
Investigating the Gait of Lower Limb Amputees Regarding the
Present Classification of Mobility Grades
Katja Orlowski
1
, Kai-Uwe Mrkor
1
, Harald Loose
1
, Stephanie John
2
and Kerstin Witte
2
1
Department of Computer Science and Media, University of Applied Sciences Brandenburg,
Magdeburger Str. 50, 14770 Brandenburg/Havel, Germany
2
Institute III: Philology, Philosophy and Sport Science, Otto-von-Guericke University Magdeburg,
Zschokkestr. 32, 39104 Magdeburg, Germany
Keywords: Gait Parameters, Transfemoral Amputees, Mobility Grade, Objectivity.
Abstract: The mobility grade determined for German patients with a lower limb amputation based on the profile survey,
which is a subjective classification in one of the five mobility grades (0 to 4). It is recommendable to establish
objective examinations to determine the mobility grade of lower limb amputees. Gait parameters captured
with mobile sensors could be suitable for the distinction between amputees of the different groups (grade G2,
G3 or G4). Within a study, standard gait parameters were determined with the InvestiGAIT system based on
inertial sensors. A descriptive analysis of the data of the twenty-one subjects (G2: 4, G3: 6, G4: 11) indicates
that there are gait parameter (especially gait velocity, step and stride length) which can be used to make the
classification of the three mobility grades. The temporal gait parameters (stride duration, swing and stance
phase, one-leg-stance and double-leg-support) as well as angles during heel strike and toe off can be addition-
ally used for the classification. Nevertheless, further investigations have to done to get a larger database in
order to confirm the presented results regarding generalization and to check, whether the found classification
can be implemented as a kind of decision support system.
1 INTRODUCTION
The Medicare’s Functional Classification Level
(MFCL) system is used to distinguish persons with
lower limb loss in five functional levels (K-Level-0
to K-Level-4) (Balk et al., 2018). This classification
is based on the level of the amputee to walk with his
prosthesis (Agrawal et al. 2013a, 2013b, Gailey et al.
2002, 2006, Theeven et al. 2013). The established
MFCL system is a kind of an activity level categori-
zation (Dudek et al., 2008), which is questioned by
different researchers and research groups due to its
subjectivity. In Germany, a similar system is used for
the classification of lower limb amputees in order to
specify which prosthesis components should be fi-
nanced by the health insurances or other funding
agencies (e.g. trade association). The system is called
mobility grades and has the same categories as the
U.S. MFCL system. This classification is based on the
profile survey sheet of the German Medical Service
of Leading Associations of Healthcare Insurance Pro-
viders, which is also a very subjective assessment
(MDS, 2008).
Addressing the lack of objectiveness, Gailey et al.
(2002) developed the Amputee Mobility Predictor
(AMP), which is a clinical tool existing in two ver-
sions: AMPPRO (assessment with prosthesis) and
AMPnoPRO (assessment without prosthesis). The
AMP system is a 21-item measuring instrument con-
sidering different functional abilities such as sitting,
standing, walking, balancing, etc. As described in the
AMP instrument instructions, the average time for an
experienced examiner is less than ten minutes. The
low examination time is a big advantage of the AMP
tool. The result depends on the experience of the ex-
aminer. It is a “point system” with a maximum score
of 47 points, where the examiner assigns a number of
points (0 to 1, 0 to 2 or 0 to 5) per item (Gailey et al.,
2002). However, objective measures based on a stop-
watch are included in the AMP tool.
Nevertheless, the classification should be based
on an objective assessment. Agrawal et al. (2013a,
2013b) showed that there are different parameters
(such as external work and symmetry of work) which
are changing wearing different feet classified for the
functional level (tested K1-, K2- and K3-foot and gait
training with the different feet). That is why objective
336
Orlowski, K., Mrkor, K., Loose, H., John, S. and Witte, K.
Investigating the Gait of Lower Limb Amputees Regarding the Present Classification of Mobility Grades.
DOI: 10.5220/0009175703360341
In Proceedings of the 13th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2020) - Volume 4: BIOSIGNALS, pages 336-341
ISBN: 978-989-758-398-8; ISSN: 2184-4305
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

methods should be used to find the best setting of
prosthesis components for each affected person.
A current research project deals with the develop-
ment of a diagnosis system based on different sensors
measuring and quantifying the abilities of the lower
limb amputees:
(1) the power of the hip muscles (maximum power,
endurance),
(2) the balance (static and dynamic), and
(3) the flexibility of the hip joint.
The developed diagnosis system addresses the
lack of objectiveness of the German profile survey ac-
tually used for the classification. The aim of the pro-
ject is the examination of different parameters
(power, balance, flexibility) regarding their potential
to be used for the determination of the mobility grade
(G0 to G4). Besides static and dynamic balance tests
conducted on a force plate, the gait of amputees is an
additional indicator of the dynamic balance, which is
also examined in the current research project. It could
be conducted without the diagnosis system and used
as an additional objective indicator.
The amputee gait is captured using the Investi-
GAIT system (Orlowski et al., 2015, 2016, 2017).
The results of the gait analysis are presented regard-
ing the classification of the transfemoral amputees
into one of the three mobility grades (G2 to G4),
which was performed during their individual clinical
or rehabilitation process after the amputation.
This paper attempts to answer the following ques-
tion: Are there gait parameters, which are different for
amputees of different mobility grades?
2 MATERIALS & METHODS
The InvestiGAIT system consisting of four inertial
sensors (6-DOF) is used to capture the gait of the
sub-
jects on a 9 m or 13 m long straight walkway, respec-
tively
1
. Two sensors are attached to the distal part of
the lower leg, slightly above the ankle, and two are
fixed to the upper body (in the middle of the posterior
superior iliac spine and at cervical vertebra II) using
elastic straps (Orlowski et al., 2017). The subjects were
asked to walk the walkway at least 12 times with their
self-selected gait velocity.
In-/Exclusion Criteria:
Subjects with a unilateral transfemoral amputation of
the lower limb were included in the study. The age cri-
teria was determined to 18 to 65 years, but due to dif-
ficulties to find enough subjects fulfill this criteria also
subjects older than 65 years were approved to the
study, when they feel healthy enough to perform the
given tests of the study (examination of power, bal-
ance, mobility and gait)
.
Participants:
Overall, twenty-one subjects with unilateral transfem-
oral amputation of the lower limb took part in the ex-
amination. Table 1 shows the distribution of subjects
in the mobility grades. Additionally, table 1 presents
the number of subjects, their mean age, body height,
stump length and time since amputation for each grade.
Informed written consent was obtained from all
subjects prior to study participation. The study was ap-
proved by the local ethics committee of the Otto-von-
Guericke university Magdeburg (no. of vote: 31/18)
and carried out in line with the Declaration of Helsinki
.
Data Analysis:
The gait parameters were calculated from the captured
acceleration and angular velocity based on the detec-
tion of gait events (initial contact (IC), midswing point
and terminal contact (TC)). The first two trials were
omitted from further statistical analysis due to their
training effect. The calculations were performed using
the in-house software InvestiGAIT developed in
MAT-LAB™ (TheMathworks Inc., Natick, MA,
USA).
Table 1: Anthropometric data (age body height, stump length and time since amputation) of the subjects with transfemoral
amputation. The number of subject per group (mobility grade) is given.
Mobility
Grade
Number of subjects
(male, female)
Age (yrs)
mean±sd
Height (cm)
mean±sd
Stump length (cm)
mean±sd
Time since Amputation (yrs)
mean±sd
G2
4
(4 m, 0 f)
69.8
(±13.1)
177.5
(±14.1)
26.0
(±10.2)
33.0
(±30.1)
G3
6
(4 m, 2 f)
63.5
(±11.6)
174.8
(±7.8)
30.8
(±4.5)
20.5
(±13.8)
G4
11
(11 m, 0 f)
49.3
(±12.3)
182.9
(±7.0)
37.4
(±12.5)
13.1
(±13.0)
1
The investigations were conducted in both institutions
(Brandenburg and Magdeburg).
Investigating the Gait of Lower Limb Amputees Regarding the Present Classification of Mobility Grades
337
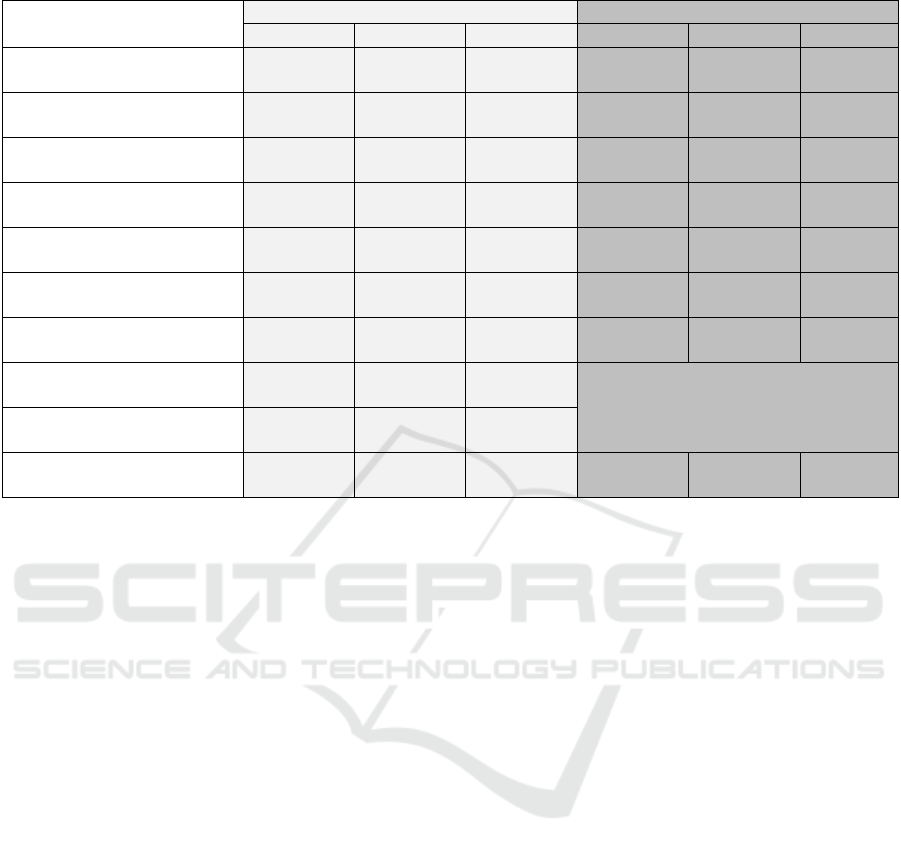
Table 2: Gait parameters as mean value and standard deviation.
Parameters
Affected Leg Sound Leg
G2 G3 G4 G2 G3 G4
Stride (s)
1.35
(± 0.20)
1.12
(± 0.09)
1.13
(± 0.09)
1.34
(± 0.20)
1.12
(± 0.09)
1.13
(± 0.08)
Swing (%)
40.60
(± 5.38)
43.97
(± 9.56)
47.53
(± 5.23)
38.63
(± 1.82)
43.12
(± 2.51)
42.08
(± 3.27)
Stance (%)
59.40
(± 5.38)
56.03
(± 9.56)
52.47
(± 5.23)
61.37
(± 1.82)
56.88
(± 2.51)
57.92
(± 3.27)
One-Leg-Stance (%)
38.50
(± 1.90)
43.09
(± 2.56)
42.04
(± 3.42)
40.64
(± 5.39)
43.93
(± 9.51)
47.52
(± 5.37)
Double-Leg-Support (%)
18.86
(± 6.86)
12.69
(± 9.04)
10.49
(± 5.36)
16.92
(± 7.65)
12.87
(± 9.16)
10.49
(± 5.28)
Put-on-angle (°)
15.61
(± 2.61)
17.85
(± 5.84)
23.33
(± 3.57)
18.64
(± 4.75)
17.81
(± 2.02)
19.05
(± 4.09)
Take-off-angle (°)
-38.40
(± 2.69)
-38.97
(± 6.05)
-42.38
(± 7.24)
-40.23
(± 6.87)
-40.84
(± 5.18)
-44.40
(± 7.92)
Gait velocity (m/s)
0.77
(± 0.15)
1.16
(± 0.14)
1.31
(± 0.17)
Same Values as affected Leg, these pa-
rameters are not determined separately for
each leg
Stride length (m)
1.01
(± 0.08)
1.29
(± 0.10)
1.47
(± 0.14)
Step length (m)
0.60
(± 0.06)
0.71
(± 0.09)
0.77
(± 0.11)
0.62
(± 0.06)
0.73
(± 0.07)
0.85
(± 0.06)
Due to the small sample size a descriptive data
analysis was conducted. The mean values and stand-
ard deviation of standard gait parameters were con-
sidered to give an overview of the difference between
the groups (e.g. G2, G3, G4).
3 RESULTS
Table 2 contains the mean value and the standard de-
viation of the gait parameter displaying an overview
of the characteristics of the found differences of the
three considered groups (G2, G3 and G4). Further-
more, a comparison of both legs of each group and
compared to the other groups is possible.
The parameters gait velocity, stride and step
length show a clear increase from G2 over G3 to G4.
This increase can be registered for the affected and
the sound leg. While the gait velocity and the stride
length are the same for both legs, a difference for the
step length of the affected and the sound leg is clearly
visible. On average the step length of G2 (0.60 and
0.62 m) and G3 (0.71 and 0.73 m) is shorter than the
step length of G4 (0.77 and 0.85 m). Moreover, the
difference between the affected and the sound legs is
smaller in amputees of G2 and G3 (0.02 m) compared
to amputees of G4 (0.08 m).
Regarding the take-off-angle, it can be noted that
the mean values of the amputees G2 and G3 (affected:
-38.40 and -38.97°; sound: -40.23 and -40.84°) are
similar having a larger difference to the mean of the
G4 (affected: -42.38°; sound: -44.40°). The parame-
ters stride duration (s), stance phase (%), and double-
leg-support (%) show a decrease with the higher mo-
bility grades (G2 to G4), while the parameter swing
phase (%) and one-leg-stance (%) have an increase
for higher mobility grades with one exception of the
G3 for the affected leg.
4 DISCUSSION
The results suggest that a distinction between ampu-
tees of the mobility grades G2, G3 and G4 is possible
using the presented gait parameters. The gait param-
eters gait velocity, stride length and step length seem
to be characteristic and suitable for describing the
three considered mobility grades. All the other pa-
rameter are as well characteristic and can be addition-
ally used for the classification of transfemoral ampu-
tees based on gait analysis.
Batten et al. (2019) examined the gait speed of
amputees (transtibial 78, transfemoral 30, and knee
disarticulation 2 with mean age 63 (±13), range 24-85
years) based on the 10-m walk test, whereby the pa-
tients walked 12 m indoors on even floor. The deter-
mined gait speed found by Batten et al. (2019) was
slower for all groups (K2: 0.38 (0.25-0.54); K3: 0.63
(0.50-0.71); K4: 1.06 (0.95-1.18)) as well as for the
BIOSIGNALS 2020 - 13th International Conference on Bio-inspired Systems and Signal Processing
338

whole group (median (IQR): 0.52 (0.37-0.67), with a
range from 0 to 1.43 m/s).
Lemaire et al. (1993) published the average gait
speed for elderly transtibial amputees (8 subjects,
mean age of 68.75 (66 to 72) years) which is compa-
rable (mean: 1.20 (0.95 - 1.46) m/s) to the gait speed
determined in our examination. Unfortunately, no in-
formation about the mobility grade of the subjects is
given. Lemaire et al. (1993) compared the determined
gait speed with those of other investigations of ampu-
tees of little lower age groups (55-67 years, 43-77
years, 21-73 years, 39-57 years, 36 -76 years) detect-
ing an average speed ranging from 0.75 to 1.22 m/s
(1.22 m/s, 1.07 m/s, 1.07 m/s, 1.17 m/s, 0.75 m/s).
Lemaire et al. (1993) also investigated the aver-
age stride length of elderly amputees. A comparison
with data from other studies is presented. Lemaire et
al. (1993) determined an average stride length of
1.41 m of the subjects (mean age of 68.75 years)
which is little higher than the stride length found in
the other studies (range 1.10 to 1.40 m). Based on the
distinction in the mobility grades in our investigation
the determined stride length is comparable and com-
prehensible (G2: 1.01 m, G3: 1.29 m and G4: 1.47 m).
The main advantage of the gait analysis using the
InvestiGAIT system is the simplicity of usage. Gait
captures and analysis can be done within a few
minutes, are feasible almost anywhere and no large
spaces are needed. These facts support the usage in
the daily clinical routine. In contrast to the Investi-
GAIT system or other mobile gait analysis systems
(GAITRite walkway, MVN Biomech from Xsens),
3D motion capture systems (Vicon) or specialized
systems (GRAIL - Gait Real-time Analysis Interac-
tive Lab (Oude Lansink et al., 2017) or CAREN -
computer-assisted research environment (Darter and
Wilken, 2011)) are not very interesting for doctors
and clinicians working with patients in the clinical
routine due to time aspects. These systems have a
large overall complexity (required space, knowledge,
time) and do not appear to be appropriate for the clin-
ical routine.
Compared to 3D-systems the accuracy of inertial
gait systems is sometimes lower, especially to spatial
gait parameters, e.g. step and stride length. These pa-
rameters are affected by systematic errors. Due to
those facts, these parameters have small deviations.
Limitations of the Study:
Most of the subjects (38 % and 47 %) investigated in
this study were categorized with mobility grade 3 and
4. The mean age of these both groups are 59.1 (±10.9)
and 46.1 (±12.2) years. Considering the facts, it
should be noted that the more active and slightly
younger persons affected from lower limb loss took
part in the examination. While the group of subjects
with mobility grade 4 consists of 20 % persons older
than 62 years, 40 % older than 55 years and 40 %
younger than 40 years, the age distribution in G3 is
different. Within the group G3, there were 33.3 % of
subjects older than 63 years and 91.7 % older than 50
years. This does not seem to be representative of the
total amputee population.
Furthermore, the number of subjects (G2: 4, G3:
6, G4: 11) within each group has to be critically
viewed. Consequently, the results should be regarded
as tendency and a generalization is currently not pos-
sible.
There is another limitation in this study. The anal-
ysis strongly relied on the assessment of the grade of
mobility done by the subject's orthopedic techni-
cian/physician. Wurdeman et al. (2014) stated some
reasons why this is problematic: “[…] the ambiguity
under which patients are classified (Gailey et al.,
2002) and the undeniable fact that the activity level
for individuals ambulating with a prosthesis is not
possibly four distinct categories but rather repre-
sented as a continuum across a spectrum. The only
clinical tool available currently to help with patient
classification in the Amputee Mobility Predictor
(Gailey et al., 2002), but even this tool is known to
have large standard deviations making it difficult on
the individual level to objectively categorize pa-
tients.”. Gailey (2006) indicated that professionals are
able to determine the needs of the patients based on
their long-lasting experience, but there were exami-
nations from Stephen and Aitken (1987) showing that
significant differences in classifications of amputees
(assessment of mobility and self-care) were found in
clinicians of the same rehabilitation team. For that
reason, the validity of the subjective classification has
to be questioned. It is, therefore, particularly im-
portant to develop objective methods to classify the
patients. Additionally, it is necessary to implement
objective methods to find out which prosthesis com-
ponents are the best for each individual.
5 CONCLUSION
The results of the study indicate that selected gait pa-
rameters have the potential to be used to distinguish
amputees of different mobility grades. Considering
the three groups (G2, G3 and G4), the gait parameters
gait velocity, stride and step length show clear differ-
ences for all three comparisons (G2 vs G3, G2 vs G4,
G3 vs G4). These parameters are characteristic for the
gait of amputees of different mobility grades investi-
gated in the presented study. All the other presented
Investigating the Gait of Lower Limb Amputees Regarding the Present Classification of Mobility Grades
339

gait parameters seem to be additionally useful for an
objective classification of transfemoral amputees.
The potential of the gait parameters contributing
to objective assessment has to be confirmed with fur-
ther investigations. Based on a larger sample size a
statistical analysis have to be performed in order to
make generalized statements and to develop an algo-
rithm to establish a decision support system for the
classification of patients with a transfemoral amputa-
tion in one of the three considered mobility grades.
Furthermore, it could be recommendable for fur-
ther studies to use the AMP tool additionally to the
determined mobility grade based on the profile survey
in order to have supplementary information.
ACKNOWLEDGEMENT
The authors are grateful for all subjects volunteering
to participate in this study. We also thank the German
Central Innovation Program SME (Zentrales Innova-
tionsprogramm Mittelstand - ZIM) for supporting the
project ‘‘Multifunctional diagnostic machine for pa-
tients of lower limb amputations” (ZF4096303TS6:
Multifunktionales Diagnostikgerät für Amputa-
tionspatentien) in which the diagnostic machine was
developed in cooperation with Guenther Bionics
GmbH and Peuker GmbH.
The authors wants to thank Hagen Theuer who
wrote his Bachelor Thesis in the course of the ZIM
project.
REFERENCES
Agrawal V, Gailey RS, O’Toole C, Gaunaurd I, Finnieston
A (2013). Influence of gait training and pros-thetic foot
category on external work symmetry during unilateral
transtibial amputee gait. Prosthetics and Orthotics In-
ternational, 37(5), 396–403. DOI: https://jour-
nals.sagepub.com/doi/10.1177/0309364612473501
Agrawal V, Gailey RS, Gaunaurd IA, O’Toole C, Fin-
nieston AA (2013). Comparison between micro-proces-
sorcontrolled ankle/foot and conventional prosthetic
feet during stair negotiation in people with unilateral
transtibial amputation. J Rehabil Res Dev. 2013; 50(7):
941–50. http://dx.doi.org/10.1682/JRRD.2012.05.0093
Balk EM, Gazula A, Markozannes G, et al. (2018). Lower
Limb Prostheses: Measurement Instruments, Compari-
son of Component Effects by Subgroups, and Long-
Term Outcomes [Internet]. Rockville (MD): Agency
for Healthcare Research and Quality (US); 2018 Sep.
(Comparative Effectiveness Review, No. 213.) Table 1,
Lower limb extremity prosthesis Medicare Functional
Classification Levels (K levels) Available from:
https://www.ncbi.nlm.nih.gov/
books/NBK531517/table/ch2.tab1/, (Online: 6.11.
2019)
Batten, H. R., McPhail, S. M., Mandrusiak, A. M., Var-
ghese, P. N., & Kuys, S. S. (2019). Gait speed as an
indicator of prosthetic walking potential following
lower limb amputation. Prosthetics and Orthotics Inter-
national, 43(2), 196–203. DOI: https://doi.org/
10.1177/0309364618792723
Darter BJ, Wilken JM (2011). Gait training with virtual re-
ality-based real-time feedback: improving gait perfor-
mance following transfemoral amputation. Phys Ther.
2011; 91(9): 1385–94. DOI: https://doi.org/
10.2522/ptj.20100360 PMID: 21757579
Dudek NL, Khan OD, Lemaire ED, Marks MB, Saville L
(2008). Ambulation monitoring of transtibial amputa-
tion subjects with patient activity monitor versus pe-
dometer. Journal of Rehabilitation Research & Devel-
opment 2008; 45 (4): 577–586.
Gailey R, Roach K, Applegate B, Nash M (2002). The Am-
putee Mobility Predictor (AMP): an instrument to as-
sess determinants of the lower limb amputee’s ability to
ambulate. Arch Phys Med Rehab 2002; 83: 613–627.
MDS Essen (ed.) (2008). Profilerhebungsbogen für die
Versorgung mit Beinprothesen. URL: https://www.
gkv-spitzen-ver-band.de/media/dokumente/krankenver
sicherung_1/hilfsmittel/fortschreibungen_aktuell/aelter
e/HiMi_Fortschr_Profilerhebungsbogen_Produktgrup
pe_24_2008.pdf, (Online: 18.11.2019).
Gailey RS (2006). Predictive Outcome Measures Versus
Functional Outcome Measures in the Lower Limb Am-
putee. American Academy of Orthotists and Prosthe-
tists. 2006; (6): 51-60.
Orlowski K, Loose H, Eckardt F, Edelmann-Nusser J, Witte
K (2015). Analyzing the Transfemoral Am-putee Gait
Using Inertial Sensors - Identifying Gait Parameters for
Investigating the Symmetry of Gait - A Pilot Study. In-
ternational Conference on Bio-inspired Systems and
Signal Processing (BIOSIGNALS), Lisbon, Portugal,
12.-15. January 2015.
Orlowski K, Loose H, Eckardt F, Edelmann-Nusser J, Witte
K (2016). Evaluation of gait parameters determined by
InvestiGAIT against a reference system. International
Conference on Bio-inspired Systems and Signal Pro-
cessing (BIOSIGNALS), Rome, Italy, February 2016.
Orlowski K, Eckardt F, Herold F, Aye N, Edelmann-
Nusser, J, Witte K (2017). Examination of the reli-abil-
ity of an inertial sensor-based gait analysis system. Bi-
omed. Eng.-Biomed. Tech. 2017; DOI 10.1515/bmt-
2016-0067.
Oude Lansink ILB, van Kouwenhove L, Dijkstra PU,
Postema K, Hijmans JM (2017). Effects of inter-ven-
tions on normalizing step width during self-paced dual-
belt treadmill walking with virtual reality, a randomized
controlled trial. Gait & posture. 2017; 58: 121–5.
Stephen P, Aitken R (1987). Morbidity survey of lower
limb amputees. Clin Rehabil 1987;1:181–186.
Theeven PJR, Hemmen B, Brink PRG, Smeets RJEM,
Seelen HEM (2013). Measures and procedures utilized
BIOSIGNALS 2020 - 13th International Conference on Bio-inspired Systems and Signal Processing
340

to determine the added value of microprocessor-con-
trolled prosthetic knee joints: a systematic review. BMC
Musculoskeletal Disorders 2013 14:333.
Wurdeman SR, Myers SA, Jacobsen AL, Stergiou N (2014)
Adaptation and Prosthesis Effects on Stride-to-Stride
Fluctuations in Amputee Gait. PLoS ONE 9(6): e100125.
doi:10.1371/journal.pone.0100125
Investigating the Gait of Lower Limb Amputees Regarding the Present Classification of Mobility Grades
341
