(Zafar, Malik & Masood, 2018; Kamińska et al.,
2018). Several studies stress the importance of
exercises that are adapted to the target group, and the
recommendation in a study on balance and strength
exercises by Howes et al. (2019), was to involve the
end users at an early stage. An interesting finding in
this study was that the older adults preferred to view
the balance exercises on a flat screen rather than in
headsets (Howes et al., 2019). The study by Porras et
al. (2018) points out that virtual reality-based
rehabilitation is rapidly developing, but that the best
results for balance and gait rehabilitation were
achieved when virtual reality exercises are combined
with conventional rehabilitation.
Another part of motoric relearning where virtual
reality is frequently used is for upper and lower limb
exercises (Kamińska et al., 2018). As highlighted by
Wang et al. (2017), most of the virtual reality exercise
systems are only developed to train the upper limbs.
However, there are several existing hybrid systems
that can provide motoric training for both upper and
lower limbs (Poli et al., 2013; Khor et al., 2014). To
avoid muscle contraction, it is important for patients
to have a continuous training after stroke (Poli et al.,
2013), where the idea of a game of virtual football
seems like a joyful lower limb exercise (Kamińska et
al., 2018).
The study by Laver et al. (2017), found that the
use of virtual reality and interactive games was not
more beneficial than the conventional therapy
approaches to improve upper limb functionality. On
the other hand, Wang et al. (2017) found that virtual
reality exercises combined with traditional therapy
made greater improvement than just conventional
methods. Kamińska et al. (2018) reported that game
exercises based on virtual reality increased the
possibilities of efficient and joyful motoric
rehabilitation. Finally, a phenomenon in motoric
relearning that needs attention is the displacement of
the centre of pressure that is an identified result from
some types of rehabilitation exercises (Sheehy et al.,
2019).
ICT4AWE 2020 - 6th International Conference on Information and Communication Technologies for Ageing Well and e-Health
148
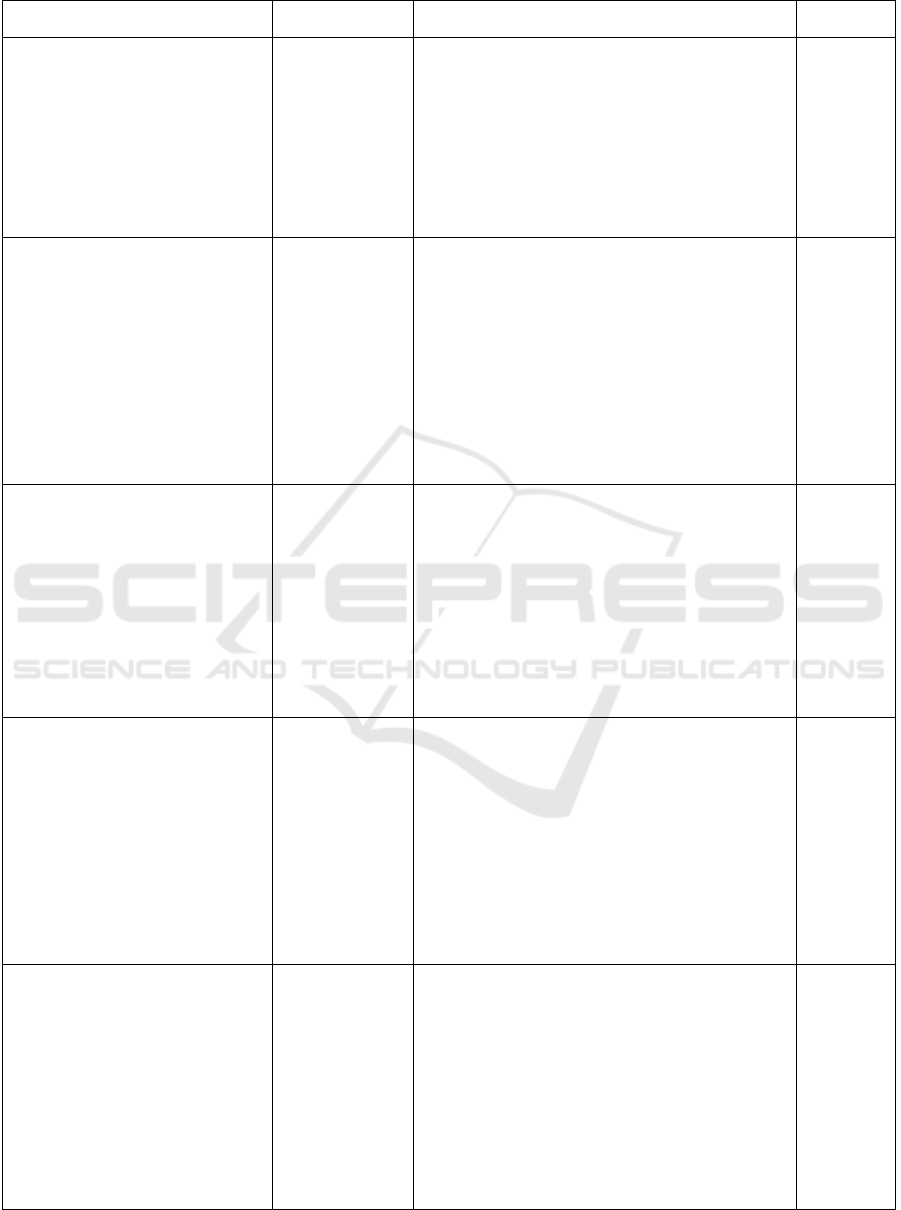
Table 1: Selected articles after the quality assessment.
Author(s), year, publication:
Method:
Interesting findings:
Category:
Zafar, A., Malik, A. N., & Masood,
T. (2018). Effect of Virtual Reality
Training on Dynamic Balance of
Chronic Stroke Patients., JIIMC
2018 Vol. 13, No.1
Quasi
interventional
pilot study.
Purposive
sampling, 8 stroke
patients
“improvement in dynamic balance after virtual reality
training, indicating that virtual reality can play an
important role in rehabilitation of balance impairment
in chronic stroke”
“VR provides a safe environment to the patient to
perform real life task without the risk of fall which is
an important factor in increasing patient's confidence
in mobility.”
Motoric
Game-based
/
Exergame
Sheehy, L., Taillon-Hobson, A.,
Finestone, H., Bilodeau, M., Yang,
C., Hafizi, D., & Sveistrup, H.
(2019). Centre of pressure
displacements produced in sitting
during virtual reality training in
younger and older adults and
patients who have had a stroke.
Disability and Rehabilitation:
Assistive Technology, 1-9.
Cross-sectional,
observational
pilot study
Game-based
learning
“Some virtual reality training games produce
greater displacements of the centre of pr essure in
sitting than others, suggesting that careful matching
between game challenge and desired therapeutic
outcome”
Stroke survivors performed similarly to healthy
older and younger adults in the gaming.
“Older adults tend to lean more than younger adults
while individuals with stroke move more or less
than others, depending on the game.”
Motoric
Game-
based
Yeh, T. M., Pai, F. Y., & Jeng, M.
Y. (2019). The factors affecting
older adults’ intention toward
ongoing participation in virtual
reality leisure activities.
International journal of
environmental research and public
health, 16(3), 333.
Quantitative
survey,
Hypothesis
testing
“experience of virtual reality leisure activities by
older adults have a significant influence on their
perception of its value” “virtual activities so that
patients can move beyond the boring and
monotonous rehabilitation methods in traditional
medical treatment” “Through interaction in games,
older adults can maintain close relationships with
others” “firms or other organizations should study
the needs and expectations of older adults toward
virtual reality leisure activities in detail.”
Motoric
Cognitive
Game-
based
Langan, J., Subryan, H., Nwogu, I.,
& Cavuoto, L. (2018). Reported use
of technology in stroke
rehabilitation by physical and
occupational therapists. Disability
and Rehabilitation: Assistive
Technology, 13(7), 641-647.
Quantitative
surveys
distributed by
mail, email and
in online
postings
“Conventional equipment such as stopwatches are
more frequently used compared to newer
technology like Wii and Kinect games.”
“The patient care experience is a priority in
healthcare, so when patients report feeling bored
and desiring greater fostering of autonomy in stroke
rehabilitation, it is troubling”
“Therapists should consider using technology in
stroke rehabilitation to better meet the needs of the
patient”
Motoric
Game-
based
Hashim, S. H. B. M., Ismail, M. B.,
Manaf, H. B. A., & Hanapiah, F. A.
B. (2018). Framework of virtual
reality game on dual cognitive task
for stroke rehabilitation. In 2018
IEEE Symposium on Computer
Applications & Industrial
Electronics (ISCAIE) (pp. 114-118).
IEEE.
Framework
designed based
on a literature
review and
questionnaires
Proposed framework
“VR is often designed to be more engaging, more
interesting and more enjoyable than conventional
stroke rehabilitation.”
“stroke patients that have problems with dual
cognitive task could use virtual reality games as part
of their rehabilitation programme. However, they
need equipment that is in-expensive and are low
health risk to them so that it would not burden
them.”
Cognitive
Motoric
Dual
cognitive
Game-
based
The Use of Virtual Reality Applications in Stroke Rehabilitation for Older Adults: Technology Enhanced Relearning
149

Table 1: Selected articles after the quality assessment.(cont.)
Porras, D. C., Siemonsma, P.,
Inzelberg, R., Zeilig, G., & Plotnik,
M. (2018). Advantages of virtual
reality in the rehabilitation of balance
and gait: systematic review.
Neurology, 90(22), 1017-1025.
Systematic
Review
and Meta-
Analysis
VR-based rehabilitation is developing rapidly,
VR improved balance and gait especially when
combined with conventional rehabilitation.
Motoric
(balance and
gait)
Gamito, P., Oliveira, J., Coelho, C.,
Morais, D., Lopes, P., Pacheco, J., ...
& Barata, A. F. (2017). Cognitive
training on stroke patients via virtual
reality-based serious games.
Disability and rehabilitation, 39(4),
385-388.
Experiment
Game
development
“The results showed significant improvements
in attention and memory functions in the
intervention group, but not in the controls”
“Overall findings provide further support for
the use of VR cognitive training applications in
neuropsychological rehabilitation.”
Cognitive
Game-based
Kamińska, M. S., Miller, A., Rotter,
I., Szylińska, A., & Grochans, E.
(2018). The effectiveness of virtual
reality training in reducing the risk of
falls among elderly people. Clinical
interventions in aging, 13, 2329.
Functional testing
Spring hand
dynamometers
“One game that strongly activated the upper
limbs was bowling”
“VR training increases the possibilities of
motor training and can help reduce the risk of
falls by improving the static and dynamic
balance”
Motori
(balance,upper
limbs, lower
limbs)
Game-based
Bevilacqua, R., Maranesi, E.,
Riccardi, G. R., Donna, V. D.,
Pelliccioni, P., Luzi, R., ... &
Pelliccioni, G. (2019). Non-
Immersive Virtual Reality for
Rehabilitation of the Older People: A
Systematic Review into Efficacy and
Effectiveness Journal of clinical
medicine, 8(11), 1882.
Literature study
“The level of realism of the virtual stimuli
seems to have a crucial role in the training of
the cognitive abilities. Nevertheless, semi-
immersive or non-immersive VR systems have
the advantage of being more accepted by the
users, as they experienced less cybersickness
after the training. Moreover, the integration of
these devices in the health management
systems are still lacking “
Motoric
Cognitive
Howes, S. C., Charles, D., Pedlow,
K., Wilson, I., Holmes, D., &
McDonough, S. (2019). User-centred
design of an active computer gaming
system for strength and balance
exercises for older adults. Journal of
Enabling Technologies.
User testing of
VR-systems
based on Oculus
Rift headsets
“Findings from this study suggested that active
computer gaming was safe way to deliver
strength and balance exercise to older people.
No adverse events were reported during use of
the system. Participants unanimously preferred
viewing the system displayed on flat screen
rather than using a VR headset.”
Motoric
(strength and
balance
exercises)
Saposnik, G., Teasell, R., Mamdani,
M., Hall, J., McIlroy, W., Cheung, D.,
... & Bayley, M. (2010). Effectiveness
of virtual reality using Wii gaming
technology in stroke rehabilitation: a
pilot randomized clinical trial and
proof of principle. Stroke, 41(7),
1477-1484.
Single-blind and
randomised
clinical trial with
two parallel
groups of stroke
patients
“VR Wii gaming technology represents a safe,
feasible, and potentially effective alternative to
facilitate rehabilitation therapy and promote
motor recovery after stroke.”
“it was possibly subject to bias in that patients
using the ‘new’ technology may have been
more motivated by the use of this treatment”
Motoric
Game-based
ICT4AWE 2020 - 6th International Conference on Information and Communication Technologies for Ageing Well and e-Health
150

Table 1: Selected articles after the quality assessment.(cont.)
Amaya, A., Woolf, C., Devane, N.,
Galliers, J., Talbot, R., Wilson, S., &
Marshall, J. (2018). Receiving aphasia
intervention in a virtual environment: the
participants’ perspective. Aphasiology,
32(5), 538-558.
Semi-structured
interviews two
weeks before
(and two weeks
after (exit) an
intervention
“intervention was strongly associated with fun
and enjoyment”
“Perceived impacts related to communication,
activity, computer use and confidence.”
Speech
Wang, Z. R., Wang, P., Xing, L., Mei, L.
P., Zhao, J., & Zhang, T. (2017). Leap
Motion-based virtual reality training for
improving motor functional recovery of
upper limbs and neural reorganization in
subacute stroke patients. Neural
regeneration research, 12(11), 1823.
Randomised
controlled pilot
study
“The Wolf Motor Function Test score for the
experimental group (Leap Motion-based virtual
reality training combined with conventional
occupational therapy) indicated greater
improvement than that attained by the control
group”
Motoric
(upper
limb)
Khor, K. X., Rahman, H. A., Fu, S. K.,
Sim, L. S., Yeong, C. F., & Su, E. L. M.
(2014). A novel hybrid rehabilitation
robot for upper and lower limbs
rehabilitation training. Procedia
Computer Science, 42, 293-300.
Kinematic study
“development of a novel hybrid rehabilitation
robot that able to perform rehabilitation training
for both upper and lower limbs”
“Stroke patients need to continue training after
stroke to avoid muscle contraction, but due to
large number of patients, they are not able to
train frequently in the hospital.”
Motoric
(upper
limbs,
lower
limbs)
4.2 Cognitive Relearning
A serious game for cognitive training was developed
by Gamito et al. (2017), a game where attention and
memory tasks in daily life activities were practiced in
a virtual reality world. Results in the study showed
significant improvements for participants in the
intervention group, but not in the control group. As
suggested by Bevilacqua et al., 2019), the quality of
realism and stimuli in virtual worlds seem to be a
crucial factor in the relearning of cognitive abilities.
At the same time, multi-modal virtual worlds can help
patients to move beyond the sometimes boring and
monotonous traditional relearning methods, where
the use of graphics and sound could stimulate older
adults' cognitive functions (Yeh, Pai & Jeng, 2019).
4.3 Speech Relearning
Despite the feature of speech interaction with virtual
reality systems (Chun et al., 2015), it was hard to find
studies on speech relearning in virtual worlds. An
explanation might be, as it was stated by, that “speech
rehabilitation intervention options are few”, but that
there have been some tests where Aphasia scripts
have been combined with speech training where the
proper articulation was illustrated by the mouth of an
avatar. Probably that the search strategy here should
be to replace "stroke rehabilitation" with “aphasia
scripts”. However, the result might be the same, and
as pointed out by Amaya et al. (2018), there is an
increasing contribution of digital systems for aphasia
therapy, but virtual reality applications still are rare.
An interesting concept is to create virtual speech
relearning exercises as multi-user environments
where patients can interact with therapists, support
staff and other patients. Many interviewed patients
mentioned their appreciation for interaction, humour
and social contact, and only one patient found the
social interaction to be fatiguing (Amaya et al., 2018).
4.4 Game-based Relearning
Considering motoric relearning, virtual bowling was
found to be the game that strongly activated the upper
limbs, and that football and downhill skiing games are
suitable exercises for the lower limbs (Kamińska et
al., 2018). In the frequently cited study by Saposnik
et al. (2010) the conclusion was that game-based
virtual reality applications offer a safe, feasible, and
potentially effective alternative for motoric
relearning after stroke. On the other hand, some types
of games need a careful matching between the desired
therapeutic outcomes and the gaming impact on
stroke patients (Sheehy et al., 2019).
To develop video games is often time consuming
and costly, and a cost-efficient approach could be to
collaborate or to work in parallel with the game
industry (Gamito et al., 2017). The idea of a
relearning process built on games that have not been
The Use of Virtual Reality Applications in Stroke Rehabilitation for Older Adults: Technology Enhanced Relearning
151

fully designed for rehabilitation (Gamito et al., 2011),
might clash with the idea of a truly individualised and
adapted relearning process (Ahmad, Mozelius &
Ahlin, 2019). A recommended way to increase users'
safety, usability and acceptability of the games is
user-centred design where stroke patients are
involved in the game development (Howes et al.,
2019).
4.5 General Discussion
Another aspect of the discussion between high-end
games with complex virtual reality worlds is the
cybersickness phenomenon. Cybersickness that is an
issue in virtual reality worlds resembles of motion
sickness with symptoms such as nausea and cold
sweating (Mazloumi et al., 2018). To avoid
cybersickness among older adults the idea could be to
choose semi-immersive or non-immersive virtual
reality systems since they induce less cybersickness.
However, the level of realism and immersion of the
virtual world seems to have a crucial role in cognitive
relearning. (Bevilacqua et al., 2019)
As in other fields where virtual reality games have
been tested there seems to be a motivational effect
also among older adult stroke patients (Hashim et al.,
2018, Yeh, Pai & Jeng, 2019). Even if it might be the
new technology itself that motivates, as remarked by
Saposnik et al. (2010), motivation should not be
underestimated in the long-term post stroke
relearning struggle. Finally, as highlighted by Gilbert
et al. (2013), participation in virtual worlds could
have a general positive impact on patients with
disabilities.
Finally, a drawback with VR solutions for stroke
patients that was found by random in a backward
search in this study is the cybersickness phenomenon.
Cybersickness is sometimes also referred to as virtual
reality sickness or simulator sickness, and is a
syndrome that arises from the use of VR. The three
main symptoms of cybersickness are oculomotor
discomfort, disorientation and nausea (Vinson et al.,
2012). This might be particularly problematic since
nausea is an identified ailment among stroke patients
(Canhao et al., 1997)
5 CONCLUSION
Virtual reality-based stroke rehabilitation is a rapidly
emerging field opening up possibilities for all the four
described categories. The greatest potential seems to
be for stroke patients' motoric and game-based
relearning, and with less applications for speech
rehabilitation. The main idea should not be to
completely replace the existing stroke rehabilitation
with virtual reality systems, but rather to combine and
extend the conventional relearning methods, and to
keep the identified importance of human-to-human
interaction (Loft et al., 2019). There are no virtual
reality applications that fits all stroke patients', but a
thoughtful selection of exercises that matches the user
needs have a potential to enhance the current
relearning therapy for older adults after stroke.
6 FUTURE WORK
A relevant and interesting follow-up study would be
to test and evaluate various variations of the found
virtual reality applications for stroke relearning. This
should be carried out in a real world setting in close
collaboration with a professional stroke rehabilitation
team. The evaluation should mainly be based on
stroke patient’s perceived use and their actual
relearning progression. Furthermore, the use of
games in stroke rehabilitation looks promising and
could be interesting to investigate further in another
separate literature review. Finally, for the category of
speech relearning for stroke patients it would be
interesting to further explore the combination of
virtual reality and aphasia scripts.
REFERENCES
Ahmad, A., Mozelius, P., Ahlin, K. (2019). Testbed
requirements for technology enhanced stroke
rehabilitation to support independent living. In
proceedings of The 5th International Conference on
Information and Communication Technologies for
Ageing Well and e-Health.
Amaya, A., Woolf, C., Devane, N., Galliers, J., Talbot, R.,
Wilson, S., & Marshall, J. (2018). Receiving aphasia
intervention in a virtual environment: the participants’
perspective. Aphasiology, 32(5), 538-558.
Bevilacqua, R., Maranesi, E., Riccardi, G. R., Di Donna,
V., Pelliccioni, P., Luzi, R., ... & Pelliccioni, G. (2019).
Non-Immersive Virtual Reality for Rehabilitation of
the Older People: A Systematic Review into Efficacy
and Effectiveness. Journal of clinical medicine, 8(11),
1882.
Brahnam, S., & Jain, L. C. (Eds.). (2011). Advanced
computational intelligence paradigms in healthcare 6:
virtual reality in psychotherapy, rehabilitation, and
assessment (Vol. 337). Springer.
Broeren, J., Bjorkdahl, A., Claesson, L., Goude, D.,
Lundgren-Nilsson, A., Samuelsson, H., ... & Rydmark,
M. (2008). Virtual rehabilitation after stroke. Studies in
health technology and informatics, 136, 77.
ICT4AWE 2020 - 6th International Conference on Information and Communication Technologies for Ageing Well and e-Health
152

Brahnam, S., & Jain, L. C. (2011). Virtual Reality in
Psychotherapy, Rehabilitation, and Neurological
Assessment. In Advanced Computational Intelligence
Paradigms in Healthcare 6. Virtual Reality in
Psychotherapy, Rehabilitation, and Assessment (pp. 1-
9). Springer, Berlin, Heidelberg.
Broeren, J., Bjorkdahl, A., Claesson, L., Goude, D.,
Lundgren-Nilsson, A., Samuelsson, H., ... & Rydmark,
M. (2008). Virtual rehabilitation after stroke. Studies in
health technology and informatics, 136, 77.
Canhao, P., Melo, T. P., Salgado, A. V., Oliveira, V., Pinto,
A. N., Crespo, M., & Ferro, J. M. (1997). Nausea and
vomiting in acute ischemic stroke. Cerebrovascular
Diseases, 7(4), 220-225.
Carnwell, R., & Daly, W. (2001). Strategies for the
construction of a critical review of the literature. Nurse
education in practice, 1(2), 57-63.
Chun, L. M., Arshad, H., Piumsomboon, T., & Billinghurst,
M. (2015). A combination of static and stroke gesture
with speech for multimodal interaction in a virtual
environment. In 2015 International Conference on
Electrical Engineering and Informatics (ICEEI) (pp. 59-
64). IEEE.
Cogollor, J. M., Rojo-Lacal, J., Hermsdörfer, J., Ferre, M.,
Waldmeyer, M. T. A., Giachritsis, C., ... & Sebastián,
J. M. (2018). Evolution of cognitive rehabilitation after
stroke from traditional techniques to smart and
personalized home-based information and
communication technology systems: literature review.
JMIR rehabilitation and assistive technologies, 5(1), e4.
Cronin, P., Ryan, F., & Coughlan, M. (2008). Undertaking
a literature review: a step-by-step approach. British
journal of nursing, 17(1), 38-43.
Deutsch, J. E., Brettler, A., Smith, C., Welsh, J., John, R.,
Guarrera-Bowlby, P., & Kafri, M. 2011. Nintendo wii
sports and wii fit game analysis, validation, and
application to stroke rehabilitation. Topics in stroke
rehabilitation, 18(6), 701-719.
Deutsch, J. E., Latonio, J., Burdea, G. C., & Boian, R.
(2001). Post-stroke rehabilitation with the Rutgers
Ankle System: a case study. Presence: Teleoperators &
Virtual Environments, 10(4), 416-430.
Ehn, M., Hansson, P., Sjölinder, M., Boman, I. L., Folke,
M., Sommerfeld, D., ... & Palmcrantz, S. (2015). Users
perspectives on interactive distance technology
enabling home-based motor training for stroke patients.
pHealth, 2015(5), 145-152.
Ely, C., & Scott, I. (2007). Essential study skills for nursing.
Elsevier Health Sciences.
Gamito, P., Oliveira, J., Coelho, C., Morais, D., Lopes, P.,
Pacheco, J., ... & Barata, A. F. (2017). Cognitive
training on stroke patients via virtual reality-based
serious games. Disability and rehabilitation, 39(4), 385-
388.
Gamito, P., Oliveira, J., Morais, D., Rosa, P., & Saraiva, T.
(2011). Serious games for serious problems: from
ludicus to therapeuticus. In Virtual reality. IntechOpen.
Gerstenecker, A., & Lazar, R. M. (2019). Language
recovery following stroke. The Clinical Neuro-
psychologist, 33(5), 928-947.
Gilbert, R. L., Murphy, N. A., Krueger, A. B., Ludwig, A.
R., & Efron, T. Y. (2013). Psychological benefits of
participation in three-dimensional virtual worlds for
individuals with real-world disabilities. International
Journal of Disability, Development and Education,
60(3), 208-224.
Glännfjord, F., Hemmingsson, H., & Larsson Ranada, Å.
(2017). Elderly people’s perceptions of using Wii
sports bowling–A qualitative study. Scandinavian
journal of occupational therapy, 24(5), 329-338.
Greener, J., Enderby, P., & Whurr, R. (1999). Speech and
language therapy for aphasia following stroke.
Cochrane Database of Systematic Reviews, (4)
Greveson, G., & James, O. (1991). Improving long-term
outcome after stroke--the views of patients and carers.
Health trends, 23(4), 161-162.
Hashim, S. H. B. M., Ismail, M. B., Manaf, H. B. A., &
Hanapiah, F. A. B. (2018). Framework of virtual reality
game on dual cognitive task for stroke rehabilitation. In
2018 IEEE Symposium on Computer Applications &
Industrial Electronics (ISCAIE) (pp. 114-118). IEEE.
Heruti, R. J., Lusky, A., Dankner, R., Ring, H., Dolgopiat,
M., Barell, V., ... & Adunsky, A. (2002). Rehabilitation
outcome of elderly patients after a first stroke: effect of
cognitive status at admission on the functional
outcome. Archives of physical medicine and
rehabilitation, 83(6), 742-749.
Hilari, K., Wiggins, R., Roy, P., Byng, S., & Smith, S.
(2003). Predictors of health-related quality of life
(HRQL) in people with chronic aphasia. Aphasiology,
17(4), 365-381.
Hoffmann, M. (2001). Higher cortical function deficits after
stroke: an analysis of 1,000 patients from a dedicated
cognitive stroke registry. Neurorehabilitation and
Neural Repair, 15(2), 113-127.
Howes, S. C., Charles, D., Pedlow, K., Wilson, I., Holmes,
D., & McDonough, S. (2019). User-centred design of
an active computer gaming system for strength and
balance exercises for older adults. Journal of Enabling
Technologies.
Jack, D., Boian, R., Merians, A. S., Tremaine, M., Burdea,
G. C., Adamovich, S. V., ... & Poizner, H. (2001).
Virtual reality-enhanced stroke rehabilitation. IEEE
transactions on neural systems and rehabilitation
engineering, 9(3), 308-318.
Johansson, M. B., Carlsson, M., & Sonnander, K. (2012).
Communication difficulties and the use of
communication strategies: from the perspective of
individuals with aphasia. International journal of
language & communication disorders, 47(2), 144-155.
Jokinen, H., Melkas, S., Ylikoski, R., Pohjasvaara, T.,
Kaste, M., Erkinjuntti, T., & Hietanen, M. (2015).
Post‐stroke cognitive impairment is common even
after successful clinical recovery. European Journal of
Neurology, 22(9), 1288-1294.
Juul, J. (2010). A casual revolution: Reinventing video
games and their players. MIT press.
Kamińska, M. S., Miller, A., Rotter, I., Szylińska, A., &
Grochans, E. (2018). The effectiveness of virtual reality
The Use of Virtual Reality Applications in Stroke Rehabilitation for Older Adults: Technology Enhanced Relearning
153

training in reducing the risk of falls among elderly
people. Clinical interventions in aging, 13, 2329.
Khor, K. X., Rahman, H. A., Fu, S. K., Sim, L. S., Yeong,
C. F., & Su, E. L. M. (2014). A novel hybrid
rehabilitation robot for upper and lower limbs
rehabilitation training. Procedia Computer Science, 42,
293-300.
Langan, J., Subryan, H., Nwogu, I., & Cavuoto, L. (2018).
Reported use of technology in stroke rehabilitation by
physical and occupational therapists. Disability and
Rehabilitation: Assistive Technology, 13(7), 641-647.
Langhorne, P., Bernhardt, J., & Kwakkel, G. (2011). Stroke
rehabilitation. The Lancet, 377(9778), 1693-1702.
Langhorne, P., Coupar, F., & Pollock, A. (2009). Motor
recovery after stroke: a systematic review. The Lancet
Neurology, 8(8), 741-754.
Laver, K. E., Lange, B., George, S., Deutsch, J. E.,
Saposnik, G., & Crotty, M. (2017). Virtual reality for
stroke rehabilitation. Cochrane database of systematic
reviews, (11).
Loft, M. I., Martinsen, B., Esbensen, B. A., Mathiesen, L.
L., Iversen, H. K., & Poulsen, I. (2019). Call for human
contact and support: an interview study exploring
patients’ experiences with inpatient stroke
rehabilitation and their perception of nurses’ and nurse
assistants’ roles and functions. Disability and
rehabilitation, 41(4), 396-404.
Malliarakis, C., Satratzemi, M., & Xinogalos, S. (2014).
Educational games for teaching computer
programming. In Research on e-Learning and ICT in
Education (pp. 87-98). Springer, New York, NY.
Maganty, N., Ilyas, M., Zhang, N., & Sharma, A. (2018).
Online, game-based education for melanoma
recognition: A pilot study. Patient education and
counseling, 101(4), 738-742.
Mazloumi Gavgani, A., Walker, F. R., Hodgson, D. M., &
Nalivaiko, E. (2018). A comparative study of
cybersickness during exposure to virtual reality and
“classic” motion sickness: are they different?. Journal
of Applied Physiology, 125(6), 1670-1680.
Mozelius, P., Ahlin, K., & Ahmad, A. (2019). A game-
based approach for motoric stroke rehabilitation–
defining the requirements. In ECGBL 2019 (Vol. 13).
Mozelius, P., Hernandez, W., Sällström, J., & Hellerstedt,
A. (2017). Teacher Attitudes Toward Game-based
Learning in History Education. International Journal of
Information and Communication Technologies in
Education, 6(4), 27-35.
Palmcrantz, S., Borg, J., Sommerfeld, D., Plantin, J., Wall,
A., Ehn, M., ... & Boman, I. L. (2017). An interactive
distance solution for stroke rehabilitation in the home
setting–A feasibility study. Informatics for Health and
Social Care, 42(3), 303-320.
Parahoo, K. (2006). Nursing research: principles, process
and issues, Hampshire.
Peters, E., Heijligers, B., de Kievith, J., Razafindrakoto, X.,
van Oosterhout, R., Santos, C., ... & Louwerse, M.
(2016). Design for collaboration in mixed reality:
Technical challenges and solutions. In 2016 8th
International Conference on Games and Virtual Worlds
for Serious Applications (VS-GAMES) (pp. 1-7).
IEEE.
Pesonen, L., Otieno, L., Ezema, L., Benewaa Kusi, D., &
Hellstén, T. (2017). Virtual Reality in rehabilitation: a
user perspective.
Poli, P., Morone, G., Rosati, G., & Masiero, S. (2013).
Robotic technologies and rehabilitation: new tools for
stroke patients’ therapy. BioMed Research
International.
Pollock, A., Baer, G., Campbell, P., Choo, P. L., Forster,
A., Morris, J., Pomeroy, V. M.,Langhorne, P. 2014.
Physical rehabilitation approaches for the recovery of
function and mobility following stroke. Cochrane
Database of Systematic Reviews, (4).
Porras, D. C., Siemonsma, P., Inzelberg, R., Zeilig, G., &
Plotnik, M. (2018). Advantages of virtual reality in the
rehabilitation of balance and gait: systematic review.
Neurology, 90(22), 1017-1025.
Rizzo, A. S., & Kim, G. J. (2005). A SWOT analysis of the
field of virtual reality rehabilitation and therapy.
Presence: Teleoperators & Virtual Environments,
14(2), 119-146.
Ross, K., & Wertz, R. (2003). Quality of life with and
without aphasia. Aphasiology, 17(4), 355-364.
Saposnik, G., Teasell, R., Mamdani, M., Hall, J., McIlroy,
W., Cheung, D., ... & Bayley, M. (2010). Effectiveness
of virtual reality using Wii gaming technology in stroke
rehabilitation: a pilot randomized clinical trial and
proof of principle. Stroke, 41(7), 1477-1484.
Seniów, J., Litwin, M., & Leśniak, M. (2009). The
relationship between non-linguistic cognitive deficits
and language recovery in patients with aphasia. Journal
of the Neurological Sciences, 283(1-2), 91-94.
Sheehy, L., Taillon-Hobson, A., Finestone, H., Bilodeau,
M., Yang, C., Hafizi, D., & Sveistrup, H. (2019). Centre
of pressure displacements produced in sitting during
virtual reality training in younger and older adults and
patients who have had a stroke. Disability and
Rehabilitation: Assistive Technology, 1-9.
Shin, J. H., Ryu, H., & Jang, S. H. (2014). A task-specific
interactive game-based virtual reality rehabilitation
system for patients with stroke: a usability test and two
clinical experiments. Journal of neuroengineering and
rehabilitation, 11(1), 32.
Skidmore, E. R., Whyte, E. M., Holm, M. B., Becker, J. T.,
Butters, M. A., Dew, M. A., ... & Lenze, E. J. (2010).
Cognitive and affective predictors of rehabilitation
participation after stroke. Archives of physical
medicine and rehabilitation, 91(2), 203-207.
Swanenburg, J., Wild, K., Straumann, D., & Bruin, E. D. D.
(2018). Exergaming in a moving virtual world to train
vestibular functions and gait; a proof-of-concept-study
with older adults. Frontiers in physiology, 9, 988
Tousignant, M., Macoir, J., Martel-Sauvageau, V., Boissy,
P., Corriveau, H., Gosselin, S., ... & Pagé, C. (2018).
Satisfaction With In-Home Speech Telerehabilitation in
Post-Stroke Aphasia: an Exploratory Analysis. Journal
of the International Society for Telemedicine and
eHealth, 6, e11-1.
ICT4AWE 2020 - 6th International Conference on Information and Communication Technologies for Ageing Well and e-Health
154

Veerbeek, J. M., van Wegen, E., van Peppen, R., van der
Wees, P. J., Hendriks, E., Rietberg, M., & Kwakkel, G.
(2014). What is the evidence for physical therapy
poststroke? A systematic review and meta-analysis.
PloS one, 9(2), e87987.
Vinson, N. G., Lapointe, J. F., Parush, A., & Roberts, S.
(2012). Cybersickness induced by desktop virtual
reality. In Graphics Interface (pp. 69-75).
Vom Brocke, J., Simons, A., Niehaves, B., Riemer, K.,
Plattfaut, R., & Cleven, A. (2009). Reconstructing the
giant: on the importance of rigour in documenting the
literature search process. In Ecis (Vol. 9, pp.2206 -
2217).
Wang, Z. R., Wang, P., Xing, L., Mei, L. P., Zhao, J., &
Zhang, T. (2017). Leap Motion-based virtual reality
training for improving motor functional recovery of
upper limbs and neural reorganization in subacute
stroke patients. Neural regeneration research, 12(11),
1823.
Weech, S., Kenny, S., & Barnett-Cowan, M. (2019).
Presence and cybersickness in virtual reality are
negatively related: a review. Frontiers in psychology,
10, 158.
Zafar, A., Malik, A. N., & Masood, T. (2018). Effect of
Virtual Reality Training on Dynamic Balance of
Chronic Stroke Patients., JIIMC 2018 Vol. 13, No.1
Yamato, T. P., Pompeu, J. E., Pompeu, S. M., & Hassett, L.
(2016). Virtual reality for stroke rehabilitation. Physical
therapy, 96(10), 1508-1513.
Yates, M., Kelemen, A., & Sik Lanyi, C. (2016). Virtual
reality gaming in the rehabilitation of the upper
extremities post-stroke. Brain injury, 30(7), 855-863.
Yeh, T. M., Pai, F. Y., & Jeng, M. Y. (2019). The factors
affecting older adults’ intention toward ongoing
participation in virtual reality leisure activities.
International journal of environmental research and
public health, 16(3), 333.
Øra, H. P., Kirmess, M., Brady, M. C., Winsnes, I. E.,
Hansen, S. M., & Becker, F. (2018). Telerehabilitation
for aphasia–protocol of a pragmatic, exploratory, pilot
randomized controlled trial. Trials, 19(1), 208.
The Use of Virtual Reality Applications in Stroke Rehabilitation for Older Adults: Technology Enhanced Relearning
155
