
Algorithmic State Machine Design for Timely Health Emergency
Management in an IoT Environment
Fadi T. El-Hassan
a
College of Engineering, Al Ain University, Al Ain, Abu Dhabi, U.A.E.
Keywords:
Smart Emergency, Prehospital Management, Algorithmic State Machine, Internet of Things, Embedded
Systems, Health Emergency Management.
Abstract:
In emergency cases related to massive accidents, environmental disasters, and war time, health professionals
face considerable challenges due to the high number of patients who are in need of emergency treatment.
Research works attempt to propose effective in-hospital and pre-hospital smart emergency systems to reduce
the mortality rate among the patients who desperately wait to receive appropriate care. This paper presents
a model of a timely prehospital emergency management system that can be implemented as an interface to
an Internet of Things (IoT) environment. This work presents the necessary stages for prehospital emergency
environments, where many factors may make the timely management of emergency systems very difficult.
The proposed model is based on an Algorithmic State Machine (ASM) that can be implemented in either
hardware or software, providing an embedded system interface for IoT. Moreover, this paper provides a timing
analysis for either a single emergency event or multiple simultaneous emergency events. Embedded systems’
developers can use the proposed model to produce an appropriate prehospital smart emergency solution.
1 INTRODUCTION
Emergency care is a right for everyone in need of ur-
gent treatment. Elderly with dehydration symptoms,
persons facing a heart attack, pregnant women who
are about to deliver a baby, passengers bleeding due
to car accidents or airplane crashes, a population hit
by an earthquake or a tsunami, and citizens wounded
from bomb attacks are all examples of patients who
absolutely need quick treatment to save their lives.
Emergency services should start on the site of dis-
asters or any health-threatening events, en route to
hospitals, and on the arrival to hospitals up to ad-
mission, diagnosis, and treatment. In all these stages,
health professionals face timely challenges to quickly
provide emergency care to save patients’ lives. De-
spite the considerable emergency effort, the mortal-
ity rate among those patients can be very high even
in the absence of major disasters. For example, a
study finds that the death rate in England is higher
for the emergencypatients admitted to hospitals at the
weekend than for the patients admitted on weekdays
(Meacock et al., 2017).
Despite the introduction of a four-hour rule to dis-
a
https://orcid.org/0000-0002-1579-2288
charge emergency patients in some hospitals, in order
to reduce patient waiting times and mortality rates, the
quality of care received by patients during this four-
hour period was questionable (Crawford et al., 2014).
In cases of environmental disasters, the challenges
of emergency service provision are considerably high.
For example, in the case of the earthquake that hit
Haiti in 2010, communication difficulties were among
the primary challenges of providing emergency ser-
vices to displaced persons (Magloire et al., 2010).
With the advances in modern technologies in gen-
eral, and in wireless communications and Internet
of Things (IoT) in particular, smart emergency sys-
tems were proposed to mitigate the mortality rate
among the emergency patients. This paper presents
a model of a prehospital smart emergency system that
can be invaluable toward the achievement of efficient
management of such systems. The presented system
model includes timely information that can be imple-
mented even if multiple health-threatening events oc-
cur simultaneously.
Taking into consideration that timely data is
recorded for each health-threatening event in prehos-
pital stages, the presented model fits well as an inter-
face between the recorded timing data and IoT-based
emergency response devices/robots/vehicles/systems,
150
El-Hassan, F.
Algorithmic State Machine Design for Timely Health Emergency Management in an IoT Environment.
DOI: 10.5220/0009183301500156
In Proceedings of the 9th International Conference on Sensor Networks (SENSORNETS 2020), pages 150-156
ISBN: 978-989-758-403-9; ISSN: 2184-4380
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
Smart
Emergency
System
Model
Emergency
Responses
IoT-based
Devices/
Robots/
Vehicles
Event Time
Recordings
Figure 1: The Model as an Interface for a Prehospital Smart
Emergency System.
as depicted in Figure 1.
In literature, researchers focus on enhancing pre-
hospital solutions through wearable devices and com-
munication technologies (Seneviratne et al., 2017)
(Wu et al., 2017) (Amato and Coronato, 2017).
On top of wearable devices, (Yu et al., 2018) pro-
pose a personalized scheme for predicting the el-
derly’s wellness condition ahead of time, by collect-
ing data from multiple monitoring devices, integrat-
ing the collected data, and improving the prediction
via statistical learning. In another healthcare predic-
tion approach, (Park et al., 2018) propose a prehospi-
tal care recording system as a result of the integration
of patients’ personal lifelogs and electronic medical
records, in addition to ambulance monitoring of pa-
tients.
(Chiou and Liao, 2018) highlight the importance
of minimizing the time of rescue response in the case
of incidents, and propose the usage of mobile devices
and a central server, which can alert medical staff in
the incident region and provide clear directions to the
incident location.
In all proposed solutions, prehospitaltimely track-
ing of health cases is implied. Practically, such so-
lutions should be coupled with a timely emergency
management that can be effectively implemented in
an IoT environment.
Integration of such technologies in the IoT en-
vironment would need hardware-based computation
element (Al-Fuqaha et al., 2015), such as microcon-
trollers, microprocessors, Field Programmable Gate
Arrays (FPGAs), and Systems on Chip (SoCs).
Therefore, the presented model can be imple-
mented in hardware using, for example, a Hard-
ware Description Language (HDL) and FPGAs
(Brown and Vranesic, 2014), in order to establish a
solid emergency management system.
Prehospital timely emergency management has
not been studied extensively despite its considerable
importance. The authors of (Wu and Ren, 2016) point
to emergencymanagement stages in the civil aviation,
taking into consideration prevention, preparation, re-
sponse, and recovery. However, it was not clear how
such stages can be implemented, in order to improve
emergency management in general, and in the context
of IoT in particular.
In (Manley et al., 2016), the authors present a
study of timely emergency evacuation using an agent-
based model, where the study focuses on evacuation
planning from an airport terminals.
In contrast to existing models, our presented
ASM-based model can be implemented in either hard-
ware or software and integrated into an IoT-based
smart emergency system, for the ultimate purpose of
greatly reducing the prehospital mortality rate.
The contributionsof this paper can be summarized
as follows:
• Prehospital emergency timing model based on
ASM is presented.
• The model can be implemented in either hardware
or software.
• The model can be an interface to an IoT environ-
ment.
• A timing analysis of a single occurrence of an
emergency event is provided.
• A timing analysis of the simultaneous occurrence
of multiple emergency events is provided.
The following sections of this paper are organized
as follows. Section 2 describes the stages that typi-
cally feature in smart prehospital emergency systems.
Section 3 presents the proposed model based on an
algorithmic state machine. Section 4 provides a tim-
ing analysis of prehospital smart emergency systems
for either a single health-threatening event or multi-
ple events. Section 5 includes further discussions. Fi-
nally, section 6 concludes this paper.
2 STAGES OF PREHOSPITAL
SMART EMERGENCY
SYSTEMS
Smart emergency systems imply the use of many
technologies, tools, and equipment through stages of
prehospital and in-hospital healthcare. First, the de-
tection of a health-threatening event once it occurs,
and the notification of such an occurrence, should
be quickly accomplished through specific technolog-
ical equipment. Second, the dispatch of appropriate
rescue vehicles, health professionals, and appropriate
tools, should be the next immediate step in order to
Algorithmic State Machine Design for Timely Health Emergency Management in an IoT Environment
151
save lives as quickly as possible. Third, the use of ef-
fective equipment is important to establish communi-
cations between dispatched personnel and in-hospital
personnel, in order to inform the hospital ahead of
time about the patients’ status. Fourth, hospitals
should be well-prepared to receive the emergency pa-
tients, diagnose them, and admit them accordingly.
Taking into consideration that some patients may seek
emergency care without any prior communications,
hospitals should be able to efficiently handle unpre-
dictable cases.
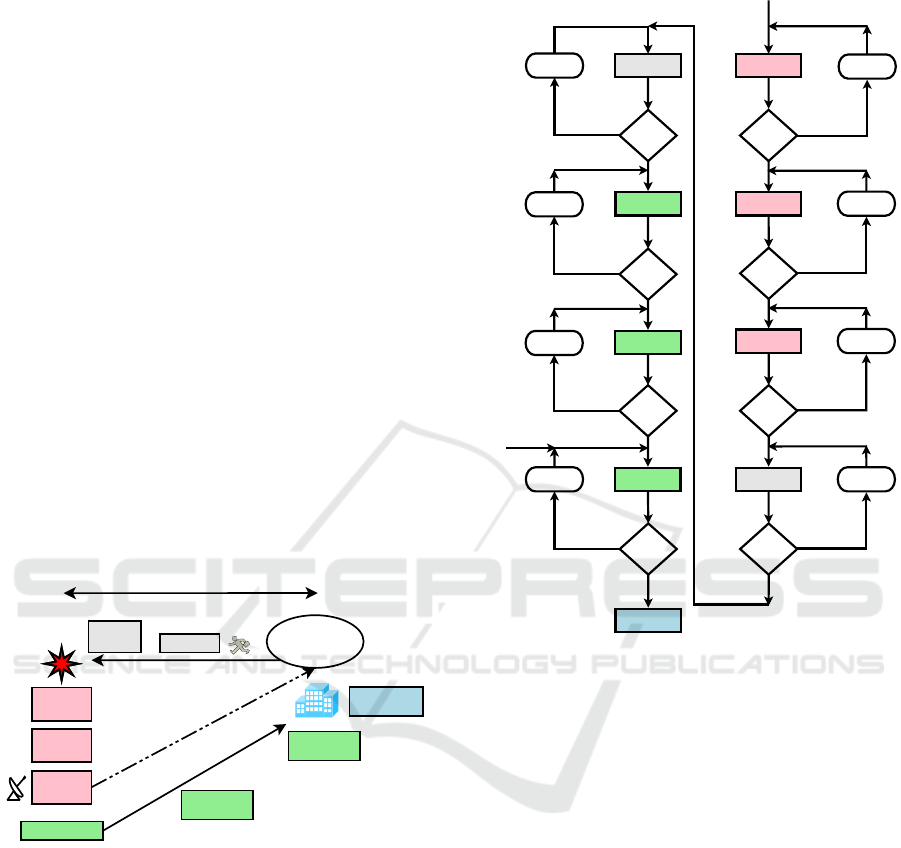
Figure 2 depicts a visual diagram showing eight
stages of a typical prehospital emergency system,
from the occurrence of a health-related event up to
patient’s arrival to the hospital for emergency care.
The sequence of stages starts with (1) event occur-
rence, (2) detection, and (3) notification, followed by
(4) dispatching of rescue team who shall have the pur-
pose of prompt (5) arrival to the event’s site. Subse-
quently, (6) on-site care shall take place prior to (7)
taking casualties to the hospital up to (8) the arrival
to the hospital, where some waiting time may happen
before the actual in-hospital emergency care.
The main aim of the proposed solution is to model
this timely sequence in an implementable way that
can be well interfaced to an IoT environment.
Health Center/
Hospital
Pre-Hospital Stages
1- Event
Occurrence
2- Event
Detection
3- Event
Notification
4- Dispatch
In-Hospital
Emergency
7- En Route
to Hospital
6- On site Care
5- On site
Arrival
8- Arrival to
Hospital
Figure 2: Stages of a Typical prehospital Emergency Sys-
tem.
3 PROPOSED ASM-BASED
MODEL FOR PREHOSPITAL
STAGES
An informative visual way of representing a prehos-
pital smart emergency system can be shown using an
Algorithmic State Machine (ASM) chart as depicted
in Figure 3.
Even though the ASM chart looks like a tradi-
tional flowchart in terms of the representation of a
sequence of states (or stages), system designers con-
External
Emergency
Event
Occurrence
Event
Detected
?
Yes
Detection
Event
Reported
?
Yes
No
T0 = T0 + 1
No
T1 = T1 + 1
Notification
Rescue
Dispatched
?
No
T2 = T2 + 1
Dispatch
Arrival to
Event Site
?
No
T3 = T3 + 1
Yes
Yes
Site_Arrival
OnSite
Initial Care
?
No
Yes
T4 = T4 + 1
OnSite_Care
En Route
to Hospital
?
No
Yes
T5 = T5 + 1
To_Hospital
Arrival
to Hospital
?
No
Yes
T6 = T6 + 1
Hosp_Emerg
Arrival
to Hospital
?
No
Yes
T7 = T7 + 1
Emergency_Care
OnSite or
Ambulance
OnSite
Difficulties
Sensors /
Witnesses
Urban / Desert /
Ocean / Air
Police /
Hospital
Ambulance /
Firetruck
Unpredictable
Emergency
Arrival
(Internal/
External)
In-Hospital Care
Route / Traffic
Issues
Waiting or Care
Figure 3: An ASM Chart for a Typical Model of a Prehos-
pital Smart Emergency System.
sider the ASM chart a better way to model sequential
stages of a system with implicit timing information
(Brown and Vranesic, 2014). When a system must
consist of hardware and software together, the ASM
chart is particularly important to import timely infor-
mation into hardware for integration with the IoT en-
vironment.
The typical smart emergency system, depicted in
Figure 3, includes eight prehospital states before the
start of the in-hospital emergency care, where each
state is associated with a timer indicating the length
of time the system stays in the corresponding state.
The least length of time accumulated through all eight
timers, the quickest would be initiating the in-hospital
care.
Health professionals should be able to record the
duration of each prehospital stage, as a part of an ef-
fective management of emergency cases. The stage
duration records can be obtained according to the data
collected from sensors, cameras, hospital records,
ambulance records, police records, and sometimes
from media and bystanders.
SENSORNETS 2020 - 9th International Conference on Sensor Networks
152

The first prehospital stage is the occurrence of
a health-threatening event. As long as no sen-
sors/witnesses detect such occurrence, the timer T0
in Figure 3 increments and the state “Occurrence" re-
mains unchanged. The location of the event (e.g. ur-
ban, desert, or ocean), its sudden occurrence, and the
absence of any instant localization methods, would
make the event undetectable for quite a long time.
Even if the event has been detected (state “Detection"
in Figure 3) and notified (state “Notification" in Fig-
ure 3), and even if a rescue team is dispatched (state
“Dispatch" in Figure 3), the localization of the event
may take long time and may even never been reached
by the dispatched personnel. Therefore, the system
would be stuck at the state “Dispatch" with long du-
ration of the timer T3 (if its limit is not exceeded),
until arrival to the event’s site. An example of such an
event is the Malaysian flight MH370 that went miss-
ing on March 8th 2014, and has neverbeen found after
five years of the incident (as of the time of writing this
article), despite extensive search efforts in the Indian
ocean (Mujeebu, 2016).
Once the occurrence of an event is detected, timer
T0 stops and timer T1 starts and increments until no-
tification of the event is performed. Detection of an
event can be done through sensors, cameras, or wit-
nesses. Event’s notification may promptly happen,
which indicates a short duration of T1, whereas timer
T2 starts and increments up to dispatching appropriate
rescue measures. Communication technologies used
in the notification stage would be based on one of
the wireless standards or cellular networks, or even
through satellites or optical fibers. Once a rescue
team is dispatched with appropriate tools, T2 stops
and timer T3 starts and increments up to the arrival
to the event’s scene. The arrival to the event’s site
marks the end of T3 duration and the beginning of T4
duration. The difficulties encountered on site can be
overwhelming, which leads to a long duration of T4.
The places hit by an earthquake or a tsunami are ex-
amples of overwhelming locations that cause lengthy
duration of T4, before any initial care starts on site.
Sometimes, on-site care can be initiated by un-
trained bystanders before the arrival of health profes-
sionals. Even though such on-site care is highly rec-
ommended in the absence of trained persons, and can
be really critical to save a victim’s life, it is not usu-
ally included in the typical emergency system since it
is not performed by health professionals. However, if
on-site care is established by trained bystanders, arriv-
ing health professionals may temporarily rely on such
care for some victims, in order to treat other victims
at the same time. Therefore, in some circumstances,
the stage of initial care on the event’s site performed
by bystanders would occur before the dispatch of a
rescue team, before the team’s arrival, or after their
arrival. Therefore, the timer T5 in the model of Fig-
ure 3 does not stop until the victim is carried to a ve-
hicle, such an ambulance, that takes its route toward a
nearby hospital.
En route to the hospital, the rescue team in a ve-
hicle or an ambulance would be able to notify the
hospital’s emergency personnel of the patient’s health
status, using wireless communications. In this stage,
the timer T6 in Figure 3 depends on the traffic cir-
cumstances and route difficulties, and it only stops
when the patient actually reaches the hospital. Sub-
sequently, the timer T7 starts and increments until the
emergency personnel start their diagnosis and treat-
ment of the patient.
4 TIMING ANALYSIS OF A
PREHOSPITAL EMERGENCY
SYSTEM
The ASM-based smart emergency system facilitates
timing analysis of the featured stages in order for the
management to evaluate the duration of each prehos-
pital emergency case. Such timing information of
many cases ensures on-going improvementof prehos-
pital emergency systems.
4.1 Single-event Prehospital Emergency
System
The typical prehospital ASM chart presented in Fig-
ure 3 is based on each health-threatening event. When
a single individual person is involved in the event, the
ASM chart identifies the prehospital stages and cal-
culates the overall prehospital emergency duration D,
where D is:
D = T0 + T1 + T2 + T3 + T4 + T5 + T6 + T7.
However, when several casualties resulted from
a single event, the timers T0, T1, and T2 (for
stages “Occurrence," “Detection," and “Notification"
respectively in Figure 3) remain the same as they
are common to the event with multiple casualties,
and the timers T3 and T4 (for stages “Dispatch" and
“Site_Arrival" respectively in Figure 3) are associated
with each team dispatched to the same event loca-
tion, whereas the timers T5, T6, and T7 (for stages
“OnSite_Care," “To_Hospital," and “Hosp_Emerg"
respectively in Figure 3) can be different for each
individual casualty. Therefore, the total emergency
event duration can be formulated as a summation of
three duration periods T
e
, T
d
, and T
i
as follows:
Algorithmic State Machine Design for Timely Health Emergency Management in an IoT Environment
153

T
e
= T0+ T1 + T2: Pre-dispatch duration for an
event. The subscript ‘e’ in T
e
is to point to the “event"
as this duration is common to the event, with multiple
rescue teams and multiple casualties.
T
d
= T3+T4: Post-dispatch Pre-initial-care dura-
tion for an event. The subscript ‘d’ in T
d
is to point to
the “dispatch team" as this duration is for each rescue
team dispatched to the same event.
T
i
= T5+ T6 + T7: Individual initial care for an
event. The subscript ‘i’ in T
i
is to indicate that this
duration is to be calculated for each “individual" ca-
sualty resulted from the same event.
D
i
= T
e
+ T
d
+ T
i
: Total prehospital “individual"
emergency duration for a single event.
As a more concrete example, assume that two res-
cue teams are dispatched to a single event, where each
rescue team provides initial care to two casualties. As
a result, there will be a total of four casualties to re-
ceive initial care. Accordingly,
D
i
1
= T
e
+ T
d
1
+ T
i
1
is the prehospital emergency
duration of one casualty who received initial care
from the first rescue team,
D
i
2
= T
e
+ T
d
1
+ T
i
2
is the prehospital emergency
duration of another casualty who received initial care
from the same first rescue team,
D
i
3
= T
e
+ T
d
2
+ T
i
3
is the prehospital emergency
duration of one casualty who received initial care
from the second rescue team, and
D
i
4
= T
e
+ T
d
2
+ T
i
4
is the prehospital emergency
duration of another casualty who received initial care
from the same second rescue team.
Note that T
e
is the same for all four casualties be-
cause they result from the same event, whereas T
d
1
is
the same for the first two casualties because they are
both rescued from the same rescue team, and T
d
2
is
the same for the other two casualties because they are
both rescued from the second rescue team. However,
T
i
is different for each individual casualty because the
needed initial care would depend on individual factors
such as the injury seriousness of each injured person.
4.2 General Multiple-event Prehospital
Emergency System
The aim of the smart emergency system management
is to minimize the prehospital emergency duration D
i
for each patient. Therefore, the previous section in-
dicates that the minimization of D
i
primarily depends
on the fast detection and notification of an event (min-
imum T
e
) and the quick arrival of dispatched rescue
teams (minimum T
d
).
When multiple health-threatening events occur at
the same time, the health professionals face more
challenges. Multiple events directly imply more res-
cue teams to be deployed, especially if a high number
of casualties are involved. Based on the ASM chart
for a single-event emergency system given in Fig-
ure 3, a generalized multiple-event smart emergency
system can be visualized as depicted in Figure 4.
This figure shows a hierarchical model of each
health-threatening event based on the described ASM
(Figure 3), where this hierarchy is replicated for addi-
tional simultaneous events.
For n health-threatening events, where r rescue
teams are dispatched and p patients are involved is
the event, a general timing equation for each individ-
ual emergency patient can be formulated as follows:
D
i
p
= T
e
n
+ T
d
r
+ T
i
p
The aim for efficient smart emergency systems is
to minimize the prehospital duration. Therefore, the
target equation for any individual prehospital duration
should be:
D
i
p
= min(T
e
n
+ T
d
r
+ T
i
p
)
Referring to Figure 4, where two or more events
simultaneously occur, and three rescue teams are dis-
patched for each event, and just two casualties receive
care from each rescue team, the following equations
evaluate the prehospital duration for twelve emer-
gency patients resulted from two simultaneous events:
D
i
1
= T
e
1
+ T
d
1
+ T
i
11
(Event 1, Rescue Team 1,
Patient 1 [abbr. 11])
D
i
2
= T
e
1
+ T
d
1
+ T
i
12
(Event 1, Rescue Team 1,
Patient 2 [abbr. 12])
D
i
3
= T
e
1
+ T
d
2
+ T
i
21
(Event 1, Rescue Team 2,
Patient 3 [abbr. 21])
D
i
4
= T
e
1
+ T
d
2
+ T
i
22
(Event 1, Rescue Team 2,
Patient 4 [abbr. 22])
D
i
5
= T
e
1
+ T
d
3
+ T
i
31
(Event 1, Rescue Team 3,
Patient 5 [abbr. 31])
D
i
6
= T
e
1
+ T
d
3
+ T
i
32
(Event 1, Rescue Team 3,
Patient 6 [abbr. 32])
D
i
7
= T
e
2
+ T
d
1
+ T
i
11
(Event 2, Rescue Team 1,
Patient 7 [abbr. 11])
D
i
8
= T
e
2
+ T
d
1
+ T
i
12
(Event 2, Rescue Team 1,
Patient 8 [abbr. 12])
D
i
9
= T
e
2
+ T
d
2
+ T
i
21
(Event 2, Rescue Team 2,
Patient 9 [abbr. 21])
D
i
10
= T
e
2
+ T
d
2
+ T
i
22
(Event 2, Rescue Team 2,
Patient 10 [abbr. 22])
D
i
11
= T
e
2
+ T
d
3
+ T
i
31
(Event 2, Rescue Team 3,
Patient 11 [abbr. 31])
D
i
12
= T
e
2
+ T
d
3
+ T
i
32
(Event 2, Rescue Team 3,
Patient 12 [abbr. 32])
SENSORNETS 2020 - 9th International Conference on Sensor Networks
154
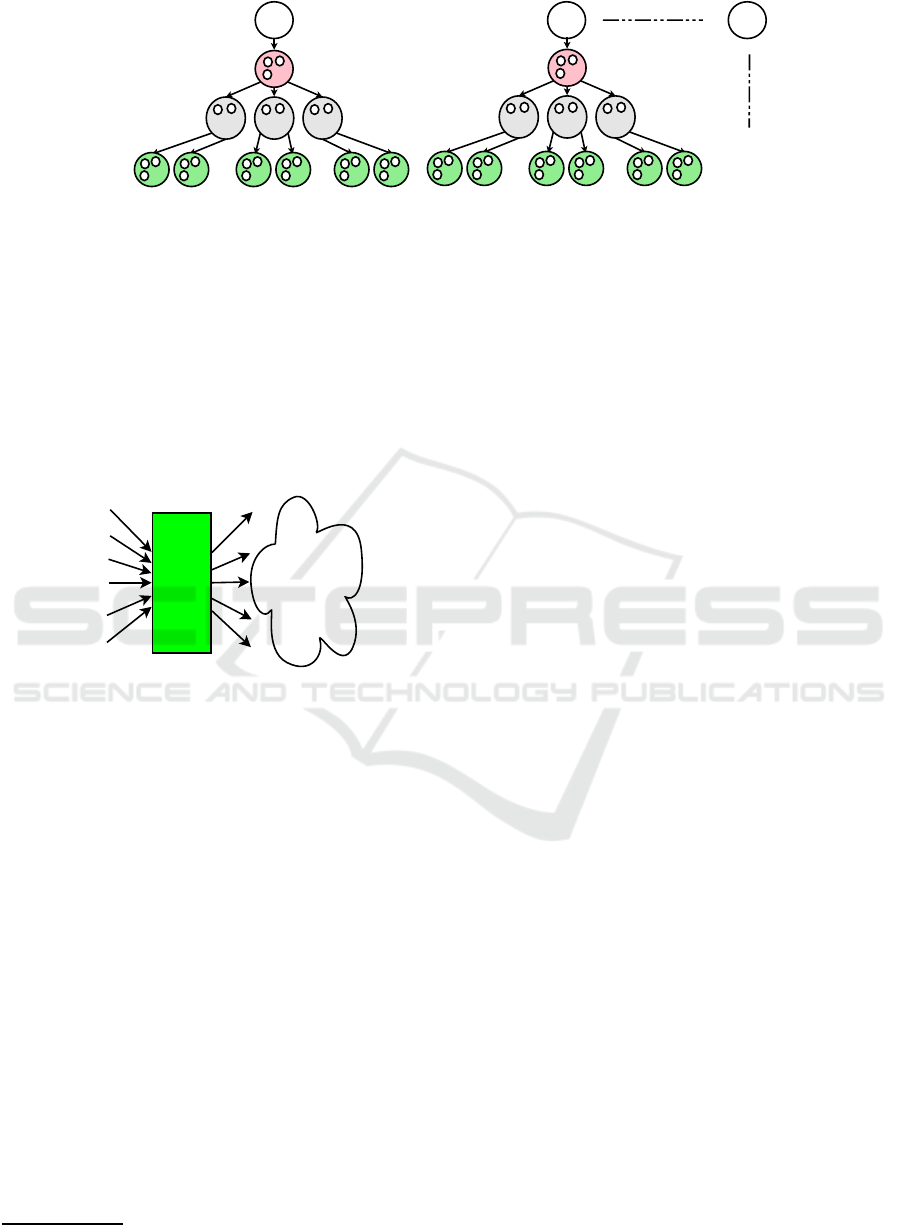
Di1 Di2 Di3 Di4 Di5 Di6 Di7 Di8
Di9
Di10 Di11 Di12
Team3
Td3
Team1
Td1
Team2
Td2
Team3
Td3
Team1
Td1
Team2
Td2
Event1
Event2
Te
Ti11 Ti12 Ti21 Ti22 Ti31 Ti32
Te
Ti11 Ti12 Ti21 Ti22 Ti31 Ti32
Eventn
Figure 4: Multiple-Event Time Management in a prehospital Smart Emergency System.
5 DISCUSSIONS
As mentioned in the introduction of this paper, the
presented model fits well as an interface between
the recorded timing data and IoT-based emergency
response devices/robots/vehicles/systems. Figure 5
highlights the multiple-event model for a smart emer-
gency system.
Multiple
Event
ASM
Charts
Event Time
Recordings
Emergency
Responses
IoT-based
Devices/
Robots/
Vehicles
Figure 5: Multiple-Event ASM-based Model for a prehos-
pital Smart Emergency System.
The timely recordings of a health-threatening
event can be fed into the presented system interface
either directly or through timing software
1
. The pre-
sented model consists of multiple-event ASM charts
that can be integrated into the hardware of emergency
response measures in order to deliver an effective IoT-
based smart emergency system.
It is important to mention that in IoT-based health-
care systems, sensors are commonly used to de-
tect health anomalies, and accordingly notify the
healthcare officials about such anomalies. Such
IoT-based sensors, which can be wearable devices,
reduce the duration of detection and notification
in a smart emergency system. However, IoT-
based emergency response devices/robots/vehicles
(e.g. (Samani and Zhu, 2016)) may automatically
move for rescue based on the timing data provided
by the presented model.
1
For example: https://www.timelinemaker.com/
6 CONCLUSION
This paper presents an ASM-based model of a pre-
hospital smart emergency system that can be an
embedded interface solution to IoT-based environ-
ments. The model possesses inherent timely informa-
tion leading to quick emergencyresponses in different
stages of a health-threatening event. In addition, it can
handle multiple eventsthat may occur simultaneously,
where multiple ASMs can be implemented to process
timely information in parallel. Parallel ASMs im-
prove prehospital smart emergency systems and sub-
sequently minimize the mortality rate that may result
from health-threatening events. This presentation of
the proposed model provides a detailed timing analy-
sis to show how prehospital emergency duration can
be minimized to save lives and reduce the mortality
rate. Embedded systems’ developers can implement
the model using hardware and software, at the pur-
pose of achieving better prehospital smart emergency
systems.
REFERENCES
Al-Fuqaha, A., Guizani, M., Mohammadi, M., Aledhari,
M., and Ayyash, M. (2015). Internet of Things: A
Survey on Enabling Technologies, Protocols and Ap-
plications. IEEE Communications Surveys & Tutori-
als, 17(4):2347–2376.
Amato, A. and Coronato, A. (2017). An IoT-Aware Archi-
tecture for Smart Healthcare Coaching Systems. IEEE
31st International Conference on Advanced Informa-
tion Networking and Applications (AINA), Taiwan.
Brown, S. and Vranesic, Z. (2014). Fundamentals of Digital
Logic with Verilog Design. McGraw-Hill, 3 edition.
Chiou, S.-Y. and Liao, Z.-Y. (2018). A Real-Time, Au-
tomated and Privacy-Preserving Mobile Emergency-
Medical-Service Network for Informing the Closest
Rescuer to Rapidly Support Mobile-Emergency-Call
Victims. IEEE Access, 6:35787–35800.
Crawford, K., Morphet, J., Jones, T., Innes, K., Griffiths,
D., and Williams, A. (2014). Initiatives to reduce
Algorithmic State Machine Design for Timely Health Emergency Management in an IoT Environment
155

overcrowding and access block in Australian emer-
gency departments: A literature review. Collegian,
21(4):359–366.
Magloire, R., Mung, K., Cookson, S., Tappero, J., Barzilay,
E., Dominguez, K., Dubray, C., Lindblade, K., Jentes,
E., Willis, M., Tohme, R., Sprecher, A., Bcheraoui,
C. E., and Walldorf, J. (2010). Rapid Establishment of
an Internally Displaced Persons Disease Surveillance
System After an Earthquake — Haiti, 2010. Morbidity
and Mortality Weekly Report (MMWR), 59(30):939–
945.
Manley, M., Kim, Y. S., Christensen, K., and Chen, A.
(2016). Airport Emergency Evacuation Planning: An
Agent-Based Simulation Study of Dirty Bomb Sce-
narios. IEEE Transactions on Systems, Man, and Cy-
bernetics: Systems, 46(10):1390–1403.
Meacock, R., Anselmi, L., Kristensen, S. R., Doran, T., and
Sutton, M. (2017). Higher mortality rates amongst
emergency patients admitted to hospital at weekends
reflect a lower probability of admission. Journal of
Health Services Research and Policy, 22(1):12–19.
Mujeebu, M. A. (2016). The Disappearance of MH370 and
the Search Operations–The Role of Technology and
Emerging Research Challenges. IEEE Aerospace and
Electronic Systems Magazine, 31(3):6–16.
Park, E., Kim, J. H., Nam, H. S., and Chang, H.-J. (2018).
Requirement Analysis and Implementation of Smart
Emergency Medical Services. IEEE Access, 6:42022–
42029.
Samani, H. and Zhu, R. (2016). Robotic Automated Exter-
nal Defibrillator Ambulance for Emergency Medical
Service in Smart Cities. IEEE Access, 4:268–283.
Seneviratne, S., Hu, Y., Nguyen, T., Lan, G., Khalifa, S.,
Thilakarathna, K., Hassan, M., and Seneviratne, A.
(2017). A Survey of Wearable Devices and Chal-
lenges. IEEE Communications Surveys & Tutorials,
19(4):2573–2620.
Wu, Q. and Ren, F. (2016). Emergency Management Ca-
pability Evaluation System in Civil Aviation Indus-
try. International Conference on Industrial Informat-
ics, China.
Wu, X., Dunne, R., Yu, Z., and Shi, W. (2017). STREMS:
A Smart Real-time Solution Toward Enhancing EMS
Prehospital Quality. IEEE/ACM International Confer-
ence on Connected Health: Applications, Systems and
Engineering Technologies (CHASE), USA.
Yu, L., Chan, W. M., Zhao, Y., and Tsui, K.-L. (2018). Per-
sonalized Health Monitoring System of Elderly Well-
ness at the Community Level in Hong Kong. IEEE
Access, 6:35558–35567.
SENSORNETS 2020 - 9th International Conference on Sensor Networks
156
