
Prototypical Implementation of a Decision-supporting System for
Operative Breast Cancer Therapy
Michael Dück
*
and Eberhard Beck
*
Department of Computer Science and Media, University of Applied Science Brandenburg,
Magdeburger Street 50, Brandenburg, Germany
Keywords: Decision Support, Breast Cancer, e-Health, BPMN.
Abstract: Based on the current edition of the German guideline on Screening, Diagnosis, Treatment and Follow-up of
breast cancer, we created a patient journey modelled in BPMN (Business Process Model and Notation V2)
serving as template for the development of a patient centered decision support system. This approach resulted
in two prototypical devices represented by a web-based information platform and a mobile application,
intended to support the decision support at the point of care. These early prototypes were discussed with a
clinical expert and the members of a regional breast cancer self-help group. The information gained by this
approach will be integrated in the further user centered design of the devices.
1 INTRODUCTION
The advent of computer assisted clinical decision
support goes back to the early 1960s (Shortliffe,
2018). Since then scientists and clinicians have
undertaken numerous efforts to create various
systems in order to improve the quality of clinical
decisions, enhance their transparency and increase the
number of guideline conform decisions, resulting not
only in patient centered decisions but also enabling
patients to engage in the process of shared decision
making (Middleton 2016, Beeler, 2014). Despite
these efforts, decision support systems are failing to
be introduced into daily routine for a number of
reasons. Among other reasons, a suspected negative
influence on the physician-patient relationship, the
extra time spent to utilize the system or that the
system could not be integrated into the routine
workflow, were named (Kilsdonk, 2017). On the
other hand, factors in favor of using computerized
decision support systems are seen in systems that e.g.
fit with routine care and provide recommendations at
the point of care (Kilsdonk, 2017). In order to address
at least some of these requirements we analyzed the
current guideline on Screening, Diagnosis, Treatment
and Follow-up of breast cancer of the German Cancer
Society (Wöckel, 2018). Based on our results we
*
https://informatik.th-brandenburg.de/
developed an early prototype of a clinical decision
support system, which should not only serve
clinicians but also support patients and their relatives.
2 METHODS
On the basis of the German S3 guideline on
Screening, Diagnosis, Treatment and Follow-up of
Breast Cancer, a patient journey as a process model
for breast cancer was extracted and modelled in
BPMN (Business Process and Model Version 2.0) as
described previously (Andrzejewski, 2015,
Andrzejewski, 2017). This resulted in the definition
of several important decision nodes, which were then
examined for their specific, decision relevant
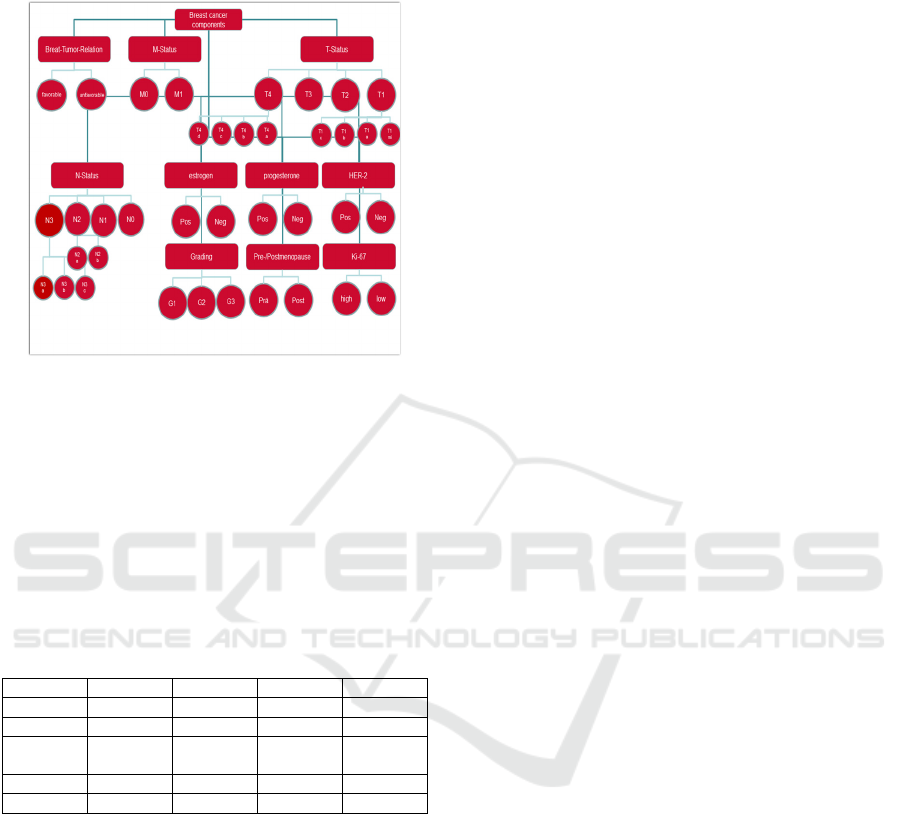
parameters. These factors consisted of the Tumor
seize, axillary lymph nodes involved (N-status),
distant metastasis present or absent (M-status), the
tumor grading, the (clinical) breast to tumor relation,
estrogen and progesterone receptor status, the HER-2
status, the Ki-67 status and finally whether the patient
was pre- or postmenopausal (Fig. 1). In contrast to our
previous work, Ki-67 was newly introduced as
relevant decision factor in the 2018 edition of the
guideline, which forced us to redesign our process
models. The aforementioned factors were then used
Dück, M. and Beck, E.
Prototypical Implementation of a Decision-supporting System for Operative Breast Cancer Therapy.
DOI: 10.5220/0009164506830686
In Proceedings of the 13th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2020) - Volume 5: HEALTHINF, pages 683-686
ISBN: 978-989-758-398-8; ISSN: 2184-4305
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
683
to create a decision matrix, which however resulted in
more than 140,000 individual combinations.
Figure 1: Factors in the treatment of breast cancer.
We thus restricted our preliminary efforts to re-
generate our computer-based decision support system
to the factors necessary to make a transparent
decision concerning surgical treatment only. Tumor
size and the clinical breast to tumor-relation were
identified as the two essential factors concerning
decisions on surgical treatment. In the following short
matrix, the possible outcomes for four of the eight
different possible combinations are shown.
Table 1: Decision matrix for the surgical treatment.
T-Status T1 T2 T3 T4
BTR G G G G
Neo - - Op
t
+
Treat BCT BCT BCT
BCT /
(Mas
t
)
Radio + + + +
/
Opt
Adju + + + +
The abbreviations in the table in order of appearance are: T-
Status: the size of the tumour;
BTR: Brest-Tumor-Relation, the size of the breast in relation to
the tumour;
G: good or rather favourable;
Neo: neoadjuvant system therapy;
Opt: optional;
Treat: surgical treatment;
BCT: breast conserving surgical
therapy;
Mast: mastectomy;
Radio: radio therapy;
Adju: adjuvant system therapy.
Based on these combinations and the resulting
actions to be recommended, we created a prototype of
a rule-based decision support system. A decision
support system is defined by Keen und Scott-Morton
(Keen, 1978) as:
"Decision Support Systems (DSS) represent a
point of view on the role of the computer in the
management decision-making process. Decision
support implies the use of computers to:
• Assist (managers) in their decision processes in
semi structured tasks
• Support, rather than replace, (managerial)
judgement
• Improve the effectiveness of decision-making
rather than its efficiency".
Our decision support system is aimed to assist
patients in a complex process of medical decisions by
delivering recommendations with very little input.
This rule-based system was primarily implemented as
an app, which advocates the respective operative
intervention, once the relevant factors are entered.
The app was built with the MIT App Inventor as a fast
prototype and to use with the treating doctor for a
shared decision making in a consultation meeting.
Also, a website with the same functions, built in
JavaScript and HTML was designed. After the
development of these prototypes, they were presented
to a health care professional and a former breast
cancer patient for a preliminary evaluation of the
system. As a second step, we presented the
application and the website at the annual meeting of
the regional cancer self-help group
Berlin/Brandenburg.
3 RESULTS
To generate the best decision support for breast
cancer patients, the precise diagnosis and all relevant
clinical and personal factors which may affect the
choice of treatment should be known. A newly
diagnosed patient, who in our view is most likely in
need of a decision support system, will not
necessarily be aware of all these data. By focusing on
the factors mentioned above which were derived from
the S3 guideline we created the prototype of an
evidence-based decision support platform. Our aim
was to test if it was possible to translate the medical
guideline into a digital rule-based system, which is
able to create relevant suggestions based on the
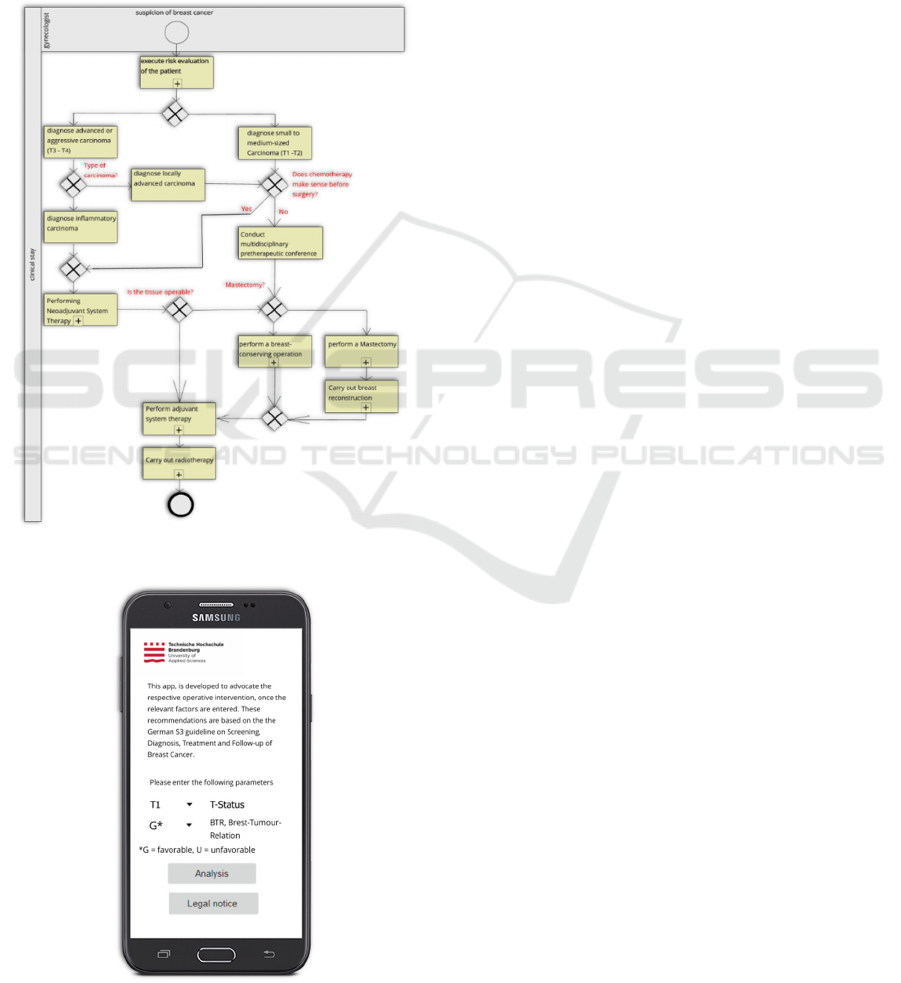
information given by a patient. In Fig. 2 the patient
journey, starting with the decision conflict between a
mastectomy or a breast-conserving operation as
initial surgical step, is visualized. In the first instance
the tumor size is used to define the disease as early
stage cancer or locally advanced tumor. Combined
with the factor “breast to tumor relation”, this results
either in a strait forward decision concerning the type
HEALTHINF 2020 - 13th International Conference on Health Informatics
684
of surgical intervention or raises the question of a
primary (neo-adjuvant) Chemotherapy. The latter
could be applied in cases of locally advanced tumors
or in early breast cancer with an unfavorable breast to
tumor relation.
These respective decisions are based on the
decision matrix shown in Tab. 1. The further process
model then describes the consecutive steps of
adjuvant chemo and/or radiation therapy once the
operative intervention was carried out.
Figure 2: Process of the breast cancer treatment.
Figure 3: Screenshot of the app.
Most of the modelled tasks like the “perform
breast-conserving therapy” are further detailed in
various sub-processes, which however for the sake of
clarity are not shown.
Based on these models and the previously
mentioned decision matrix, two prototypes of a
decision support system were developed. Figure 3
shows the app. The app was primarily designed in
order to serve as a mobile device available for the
evidence-based decision support at the point of care.
4 EVALUATION
In order to improve these first iterations of the
applications, two interviews were conducted with a
medical expert and a person affected by breast cancer.
The recommendations extracted from these
interviews were applied to further improve the
prototypes before we presented them on the annual
meeting of the regional cancer self-help group
Berlin/Brandenburg. While the website was assessed
as appropriate for making an informed decision, the
app however raised major concerns. The approach to
have a fast and mobile decision support system at
hand, was viewed as a useful development. However,
it was stated, that without a consultation with the
treatment overseeing physician or another health care
professional, the information given by the system
could lead to confusion and insecurities, which would
counteract to the expected result.
5 CONCLUSIONS
Based on the various tasks and decision nodes
extracted from the S3 guideline on Diagnosis,
Treatment and Aftercare of Breast Cancer we were
able to map the complete clinical process, starting
with the first suspicious findings and ending with the
completion of adjuvant treatment utilizing BPMN.
The complexity of the information provided in the
guideline, however, constrained us in the first
instance to restrict our efforts in developing a
computer-based decision support system to the tasks
related to the decisions concerning the operative
intervention. Utilizing the TNM classification and the
breast-to-tumor relation, we created a decision
matrix. Based on these rather preliminary results, two
applications were developed in parallel, a website that
serves as a breast cancer information platform and an
app that represents only the decision matrix. The
website contains not only information about breast
Prototypical Implementation of a Decision-supporting System for Operative Breast Cancer Therapy
685

cancer, but also user-controlled information paths that
allow patients to navigate freely according to their
individual information needs and thus receiving
specific, patient centered information. These
pathways lead the users to the decision matrix in
which they can enter their individual clinical data
resulting in a suitable recommendation.
In summary, we developed two prototypical
systems, which were designed to support the
decision-making process in breast cancer. These
prototypes, however, will have to be tested by
independent experts on the basis of a larger number
of realistic case reports. By applying the best
available evidence for the diagnosis and treatment of
breast cancer, represented by the S3 guideline we are
convinced, that our systems could not only help to
increase the number of guideline conform decisions
in the near future, but could also help to improve the
patients knowledge and thus assist in shared decision
making.
REFERENCES
Shortliffe EH, Sepúlveda MJ. Clinical decision support in
the era of artificial intelligence. JAMA. (2018) Dec
4;320(21):2199-2200. doi: 10.1001/jama.2018.17163.
Middleton B, Sittzig DF, Wright A. Clinical decision
support: a 25 year retrospective and a 25 year vision.
Yearb Med Inform (2016) Suppl. S103 -16,
http://dx.doi.org/10.15265/IYS-2016-s034.
Beeler PE, Bates DW, Hug BL. Clinical decision support
systems. Swiss Med Wkly (2014) 144:w14073,
doi:10.4414/smw.2014.14073.
Kilsdonk E, Peute LWP, Jaspers WM. Factors influencing
implementation success of guideline-based clinical
decision support systems: A systematic review and gaps
analysis. Int J Med Inform. (2017) Feb;98:56-64. doi:
10.1016/j.ijmedinf.2016.12.001. Epub 2016 Dec 5.
Wöckel A, Albert S, Janni W, Scharl ., Kreienberg R,
Stüber T. The screening, diagnosis, treatment and
follow-up of breast cancer. Dtsch Arztebl. Int. (2018)
115 (18) 316 – 323. doi: 10.3238/arztebl.2018.0316.
Andrzejewski D, Tetzlaff L, Beck E, Haeusler N. The
transparent representation of medical decision
structures based on the example of breast cancer
treatment, Conference paper. International Conference
on Health Informatics (BIOSTEC), 2015. Lissabon.
Andrzejewski D, Breitschwerdt R, Fellmann M, Beck E,
Supporting breast cancer decisions using formalized
guidelines and experts decision patterns: initial
prototype and evaluation. HealthInfSciSyst, (2017)
5(1):12. doi: 10.1007/s13755-017-0035-8.
Keen P, Scott Morton M. Decision Support Systems: An
Organizational Perspective. Addison-Wesley Inc.
(1978) https://link.springer.com/chapter/10.1007%2
F978-3-663-09143-1_9
HEALTHINF 2020 - 13th International Conference on Health Informatics
686
