
Legislation and the Negative Impact on Cybersecurity in Healthcare
Jesse Daniels and Sajal Bhatia
∗
School of Computer Science and Engineering, Sacred Heart University, Fairfield, CT, U.S.A.
Keywords:
Healthcare, Regulation, Security, Privacy, HIPAA, Stark Law, HITECH, Legislation, Medical Devices, FDA.
Abstract:
Healthcare is a rapidly growing industry that is continuously expanding with technological advances. Similar
to many other critical industries, healthcare faces an onslaught of daily cybersecurity challenges, however is
largely at a disadvantage due to outdated and antiquated legislation. As of 2019, no legislation or regulatory
body in healthcare adequately cover the needs of cybersecurity. However, regulations have forced healthcare
to deploy technology at an expansive rate as well as having them deploy FDA, a regulatory body, approved
medical devices from the assembly line that are inherently insecure. By looking at reported incidents, the
authors will examine modifications to legislation in healthcare and the impact on cybersecurity-related events
facing the organizational vertical. Legislation such as the Ethics in Patient Referrals Act of 1989 adversely
impacts healthcare as cybersecurity is not considered a “service,” and as such, cannot be shared between two
healthcare organizations. By bringing light to the inadequacies of cybersecurity in legislation and regulation of
the United States healthcare system, the paper aim to bring cybersecurity to the forefront of future legislation
and regulation.
1 INTRODUCTION
On Friday May 12
th
, 2017, using leaked National Se-
curity Agency exploits, the National Health Service
of the United Kingdom saw a ransomware attack that
cost the organization £20 million ($25 million USD)
in one week. The incident cost a total of £92 million
($115 million USD), while over 19,000 patient ap-
pointments were canceled (Field, 2018). The authors
wanted to examine the correlation between the in-
crease in cybersecurity events seen in healthcare and
the regulations this industry faces. According to Bea-
zley Breach Response, 41 percent of all cyber-related
incidents tracked are from healthcare organizations,
while the financial sector is a distant second at 20 per-
cent (Beazley, 2019).
Healthcare is one of the most vital functions of so-
ciety across the developed and underdeveloped world.
According to CDC, 883.7 million patients visited
Ambulatory Care Use and Physician office visits dur-
ing 2018 (for Disease Control and Prevention, 2018)
who could possibly be data breach victim. We hope
that our loved ones can receive the care they need
when in these facilities, but as of late the number
of cybersecurity events have risen across the globe.
We have seen ransomware close healthcare facilities
∗
Corresponding author.
and cause patients to seek treatment in other health-
care facilities. In 2017 the National Health Services
of the United Kingdom was forced to turn away and
reschedule 19,000 patients. While National Health
Service representatives state no patients died during
this incident, an attack of this magnitude has the mas-
sive potential to disrupt patient care, and cause harm
to life (Field, 2018).
A multitude of cybersecurity threats face health-
care facilities all across the world. The most com-
mon forms of compromise are: insider threats, busi-
ness email compromise, phishing, DDoS attacks, data
breaches, ransomware, mobile devices, rise of the
cloud, online file-sharing, encryption blind spots.
These threats are not unique to healthcare; how-
ever, they produce an array of new challenges in the
healthcare arena. Unlike other sectors , there is an ad-
ditional vulnerability in healthcare. Legislation and
regulation have caused healthcare to have a poor cy-
bersecurity posture. Hospitals have been forced to de-
ploy technology at a rapid pace in an effort to not
lose Medicare and Medicaid reimbursement. After
the rapid implementation of Electronic Health Record
systems, multiple organizations reported that during
unexpected downtime of Electronic Health Record
systems “an unexpected theme that emerged during
the interviews was how essential tenured staff was to
the organizational response and recovery from the at-
Daniels, J. and Bhatia, S.
Legislation and the Negative Impact on Cybersecurity in Healthcare.
DOI: 10.5220/0009157906910697
In Proceedings of the 6th International Conference on Information Systems Security and Privacy (ICISSP 2020), pages 691-697
ISBN: 978-989-758-399-5; ISSN: 2184-4356
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All r ights reserved
691
tack. This theme was mentioned by at least one stake-
holder from all three facilities. The participants ex-
plained that staff who had been in healthcare longer
were able to shift back to pen and paper records much
easier than newer staff. This group of individuals had
experience with paper charting during their careers.
In contrast, the participants mentioned the hard time
that younger staff had with switching back to paper
charts” (Branch, 2018).
Security rules written into legislation are sixteen
years old, and medical devices are the “wild west” of
security flaws. This begs the question of what have
lawmakers and policymakers done in the wake of the
significant rise in attacks on the healthcare industry?
Well, the answer is quite simple- nothing.
The main contributions of this position paper are
to unpack the negative consequences that legislation
and regulation produce in the cybersecurity of health-
care. The authors feel that legislation such as HIPAA,
HITECH, and the Stark Law have inherently created
a state of disrepair in healthcare cybersecurity. By
bringing to light these legal inadequacies, the authors
would like to see future legislation consider potential
cybersecurity ramifications moving forward.
Rest of the paper is organized as follows: Sec-
tion 2 summarized the recent security breaches and
events in healthcare. Section 3 gives an overview of
the Stark Law which is intended to prevent physi-
cian self-referral; however, this legislation prevents
the donation of cybersecurity goods and services to
other healthcare facilities. Section 4 presents the
HIPAA healthcare privacy and accountability legis-
lation, while unpacking the lack of updates to the
Security Rule. Section 5 delves into the HITECH
legislation which is directly attached to the adoption
rate of technology in the healthcare sector. Section 6
makes reference to the U.S. Food and Drug Admin-
istrations regulations on medical devices, causing in-
herent vulnerabilities in the ever increasing intercon-
nected healthcare environment. Section 7 summa-
rizes the paper and gives directions for future research
work in this area.
2 RECENT CYBERSECURITY
EVENTS IN HEALTHCARE
Healthcare has been under siege by cyber adversaries
for years. According to the Office of Civil Rights
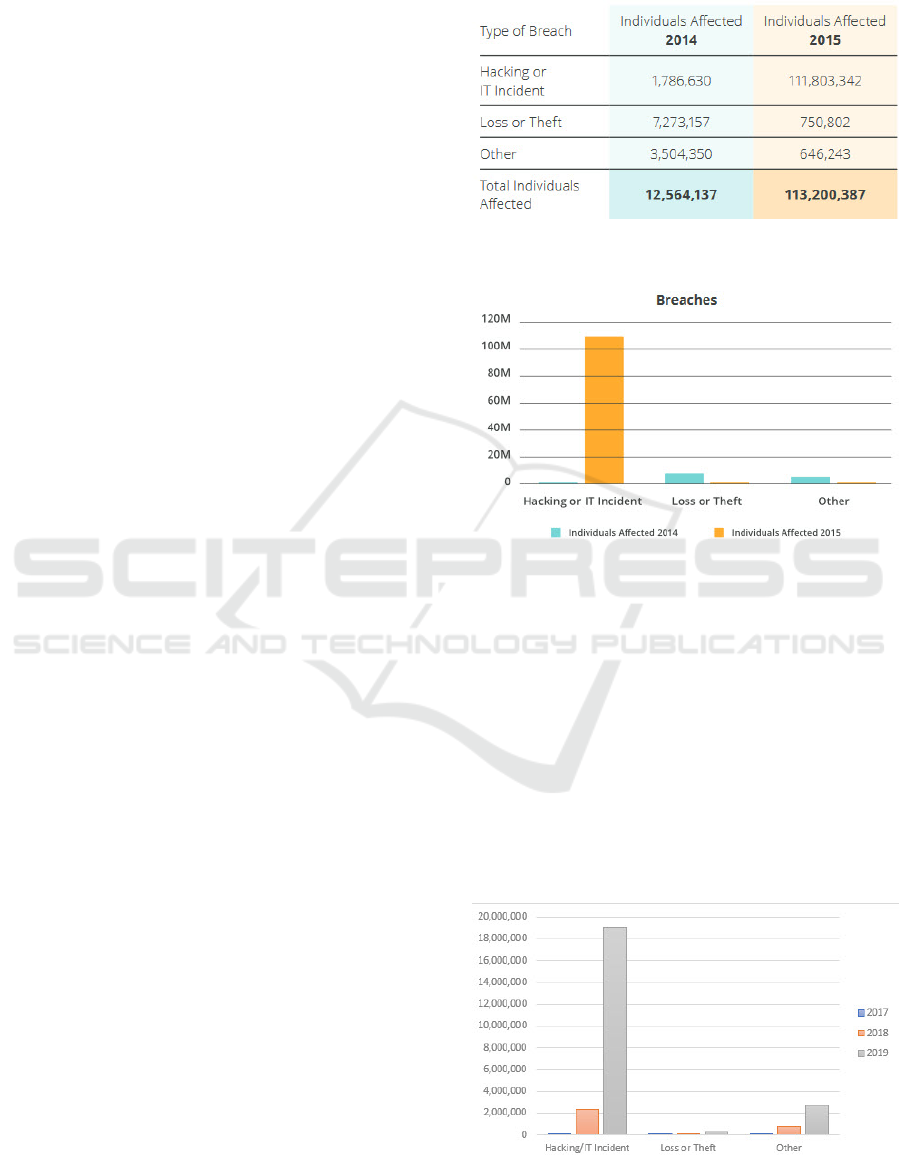
(OCR), in 2014, there were 31 hacking incidents
in healthcare affecting 1,786,630 individuals (Bit-
glass, 2016). By 2015 56 hacking incidents affected
111,803,342 individuals, as shown in Figure 1. Figure
2 shows individuals affected by breach incident type
for 2014 and 2015 (Bitglass, 2016).
Figure 1: Bitglass Healthcare Breach Report 2016 (Bit-
glass, 2016).
Figure 2: Bitglass Healthcare Breach Report 2016.
According to the Office of Civil Rights, which is re-
quired to post breaches affecting 500 individuals or
more, 12,385,888 individual records became compro-
mised due to hacking/IT incidents from healthcare
providers between November of 2017 and November
of 2019. The largest of these breaches submitted to
the Office of Civil Rights occurred on July 13
th
, 2019
when a staggering 10,251,784 individual records were
stolen after Laboratory Corporation of America Hold-
ings dba LabCorp was hacked (OCR, 2019). Figure 3
shows the total individual affected between 2017 and
2019 according to the OCR (OCR, 2019).
Figure 3: OCR Breaches of healthcare providers between
2017 and 2019.
ICISSP 2020 - 6th International Conference on Information Systems Security and Privacy
692
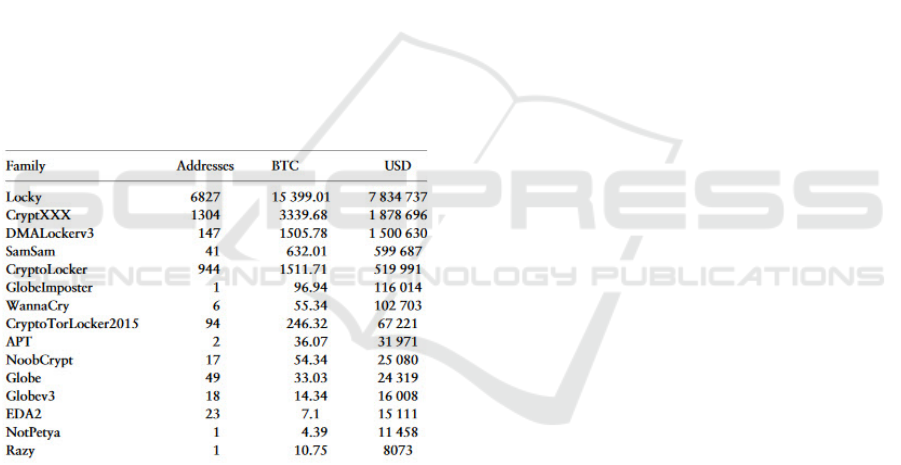
In 2016 we saw the rise of ransomware at-
tacks against healthcare facilities. On February
5
th
, 2016 Hollywood Presbyterian Medical Center
staff reported that they were unable to access elec-
tronic resources. Their network had become in-
fected with the ransomware Locky, and the malicious
actors were demanding 40 Bitcoin, worth approx-
imately $17,000 at the time of the event (Winton,
2016). A study regarding ransomware and crypto-
currencies determined “that the ransomware family
that generated the largest direct financial impact in our
data-set is Locky, which received payments totaling
$7,834737.00 USD” (Paquet-Clouston et al., 2019).
During this incident, doctors reported the inabil-
ity to access patient medical histories, share medi-
cal imaging, and access test results. Several patients
were also diverted to nearby hospitals for treatment.
Hollywood Presbyterian Medical Center paid the de-
manded ransom and reported that services were re-
stored ten days later on February 15
th
; however, the
damage to the hospital’s system and reputation in the
public eye remained (Winton, 2016). Figure 4 shows
the total payments received by the top 15 ransomware
families (Paquet-Clouston et al., 2019).
Figure 4: Received payments per ransom family (Top 15).
Just one month after the events in California, The Ot-
tawa Hospital was infected with a variant of Cryp-
tolocker in March of 2016. Fortunately, The Ottawa
Hospital had sufficient backup and restoration pro-
cesses in place to bring their systems back online
without paying the ransom fee. The Ottawa Hos-
pital stated that four systems out of 9,800 were af-
fected (Spence et al., 2017).
One year later in March of 2017, we saw the rapid
spread of WannaCry. This ransomware attack was the
most significant cyberattack against the healthcare in-
dustry. As a result, the National Health Services of the
United Kingdom had services wholly disrupted. Dur-
ing this incident, 19,000 patients were impacted as
medical services were disrupted and thousands of ap-
pointments were canceled and rescheduled. The De-
partment of Health in the United Kingdom estimated
that the total financial cost of the Wannacry event cost
£92 million ($115 Million USD) (Field, 2018).
The year of 2019 started with UCONN Health in
Connecticut reporting that 326,000 patient records be-
came breached after a cyber-attack. While conducting
its incident response investigation, the health system
had determined that an unauthorized third party had
accessed various employee email accounts. UCONN
Health manually reviewed 285,000 emails and attach-
ments to find what patients and which information
became breached. Patients were notified roughly six
months after the breach occurred in late 2018 (Davis,
2019b). The simplicity of phishing is an easy way to
bait healthcare employees to submit their valid cre-
dentials to malicious actors. In a recent study, ten
major incidents were found where phishing allowed
unauthorized access to patient records. The research
found that 74,910 individuals had their Personally
Identifiable Information (PII) breached (Wright et al.,
2016).
In summary, an ever increasing trend can be
seen in Protected Health Information(PHI) breaches
caused by “Hacking or IT Incident“. The authors be-
gin dissecting legislation in Section 3 to see the ad-
verse affects of legislation on healthcare cybersecu-
rity.
3 THE “TONY” STARK LAW
The United States Omnibus Budget Reconciliation
Act of 1990 included a bill entitled “Ethics in Patient
Referrals Act.” The law would become commonly
referred to as “Stark I” in the namesake of the pri-
mary author United States Congressman Pete Stark,
D-CA. The United States Omnibus Budget Reconcil-
iation Act of 1993 would see amendments added to
the original Stark Law, which was later coined “Stark
II” (Salcido, 2000)
The initial motivator behind the Stark Law was to
prevent physician self-referral. The primary concern
was physicians ordering unnecessary testing by refer-
ring patients to testing centers to which they had a fi-
nancial relationship. While this bill intended to keep
the cost of health services down, it inherently created
an issue before the Internet, and Electronic Medical
Record systems were in extensive use.
The Stark Law states that a healthcare facility can-
not provide services or goods to a physician prac-
tice without charging “fair market value.” Excep-
tions were made in 2006 to allow healthcare facili-
Legislation and the Negative Impact on Cybersecurity in Healthcare
693

ties to “donate” EMRs to physician practices, but no
clauses were added for cybersecurity and computer-
related technology. Under the current Stark Law, a fa-
cility upgrading to a more extensive firewall that did
not have end of life products could not donate their
old infrastructure to a facility in need. By not allow-
ing smaller practices that interconnect with more ex-
tensive facilities appropriate access to cybersecurity-
related hardware and software, the healthcare sector
is inherently less secure.
4 LET’S TALK ABOUT THE
HIPAA IN THE ROOM
The Health Insurance Portability and Accountability
Act (HIPAA) of 1996 was signed into law by for-
mer United States President Bill Clinton on August
21st, 1996. The primary intention of HIPAA was
to protect Personally Identifiable Information (PII),
and to prevent fraud and theft while allowing indi-
viduals to request a copy of their medical records.
On February 20
th
2003, the Final Rule on Security
Standards was added to HIPAA. The Security Rule
was designed to complement the Privacy Rule by ex-
plaining how Electronic Protected Health Information
(EPHI) is managed and maintained. Components of
the Security Rule include Administrative Safeguards,
Physical Safeguards, and Technical Safeguards were
components of the Security Rule (Assistance, 2003).
The Technical Safeguards implemented by the Se-
curity Rule boil down to the following:
• Systems containing PHI have protections in place
to prevent intrusion.
• Explaining the encryption requirement for elec-
tronically transmitting PHI over open networks.
• A covered entity must ensure data integrity and
prevent data manipulation.
• Entities must maintain access records providing
authentication.
Since this amendment, HIPAA was modified one last
time in 2013 with the Final Omnibus Rule Update.
This juncture in time would have been an opportune
point in time to add regulations regarding cyberse-
curity. Instead, it added the requirement to report
breaches to the Office of Civil Rights, implemented
severe penalties for violations of privacy and allowed
waving of the HIPAA Privacy Rule during a natural
disaster.
During the ten years between the two amend-
ments, several cybersecurity events have happened,
which should highlight the need to implement some
form of cybersecurity standards.
• 2003 - The Slammer worm begins to spread to
SQL servers quickly.
• 2004 - MyDoom quickly develops as one of the
fastest spreading mass-mailer worms.
• 2005 - The Gpcoder Trojan is discovered, which
encrypts data files and requires a $200 payment
for the decoder.
• 2006 - A Veterans Affairs Department employee
loses a laptop with the PII of 26.5 million active-
duty troops and veterans.
• 2007 - The FBI finds over 1 million botnet vic-
tims.
• 2008 - The United States was a victim of a cyber-
attack when an infected USB drive was left in the
parking lot of a Department of Defense facility in
the Middle East.
• 2009 - The Conficker worm rapidly spreads in-
fecting millions of PCs worldwide.
• 2010 - The discovery of the first cyber weapon
Stuxnet targets Iran’s nuclear facilities.
• 2011 - Sony’s PlayStation Network is breached
and goes offline. The total of individuals affected
by the PII breach was approximately 77 million.
• 2012 - LinkedIn is hacked, and 6.5 million user
accounts and passwords were stolen.
• 2013 - Tumblr is hacked, and over 65 million
unique emails and passwords were leaked.
While these significant cybersecurity events hap-
pened, the Security Rule in HIPAA was written at a
period where Windows XP Service Pack 1 was only
one year old. As highlighted in Section 7, the au-
thors would like to see Security Rule reviewed and
amended annually, to encompass the latest innova-
tions in technology, while ensuring lessons from ma-
jor cybersecurity events are taken into consideration.
5 HITECH HIT BY LOW TECH
EXPLOITS
During the recession of 2009, former United States
President Barack Obama signed the American Recov-
ery and Reinvestment Act of 2009 into law. Inside
this piece of legislation was the Health Information
Technology for Economic and Clinical Health Act
(HITECH). The HITECH Act was enacted to have
healthcare facilities implement an Electronic Health
Record (EHR) system to promote interoperability
ICISSP 2020 - 6th International Conference on Information Systems Security and Privacy
694
amongst healthcare facilities. The intended direction
was to make healthcare facilities use a certified EHR
and provide “Meaningful Use,” such as e-prescribing.
As part of the Obama Administration, this was an at-
tempt to provide a stimulus to the healthcare field.
HITECH authorized up to $27 billion in Medicare and
Medicaid payments over the next decade to providers
who implemented an EHR and met the Meaningful
Use requirements (DesRoches et al., 2013).
Starting in 2011 and for the next six years,
providers who adopted an EHR successfully received
a promised maximum incentive for $63,750 per year
from Medicaid. The EHR system had to be imple-
mented by 2016 to qualify for this program. Medi-
care offered a maximum payment of $44,000 over
the next five years. Any facility that did not imple-
ment an EHR by 2015 would be penalized 1% of
Medicare payments with the penalty increasing to 3%
over the next three years (DesRoches et al., 2013).
With the incentive of being rewarded with grant and
loan money, healthcare facilities began to quickly and
rapidly adopt EHR. The monetary penalties of not
having an EHR for Medicare and Medicaid reim-
bursement also impacted the haste in which EHRs be-
came implemented by healthcare facilities.
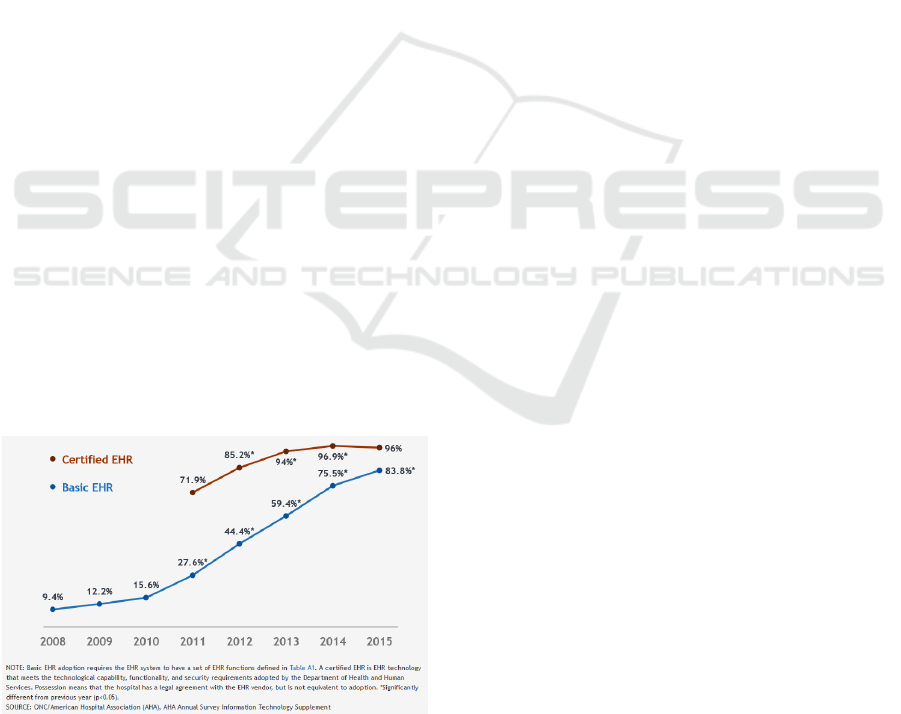
According to the Office of the National Health
Coordinator for Health Information Technology, in
2009 12.2% of non-Federal acute care hospitals had
a basic EHR. In the year 2012, the number of non-
Federal acute care hospitals with a basic EHR jumped
to 44.4%. Of these deployments, 85.2% qualified as
a certified EHR. In just three years, there was over
a 300% increase in implementing an EHR. By 2015
this number jumped to 83.8% in the ever-increasing
demand to implement an EHR before the penalties of
Medicare reimbursements (Henry et al., 2016).
Figure 5: Non-Federal acute care hospitals with adoption of
at least a Basic EHR.
Figure 5 Percent of non-Federal acute care hospitals
with adoption of at least a Basic EHR with notes
system and possession of a certified EHR: 2008-
2015 (Henry et al., 2016).
While the implementation of EHR for interoper-
ability is fantastic, the pace at which healthcare was
forced to implement these systems meant some cor-
ners had to be cut. Many health systems could not
afford an EHR, which is why only 12.2% of non-
Federal acute care hospitals had an EHR before the
enactment of HITECH (Henry et al., 2016). Unfor-
tunately, security was not on the agenda of things to
implement. Due to time restrictions, getting an EHR
running was more imperative than appropriately im-
plementing it with proper security controls.
According to research conducted by Texas State
University in 2016, it affirmed that cybersecurity at-
tacks on healthcare were up 125% since 2010. They
found that healthcare organizations spent around 95%
of their Information Technology budget on implemen-
tation and adoption, yet spent only the remaining 5%
on information security. Due to the rapid technolog-
ical advancements by federal policy initiatives, the
healthcare sector has become the number one target
of cyberattacks (Kruse et al., 2017).
One of the reason that healthcare is such a lucra-
tive industry to attack is because of the content of
medical records. A medical record contains Social
Security Numbers, addresses, phone numbers, and in-
surance information. Unlike stolen financial data, one
cannot put a freeze on their medical record or request
a new medical record number. A complete medical
record sells for an average on $50 on the black mar-
ket (Le Bris and El Asri, 2006). Due to the sensi-
tive information contained in a full medical record
there are various forms of fraud that can be commit-
ted. With ones Social Security Number, malicious ac-
tors could open and create new lines of credit under a
persons identity. With their full address information
they can fully compromise their identity. By having
access to their medical history and insurance informa-
tion, malicious actors could use this as a method for
prescription or healthcare fraud. One aspect that of-
ten goes overlooked, what will happen when the lose
of protected health information causes death. While
there are no reported cases, what could the opposition
of a nation state gain by knowing what medications
another world leader is allergic to? Will it take this
lose of life before cybersecurity legislation in health-
care is taken seriously?
Legislation and the Negative Impact on Cybersecurity in Healthcare
695

6 FDA (FAULTY DEVICE
ARRIVED) MEDICAL DEVICES
The greatest threat facing healthcare facilities are net-
works of interconnected medical devices that are in-
herently vulnerable. These devices are crucial in
patient care and could mean the difference between
life and death. Such devices are diagnostic devices
such as a MRI machine, infusion pumps, life support
equipment, and medical monitors such as a electroen-
cephalogram (EEG), laboratory analyzers, or insulin
pumps.
In 2011 Barnaby Michael Douglas Jack showed
the first exploit of a medical device at McAfee FO-
CUS 11 when he was able to have an insulin pump
deliver the maximum dose of 25 units until all 300
units had dispensed into a test dummy. A dosage of
10 units is enough to send an average diabetic patient
to the hospital. An insulin unit containing 300 units
should provide a patient three to four days worth of
insulin supplies (Viega and Thompson, 2012).
At the RSA Security Conference the following
year, Barnaby Jack was able to once more wire-
lessly hack an insulin pump from 90 meters away us-
ing high-gain antenna. Later in 2012, Barnaby Jack
was able to demonstrate the ability to hack a pace-
maker (Viega and Thompson, 2012). He was due
to present his hacking of pacemakers at Black Hat
2013, but was unfortunately found unresponsive in
his apartment and pronounced dead (Leyden, 2014).
While we lost one of the pioneers in medical device
exploitation, Barnaby Jack highlighted just how vul-
nerable these devices are. Unfortunately, since Barn-
aby Jack highlighted the weaknesses in medical de-
vices, security regarding them has not improved.
The United States has put the U.S. Food and
Drug Administration (FDA) in charge of regulating
the sale of medical device products in the United
States. With the adoption rate of technology after
HITECH became established, medical devices have
gone from stand-alone devices to networked devices.
On December 27th 2016 the FDA released its “Fi-
nal Guidance: Postmarket Management of Cyberse-
curity in Medical Devices.” Across the top of every
page it states “Contains Nonbinding Recommenda-
tions” (FDA, 2016). The organization that should be
assisting in securing medical devices can only make
recommendations that they feel are nonbinding.
The FDA states in these nonbinding agreements
that patches and update plans need to be submitted
to the FDA for review. In the field of cybersecu-
rity, patches and updates are one of the best defenses
we have, especially when critical vulnerabilities such
as EternalBlue or BlueKeep become commonplace.
With monthly patches coming out for Microsoft Win-
dows, it is an impossible task to re-certify every med-
ical device monthly. The gap in patch release to de-
ployment is immense. If there is a patch for a medical
device, the vendor must perform engineering analysis
before it can be submitted to the FDA for verification
and validation. After release, testing must be done
to ensure that target environments will not produce a
negative impact on patient safety or workflows. Once
completed, the deployment of the roll-out across all
the vendor’s customers and products must begin. This
complete process can take months to patch one critical
vulnerability, which is unacceptable when lives are on
the line (Williams and Woodward, 2015).
7 CONCLUSION AND FUTURE
WORK
As per our research, and experiences the authors
have found that as healthcare becomes more intercon-
nected and reliant on technology, cybersecurity needs
to become a priority in future legislation. The current
legislation and regulations that the United States has
enacted on healthcare have inherently weakened the
sector in cybersecurity. Healthcare has been forced to
implement technology at a rapid pace to avoid finan-
cial penalties. Regulations on medical devices cause
a direct hindrance to the process of securing medical
devices, putting lives at risk.
The authors would like to see modifications to
current legislation that adequately encompasses the
needs of cybersecurity in healthcare. HIPAA, which
intended to protect patient privacy and data, has not
seen an update to the Security Rule since 2003. While
HIPAA does not dictate security software or technol-
ogy, rather patient privacy, the authors would like to
see the Security Rule reviewed and amended annu-
ally, to encompass the latest innovations in technol-
ogy, while ensuring lessons from major cybersecu-
rity events are taken into consideration. When the
Security Rule was authored, it stated that computer
drives containing E-PHI should be destroyed using
a “reasonable” method. With the advent of Solid
State Drives what is considered “reasonable”? Fu-
ture legislation such as HITECH that forces technol-
ogy upon organizations should look at cybersecurity-
related ramifications before enactment. We can-
not legislate technology for the sake of advancement
without these critical considerations.
As additional future works the authors would like
to expand out from just legislation in the United
States and begin moving globally. With recent im-
plementation of the General Data Protection Regu-
ICISSP 2020 - 6th International Conference on Information Systems Security and Privacy
696

lation (GDPR) across the European Union, it sparks
the question; what potential vulnerabilities has GDPR
created in European healthcare? In the United States
under HIPAA and organization can be fined a maxi-
mum of $1.5 Million USD, where as the highest level
of fines under GDP are up to 20 million Euro or 4%
of worldwide annual revenue (Hilliard, 2019).
During our research, the United States Depart-
ment of Health and Human Services (HHS) proposed
changes to the Stark Law that would provide a safe
harbor for those that donate cybersecurity technol-
ogy. Per a HHS representative “We believe that omit-
ting a contribution requirement may allow providers
with limited resources to receive protected cyberse-
curity donations, while also using their own resources
to invest in other technology not protected by the safe
harbor, such as updating legacy hardware that may
pose a cybersecurity risk, or simply investing in their
own computers, phones, and other hardware” (Davis,
2019a). Similar to herd immunity, when smaller
healthcare facilities are secured, all of healthcare is
more secure. Until these issues in legislation and
regulation become wholly addressed, healthcare will
continue to be the number one target of malicious
threats.
REFERENCES
Assistance, H. C. (2003). Summary of the hipaa privacy
rule. Office for Civil Rights.
Beazley (2019). Beazley breach insights - february 2019.
Bitglass (2016). what a difference a year makes.
Branch, L. E. (2018). Cyber threats and healthcare orga-
nizations: A public health preparedness perspective.
Cyber Threats and Healthcare Organizations: APub-
lic Health Preparedness Perspective.
Davis, J. (2019a). Hhs stark law proposal permits cyberse-
curity donations to providers.
Davis, J. (2019b). Patients sue uconn health over data
breach caused by phishing attack.
DesRoches, C. M., Worzala, C., and Bates, S. (2013). Some
hospitals are falling behind in meeting ‘meaningful
use’criteria and could be vulnerable to penalties in
2015. Health Affairs, 32(8):1355–1360.
FDA (2016). Postmarket management of cybersecurity in
medical devices - guidance.
Field, M. (2018). Wannacry cyber attack cost the nhs £92m
as 19,000 appointments cancelled. The Telegraph.
for Disease Control, C. and Prevention (2018). Summary
health statistics: National health interview survey,
2018.
Henry, J., Pylypchuk, Y., Searcy, T., and Patel, V. (2016).
Adoption of electronic health record systems among
u.s. non-federal acute care hospitals: 2008-2015.
Hilliard, R. (2019). Hipaa versus gdpr.
Kruse, C. S., Frederick, B., Jacobson, T., and Monticone,
D. K. (2017). Cybersecurity in healthcare: A system-
atic review of modern threats and trends. Technology
and Health Care, 25(1):1–10.
Le Bris, A. and El Asri, W. (2006). State of cybersecurity
& cyber threats in healthcare ...
Leyden, J. (2014). Atm hacker barnaby jack’s death blamed
on accidental drug overdose.
OCR (2019). U.s. department of health and human services
office for civil rights breach portal: Notice to the sec-
retary of hhs breach of unsecured protected health in-
formation.
Paquet-Clouston, M., Haslhofer, B., and Dupont, B. (2019).
Ransomware payments in the bitcoin ecosystem.
Journal of Cybersecurity, 5(1).
Salcido, R. (2000). The government unleashes the stark law
to enforce the false claims act: The implications of the
government’s theory for the future of false claims act
enforcement. Health Law., 13:1.
Spence, N., Paul, D. P., and Coustasse, A. (2017). Ran-
somware in healthcare facilities: The future is now.
Marshall University Marshall Digital Scholar.
Viega, J. and Thompson, H. (2012). The state of embedded-
device security (spoiler alert: Its bad). IEEE Security
& Privacy, 10(5):68–70.
Williams, P. and Woodward, A. (2015). Cybersecurity vul-
nerabilities in medical devices: a complex environ-
ment and multifaceted problem. Medical Devices: Ev-
idence and Research, page 305.
Winton, R. (2016). Hollywood hospital pays $17,000 in bit-
coin to hackers; fbi investigating. Los Angeles Times.
Wright, A., Aaron, S., and Bates, D. W. (2016). The
big phish: Cyberattacks against u.s. healthcare
systems. Journal of General Internal Medicine,
31(10):1115–1118.
Legislation and the Negative Impact on Cybersecurity in Healthcare
697
