
Towards Adoption of Standards for Communication
Infrastructure/Technologies in Healthcare Systems in LMICs:
Theories, Practice and Evaluation
Andrew Alunyu Egwar
1,2
, Richard Ssekibuule
2
and Josephine Nabukenya
2
1
Department of Computer Engineering, Busitema University, Tororo, Uganda
2
Department of Information Systems, Makerere University, Kampala, Uganda
Keywords: Adoption, Communication Infrastructure, Health Information Exchange, Ehealth, Readiness, Standards.
Abstract: While electronic health offers great promise to improve healthcare in low and middle-income countries
(LMICs), the communication infrastructure/technologies (CI/T) requires standards to improve the current
state of none to limited interoperability. This study reviewed theories that inform the assessment of the health
system’s readiness to adopt ehealth CI/T standards. The study involved a scoping review of published articles
reporting adoption to the use of ICT, technologies, and standards in health. Articles published in English
between 2012-2019 were identified through PubMed Central and Google Scholar. Also, grey literature from
websites of WHO, standards development organisations and Uganda’s Ministry of Health were searched.
Data extraction involved coding to identify key themes that inform the readiness of health systems to adopt
standards for eHealth CI. Of the 3,817 published articles, only 32 met the inclusion criteria. 17 grey literature
was also included in our discussion. Results identified determinants for eHealth CI/T and that concepts from
the technology adoption theories can be used as metrics to assess readiness to adopt standards for ehealth
CI/T. The metrics for drivers to adopt standards were higher than inhibitors in Uganda’s health system. The
metrics will lead to the development of a readiness assessment framework.
1 BACKGROUND
Electronic health (ehealth) has lately received much
attention from various health stakeholders. However,
much of ehealth technological developments have
remained fragmented and mostly proprietary,
contributing to a lack of interoperability between
health information systems and supporting technology
(Fontaine et al., 2010; Neuhaus et al., 2011; Tamburis
et al., 2012). Consequently, many ehealth initiatives
have not scaled up (Huang et al., 2017; Kiberu et al.,
2017; McCann, 2012). This greatly hinders the
attainment of the ehealth key goal which is access to
health information by authorised persons when and
where required. According to the IEEE standards site,
interoperability is the ability of a system to work with
other systems without special effort on the part of the
user (IEEE Website, n.d.). In this concept,
interoperability allows health data / information
generated by one system to be accessible and
meaningfully reusable to another system, whether or
not they are based on different technologies. Health
system access to data or information is achieved over a
communication network, which should also be
interoperable. This study focuses on the
interoperability of the secure communication
infrastructure required to support health data transfer
and information exchange (Kuziemsky and Peyton,
2016).
Communication infrastructure (CI) consists of
communication hardware, software and network
interfaces that share healthcare information between
stakeholders (Gillwald, 2008; Yiming et al., 2016).
Implementation and use of the CI should follow
uniform standards across the healthcare system.
Standards are specifications necessary for proper co-
existence and interoperability of communicating
systems, necessary for meeting national and
international regulations (Adebesin et al., 2013;
European Telecommunications Standards Institute,
2013; ITU-T, 2012). Standards are rules for common
and voluntary use, decided by one or several people or
organisations (Brunsson et al., 2012). Regards ehealth,
standards guide the capture, storage, exchange, and
secure use of ehealth information (Vincent et al., 2015;
WHO, 2013). For the CI/T, the standards do describe
Egwar, A., Ssekibuule, R. and Nabukenya, J.
Towards Adoption of Standards for Communication Infrastructure/Technologies in Healthcare Systems in LMICs: Theories, Practice and Evaluation.
DOI: 10.5220/0009171907350744
In Proceedings of the 13th Inter national Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2020) - Volume 5: HEALTHINF, pages 735-744
ISBN: 978-989-758-398-8; ISSN: 2184-4305
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
735
accurately and unambiguously how information is
transmitted over the communication systems (Eduqas,
2015); similarly, ehealth CI standards must explicitly
specify how both the internal and external CI will
transmit health information across the health system.
Although, WHO recognises the need for electronic
transmission of personal requirements to adhere to
standards in health data and technology (WHO, 2013),
Adebesin et al., (2013) argue that adoption must pay
attention to specific requirements of a country such as
the available communication resources of the
communicating parties. In fact, consideration should
be made of the other ehealth and communication
constraints like the finance, human resources, etc
required to establish and maintain such communication
infrastructure. It is argued that, existing global ehealth
standards may not necessarily apply to resource-
constrained environments (Adebesin et al., 2013; ITU-
T, 2009). In this research context, particularly CI/T, the
concept of resource constrain will refer to data
communication inhibitions including but not restricted
to limited bandwidth; limited or no network
connectivity; limited ICT skills; and limited power
supply. Such environments provide unique
infrastructure, technical, and social constraints that
require innovative design approaches and need to be
guided by technology standards, standardized
terminologies, and data format and interoperability
standards (Anderson et al., 2012).
In addition, despite multiple benefits of health
information exchange (HIE) (Rahurkar et al., 2016), it
is challenged with a lack of suitable CI standards
(Kiberu et al., 2017; Uganda Ministry of Health, 2016).
For example, in Uganda’s context, a situation analysis
of its health system showed that 79% of the health
facilities had computers and 56% had some form of
Internet connectivity (Hindemark, 2013; Kiberu et al.,
2017; Ministry of Health, Republic of Uganda, 2015).
However, they are stand-alone, and this, amidst a
genuine acknowledgment for connectivity supporting
HIE poses the need to assess readiness to adopt
standards for ehealth CI/T.
Based on the definition of Rajiv and McLean,
(1998) and Rogers, (1983), who define adoption as a
formal process that may include an agreement between
ehealth stakeholders to use given standards in the entire
health system, we motion that to date Uganda has not
yet formally adopted ehealth standards specific to the
CI/T. In fact, LMICs lack guidelines, criteria, and
frameworks to guide the adoption of suitable ehealth
standards to support their healthcare systems.
Therefore, this study reviewed existing ehealth
standards and the technology adoption theories with an
aim to identify the barriers and motivators to adopting
standards and identify metrics for assessing the
readiness of healthcare systems in LMICs to adopt
standards for ehealth CI/T. Second, we used the
metrics to assess the readiness of Uganda’s health
system to adopt standards for ehealth CI/T.
2 METHODS
Two distinguished methods were used to achieve the
objectives of the scoping review and assessing
readiness to adopt standards. In order to achieve the
objectives of a scoping review, health informatics
literature was retrieved from PubMed Central and
Google Scholar. Additionally, grey literature
(standards development processes and government
reports) were retrieved from through website search. A
full search of PubMed Central was done. The
following keywords were used to retrieve relevant
documents: ‘electronic health’, ‘health information
exchange’, ‘standards’, ‘health technology’,
communication infrastructure’, and ‘resource-
constrained countries’. To exhaust the search,
keywords were replaced with synonyms. The search
retrieved 3,817 peer-reviewed articles on which we
applied the inclusion and exclusion criteria in Table 1.
With the exception of the definition of key
concepts/theories, the study only considered
publications between 2012-2018.
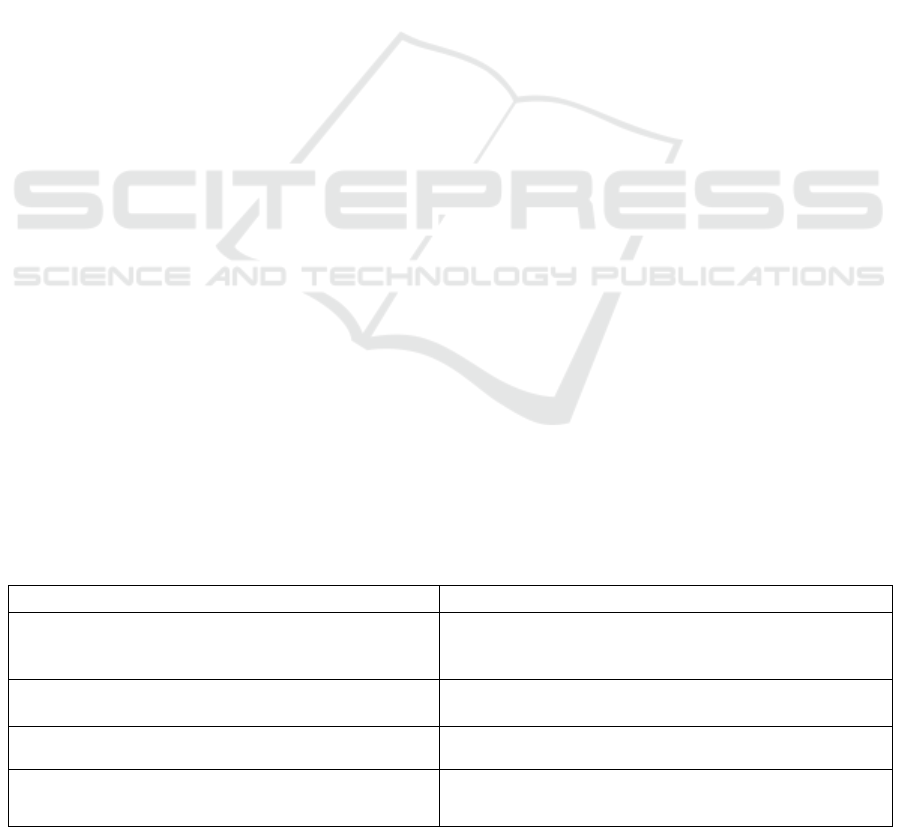
Table 1: Inclusion and Exclusion Criteria.
Inclusion criteria Exclusion criteria
Studies that focus on streamlining healthcare systems
(Health Management Information System, Electronic
Medical Records, etc) to ensure HIE
Studies that only focus on health data capture, processing
and storage or on research evidence, surveillance data,
survey data, or other non-routine sources and types of data.
Studies that focus on standardization of ehealth CI / T,
privacy and security of shared health data / information
Studies that focus on clinical health equipment /
technologies
Studies on ICT, technology & innovation adoption and
or diffusion-based on theories
Studies not specific to ICT technology / innovation
adoption nor based on theories of adoption / diffuse
Studies that examined organizational readiness to adopt
new technology / innovation
Studies that only made general consideration for adoption
of technology / innovation
HEALTHINF 2020 - 13th International Conference on Health Informatics
736

The authors independently coded and later agreed on
the emerging themes. Key themes were refined by a
discussion with experts from Uganda’s MoH.
The method followed to assess readiness to adopt
standards for ehealth CI/T involved the use of
secondary data from Uganda’s health system to assess
the country’s readiness. The data sources include
published articles and reports from the ministry of
health, NITA-U, and UCC that discuss ehealth in
Uganda. We also held informal discussions with 05
experts from the division of health informatics.
3 RESULTS
3.1 Literature Review
Only 53 studies, websites, and reports were included in
reporting the results of the review and subsequent
discussions. Key results of the review are presented in
two parts;
(A) Determinants for eHealth CI/T: Network
infrastructure consists of the hardware and software
resources for an entire network that enables
connectivity, communication, operations, and
management of an organisation’s network (Gillwald,
2008; Yiming et al., 2016). In the ehealth information-
sharing environment, communications include people-
to-people, people-to-things, and things-to-things
communications as well as the physical backbone for
all e-applications (ITU and UIT, 2017). Thus, ehealth
communication infrastructure includes the hardware
and the software of an entire communication network,
and the network backbone that supports healthcare
communication. Components of the CI/T supporting
HIE are shown in Table 2. Current modes of health
data communication include the sharing of text,
images, audio, and video (Al-Safadi, 2016; Widya et
al., 2003). These are multimedia content with high
communication requirements (Widya et al., 2003)
requiring the ehealth CI/T and network backbone to be
fast, flexible, large, reliable and with appropriate
security and privacy measures (Reid et al., 2005).
Table 2: Determinants of Health System Readiness to Adopt Standards for eHealth CI/T.
CI/T components
Brief Description
Use of ICT
networks
How the ICT network that supports healthcare is used as a contributing factor to the success of
ehealth data sharing. In fact, readiness is reflected by how ehealth technology users engage in the
use of existing data-sharing networks (Rezai-Rad et al., 2012).
Available hardware
and software
systems
The health system requires the hardware and software that support health data transmission
requirements. As such the standards must be adopted for these devices, equipment, and physical
security measures to harmonize the diversity and ensure interoperability.
Affordability
This is the organisation’s financial capacity to acquire and maintain ehealth communication
technologies. It also includes the cost of the bandwidth for health data transmission to other health
institutions, cost of hardware and software, maintenance cost and human resources. Similarly,
with ehealth standards, the concern is how accessible, open or affordable the specifications are to
the implementors (Baker et al., 2015).
Quality of
infrastructure
A measure of the quality (regards usability and performance) of the established CI/T.
Inappropriate infrastructure impacts usability and performance and therefore can negatively shape
the user attitudes towards health information systems (Cresswell and Sheikh, 2013). The
telecommunication service provider/governments supply part of the quality. It is important to
regulate the CI quality both internally (within the organisation) and externally.
Level of ICT
literacy and support
personnel
eHealth technology literacy levels of users and expertise of the support personnel are key in the
capture, storage, and sharing of health information. Whereas the perceived high level of ICT
literacy has a positive relationship to the adoption of technology (Ketikidis et al., 2012), anxiety
to use of technology negatively influences such adoption (Mac Callum and Jeffrey, 2014).
Equally, literacy level and support personnel influence the kind of standards adopted to guide the
implementation and use of ehealth CI/Ts.
eHealth CI security
& information
privacy
Privacy and security concerns of patient data and or information necessitates securing the CI/T
supporting HIE. The level of hardware and software security may influence security upgrades
(standards) to be adopted by the health system to protect health data (Rezai-Rad et al., 2012).
Towards Adoption of Standards for Communication Infrastructure/Technologies in Healthcare Systems in LMICs: Theories, Practice and
Evaluation
737

(B) Technology Adoption Theories: Review of the
technology adoption theories guided the selection of
metrics for assessing readiness to adopt ehealth
CI/T standards. Reviewed theories include;
Technology Adoption Model (TAM): TAM
focuses on the motivation of a technology user, the
‘perceived usefulness’ and ‘perceived ease of use’
(Godoe and Johansen, 2012; Taherdoost, 2018).
Perceived usefulness is the degree to which a person
believes the use of a particular system enhances his
or her job performance. Perceived ease of use is the
degree to which a person believes the use of a
particular system is free of effort. Although
perceived usefulness results from extrinsic
motivation (Godoe and Johansen, 2012) output
quality and perceived ease of use (intrinsic
motivation) have an impact on the perceived
enjoyment and perceived usefulness (Taherdoost,
2018). This raises user acceptance of a given
technology and or standard.
Technology Readiness Index: Technology
readiness (TR) index is the inclination to embrace
and use new technologies to accomplish routine
goals (Parasuraman, 2000; Son and Han, 2011). TR
are factors that foster or hinder the adoption of new
technologies (Liljander et al., 2006). It has four
dimensions of both positive and negative
technology-related beliefs, that is, optimism (a
belief that technology offers people increased
flexibility, control, and efficiency), innovativeness
(a tendency to be a technology pioneer and a
thought leader), discomfort (a belief that one can
lose control and be overwhelmed by technology),
and insecurity (distrust and skepticism about
technology and its ability to work properly)
(Parasuraman, 2000). Whereas optimism and
innovativeness are key drivers of technology
readiness propelling users towards new
technologies, discomfort and insecurity are
inhibitors of technology readiness, which hold users
back.
Diffusion of Innovation Theory (DOI):
Diffusion is the process where adopters become
aware of the standards over time and consider it for
adoption (Rogers, 1983). DOI is a process that
occurs as people adopt a new idea, product, practice,
and philosophy (Oliveira and Martins, 2011). The
process begins with an initial few who adapt to the
use of innovation, technology or standards, then
with the increase in their perceived usefulness and
perceived ease of use, more people and
organisations are driven to adopt its use. DOI covers
the technological context (all technologies that are
relevant to the organisation), characteristics of an
innovation (attributes that determine the rate of
adoption) (Baker, 2011), and adopter characteristics
(degree of being early or late adopters of
innovation) (Ramdani et al., 2013; Rogers, 1983).
Technology, Organisation, and Environment
(TOE): The TOE framework has components for
organisation characteristics (characteristics and
resources of the organisation), technology
characteristics, and environment characteristics
(Baker, 2011). TOE has been used to study the
adoption of different types of IT and IS innovations
(Rajiv and McLean, 1998). Unlike DOI, TOE
introduces environmental context besides the
technology and organisational contexts of
technology or innovation adoption. The
environment includes industry characteristics,
support structures, and regulations. The
environment characteristics influence decisions to
adopt and implement technological innovation in
the adopter organisation, therefore play a vital role
in the decision process to adopt technology and or
standards.
Internet Standards Adoption (ISA): According
to Hovav et al., (2004) standards adoption as
represented by the ISA model is a function of the
utility of the standard’s characteristics (individual
perspective) and the environment in which the
adopter operates (community perspective). ISA
framework acknowledges that besides the standards
features having high utility (useful features),
successful adoption requires an adoption
environment that is conducive (Hovav et al., 2004).
Both dimensions must be of high quality for the
standard to be fully adopted. Useful features of a
standard may appeal differently to potential
adopters. However, ISA does not consider
organisation characteristics that are fundamental to
the successful adoption of technologies and or
standards.
Table 3 presents a summary of the metrics
derived from the related technology adoption
theories (models and frameworks) that can be used
to assess readiness to adopt standards for ehealth
CI/T. Since none of the satisfies all the metrics, we
apply suggestion of Ketikidis et al., (2012) to
improved/develop a model to assess adoption in
health, The study argues that components/metrics
form TRI, TOE, and ISA can be integrated to assess
healthcare systems readiness to adopt standards for
CI/T. Thus, the study developed a framework (refer
to Figure 1) that integrates evaluation metrics from
TRI, TOE, and ISA to assess readiness to adopt
standards for CI/T.
HEALTHINF 2020 - 13th International Conference on Health Informatics
738
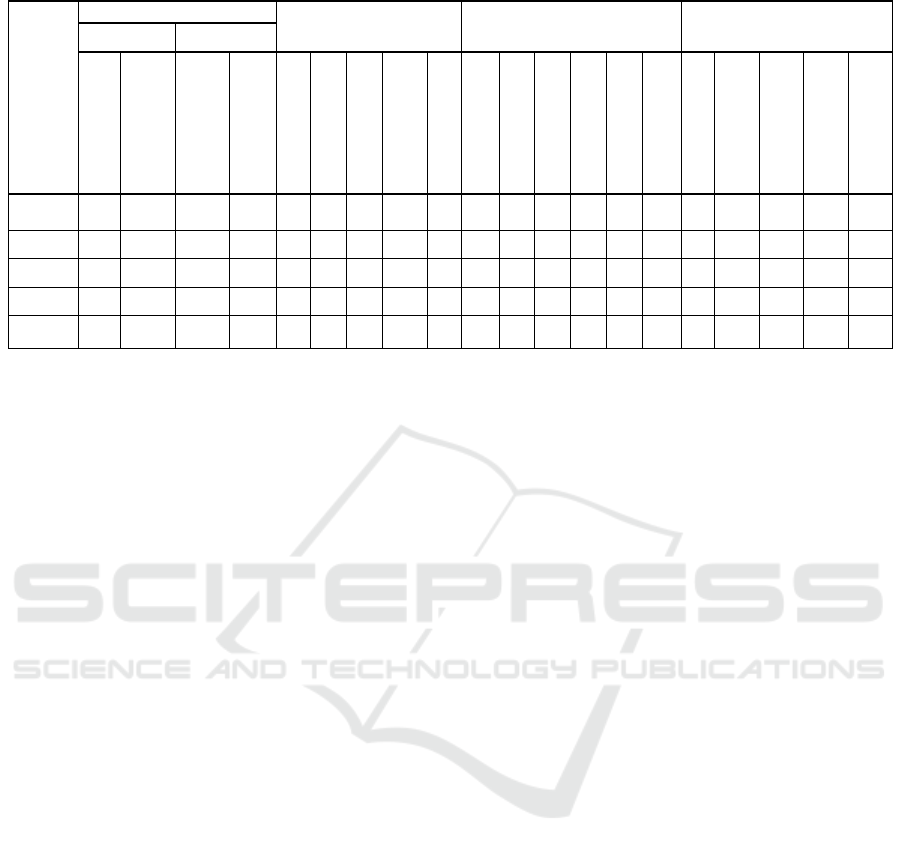
Table 3: Metrics for Assessing Technology / Innovation Adoption Readiness.
T
heories
Technology use belief
Characteristic of
adopter Organisation
Characteristics of a
technology / innovation
Deployment Environment
Usefulness Ease of use
Optimis
m
Innovativeness
Discomfort
Insecurit
y
Mangt support
Decision process
Organisation size
Use experience
Financial resource
Availabilit
y
Regulation
Compatibilit
y
Complexit
y
Trialabilit
y
Observabilit
y
N
etwork extensity
Related technology
Install base /scope
Competitive use
External support
TAM
─ ─ ─ ─ ─
─ ─ ─ ─ ─ ─ ─ ─ ─ ─
TRI
─ ─ ─ ─ ─
─ ─ ─ ─ ─ ─ ─ ─ ─ ─
DOI
─
─
─
─
TOE
ISA
─
─
Key. =Support the metric; =Do does not support metric; ─ =lack of sufficient information.
(C) Global Standards for eHealth CI/T: The study
identified the following about existing global
standards for ehealth; One, there are many and often
overlapping ehealth standards. Two, they are
developed by international standards organisations,
ITU and foreign governments to support ehealth.
Three, existing ehealth standards, both international
and national do support different dimensions of
ehealth. Those aligned to ehealth CI/T supporting
HIE span the breadth of communications of
electronic records, digital images, clinical
communications, and health information
communication. They include but are not limited to
ISO 12052:2017 Digital imaging and
communication in medicine; ISO 13606-5 EHR
communication for Interface specification;
ISO/HL7 27931 for data exchange; IEEE 11073 for
health devices; ENV 13606: Part 2 for archetype
interchange; CR- CEN for quality of service that
support health information interchange; IEEE
1073.3.x–standards for medical device
communications; ISO 27799:2016 for health
informatics information security management in
health; ISO/DTS 14441 for security and privacy of
EHR systems; CR 14301:2002 framework for
security protection of health care communication;
CR 14302:2002 framework for security
requirements of intermittently connected devices;
and ISO 17090-public key infrastructure for digital
certificates (HL7 International, 2017; IEEE
Website, n.d.; ISO, 2017).
(D) Metrics for Assessing Readiness to Adopt
Global Standards for eHealth CI/T: The metrics in
Table 3 can be customised to suitably assess
Uganda’s health system readiness to adopt
standards for ehealth CI/T to support HIE in
resource-constrained environments. The metrics are
categorised in Figure 1 as characteristics of the
standards for CI/T (ehealth CI/T standards),
characteristics of adopter organisation (adopter
environment) and standards implementation
environment (implementation environment)
(Hovav et al., 2004; Ramdani et al., 2013). To
examine the drivers and inhibitors of organisational
readiness to adopt self-service technologies, we
adopted Liljander et al., (2006) ideology; that is, an
organisation is likely to succeed in standards
adoption in cases where there are high optimism and
innovativeness (drivers for standards adoption) than
discomfort or insecurity (inhibitors) in use of the
standards. Drivers for standard adoption relate to
the high utility, while inhibitors relate to the low
utility. Besides, adopting internationally recognised
standards for ehealth CI, privacy and security
should in addition focus on the dynamics of
resource constrained environments, in our case
Uganda.
• Standards for eHealth CI/T – motivators for the
health system to adopt standards for ehealth
technology include availability of the standard;
perceived advantages from the adoption of such
a standard to support the existing and future
technologies; complexity of application stages,
severity of changes it can cause and clarity of
outcomes; possible forward and backward
compatibility with other standards and or
technologies from other vendors; trialability and
observability. Whereas trialability examines the
possibility of piloting and scaling to include the
entire healthcare system, observability is the
Towards Adoption of Standards for Communication Infrastructure/Technologies in Healthcare Systems in LMICs: Theories, Practice and
Evaluation
739
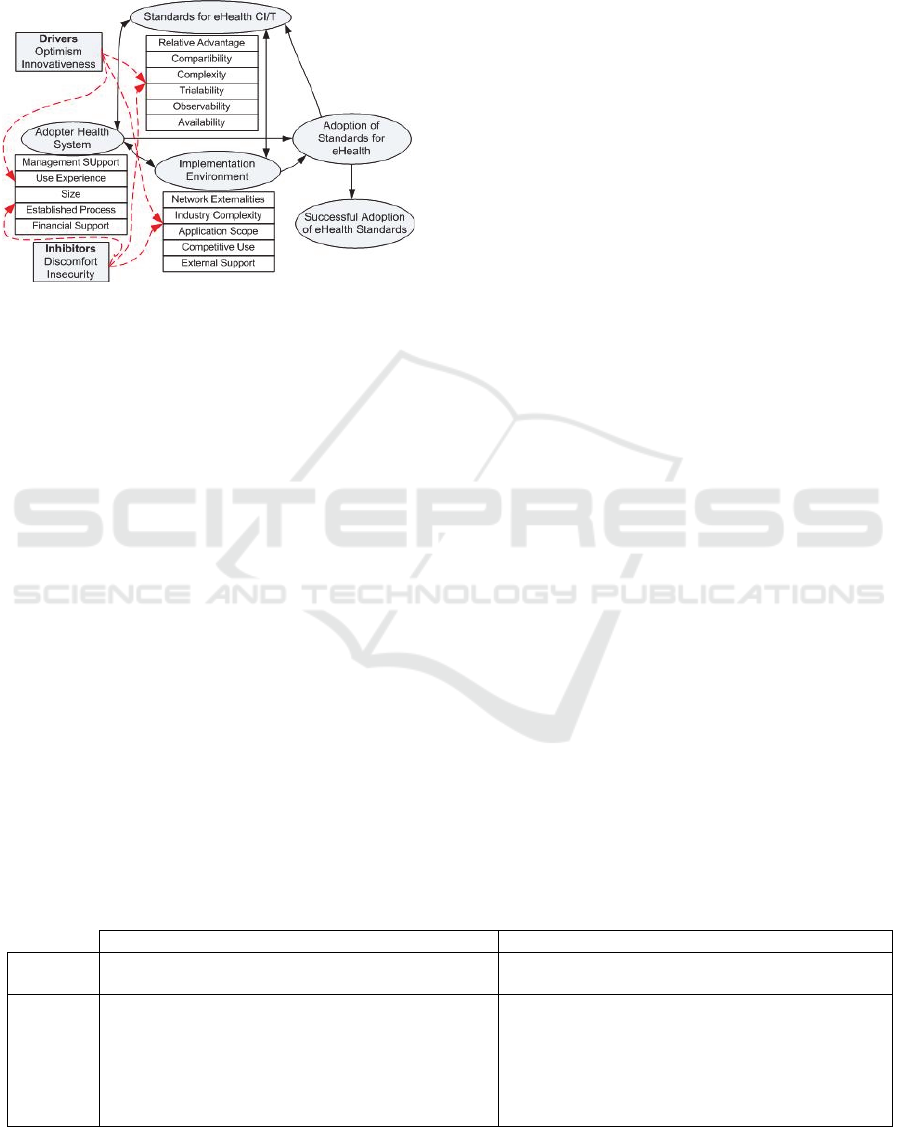
extent to which results of ongoing ehealth CI/T
standards processes can be observed due to the
selective perception of the beneficiary
stakeholders
Figure 1: Framework for assessing health system’s
readiness to adopt ehealth CI/T standards.
• Adopter Health System – the health system
management support, size, financing, standards
use experience, and standards adoption procedure
and use process, are factors that determine the
readiness of the health system and personnel to
successfully adopt and use the ehealth standards.
To assess the existence of any established
structured process for the adoption of the
standard, there is a need to evaluate the
management decision process to adopt and
enforce the use of the standards. Also, the
personnel capacity to comply with the set of
standards is paramount to the overall success of
any standards adoption. The organisational size
and financial capability are also key influencers
of adoption. A great size and a good financial
capacity imply more resources can be allocated to
support the adoption and implementation process
(Maunder et al., 2018).
• Implementation Environment – the standard
deployment environment imposes restrictions on
what is and what isn’t applicable. For example,
the need for patient safety technology may limit
the use of the radio frequency power levels of the
medical / healthcare sensors. We examine the
standards implementation environment in light of
the external pressures arising from the
complexity of the healthcare industry, the scope
of applicability of the standard being considered
across the healthcare system, the standards
competitive use and the existence of any external
support for the use of the adopted standard.
3.2 Assessing Readiness to Adopt
Standards for CI/T
(A) CI/T Status in Uganda’s Health System: As
presented in Table 4, results show that existing CI/T
in Uganda’s health system continues to be
characterized by rigid, small, slow, intermittent /
unreliable and insecure connections (Huang et al.,
2017; Kiberu et al., 2017; Uganda Ministry of Health,
2016).
(B) Status of eHealth CI/T Standards in Uganda:
The desired state is a set of standards that satisfices
all the metrics for the readiness of the health system
to adopt standards for ehealth CI/T. Thus, we review
current ehealth CI/T standards, both global and
Uganda’s as a case of resource-constrained setting.
Despite their existence, these standards have received
little attention in resource-constrained settings, both
via limited or no participation in their development
and or adoption to using (Adebesin et al., 2013;
Alunyu and Nabukenya, 2018). Both authors claim
there is no evidence of adoption or contextualization
of global standards by LMICs in the African region.
In order to examine their claim of no evidence of
adoption of ehealth standards by African countries
other than the ICD codes, we assessed the status of
adoption of ehealth CI/T standards in Uganda’s
health system. Thus, we used metrics for the
evaluation of technology adoption readiness from
Table 3 and obtained the result presented in Table 5.
The results are based on data from government
reports, MoH website, NITA-U website, and UCC
regards the status and use of ICT in healthcare.
Table 4: Current and envisioned standardised ehealth CI/T for Uganda’s health system.
Current state Envisioned state
Nature
Slow, rigid, small, unreliable and insecure
connections
Fast, scalable, robust, reliable, secure and private
connections
Charact-
eristics
• Diverse network devices
• Varied networked departments and services
• Variation in data transmission rates
• Limited/intermittent bandwidth/Internet
• Varied implementation and enforcement of
computer use’ security measure and levels
• Standardised implementation of network devices,
software, network protocols, and processes
• Existence of technical and institutional
interoperability
HEALTHINF 2020 - 13th International Conference on Health Informatics
740
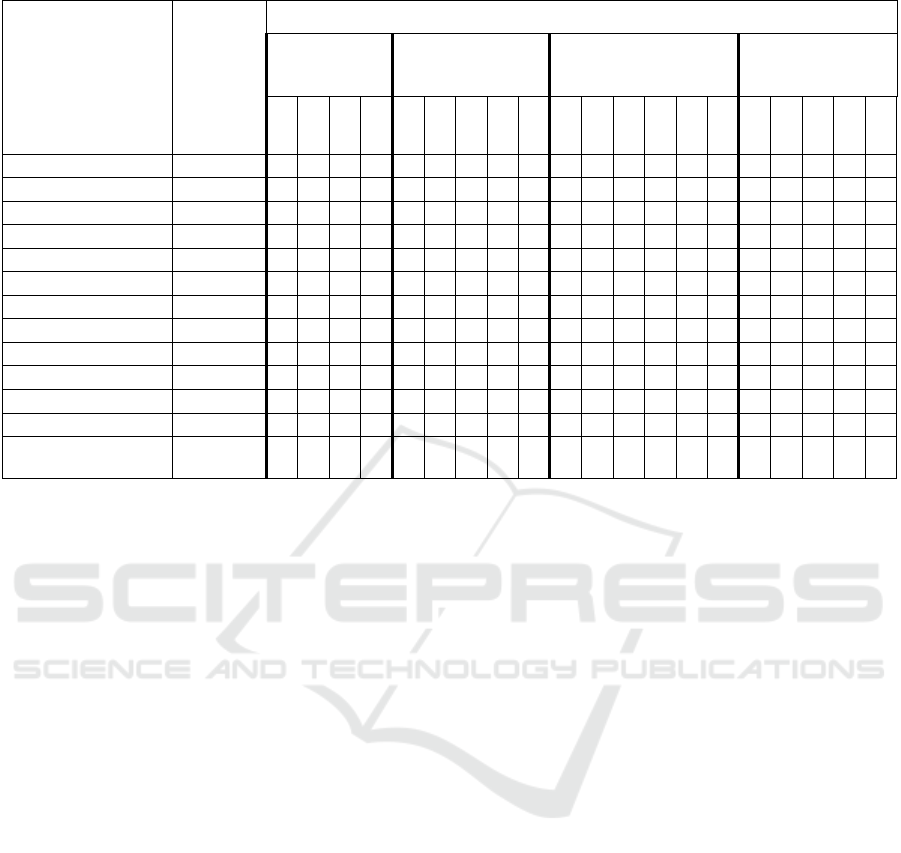
Table 5: Uganda’s readiness to adopt existing global eHealth CI/T standards.
Global eHealth CI/T
Standards
Status in
Uganda’s
eHealth
Environm
ent
What should the eHealth CI/T Standards be like in Uganda?
Use belief
Characteristic of
adopter
organisation
Characteristics of the
standard
Deployment
environment
Opt
Inn
Dis
Insec
Mgt
Proc
Size
XP
Fin
Ava
Reg
Pat
Plex
Trial
Ob
Ext
Rel
Inst
Pet
sup
ISO 11073 U, NA
──
─
─
IEEE1073.x-MDDL U, NA
──
─
─
ISO 12052:2006 U, NA
──
─
─
HL7 27931:2009 NU, NA
──
─
─
ISO 11073-91064 NA
──
─
─
ENV 13606: Part2 NA
──
─
─
CR NU, NA
──
─
─
IEEE 1073.3.x NU, NA
──
─
─
PISO 27799:2016 NU, NA
──
─
─
ISO/DTS 14441 U, NA
──
─
─
CR 14301:2002 NU, NA
──
─
─
CR 14302:2002 NU, NA
──
─
─
ISO 17090
U, A Part
1, 2 & 3
─
Key: Opt=optimism; Inn=Innovativeness; Dis=Discomfort; Insec=Insecurity; Mgt=Management support; Proc=Decision
process; Size=Organisation size; XP=Use experience; Fin=Financial resource; Ava=Availability; Reg=Regulation;
Pat=Compatibility; Plex=Complexity; Trial=Trialability; Ob=Observability; Ext=Network extensity; Rel=Related
technology; Inst=Install base /scope; Pet=Competitive use; Sup=External support; A=adopted; NA=Not formally adopted;
U=In use; NU=Not in use; =satisfies; =does not satisfy; and ─ =lack of sufficient information.
4 DISCUSSION
Standards are ever-evolving in response to
technological changes and health care needs.
Therefore, Uganda’s health system, as the adopters
and implementers of ehealth standards, should
recognize and adapt to changes. In this study, we
needed to assess the readiness of Uganda’s health
system to adopt standards for ehealth by examining
the adopter organisation (the Uganda health system),
the adopter environment and features of the standard
for ehealth CI/T. We recognise that the lack of
adoption can be attributed to a lack of metrics, and or
systematic procedure for adoption of standards for
ehealth.
Uganda’s health system is challenged by diverse
network and communications systems
implementations (Kiberu et al., 2017; Uganda
Ministry of Health, 2016). As shown in Table 4, the
health system is varied with a number of networked
departments and services, data transmission rates,
intermittent Internet, limited bandwidth, and different
computer-use security levels, among others (Huang et
al., 2017; Kiberu et al., 2017; Uganda Ministry of
Health, 2016). These variations cause unnecessary
delays in data sharing; data loss due to transmission
errors, dropped data packets, and in worst cases a
denial of service; which in the case of emergency lead
to delayed service and eventual loss of life. In
addition, it is clear that Uganda’s healthcare few CI/T
resources (Uganda Ministry of Health, 2016), the
human resources lack requisite skills and technical
support (Uganda Ministry of Health, 2016), lack of
experience in implementation and monitoring
conformance to standards that support the various
dimensions of ehealth CI/T, etc. Such challenges
drive the need for standardised high-capacity
communication systems to handle the high-volume of
healthcare data generated (Song et al., 2014). Thus,
effort must be made to bridge these gaps in the
standardisation of ehealth in LMICs.
The challenges are complicated by the lack of a
structured procedure/process at the health system
level to support the standards adoption and
implementation (Ministry of Health, Republic of
Uganda, 2015). Both the public and private healthcare
facilities have neither reached a level of coordinated
nor interoperable ehealth systems (Hindemark, 2013;
Kiberu et al., 2017). Although NITA-U oversees the
Towards Adoption of Standards for Communication Infrastructure/Technologies in Healthcare Systems in LMICs: Theories, Practice and
Evaluation
741

standardisation of the communication and the
external support for standards implementation in
Uganda (NITA-U, n.d.), they have not adopted,
developed and or harmonised the standards to suit
ehealth communication devices and health system
networks, particularly the unique nature of health data
transmission required for health system
communication in a resource-constrained
environment (Uganda Ministry of Health, 2016). In
fact, the results in Table 5 show Uganda has adopted
only one set of standards i.e., standards for the public
key infrastructure. This cannot work in isolation of
other security or CI/T standards. Other global
standards for ehealth CI/T (in-use or not-in-use) have
not been formally adopted. the existing UCC
communication standards for data transmission do
not explicitly stipulate the minimum specifications
for timely, error-free and secure data sharing
requirements suitable for healthcare (Song et al.,
2014). This means Uganda does not have suitable
standards to support ehealth data communication
requirements for their usually resource-constrained
environments.
The Assessment of standards that have been
developed or adopted by NITA-U as of June 2017
regards ehealth communication infrastructure show,
first, gaps in the statement of minimum requirements
that meet big data communication requirements for a
timely, error-free and secure exchange of health
data/information. Whereas health informatics should
facilitate the coherent and consistent interchange and
use of health-related data, information and
knowledge, NITA-U only adopted ISO 17090 Part 1,
Part 2 and Part 3 of the public key infrastructure for
digital certificates. Second, exposed component areas
of the ehealth communication infrastructure without
standards / minimum specifications to guide
implementation and compliance monitoring.
Examples include network capacity, quality of
service parameters, communication equipment, etc
suitable for healthcare data sharing; and third, show a
lack of consistency in the structure/presentation of
standards. This shows inconsistency in procedure and
manner in which the standards are developed or
adapted. The December 3
rd
– 4
th
(2012) WHO forum
on health data standardisation and interoperability
discussed perspectives on the health data standards
implementation (WHO, 2012). They relate to the five
antecedents of organisational readiness to adopt
information systems identified by (Aziz, 2012),
which include desired change, leadership support,
organisational context, attributes of change target and
IT support and can be mapped to the three dimensions
of the TOE.
Furthermore, the lag between published standards
and their implementation means that future adoption
and implementation should be a continuous and
cyclic process. Assessment of the health system level
of preparedness to adopt ehealth standards can guide
their decisions to adopt and use standards. Moreover,
ehealth standards adoption can be motivated by the
likelihood to realise the lasting benefits of such
adoption. The benefit of the adoption is a measure of
the success of adoption and in future studies, we will
explore the potential ehealth standards adoption
success for resource-constrained settings.
5 CONCLUSIONS
This study argued that existing global standards
(developers are commonly from high-resourced
environments) may not apply as is to resource-
constrained settings common in LMICs. Thus, need
to be contextualised for applicability in resource-
constrained work environments. However, there is
lack of suitable metrics to assess readiness to adopt
and or adapt the global standards. Therefore, the
study reviewed ehealth literature to establish
determinants of ehealth CI/T and security and metrics
of ehealth standards adoption. The identified metrics
(16 adoption readiness metrics) for assessing
readiness to adopt standards for ehealth CI/T were
used to assess the readiness of Uganda’s health
system to adopt 13 global standards related to ehealth
communication infrastructure and security measures
to support HIE. Based on the situation analysis of
Uganda’s health system as an example of LMICs, it
is a promising mechanism to determine the readiness
to adopt standards for ehealth CI/T for LMICs.
Although the identified metrics for assessing
readiness to adopt standards for ehealth CI/T seem
adequate in guiding the health system’s adoption
decisions, they may not in the current form support
the adoption and adaption processes nor determine
the “structure” of standards suitable for LMICs. In
addition, the review might have been limited by
incomplete retrieval of research on adoption or
diffusion of standards (not indexed by PubMed
Central and Google Scholar) or any reporting bias by
literature considered in this review. Future research
will focus (1) on developing and validating the
readiness assessment framework for ehealth CI/T
standards adoption readiness and exploring the
potential adoption success with an aim to
contextualise it for Uganda’s resource-constrained
health system. (2) Determining the criteria for
selecting standards for ehealth CI/T that resourced-
HEALTHINF 2020 - 13th International Conference on Health Informatics
742

constrained settings like Uganda’s healthcare system
may use to select suitable global standards to support
their HIE. (3) Develop a structured process to guide
the adoption and adaption of ehealth CI/T
standardisation efforts within Uganda’s health
system.
ACKNOWLEDGMENTS
This study was funded in part by the Swedish
International Development Cooperation Agency
(Sida) and Makerere University under Sida
contribution No: 51180060. Also, part of the funds
was provided by Makerere University Research and
Innovations Fund through the project, “Exploring the
Feasibility for Strengthening Uganda’s Health
System through Standardizing Digital Health”.
REFERENCES
Adebesin, F., Kotze, P., Foster, R., Van Greunen, D., 2013.
A Review of Interoperability Standards in E-health and
Imperatives for their Adoption in Africa. South African
Computer Journal 50, 55–72.
Al-Safadi, L., 2016. The effects of real-time interactive
multimedia teleradiology system. BioMed research
international 2016.
Alunyu, A.E., Nabukenya, J., 2018. A Conceptual Model
for Adaptation of eHealth Standards by Low and
Middle-Income Countries. J Health Inform Afr 5, 10–
16. https://doi.org/10.12856/JHIA-2018-v5-i2-199
Anderson, R.E., Anderson, R.J., Borriello, G., Kolko, B.,
2012. Designing technology for resource-constrained
environments: Three approaches to a multidisciplinary
capstone sequence, in: Frontiers in Education
Conference (FIE), 2012. IEEE, pp. 1–6.
Aziz, K., 2012. Measuring organizational readiness in
information systems adoption, in: The Eighteenth
Americas Conference on Information Systems.
Presented at the AMCIS, Seattle, Washington.
Baker, D.B., Perlin, J.B., Halamka, J., 2015. Evaluating and
classifying the readiness of technology specifications
for national standardization. J Am Med Inform Assoc
22, 738–743. https://doi.org/10.1136/amiajnl-2014-
002802
Baker, J., 2011. The Technology–Organization–
Environment Framework. https://doi.org/10.1007/978-
1-4419-6108-2_12
Brunsson, N., Rasche, A., Seidl, D., 2012. The dynamics of
standardization: Three perspectives on standards in
organization studies. Organization studies 33, 613–632.
Cresswell, K., Sheikh, A., 2013. Organizational issues in
the implementation and adoption of health information
technology innovations: an interpretative review.
International journal of medical informatics 82, e73–
e86.
Eduqas, 2015. The importance of protocols and standards
[WWW Document]. URL http://the
teacher.info/index.php/fundamentals-of-cs/3-data-
transmission/topics/2652-the-importance-of-protocols-
and-standards (accessed 9.12.18).
European Telecommunications Standards Institute, 2013. A
Guide to Writing World Class Standards.
Fontaine, P., Ross, S.E., Zink, T., Schilling, L.M., 2010.
Systematic review of health information exchange in
primary care practices. The Journal of the American
Board of Family Medicine 23, 655–670.
Gillwald, A., 2008. Communication Infrastructure. Wiley
Publishing.
https://doi.org/10.1111/b.9781405131995.2008.x
Hindemark, F., 2013. E-Health at Outpatient Clinics in
Uganda.
HL7 International, 2017. Health Level Seven International
(HL7).
Hovav, A., Patnayakuni, R., Schuff, D., 2004. A model of
Internet standards adoption: the case of IPv6.
Information Systems Journal 14, 265–294.
Huang, F., Blaschke, S., Lucas, H., 2017. Beyond pilotitis:
taking digital health interventions to the national level
in China and Uganda. Globalization and Health 13, 49.
https://doi.org/10.1186/s12992-017-0275-z
IEEE Website, n.d. IEEE Standards Glossary [WWW
Document]. URL
https://www.ieee.org/standards/index.html (accessed
3.5.18).
ISO, 2017. Health informatics Standards.
ITU, UIT, 2017. World Telecommunication Development
Conference (WTDC-17). Buenos Aires, Argentina.
ITU-T, 2012. E-health Standards and Interoperability.
ITU-T, 2009. Bridging the Standardisation Gap: Measuring
and Reducing the Standards Gap.
Ketikidis, P., Dimitrovski, T., Lazuras, L., Bath, P.A., 2012.
Acceptance of health information technology in health
professionals: An application of the revised technology
acceptance model. Health informatics journal 18, 124–
134.
Kiberu, V.M., Mars, M., Scott, R.E., 2017. Barriers and
opportunities to implementation of sustainable e-Health
programmes in Uganda: A literature review. African
Journal of Primary Health Care and Family Medicine 9,
1–10.
Kuziemsky, C.E., Peyton, L., 2016. A framework for
understanding process interoperability and health
information technology. Health Policy and Technology
5, 196–203.
Liljander, V., Gillberg, F., Gummerus, J., Van Riel, A.,
2006. Technology readiness and the evaluation and
adoption of self-service technologies. Journal of
Retailing and Consumer Services 13, 177–191.
https://doi.org/10.1016/j.jretconser.2005.08.004
Mac Callum, K., Jeffrey, L., 2014. Comparing the role of
ICT literacy and anxiety in the adoption of mobile
learning. Computers in Human Behavior 39, 8–19.
Towards Adoption of Standards for Communication Infrastructure/Technologies in Healthcare Systems in LMICs: Theories, Practice and
Evaluation
743

Maunder, K., Walton, K., Williams, P., Ferguson, M.,
Beck, E., 2018. eHealth readiness of dietitians. Journal
of Human Nutrition & Dietetics 31, 573–583.
https://doi.org/10.1111/jhn.12542
McCann, D., 2012. A Ugandan mHealth Moratorium Is a
Good Thing - ICTworks [WWW Document]. URL
https://www.ictworks.org/ugandan-mhealth-
moratorium-good-thing/ (accessed 8.27.18).
Ministry of Health, Republic of Uganda, 2015. National
eHealth Infrastructure Assessment Report: Uganda’s
ICT Infrastructure status at Health Service deliver sites.
Neuhaus, C., Polze, A., Chowdhuryy, M.M., 2011. Survey
on healthcare IT systems: standards, regulations and
security. Universitätsverlag Potsdam.
NITA-U, n.d. NITA | National Information Technology
Authority [WWW Document]. URL
https://www.nita.go.ug/ (accessed 9.12.18).
Oliveira, T., Martins, M.F., 2011. Literature review of
information technology adoption models at firm level.
Electronic Journal of Information Systems Evaluation
14, 110.
Parasuraman, A., 2000. Technology Readiness Index (TRI)
a multiple-item scale to measure readiness to embrace
new technologies. Journal of service research 2, 307–
320.
Rahurkar, S., Dixon, B.E., Menachemi, N., 2016. Drivers
and Barriers to Adoption: Towards the Last Mile, in:
Dixon, B.E. (Ed.), Health Information Exchange. pp.
41–57.
Rajiv, K., McLean, E., 1998. Diffusion and Infusion: Two
Dimensions of “Success of Adoption” of IS Innovations
Rajiv Kish, in: Americas Conference on Information
Systems. p. 731.
Ramdani, B., Chevers, D., A. Williams, D., 2013. SMEs’
adoption of enterprise applications: A technology-
organisation-environment model. Journal of Small
Business and Enterprise Development 20, 735–753.
Reid, P.P., Compton, W.D., Grossman, J.H., Fanjiang, G.,
2005. Information and communications systems: The
backbone of the health care delivery system, in:
Building a Better Delivery System: A New
Engineering/Health Care Partnership. National
Academies Press (US), pp. 63 – 82.
Rezai-Rad, M., Vaezi, R., Nattagh, F., 2012. E-health
readiness assessment framework in iran. Iranian journal
of public health 41, 43.
Rogers, E.M., 1983. Diffusion of innovations. The Free
Press.
Son, M., Han, K., 2011. Beyond the technology adoption:
Technology readiness effects on post-adoption
behavior. Journal of Business Research 64, 1178–1182.
Song, J., Ding, W., Yang, F., Yang, H., Wang, J., Wang, X.,
Zhang, X., 2014. Indoor hospital communication
systems: An integrated solution based on power line
and visible light communication, in: 2014 IEEE Faible
Tension Faible Consommation. Presented at the 2014
IEEE Faible Tension Faible Consommation, pp. 1–6.
https://doi.org/10.1109/FTFC.2014.6828620
Tamburis, O., Mangia, M., Contenti, M., Mercurio, G.,
Mori, A.R., 2012. The LITIS conceptual framework:
measuring eHealth readiness and adoption dynamics
across the Healthcare Organizations. Health and
Technology 2, 97–112.
Uganda Ministry of Health, 2016. Uganda National eHealth
Strategy and Policies.
Vincent, C.J., Niezen, G., O’Kane, A.A., Katarzyna, S.,
2015. Can Standards and Regulations Keep Up With
Health Technology? JMIR Mhealth Uhealth 3.
https://doi.org/10.2196/mhealth.3918
WHO, 2013. eHealth standardization and interoperability.
Executive Board, 132.
WHO, 2012. WHO Forum on Health Data Standardization
and Interoperability. Geneva, Switzerland.
Widya, I., Van Halteren, A., Jones, V., Bults, R.,
Konstantas, D., Vierhout, P., Peuscher, J., 2003.
Telematic requirements for a mobile and wireless
healthcare system derived from enterprise models, in:
Proceedings of the 7th International Conference on
Telecommunications, 2003. Con℡ 2003. IEEE, pp.
527–534.
Yiming, W., Davood, B., Lars, N., 2016. Modeling of
Communication Infrastructure Compatible to Nordic 32
Power System, in: IEEE Power and Energy Scociety
General Meeting (PESGM). pp. 1–5.
https://doi.org/10.1109/PESGM.2016.7741521
HEALTHINF 2020 - 13th International Conference on Health Informatics
744
