
Sensor-based Solutions for Mental Healthcare: A Systematic Literature
Review
Nidal Drissi
1
, Sofia Ouhbi
2
, Jos
´
e Alberto Garc
´
ıa-Bern
´
a
3
, Mohammed Abdou Janati Idrissi
1
and Mounir Ghogho
4
1
ENSIAS, Mohammed V University in Rabat, Rabat, Morocco
2
Dept. of Computer Science & Software Engineering, CIT, UAE University, Al Ain, U.A.E.
3
Dept. of Informatics and Systems, University of Murcia, Murcia, Spain
4
TICLab, International University of Rabat, Rabat, Morocco
mounir.ghogho@uir.ac.ma
Keywords:
Sensors, e-Mental Health, Mental Health, Systematic Literature Review.
Abstract:
Mental well-being is a crucial aspect of the person’s general health, compromised mental health impairs the
person’s functioning, decreases the quality of life, and limits the person’s contribution to society. The mental
health industry is still facing some barriers to healthcare delivery such as costs, mental health illiteracy, and
stigma. Incorporating technological interventions in the treatment and the diagnosis processes might help
overcome these barriers. Sensors are devices that have been used for healthcare since the 1990s and have
been incorporated into mental healthcare in different forms. In this study, we conducted a systematic literature
review to identify and analyze sensor-based solutions for mental healthcare. 12 studies were identified and
analyzed. The majority of the selected studies presented methods and models and were empirically evaluated
and showed promising accuracy results. Different types of sensors were used to collect different types of data
about the patient such as physical and behavioral information. The selected studies mainly addressed the use
of sensors for common mental issues like stress and depression or the analysis of general mental status. Some
studies reported some limitations mainly related to technological issues and lack of standards.
1 INTRODUCTION
According to the World Health Organization (WHO),
mental health is “a state of well-being in which the
individual realizes his or her own abilities, can cope
with the normal stresses of life, can work produc-
tively and fruitfully, and is able to make a contribu-
tion to his or her community” (Galderisi et al., 2015).
Many mental disorders represent a life-long resource
of dysfunction and are consistently associated with in-
creased disability as they have a personal and socioe-
conomic impact (Ormel et al., 1994). Serious men-
tal illnesses have a marked impact on life expectancy
as well, which is generally higher than the impact of
other well-recognized exposures such as smoking, di-
abetes, and obesity (Chang et al., 2011). Unfortu-
nately, most people in need for mental care services,
in both developed and developing countries, receive
no services at all (Kazdin, 2019).
Many barriers to mental healthcare delivery exist,
such as cost and reimbursement; policy and legal con-
straints; limited number of providers; stigma and self-
stigma for seeking treatment; mental health illiter-
acy; and cultural and ethnic influences (Hinshaw and
Stier, 2008; Andrade et al., 2014). Another less fre-
quently discussed barrier, yet a very important one, is
the dominant model of delivering psychosocial care,
which is based on a one-to-one, in-person treatment,
with a trained mental health professional, provided in
clinical setting (Kazdin, 2019).
Incorporating information and communication
technologies (ICT) in the treatment and diagnosis pro-
cesses of mental disorders might help overcome some
of the aforementioned mental healthcare delivery bar-
riers. ICT provide several technology-enabled ther-
apies, including internet-based programs, mobile ap-
plications and informational websites (Stone and Wal-
dron, 2019; Drissi et al., 2019c; Drissi et al., 2019b).
Sensors have been used for health purposes since the
1990s, and have been successfully used for mental
healthcare purposes as well (Abdullah and Choud-
Drissi, N., Ouhbi, S., Garcà a-Bernà ˛a, J., Idrissi, M. and Ghogho, M.
Sensor-based Solutions for Mental Healthcare: A Systematic Literature Review.
DOI: 10.5220/0009100805930600
In Proceedings of the 13th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2020) - Volume 5: HEALTHINF, pages 593-600
ISBN: 978-989-758-398-8; ISSN: 2184-4305
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
593
hury, 2018; Harari et al., 2017). Their use provides
different methods of data collection that can help
identify the person’s behaviors, physical indicators,
thoughts, feelings, and traits (Mohr et al., 2017), in
addition to several forms of patient’s monitoring and
treatment.
Researchers are showing interest in the use of sen-
sors for mental healthcare. Among others. (Baig
et al., 2017) conducted a systematic review of wear-
able patient monitoring systems and described chal-
lenges and opportunities. (Mukhopadhyay, 2014)
reviewed sensors-based activity monitoring systems
and described challenges and issues. (Drissi et al.,
2019a) provided a survey of literature on the use of
sensors for mental healthcare, describing addressed
topics and weak areas of the research.
2 METHODOLOGY
The present study is a systematic literature review
(SLR), based on guidelines proposed by (Keele,
2007), conducted on 12 studies proposing sensors-
based solutions for mental healthcare. The studies se-
lection and analysis processes are presented below.
2.1 Research Questions
Table 1 presents the research questions (RQs) of this
study and their motivation.
2.2 Research Strategy
The search process started by consulting the follow-
ing sources: IEEE Digital Library, ACM Digital Li-
brary, ScienceDirect, Springer Link and PubMed.
The following search string was used for the auto-
matic search of publications in the mentioned digi-
tal sources: “Sensors” AND “Mental” AND “Health”
AND “Care”. The search string was formulated to
include a broad selection of literature. In order to
determine whether to include or exclude a study, the
first author conducted a primary analysis by inspect-
ing each paper’s title, abstract and keywords.
2.3 Papers Selection
After the identification of relevant publications for the
study by the first author, information about each paper
from the outcome of search were filled in an excel file.
The second author revised the final selection. The in-
clusion criterion (IC) was limited to:
IC: Publications that address the use of sensors for
mental healthcare.
The studies that met the following exclusion criterion
(EC) were eliminated:
EC: Publications that were not solution proposals
such as, opinion papers and reviews.
2.4 Data Extraction Strategy
The data extraction process was mainly centered
around providing answers to the RQs. Data extracted
from each selected study were:
• Type of the proposed solution, which can be clas-
sified as: models, methods, tool-based techniques
or others.
• Types of sensors used in the proposed solution:
how they operate and what data they collect.
• Types of data collected by the sensors.
• Limitation of the proposed solution.
• Whether the proposed solution has been empir-
ically evaluated and how. An empirical evalua-
tion method can be classified as: experiment, case
study, survey, interview, or other.
• Mental disorders and mental health related issues
addressed by the selected solution proposals.
3 RESULTS
12 studies were selected as shown in Figure 1. Re-
sults from the papers selection and data extraction
processes are presented in Table 2.
Figure 1: Selection process.
3.1 RQ1. Types of the Proposed
Solutions (Contribution Types)
The contributions of the papers were mainly methods
and models with 41,67% each, and 16.66% tool-based
techniques. This section describes each solution and
how sensors were used in it.
(Yamaguchi et al., 1998) developed an indoor
monitoring system based on infrared positioning sen-
sors and magnetic sensors to observe the person’s be-
HEALTHINF 2020 - 13th International Conference on Health Informatics
594
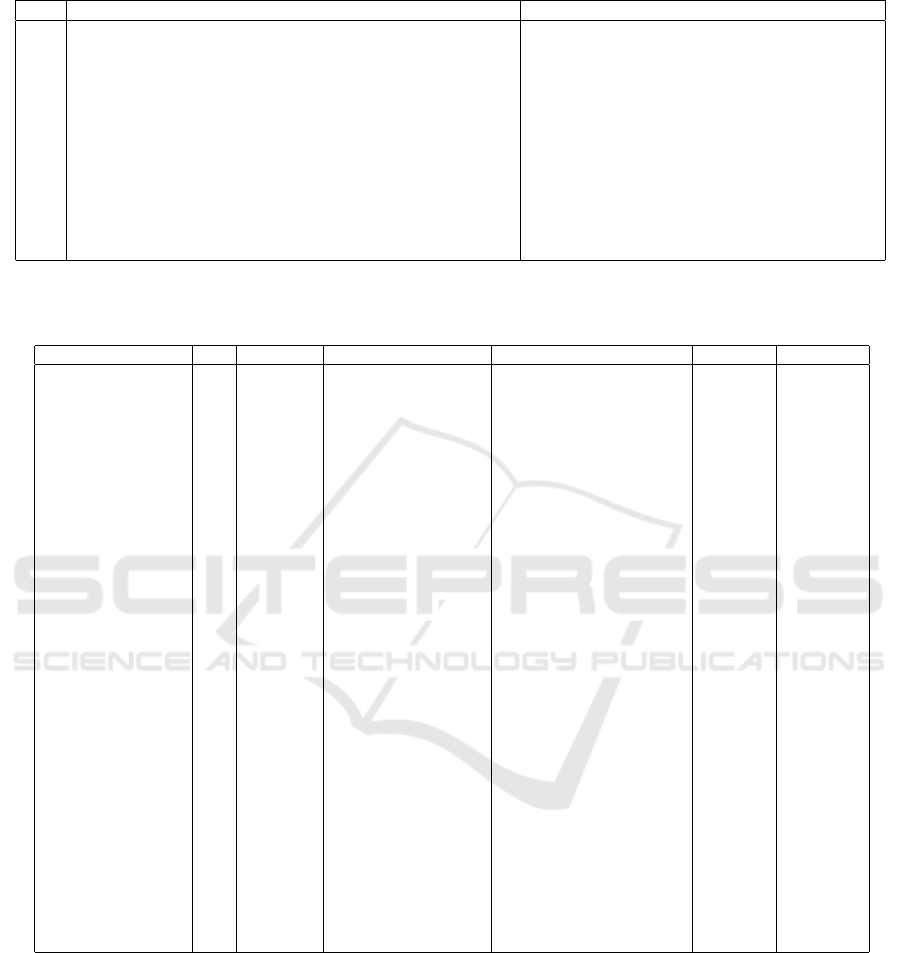
Table 1: Research questions and their motivations.
ID Research Question Motivation
RQ1 What is the type of the proposed solution ? To identify the different contribution types of the selected pa-
pers
RQ2 What are the types of sensors used in the proposed solutions ? To identify the different types of sensors and the most used
ones for mental healthcare purposes
RQ3 What are the types of data collected by the sensors ? To identify the different types of data that could be collected
by sensors and used for mental health care
RQ4 What are the limitations of the proposed solutions ? To identify problems and limitations associated with the use
of sensors for mental healthcare
RQ5 Are the proposed solutions empirically validated or evaluated ? To discover whether the efficiency of a proposed solution has
been empirically validated or evaluated
RQ6 What are the most addressed mental disorders and mental health related issues
in publications proposing sensors-based solutions for mental illnesses ?
To identify mental issues and disorders that are likely to be
managed with sensors-based solutions
Table 2: Results. Acronyms: Electroencephalography (EEG), Electrooculography (EOG), Electrocardiogram (ECG), Gal-
vanic Skin Response (GSR), Global Positioning System (GPS), Heart Rate (HR), Short Message Service (SMS).
Ref. Year RQ1 RQ2 RQ3 RQ5 RQ6
(McGinnis et al., 2018) 2018 Method Belt-worn sensor Motion: acceleration and angular
velocity
Experiment Depression,
anxiety
(Sahu and Sharma, 2016) 2016 Model EEG and EOG sensors Brainwaves and eye movement No General
mental status
(Farhan et al., 2016) 2016 Method Smartphone sensors Physical Activity, light informa-
tion, conversations, phone lock,
GPS location, audio
Experiment Depression
(Sano et al., 2015) 2015 Method Wrist sensor Skin temperature, skin conduc-
tance, activity, light exposure,
call, SMS, location, internet us-
age and “screen on” timing
Experiment General
mental sta-
tus, sleep
quality
(Sandulescu et al., 2015) 2015 Method Wristband sensor Electro-dermal activity, pulse
plethysmograph and blood
volume
Experiment Stress
(Palmius et al., 2014) 2014 Model Wrist sensor and smart-
phone sensors
Activity, sleep, ambient light lev-
els and social network activity
Experiment General
mental status
(Sano and Picard, 2013) 2013 Tool-based
technique
Wrist sensor Acceleration information and
skin conductance
Experiment Stress
(Burns et al., 2011) 2011 Model Smartphone sensors GPS location, ambient light, re-
cent calls, SMS, emails
Experiment Depression
(Wijsman et al., 2011) 2011 Method Wireless chest belt, piezo-
electric film sensor, wire-
less hand sensor and com-
mercial gel electrodes
Electrocardiography, respira-
tion, skin conductance, and
electromyography signals
Experiment Stress
(Fletcher et al., 2010) 2010 Tool-based
technique
Electrodermal activity sen-
sors, mobile Photoplethys-
mography sensors
Skin conductance, blood volume
pulse, HR
No General
mental status
(Sun et al., 2010) 2010 Model ECG sensor, chest strap,
GSR sensor, accelerometer
HR variability, GSR and move-
ment
Experiment Stress
(Yamaguchi et al., 1998) 1998 Model Infrared positioning sen-
sors and magnetic sensors
Activity and behavior (use of
rooms, equipment, bed. etc)
Experiment Behavior
havior and activity. Results showed that it is possi-
ble to learn and measure a person’s behavior, which
can be used for behavioral prediction if analyzed cor-
rectly. (Sun et al., 2010) presented an activity-aware
mental stress detection system, where physiological
measures like heart rate variability, galvanic skin re-
sponse (GSR) and movement data were collected dur-
ing three physical activities (sitting, standing, and
walking) using an Electrocardiogram (ECG) sensor,
a chest strap, a GSR sensor, and an accelerometer.
Collected data was analyzed and classified using ma-
chine learning features to detect stress. The system
achieved a classification accuracy of 80%.
(Fletcher et al., 2010) described a list of differ-
ent types of sensors and wireless solutions, and pre-
sented a list of opportunities and challenges associ-
ated with the use of these technologies. (Wijsman
et al., 2011) presented an approach to detect stress
Sensor-based Solutions for Mental Healthcare: A Systematic Literature Review
595

Table 3: Categories of the used sensors. Acronyms: Electroencephalography (EEG), Electrooculography (EOG), Electrocar-
diogram (ECG), Galvanic Skin Response (GSR).
Ref Category Sensors
(McGinnis et al., 2018; Sahu and Sharma,
2016; Sano et al., 2015; Sandulescu et al.,
2015; Palmius et al., 2014; Sano and Picard,
2013; Wijsman et al., 2011; Fletcher et al.,
2010; Sun et al., 2010)
Sensors attached to the
users body
EEG, ECG and EOG sensors, belt-
worn sensors, wrist sensors, chest
straps, piezoelectric film sensors, wire-
less hand sensors, commercial gel elec-
trodes, electrodermal Activity sensors,
accelerometers, and GSR sensors
(Farhan et al., 2016; Sano et al., 2015;
Palmius et al., 2014; Sano and Picard, 2013;
Burns et al., 2011; Yamaguchi et al., 1998)
Sensors attached to objects
used by the user or objects
surrounding the user
Built-in smartphone sensors, position-
ing sensors, and magnetic sensors
using physiological indicators. Different physiologi-
cal signals were measured using different sensors, an
analysis of the collected data resulted in a set of 7
principal components that could be used for stress de-
tection. The study showed a classification accuracy of
80% between stress and non-stress conditions.
(Burns et al., 2011) studied the feasibility and ef-
fectiveness of a mobile phone- and Internet-based in-
tervention for depression sufferers (Mobilyze!). The
study yielded an accuracy of (60% to 91%) predict-
ing categorical contextual states (e.g., location) and
a poor predictive capability for states rated on scales
(e.g., mood). The study also showed the potential ef-
ficacy of these types of interventions and described a
list of lessons learned and limitations of the approach.
(Sano and Picard, 2013) presented a tool-based
technique aiming to find physiological or behavioral
markers for stress, the technique is based on data
about the patient’s acceleration information and skin
conductance collected from a wrist-worn sensor, sur-
veys, and mobile phone usage. Correlation analysis of
the collected data showed over 75% accuracy of low
and high perceived stress recognition.
(Palmius et al., 2014) proposed a smartphone-
based system that allows the remote realtime collec-
tion of data about psychiatric patient symptoms to en-
able efficient allocation of psychiatric resources. The
data collection process is based on a wrist-worn ac-
tivity and sleep tracker and an Android-based mobile
application.
(Sano et al., 2015) proposed an approach to deter-
mine academic performance, sleep quality and mental
health conditions based on data collected from wear-
able wrist sensors like skin conductance, activity and
light exposure, as well as data on smartphone usage
such as calls, SMS and “screen on” timing. Collected
data was then analyzed using feature selection and
machine learning techniques. The evaluation process
yielded classification accuracies that ranged from 67
to 92% between the method and self-filed tests by par-
ticipants.
(Sandulescu et al., 2015) presented a machine
learning approach for stress detection using wearable
physiological sensors. Physiological data were col-
lected using a wristband sensor then analyzed using
machine learning techniques to classify the state of a
patient into “stressful” or “non-stressful” situations.
Classification results were found to be 73% to 83%
accurate.
(Farhan et al., 2016) introduced an approach to
find behavioral features that are correlated with de-
pression. The approach is based on smartphone data
collection to collect information about the patient
such as physical activity, light information, conver-
sation, phone lock and GPS location, with the help of
built-in smartphone sensors, then applies a multi-view
bi-clustering algorithm to identify homogeneous be-
havioral groups. A validation process of the approach
yielded an accuracy of 87%.
(Sahu and Sharma, 2016) presented a system that
collects certain parameters of brainwaves and eye
movement then interprets them using signal process-
ing modules to determine the mental status of the pa-
tient. Results can be displayed, used to initiate a mes-
sage alerts or feed the data to other systems.
(McGinnis et al., 2018) proposed a new approach
of diagnosing depression and anxiety in young chil-
dren, by the use of a 90-seconds fear induction task
during which the child movement is monitored us-
ing a commercially available belt-worn sensor cou-
pled with machine learning. The method has been
empirically evaluated by an experiment that showed
an accuracy that can reach 75%.
3.2 RQ2. Types of Sensors used in the
Proposed Solutions
Table 3 presents the different types of sensors used
in each solution. Two different categories of sen-
sors were identified: sensors that operate by being at-
tached to the user’s body and sensors that are either
attached to objects used by or surrounding the user.
Some studies used more than one type of sensors.
HEALTHINF 2020 - 13th International Conference on Health Informatics
596
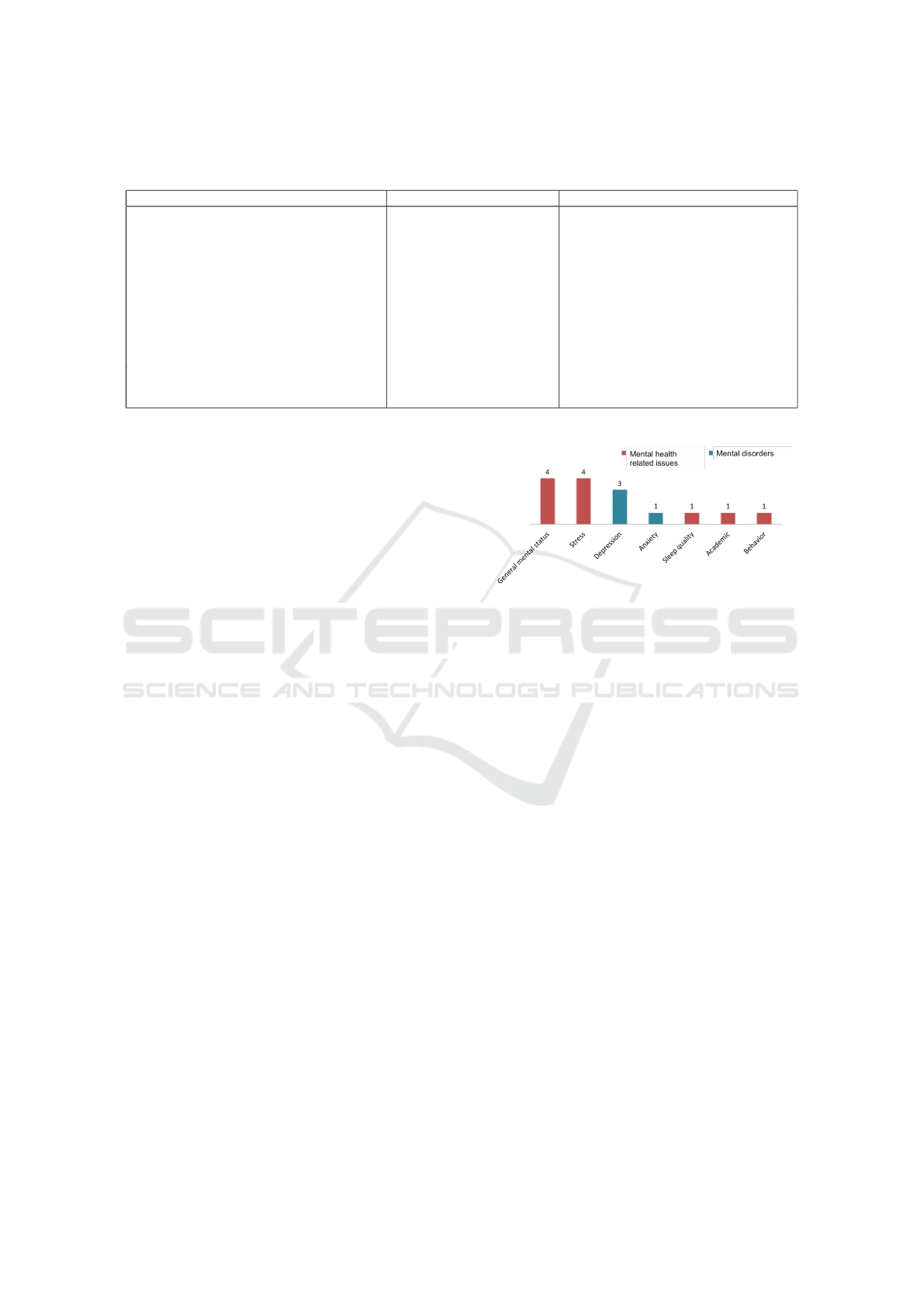
Table 4: Categories of the collected data. Acronyms: Galvanic Skin Response (GSR), Global Positioning System (GPS), Heart
Rate (HR), Short Message Service (SMS).
Ref Category Data
(Sahu and Sharma, 2016; Sano et al., 2015;
Sandulescu et al., 2015; Sano and Picard,
2013; Wijsman et al., 2011; Fletcher et al.,
2010; Sun et al., 2010)
Physical information Brainwaves, eye movement, skin tem-
perature, skin conductance, electro-
dermal activity, pulse plethysmography,
blood volume, sleep, electrocardiogra-
phy, respiration, HR, GSR and elec-
tromyography signals
(McGinnis et al., 2018; Farhan et al., 2016;
Sano et al., 2015; Palmius et al., 2014; Sano
and Picard, 2013; Sun et al., 2010; Yam-
aguchi et al., 1998)
Activity and behavior Acceleration, angular velocity, physical
Activity, movement, sleep and behavior
(Farhan et al., 2016; Sano et al., 2015;
Palmius et al., 2014; Sano and Picard, 2013;
Burns et al., 2011)
Smartphone usage Ambient light, phone Lock, GPS Loca-
tion, audio, calls, SMS, emails, internet
usage and “screen on” timing
3.3 RQ3. Data Collected by the Sensors
We identified three categories of the collected data:
physical information, activity and behavior, and
smartphone usage as presented in Table 4. Some so-
lutions used more than one category of data. Table 2
shows data used in each solution.
3.4 RQ4. Limitations of the Proposed
Solutions
Only 5 out of the 12 selected studies reported some
limitations to their solutions. A number of the se-
lected studies reported some similar limitations, like
connectivity problems, power consumption issues,
amount and accuracy of the collected data, and ac-
curate analysis and interpretation of the data (Burns
et al., 2011; Wijsman et al., 2011; Fletcher et al.,
2010; Sun et al., 2010). When using positioning and
magnetic sensors for activity and behavior sensing,
some limitations were reported such as the limited
functioning of the sensors under some external envi-
ronmental factors like hot air, and the inability to dis-
tinguish data in case of multiple users, which makes
the system helpful only in case of monitoring one pa-
tient (Yamaguchi et al., 1998). Adaptability limita-
tions and lack of standards were also reported (Burns
et al., 2011; Fletcher et al., 2010).
3.5 RQ5. Empirical Evaluation of the
Solutions
The majority of the selected solutions (83%) were
empirically evaluated by experiments, only 17%
(Sahu and Sharma, 2016; Fletcher et al., 2010) were
not empirically evaluated and classified as theories.
Figure 2: Addressed mental disorders and mental health re-
lated issues in the proposed solutions.
3.6 RQ6. Addressed Mental Disorders
and Mental Health Related Issues
Stress is the most addressed issue by the selected so-
lutions and depression is the most addressed disorder.
Many studies did not address a specific mental dis-
order and proposed solutions to predict the general
mental status of the user. Other studies used sensors
to observe indicators of the sanity and mental status
of the user such as behavior, academic performance,
and sleep quality. Figure 2 presents all the addressed
mental disorders and mental health related issues.
4 DISCUSSION
4.1 Types of the Proposed Solutions
The selected studies were not limited to providing IT-
related solutions on the use of sensors, but also pro-
vided new psychotherapy-related approaches for the
diagnosis, treatment, and monitoring of mental dis-
orders that are only possible by the use of sensors
such as associating behavioral traits with the mental
status (Farhan et al., 2016; Yamaguchi et al., 1998),
Sensor-based Solutions for Mental Healthcare: A Systematic Literature Review
597

predicting mental status by analyzing use of smart-
phones (Sano and Picard, 2013; Sano et al., 2015) and
detection and diagnosis of mental illnesses based on
physiological indicators (Sandulescu et al., 2015; Wi-
jsman et al., 2011; Sahu and Sharma, 2016). The use
of sensors in mental healthcare has opened a new win-
dow of opportunities not only in creating new systems
and technologies but also in creating new approaches
and methods for the diagnosis and treatment of mental
disorders. A need for publications proposing guide-
lines and recommendations on the use of sensors for
mental healthcare has been identified, which is neces-
sary to prevent errors and create effective solutions.
4.2 Sensors Types
Sensors were incorporated in different ways in the se-
lected solutions, depending on the type, sensors were
used to collect data from the patient’s body and envi-
ronment, and to detect habits and behaviors. Sensors
are convenient devices that can easily be attached to
the body, or objects from the environment, and that
are already integrated into devices like smartphones
and computers. The variety in the types of sensors
helped detect different indicators and gather different
types of information that are helpful in the diagnosis
and management of mental illnesses, and also encour-
aged researchers to find associations between differ-
ent types of data and mental status.
4.3 Data Collected by the Sensors
The selected solutions used sensors mainly to collect
and detect three categories of data: physical informa-
tion, activity and behavior, and smartphone usage.
• Patterns of physical symptoms are associated with
certain mental illnesses, therefore can be used
to detect psychological disorders (Larson et al.,
2001).
• Activity and behavior were found to have a bidi-
rectional connection with mental disorders, as
regular physical activity have an inverse associa-
tion with depression and anxiety symptoms (King
et al., 2013), also physical activity is associated
with reduced risk of some mental disorders and
reduced degree of co-morbidity (Str
¨
ohle et al.,
2007) and may be used as a safe and cost-effective
prevention and treatment tool (King et al., 2013),
analyzing activity and behavior can create an un-
derstanding of the mental status of the person.
On the other hand, some mental barriers like
fear were proved to have a negative impact on
the person’s physical activity and social behav-
ior (Stafford et al., 2007), changing bad behaviors
and improving physical activity can improve the
mental status.
• Analyzing smartphone usage habits can provide
an initial view of the mental status of the per-
son. Compulsive usage of smartphones is re-
lated to some psychological traits like anxiety
(Lee et al., 2014), self-control and communica-
tion issues, and general mental discomfort (Jang
and Kwag, 2015).
4.4 Limitations of the Proposed
Solutions
The use of sensors for mental healthcare offers many
opportunities, yet it faces some limitations that need
to be addressed to benefit effectively from the sen-
sors technology. Most of the reported limitations were
related to technological issues which are relatively
straightforward to fix once recognized, either by us-
ing a different technology or approach. Technologi-
cal issues are common and are usually overcome due
to the continuous technological development. Lack
of standards was also among the reported limitations,
which needs to be addressed by standardization or-
ganizations, as standards and guidelines are crucial
to the making and success of the solutions, more re-
search and solutions are needed in this area.
4.5 Empirical Evaluation
The only identified empirical evaluation method in the
selected studies was experiments, which was adopted
mainly for the controlled conditions and environment.
All empirically evaluated solutions followed similar
processes and had the main necessary elements of ex-
periments (Jedlitschka and Pfahl, 2005). The empir-
ical evaluation of the sensors-based solutions yielded
promising accuracy results, with a maximum reported
accuracy level of 92% (Sano et al., 2015). But the
controlled environment of experiments raises some
concerns, as most of the proposed solutions are sup-
posed to be used by the patients in real and not con-
trolled circumstances, that differ from a patient to
another and from an environment to another, which
might affect the reported accuracy.
The use of other empirical evaluation methods can
be beneficial and help improve the proposed solu-
tions, for example, case studies can help detect possi-
ble issues and barriers of implementing the solutions
in real life, surveys can help gather needed data, and
interviews can be used to identify and understand pa-
tients’ and clinicians’ opinion on the solutions, which
is crucial and taking it into consideration may result
in more effective solutions.
HEALTHINF 2020 - 13th International Conference on Health Informatics
598

4.6 Addressed Mental Disorders and
Mental Health Related Issues
Depression and stress were proved to have an associa-
tion with physical indicators like heart rate and phys-
ical activity (King et al., 2013), which makes sensors
a helpful tool to manage these types of disorders and
issues, as sensors are mainly used to measure physi-
cal indicators and observe activity and behavior. The
selected solutions do not address complex disorders
such as schizophrenia, bipolar disorder or psychosis,
which might be due to the complex nature of these
disorders and the unwillingness or inability of patients
with these types of mental illnesses to use sensors-
based treatments. The use of sensors in mental health-
care creates new ways of diagnosis, treatment, and
monitoring. Future studies should address the use of
sensors for different types of mental disorders.
4.7 Limitations
This study may have some limitations, such as: (i)
missing terms from the search string might have im-
plications on the results; and (ii) other RQs might
have been relevant to extract further information from
the selected studies.
5 CONCLUSION
Sensors have been incorporated in mental healthcare
for several purposes, sensors can be used to moni-
tor the physical activity and behavior, measure phys-
ical indicators or collect daily habits and information
about the person. In this paper, we identified and an-
alyzed 12 sensors-based solutions for mental health-
care. Different types of sensors were used in the solu-
tions, to collect and manage different types of infor-
mation about the patients. The majority of the solu-
tions were designed to monitor stress, depression and
general mental status, and were empirically evaluated
and showed promising results.
ACKNOWLEDGEMENTS
This paper is part of the Startup project 1093 funded
by UAE University (2019-2021).
REFERENCES
Abdullah, S. and Choudhury, T. (2018). Sensing technolo-
gies for monitoring serious mental illnesses. IEEE
MultiMedia, 25(1):61–75.
Andrade, L., Alonso, J., Mneimneh, Z., Wells, J., Al-
Hamzawi, A., Borges, G., Bromet, E., Bruffaerts,
R., De Girolamo, G., De Graaf, R., Florescu, S.,
Gureje, O., HR, H., Hu, C., Huang, Y., Hwang, I.,
Jin, R., Karam, E., Kovess-Masfety, V., Levinson, D.,
Matschinger, H., O’Neill, S., Posada-Villa, J., Sagar,
R., Sampson, N., Sasu, C., Stein, D., Takeshima, T.,
Viana, M., Xavier, M., and Kessler, R. (2014). Barri-
ers to mental health treatment: results from the WHO
world mental health surveys. Psychological medicine,
44(6):1303–1317.
Baig, M. M., GholamHosseini, H., Moqeem, A. A., Mirza,
F., and Lind
´
en, M. (2017). A systematic review
of wearable patient monitoring systems–current chal-
lenges and opportunities for clinical adoption. Journal
of medical systems, 41(7):115.
Burns, M. N., Begale, M., Duffecy, J., Gergle, D., Karr,
C. J., Giangrande, E., and Mohr, D. C. (2011). Har-
nessing context sensing to develop a mobile interven-
tion for depression. Journal of Medical Internet Re-
search, 13(3):e55.
Chang, C.-K., Hayes, R. D., Perera, G., Broadbent, M. T.,
Fernandes, A. C., Lee, W. E., Hotopf, M., and Stewart,
R. (2011). Life expectancy at birth for people with
serious mental illness and other major disorders from
a secondary mental health care case register in london.
PloS one, 6(5):e19590.
Drissi, N., Ouhbi, S., Janati Idrissi, M. A., El Koutbi, M.,
and Ghogho, M. (2019a). On the use of sensors
in mental healthcare. Intelligent Environments 2019,
26:307–316.
Drissi, N., Ouhbi, S., Janati Idrissi, M. A., and Ghogho,
M. (2019b). Gamification-based apps for PTSD:
an analysis of functionality and characteristics. In
16th ACS/IEEE International Conference on Com-
puter Systems and Applications (AICCSA), pages 1–6.
Drissi, N., Ouhbi, S., Janati Idrissi, M. A., and Ghogho, M.
(2019c). Mobile apps for Post Traumatic Stress Dis-
order. In 41st Annual International Conference of the
IEEE Engineering in Medicine and Biology Society
(EMBC), pages 4279–4282. IEEE.
Farhan, A. A., Lu, J., Bi, J., Russell, A., Wang, B., and
Bamis, A. (2016). Multi-view bi-clustering to identify
smartphone sensing features indicative of depression.
In IEEE First International Conference on Connected
Health: Applications, Systems and Engineering Tech-
nologies (CHASE), pages 264–273. IEEE.
Fletcher, R. R., Ming-Zher Poh, R., and Eydgahi, H. (2010).
Wearable sensors: opportunities and challenges for
low-cost health care. In Annual International Confer-
ence of the IEEE Engineering in Medicine and Biol-
ogy Society (EMBC). Institute of Electrical and Elec-
tronics Engineers (IEEE).
Galderisi, S., Heinz, A., Kastrup, M., Beezhold, J., and Sar-
torius, N. (2015). Toward a new definition of mental
health. World Psychiatry, 14(2):231–233.
Sensor-based Solutions for Mental Healthcare: A Systematic Literature Review
599

Harari, G. M., M
¨
uller, S. R., Aung, M. S., and Rentfrow,
P. J. (2017). Smartphone sensing methods for study-
ing behavior in everyday life. Current opinion in be-
havioral sciences, 18:83–90.
Hinshaw, S. P. and Stier, A. (2008). Stigma as related to
mental disorders. Annu. Rev. Clin. Psychol., 4:367–
393.
Jang, H.-J. and Kwag, Y.-K. (2015). Comparison of factors
associated with smartphone over-usage: Focusing on
self-control, mental health and interrelationship. Jour-
nal of the Korea Academia-Industrial cooperation So-
ciety, 16(1):146–154.
Jedlitschka, A. and Pfahl, D. (2005). Reporting guidelines
for controlled experiments in software engineering. In
International Symposium on Empirical Software En-
gineering, 2005., pages 10–pp. IEEE.
Kazdin, A. E. (2019). Annual research review: Expand-
ing mental health services through novel models of in-
tervention delivery. Journal of Child Psychology and
Psychiatry, 60(4):455–472.
Keele, S. (2007). Guidelines for performing systematic lit-
erature reviews in software engineering. Technical re-
port, Technical report, Ver. 2.3 EBSE Technical Re-
port. EBSE.
King, W. C., Kalarchian, M. A., Steffen, K. J., Wolfe, B. M.,
Elder, K. A., and Mitchell, J. E. (2013). Associations
between physical activity and mental health among
bariatric surgical candidates. Journal of psychoso-
matic research, 74(2):161–169.
Larson, G. E., Booth-Kewley, S., Merrill, L. L., and
Stander, V. A. (2001). Physical symptoms as indi-
cators of depression and anxiety. Military medicine,
166(9):796–799.
Lee, Y.-K., Chang, C.-T., Lin, Y., and Cheng, Z.-H. (2014).
The dark side of smartphone usage: Psychological
traits, compulsive behavior and technostress. Com-
puters in human behavior, 31:373–383.
McGinnis, R. S., McGinnis, E. W., Hruschak, J., Lopez-
Duran, N. L., Fitzgerald, K., Rosenblum, K. L., and
Muzik, M. (2018). Wearable sensors and machine
learning diagnose anxiety and depression in young
children. In IEEE EMBS International Conference on
Biomedical & Health Informatics (BHI), pages 410–
413. IEEE.
Mohr, D. C., Zhang, M., and Schueller, S. M. (2017).
Personal sensing: understanding mental health using
ubiquitous sensors and machine learning. Annual re-
view of clinical psychology, 13:23–47.
Mukhopadhyay, S. C. (2014). Wearable sensors for human
activity monitoring: A review. IEEE sensors journal,
15(3):1321–1330.
Ormel, J., VonKorff, M., Ustun, T. B., Pini, S., Korten, A.,
and Oldehinkel, T. (1994). Common mental disorders
and disability across cultures: results from the who
collaborative study on psychological problems in gen-
eral health care. JAMA, 272(22):1741–1748.
Palmius, N., Osipov, M., Bilderbeck, A., Goodwin, G.,
Saunders, K., Tsanas, A., and Clifford, G. (2014). A
multi-sensor monitoring system for objective mental
health management in resource constrained environ-
ments. In Appropriate Healthcare Technologies for
Low Resource Settings (AHT). IET.
Sahu, S. and Sharma, A. (2016). Detecting brainwaves to
evaluate mental health using labview and applications.
In International Conference on Emerging Technologi-
cal Trends (ICETT), pages 1–4. IEEE.
Sandulescu, V., Andrews, S., Ellis, D., Bellotto, N., and
Mozos, O. M. (2015). Stress detection using wear-
able physiological sensors. In International Work-
Conference on the Interplay Between Natural and Ar-
tificial Computation, pages 526–532. Springer.
Sano, A., Phillips, A. J., Amy, Z. Y., McHill, A. W., Tay-
lor, S., Jaques, N., Czeisler, C. A., Klerman, E. B.,
and Picard, R. W. (2015). Recognizing academic
performance, sleep quality, stress level, and mental
health using personality traits, wearable sensors and
mobile phones. In IEEE 12th International Confer-
ence on Wearable and Implantable Body Sensor Net-
works (BSN), pages 1–6. IEEE.
Sano, A. and Picard, R. W. (2013). Stress recognition us-
ing wearable sensors and mobile phones. In Humaine
Association Conference on Affective Computing and
Intelligent Interaction, pages 671–676. IEEE.
Stafford, M., Chandola, T., and Marmot, M. (2007). As-
sociation between fear of crime and mental health
and physical functioning. American journal of pub-
lic health, 97(11):2076–2081.
Stone, L. and Waldron, R. (2019). Great expectations and e-
mental health: The role of literacy in mediating access
to mental healthcare. Aust J Gen Pract, 48(7):474–79.
Str
¨
ohle, A., Hoefler, M., Pfister, H., Mueller, A.-G., Hoyer,
J., Wittchen, H.-U., and Lieb, R. (2007). Physical ac-
tivity and prevalence and incidence of mental disor-
ders in adolescents and young adults. Psychological
medicine, 37(11):1657–1666.
Sun, F.-T., Kuo, C., Cheng, H.-T., Buthpitiya, S., Collins, P.,
and Griss, M. (2010). Activity-aware mental stress de-
tection using physiological sensors. In International
conference on Mobile computing, applications, and
services, pages 282–301. Springer.
Wijsman, J., Grundlehner, B., Liu, H., Hermens, H., and
Penders, J. (2011). Towards mental stress detec-
tion using wearable physiological sensors. In An-
nual International Conference of the IEEE Engineer-
ing in Medicine and Biology Society, pages 1798–
1801. IEEE.
Yamaguchi, A., Ogawa, M., Tamura, T., and Togawa, T.
(1998). Monitoring behavior in the home using posi-
tioning sensors. In 20th Annual International Confer-
ence of the IEEE Engineering in Medicine and Biol-
ogy Society. Vol. 20 Biomedical Engineering Towards
the Year 2000 and Beyond (Cat. No. 98CH36286),
volume 4, pages 1977–1979. IEEE.
HEALTHINF 2020 - 13th International Conference on Health Informatics
600
