
A Smart Healthcare: Methods based on WBAN and Multi-engine
Artificial Intelligence
Nourhene Ellouze
1
and Noureddine Boudriga
2
1
ISLAIB, Jendouba University, Tunisia
2
SUP’COM, Carthage University, Tunisia
Keywords:
Healthcare Systems, Wearable Body Area Network, Implantable Medical Devices, Artificial Intelligence.
Abstract:
Healthcare systems are promising solutions to improve medical services offered to patients suffering from
chronic illness. The majority of the healthcare systems proposed in the literature are built to monitor and
treat a single type of disease. In this paper, we propose an architecture of a Smart Healthcare System carried
by a Wireless Body Area Network to supervise multiple diseases and promote the diagnosis and reactions to
occurred health anomalies. We also implement a multi-engine artificial intelligence allowing the correlation
between the different occurred anomalies related to multiple diseases. Forward and backward reasoning were
also integrated to handle the early detection of anomalies and the provision of medical explanations of occurred
health situations, respectively. A case study exemplifying our proposal were also detailed.
1 INTRODUCTION
Healthcare systems promoted great development to
medicare services and brought immense benefits to
human being. In particular, they have enabled the
improvement of the life quality of patients suffering
from chronic diseases, since they provide continuous
surveillance of their health status independently of
their locations. The concept of Wireless Body Area
Network (WBAN) highlights efficient technologies
for such systems. A WBAN is a network of wearable
devices, which can be either implanted in the patient’s
body or placed on a fixed body position. It allows the
surveillance of the patient’s health status and the de-
livery of appropriate therapies, when required.
Multiple research works addressed the design of
WBAN based healthcare systems and discussed the
suitable communication technologies. An overview
of these proposals will be provided in the sequel. The
majority of the proposed healthcare systems exhibit a
set of limits. First, the capacity of these systems in
supervising and managing various parameters is re-
duced. This is due to the lack of suitable techniques
allowing WBAN to firstly filter, merge and aggregate
the sensory data it collects and then to reason and in-
terpret aggregated data, to detect healthcare anoma-
lies. Second, the majority of healthcare systems allow
the supervision of a single type of diseases. In partic-
ular, they do not implement techniques allowing the
assessment of the interdependence of the evolution of
multiple physiological parameters related to different
diseases. Nevertheless, sometimes it becomes crucial
to monitor and treat multiple diseases, especially that
a patient could suffer from multiple chronic diseases
and may need the supervision of multiple physiolog-
ical parameters; therefore, he/she may carry multi-
ple medical devices. Third, the WBAN based health-
care systems exhibit the absence of communication
technologies allowing the intra-nodes communication
when the WBAN integrates Implantable Medical de-
vices (IMDs), especially that such a communication
improves the efficiency of IMDs in detecting occurred
anomalies and delivering the suitable therapies.
We propose in this paper to design a healthcare
system which allows: handling near real time
1
event
diagnosis, enabling early detection of anomalies, re-
porting health information, and contributing to the re-
mote reactions to occurring events. This requires the
WBAN to be equipped with a certain extent of intel-
ligence related to multiple disciplines. This can be
achieved thanks to the use of a multi-engine artifi-
cial intelligence allowing the diagnosis of multiple
diseases. In fact, every single-engine performs the
diagnosis of a single disease. The WBAN can then
1
Near real time means real time with a small delay
which allows the achievement of the diagnosis related to
occurred events and does not exceed a predefined threshold.
184
Ellouze, N. and Boudriga, N.
A Smart Healthcare: Methods based on WBAN and Multi-engine Artificial Intelligence.
DOI: 10.5220/0009095301840191
In Proceedings of the 13th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2020) - Volume 1: BIODEVICES, pages 184-191
ISBN: 978-989-758-398-8; ISSN: 2184-4305
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

infer the decisions suitable to detected anomalies by
operating the inter-operation of the engines. The de-
cisions obtained are achieved through multiple infer-
ence rules, multi-point measures, and a variety of ex-
pert knowledge about pathologies.
The paper contribution is three-fold. First, we
propose an architecture of a smart healthcare system
carried by a WBAN, which integrates heterogeneous
wearable and implantable medical devices and sen-
sors, to supervise multiple diseases and promote the
diagnosis and reactions to occurred anomalies. Sec-
ond, we implement a multi-engine artificial intelli-
gence, to allow analyzing the interdependence be-
tween the evolution of measured parameters and the
health anomalies occurrence, and correlating between
the different occurred anomalies related to multiple
diseases. Third, we integrate the use of a smart central
node which implements the multi-engine artificial in-
telligence. This node integrates at least two communi-
cation interfaces to ensure the data exchange between:
the IMDs and the nodes part of the WBAN, and be-
tween the WBAN and a remote supervision system.
The remaining part of the paper is organized as
follows. Section 2 provides a literature review of
the developed WBAN based healthcare systems and
presents the requirements of an efficient healthcare
system. In Section 3, we detail the proposed archi-
tecture of the healthcare system. Section 4 illustrates
the implementation of the multi-engine artificial intel-
ligence. In Section 5, we present a case study exem-
plifying our proposal. Section 6 concludes the paper.
2 OVERVIEW OF HEALTHCARE
SYSTEMS
This section reviews WBAN based healthcare sys-
tems and highlights the main requirements.
2.1 Literature Review
Because of the life-staining functions they can pro-
vide to patients, several research works addressed the
design of WBAN based healthcare systems. For in-
stance, a body sensor network for the detection of a
cardiac arrhythmia, namely Atrial Fibrillation (AF),
was proposed in (AlMusallam and Soudani, 2019).
This system uses a smart electrocardiogram (ECG)
sensor to detect AF episodes and to send alerts to the
base station. This proposal can only detect a single
type of arrhythmia, which makes it inefficient. In-
deed, a patient could suffer from multiple arrhythmia.
In (Sahoo et al., 2018), a healthcare system for the
detection of multiple arrhythmia was proposed. This
system supervises the non-invasive seismocardiogram
and the ECG signals, to guarantee a reliable detection
of arrhythmia. However, it does not consider the case
when the patient carries an IMD (e.g., cardiac defib-
rillator) treating detected arrhythmia.
A healthcare system for diabetic patients was pro-
posed in (Alfian et al., 2018). This system measures
the patient’s vital sign and transmits the sensed data
to a remote server, which performs data processing to
predict diabetes and blood glucose level, using ma-
chine learning methods. Another healthcare system
to manage Bipolar disease, was proposed in (Valenza
et al., 2016). This system implements a methodology
allowing it to assess the patients mood status and pre-
dict mood changes based on heartbeat dynamics.
All of the presented healthcare systems provide
the supervision of the patient’s health status, to man-
age a single disease. Some of these proposals allow
the prediction of anomalies, while others only provide
the real time detection . Moreover, these systems ex-
hibit the lack of proactive techniques allowing them
to respond to the detected anomalies. The only reac-
tion consists in notifying healthcare professionals. In
particular, no one of these systems discusses the in-
tegration of medical devices to enable delivery of the
suitable treatments when detecting anomalies.
Multiple research works reviewed the communi-
cation technologies for a WBAN based healthcare
system and discussed their efficiencies. In (Teshome
et al., 2018), the authors reviewed the progress
of communication technologies of implants (devices
which are surgically implanted, ingested, or injected
in the patient’s body). The authors in (Rizwan
et al., 2018) reviewed the nano-sensors integrated in
WBANs together with the nano-communication net-
works intended for healthcare applications. They
highlight the need of robust solution ensuring a nano-
communication in large-scale nano-networks.
2.2 Healthcare System Requirements
To provide an efficient supervision and control, the
healthcare system should at least fulfill the following
requirements. First, it should guarantee continuous
and real-time surveillance of the patient’s physiolog-
ical parameters. Indeed, the suspension or the delay-
ing of the surveillance of any parameter could lead
to an erroneous evaluation of the health status. This
makes the system unsafe, since an erroneous evalua-
tion induces the absence or the inappropriate delivery
of treatments, which could cause harms to the patient.
Second, the healthcare system should allow man-
aging multiple diseases. For this, various physiolog-
ical parameters need to be monitored. This could be
A Smart Healthcare: Methods based on WBAN and Multi-engine Artificial Intelligence
185

Table 1: Comparison between healthcare systems.
Healthcare systems
Monitored
parameters
Anomalies detection
Reactions to
detected anomalies
Diseases
Control
(AlMusallam and
Soudani, 2019)
Single Real time detection Absence Single
(Sahoo et al., 2018) Multiple Real time detection Alerting Single
(Alfian et al., 2018) Multiple Real time and early detection Alerting Single
(Valenza et al., 2016) Multiple Real time and early detection Absence Single
Our system Multiple Real time and early detection
Alerting and
therapies delivery
Multiple
achieved through the integration of multiple types of
biomedical sensors and medical devices in the WBAN
part of the healthcare system. Moreover, the system
should also enable the analysis and the processing of
collected data, to provide an accurate evaluation of
the health status, whatever the supervised diseases.
Third, for safety purposes, the healthcare system
should promote the early detection of critical health
status. In particular, such a functionality would allow
the system to apply the suitable reactions in order to
prevent the occurrence of the critical health status.
Fourth, the healthcare system should promote the
delivery of proactive reactions to occurred anoma-
lies. This could be achieved through the integration
of medical devices, which guarantee the delivery of
treatments, suitable to the detected anomalies. More-
over, the healthcare system should also implement
proactive techniques allowing it to generate the suit-
able decisions to be implemented by these devices.
Table 1 provides a summary comparison of the
presented healthcare systems. Based on this table,
we notice that our system provides several enhance-
ments in comparison to the other systems. First, like
some healthcare systems, our system offers, not only
the real time detection, but also the early detection of
anomalies. Second, further the delivery of alerts, our
system enables the implementation of proactive reac-
tions by delivering therapies. Third, our healthcare
system allows controlling multiple diseases. Such a
function is not provided by the other systems.
3 ARCHITECTURE OF A SMART
WBAN BASED HEALTHCARE
SYSTEM
The purpose of this section is to present the architec-
ture of the proposed healthcare system.
3.1 Healthcare System Architecture
The healthcare system architecture integrates two
components (WBAN and remote supervision system)
which interact via public communication networks.
Wireless Body Area Network (WBAN). It con-
sists of interconnected nodes, which are carried or im-
planted into the patient’s body. Based on their func-
tions, we distinguish three types of WBAN nodes:
Biomedical Sensors: They measure physiologi-
cal parameters and collect vital signs. The data they
gather are wirelessly sent to the central node, using
Bluetooth Low Energy (BLE) protocol, for example.
Medical Devices: Based on the sensed prameters,
a medical device detects anomalies and treats them by
delivering the suitable therapies. It also sends data de-
scribing detected anomalies and delivered therapies to
the central node using the Medical Implant Commu-
nication System (MICS) band, and it implements the
decisions received from the central node.
A central Node: It acts as a gateway between
the WBAN nodes and the remote supervision sys-
tem, to exchange data (i.e., physicians queries, health
status, and sensory data). It also provides a set of
features. First, it analyzes the data received from
WBAN nodes. Second, it ensures the early detection
of anomalies and generates the suitable decisions to
them. Third, it sends the generated decisions to the
RSS to be validated by physicians, then it sends them
to the medical devices to be implemented through
therapies delivery. Fourth, it provides medical expla-
nations of occurred anomalies. Such features provide
a certain degree of autonomy to the WBAN, since
they allow it to react to occurred critical situations and
rescue patients until receiving medical assistance.
A WBAN may integrate a central node and a sin-
gle IMD. The selection of IMDs depends on the con-
trolled diseases. For instance, to manage heart failure,
we use an implantable cardiac device, which includes
its appropriate sensors (e.g., cardiac sensors). Never-
theless, to increase visibility and ameliorate the accu-
BIODEVICES 2020 - 13th International Conference on Biomedical Electronics and Devices
186

racy of the detection and reaction to occurred anoma-
lies, multiple biomedical sensors may be integrated.
Remote Supervision System (RSS). It integrates a
dedicated server and a thin client interface. The ded-
icated server integrates: a remote database to store
the patient’s health status; and a data analysis and
processing module to perform an advanced data pro-
cessing. In this research work, we propose that the
data analysis and processing module is equipped with
an advanced extent of intelligence related to multi-
ple disciplines, so that it can assist physicians in vali-
dating the decisions generated by the central node or
generating new decisions. The client interface allows
physicians to access to the dedicated server function-
alities and exchange data with the WBAN.
In the proposed healthcare system, we distinguish
two interaction scenarios between the WBAN and the
RSS. The first scenario is initiated by the central node,
when detecting anomalies, to send alerts (which in-
clude the health status description) to the RSS to-
gether with the generated decisions to be validated.
The second interaction scenario is initiated by the
RSS to: collect health status data, request medical ex-
planations about an occurred anomaly, or to perform a
regular diagnosis by requesting real time sensory data.
3.2 Artificial Intelligence (AI) for Smart
WBAN
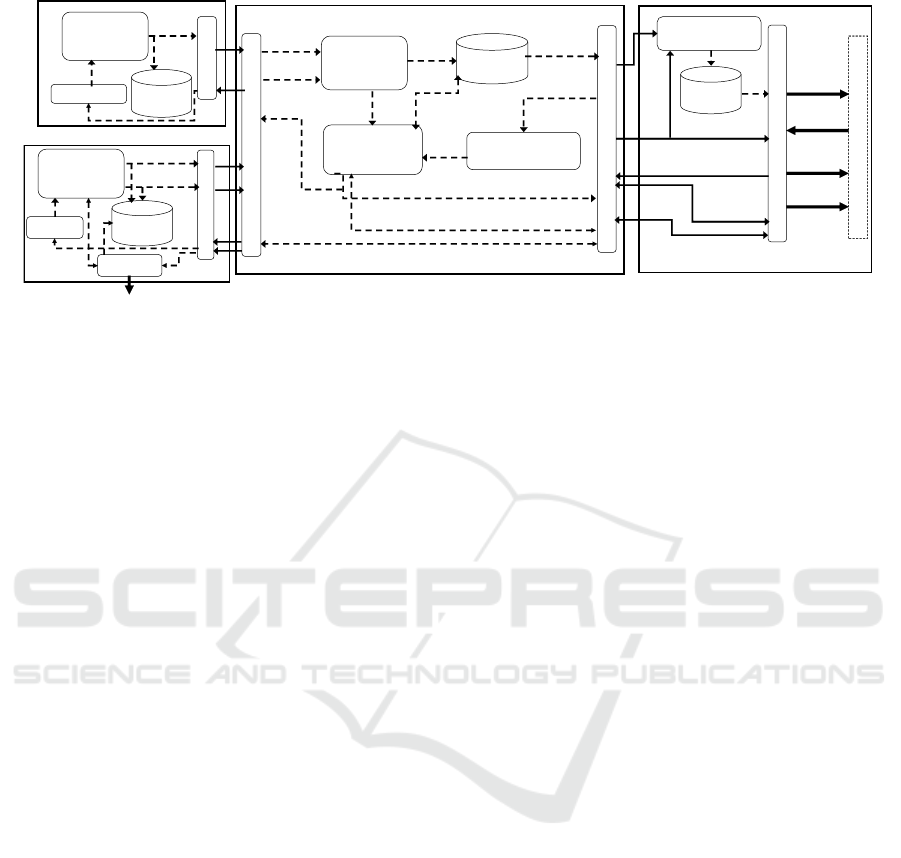
In this subsection, we detail the architecture of the
healthcare system, depicted in Figure 1, together with
the AI implementation within the WBAN .
Data Processing and Analysis. Due to the limited
energy resources and computational capabilities at the
WBAN nodes level, the analysis and processing of
health data is performed at three levels using specific
data processing and analysis techniques. The first
level is provided thanks to the data processing and
analysis module, which is integrated at the biomedical
sensors and medical devices levels. This module con-
verts the large volume of data (e.g., values, signals) it
receives from the sensing module into a usable infor-
mation (e.g., features, states), eliminates duplicates,
and stores them into its local database.
The second level refers to the data processing
analysis module part of the central node. This module
periodically collects data from sensors and medical
devices and then transforms them into health status. A
health status S
i
=
{
s
1
, s
2
, ..., s
n
}
consists of heteroge-
neous simple medical states (e.g., hypoglycemia, hy-
perkalemia), where a simple medical state, say s
i
, pro-
vides an overview of an event occurred in a specific
organ of the body. When identifying a health status,
this module records it in the health status database and
notifies the multi-engine inference module.
The third level refers to the data processing anal-
ysis module part of RSS. This module collects health
records from the central node and performs to them
an advanced analysis to provide data showing the pro-
gression of the patient’s health status. It also allows
assisting physicians in validating received decisions.
Health Databases. Three types are distinguished:
Local Database: it is integrated in the architec-
ture of sensors and medical devices in the form of
nonvolatile memory. It only stores recent sensory and
acting data, due to its limited memory space.
Health Status Database: it is part of the central
node architecture allowing the storage of health sta-
tus records. Each time the data processing and analy-
sis module of the central node identifies a new health
status S
i
, it records it in the health status database, to-
gether with a time stamp, say t
i
, which is the instant
of the identification of S
i
. Therefore, a health status
record, say H
i
, takes the form: H
i
= (S
i
, t
i
). Due to the
limited memory space of the health status database,
the latter selects health records showing an old time
stamp and overwrite them to store recent records.
Remote Health Database: it is integrated in the
RSS architecture to store the health records processed
by the data processing and analysis module part of the
RSS. It ensures a long-term storage of data.
Multi-engine Inference. This module is part of the
central node architecture. It ensures the execution of
the forward and backward reasoning. Forward rea-
soning allows the early detection of critical health sta-
tus. It starts from a current health status, which is
identified by the data processing and analysis mod-
ule, and uses the libraries of rules and hypothesizes to
predict health status that could occur. Backward rea-
soning enables the provision of medical explanations
of an occurred critical health situation. It starts from a
detected critical health status and infers rules to gen-
erate plausible medical scenarios. A description of
the reasoning methods will be provided in the sequel.
Knowledge Base It is integrated in the central node
architecture. It includes three libraries namely, hy-
pothesizes, medical rules, and decision rules. The hy-
pothesizes and the inference rules of these libraries
are built based on the expertise of physicians and re-
trieved from the RSS. They are crucial for the well
functioning of the multi-engine inference module,
since they allow it to execute the reasoning methods.
A Smart Healthcare: Methods based on WBAN and Multi-engine Artificial Intelligence
187
^ĞŶƐŽƌLJ
ĚĂƚĂ
<ŶŽǁůĞĚŐĞĂƐĞ
džƉĞƌƚŝƐĞ
ĞĐŝƐŝŽŶƐ
ĂŶĚĂůĞƌƚƐ
ZƵůĞƐ
ŚLJƉŽƚŚĞƐŝƐ
DƵůƚŝͲŶŐŝŶĞ
/ŶĨĞƌĞŶĐĞ
ĂƚĂ
ƉƌŽĐĞƐƐŝŶŐ
ĂŶĚĂŶĂůLJƐŝƐ
^ĞŶƐŽƌLJ
ĚĂƚĂ
dŚĞƌĂƉŝĞƐ
ZĞƐƵůƚƐ
ƐƚŽƌĂŐĞ
,ĞĂůƚŚ
ƐƚĂƚƵƐĚĂƚĂ
ĞĐŝƐŝŽŶƐ
ĞĐŝƐŝŽŶƐ
ĂŶĚĂůĞƌƚƐ
YƵĞƌŝĞƐͬZĞƐƉŽŶƐĞƐ
ŽĨƌĞĂůͲƚŝŵĞƐĞŶƐŽƌLJĚĂƚĂ
tEĐĞŶƚƌĂůŶŽĚĞ
ZĞŵŽƚĞƐƵƉĞƌǀŝƐŝŽŶƐLJƐƚĞŵ
,ĞĂůƐƚĂƚƵƐ
ΘƐĞŶƐŽƌLJ
ĚĂƚĂ
DƵůƚŝĚŝƐĐŝƉůŝŶĂƌLJWŚLJƐŝĐŝĂŶƐ
WŚLJƐŝĐŝĂŶƐĞdžƉĞƌƚŝƐĞ
YƵĞƌŝĞƐͬZĞƐƉŽŶƐĞƐŽĨƌĞĂůͲƚŝŵĞƐĞŶƐŽƌLJĚĂƚĂ
ĞĐŝƐŝŽŶƐĂŶĚĂůĞƌƚƐ
,ĞĂůƚŚƐƚĂƚƵƐ
ĚĂƚĂ
WŚLJƐŝĐŝĂŶƐ
ĞdžƉĞƌƚŝƐĞ
ŽŵŵƵŶŝĐĂƚŝŽŶEĞƚǁŽƌŬƐ/ŶƚĞƌĨĂĐĞ
WŚLJƐŝĐŝĂŶƐ/ŶƚĞƌĨĂĐĞ
ZĞŵŽƚĞ
ĚĂƚĂďĂƐĞ
EŽƚŝĨŝĐĂƚŝŽŶƐ
DĞĚŝĐĂů
džƉůĂŶĂƚŝŽŶ
YƵĞƌŝĞƐͬZĞƐƉŽŶƐĞƐŽĨ
ŵĞĚŝĐĂůĞdžƉůĂŶĂƚŝŽŶƐ
YƵĞƌŝĞƐͬZĞƐƉŽŶƐĞƐŽĨŵĞĚŝĐĂůĞdžƉůĂŶĂƚŝŽŶƐ
ĂƚĂƉƌŽĐĞƐƐŝŶŐ
ĂŶĚĂŶĂůLJƐŝƐ
tE/ŶƚĞƌĨĂĐĞ
ĂƚĂ
ƉƌŽĐĞƐƐŝŶŐ
ĂŶĚĂŶĂůLJƐŝƐ
^ĞŶƐŝŶŐ
/ŶƚĞƌĨ ĂĐĞ
tEƐĞŶƐŽƌŶŽĚĞ
/ŶƚĞƌĨ ĂĐĞ
tEŵĞĚŝĐĂůĚĞǀŝĐĞ
^ĞŶƐŽƌLJĚĂƚĂ
ĂƚĂ
ƉƌŽĐĞƐƐŝŶŐ
ĂŶĚĂŶĂůLJƐŝƐ
^ĞŶƐŝŶŐ
ĐƚŝŶŐ
ĞĐŝƐŝŽŶƐ
dŚĞƌĂƉŝĞƐ
>ŽĐĂů
ĚĂƚĂďĂƐĞ
>ŽĐĂů
ĚĂƚĂďĂƐĞ
,ĞĂůƚŚƐƚĂƚƵƐ
ĚĂƚĂďĂƐĞ
Figure 1: Healthcare system architecture.
4 MULTI-ENGINE ARTIFICIAL
INTELLIGENCE
In this section, we detail the AI implementation in the
proposed WBAN based healthcare system.
4.1 Hypothesis and Inference Rules
In this subsection, we model hypothesizes and infer-
ence rules (medical and decision rules) through the
use of heterogeneous simple medical states. Two
types of simple medical states can be distinguished: a)
observable state (e.g., ventricular arrhythmia), which
refers to a state that can be evaluated by senors or by
medical devices; and b) unobservable state (e.g., in-
tracellular Ca
2+
), which cannot be measured neither
by senors nor medical devices. Unobservable states
are identified based on the physicians expertise.
Hypothesizes: Some diseases could contribute to
the occurrence of specific medical states. This infor-
mation can be modeled through hypothesizes. An hy-
pothesis (Ht) takes the following form: CD
High risk o f
→
S, where CD refers to a Chronic Disease and S is
a conjunction and/or disjunction of simple medical
states. Such hypothesis means that a patient who ex-
hibits CD is highly vulnerable to the occurrence of S.
Medical Rules: A Medical Rule (MR) is modeled
as follows: S →
T
S
0
, where S (as well as S
0
) repre-
sents a conjunction and/or disjunction of simple med-
ical states. Such a rule means that the occurrence of S
leads to the occurrence of S
0
, within a time period T .
Decision Rules: As discussed previously, our
healthcare system allows generating decisive deci-
sions to rescue a patient when detecting a critical
health status. To do so, a set of decisions rules are
used. A Decision Rule (DR) is modeled as: S → D,
where S represents a conjunction and/or disjunction of
medical states and D represents a conjunction and/or
disjunction of simple decisions. The meaning of such
a decision rule is when detecting S applies D. Two
types of simple decisions can be distinguished: a) de-
cisions sent to medical devices after being validating
to be implemented in the form of therapies; and b)
decisions sent to the RSS in the form of alerts.
4.2 Forward Chaining
Forward reasonning is implemeneted, to provide early
detection of anomalies. It starts from: a) a current pa-
tient’s health status, which is identified by the data
processing and analysis module part of the central
node; and b) a set of rules retrieved from the knowl-
edge base. When applying forward chaining, multi-
ple conclusions describing the subsequent health sta-
tus can be generated. The output of such a reasoning
is a tree, which includes: a root node representing the
current health status of the patient, say S
0
, and a set of
nodes representing the generated conclusions, which
refer to the predicted health status. Assuming that S
i
is a health status represented by a node in the tree un-
der construction. Starting from S
i
, rules are executed
in forward chaining as follows. For every inference
rule, which can be in the form S →
T
S
0
(or S → D)
within the knowledge base: if its premise S is part of
S
i
(i.e., S v S
i
), then a node, say S
j
(or D
j
, respec-
tively), which represents the consequence of the rule
S
0
, is appended to the tree (if it does not exist), and
then linked to the node S
i
. Such a process is repeated
until: none of the inference rules within the knowl-
edge base can be executed; or a new current health
status is identified. In this case, forward chaining is
restarted, to begin its reasoning from the new status.
Each time, a node representing decisions is cre-
BIODEVICES 2020 - 13th International Conference on Biomedical Electronics and Devices
188
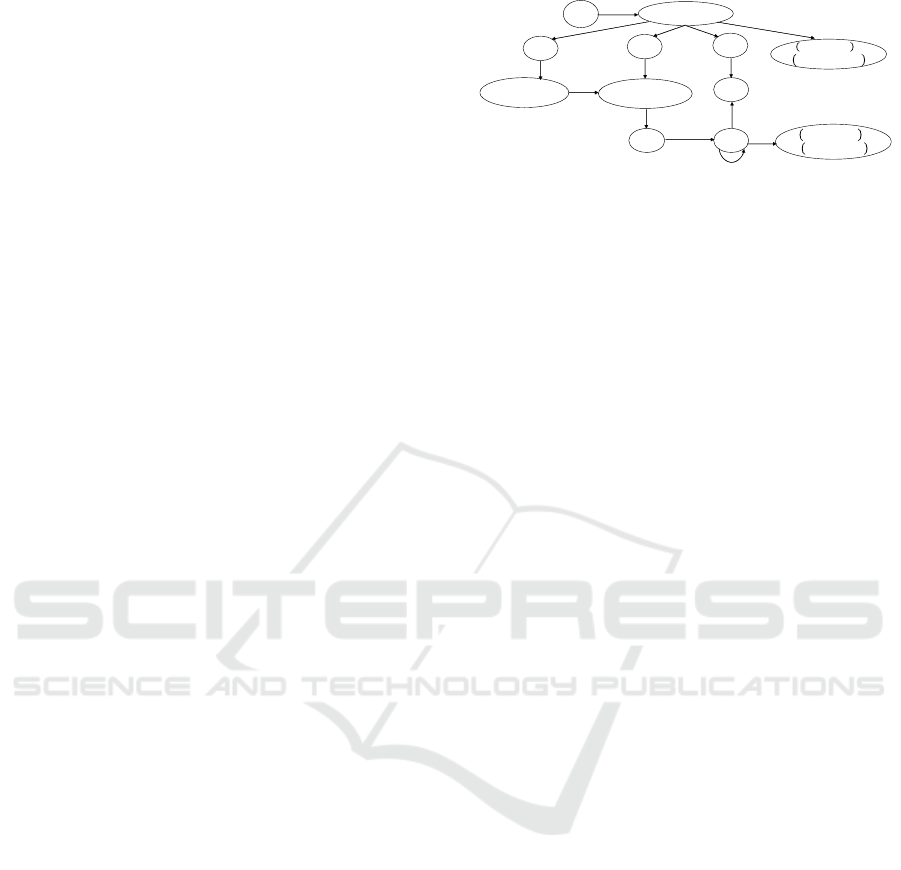
ated, the central node reacts by alerting the RSS. The
physicians can then validate received decisions, ad-
just them or generated new ones through the RSS.
According to the received RSS response, the central
nodes applies the decisions. These decisions allow
the WBAN to react by even preventing the anomaly
occurrence or by treating it when it occurs.
4.3 Backward Chaining
To provide a medical explanation of an occurred
health status, a backward reasoning is implemented.
Such a reasoning starts from a detected critical health
status, say S
c
, and executes inference rules in back-
ward chaining, to generate a set of plausible med-
ical scenarios. The generated scenarios satisfy the
health status progression over time, and take the form
of a tree, whose root node represents S
c
. We de-
note by H =
{
H
1
, H
2
, ..., H
i
, ..., H
c
}
the health records
showing the health status progression, which are re-
trieved from the health status database, where H
c
is
the record describing S
c
, and H
1
is the oldest record
in the database. The construction process of medical
scenarios is detailed as follows. Assuming that S
i
is
a node representing a health status in the tree under
construction. Starting from S
i
, a medical inference
rule (S →
T
S
0
) retrieved from the knowledge base can
be executed in backward only after verifying whether
the two following conditions are met: a) The conse-
quence S
0
in the rule is part of S
i
(S
0
v S
i
); and b) If
the premise S is observable (i.e., S is a conjunction
and/or disjunction of observable medical states), then
S should be part of the health status S
i−1
immediately
preceding the health status S
i
in the health records H
and occurring no earlier than the time period T (i.e.,
S v S
i−1
∧t
i
−t
i−1
≥ T ). If a rule is executed, a node
representing S
i−1
(if S is observable) or S (if S is un-
observable) is appended to the tree and linked to S
i
.
Inferring rules in backward is repeated until one
of these two conditions is met: none of the infer-
ence rules within the knowledge base can be exe-
cuted; or the oldest record H
1
in H has been included
in the tree. These two conditions allow ensuring the
termination of the chaining process. Indeed, back-
ward chaining is a finite process whose iteration num-
bers depend on the number of the inference rules in
the knowledge database and the number of collected
health records. Moreover, to prevent the occurrence
of loops, we propose to limit the execution of infer-
ence rules, whose conditions and premises only in-
clude unobservable medical states, to a threshold.
When the inferring process terminates, some hy-
pothesizes can be retrieved from the knowledge base
to explain the occurrence of some health status.
↓
,LJƉŽŐůLJĐĞŵŝĂ
↓+
↑
, ∧
,
,LJƉŽŬĂůĞŵŝĂ
Yd
ƉƌŽůŽ ŶŐĂƚŝŽŶ
↑
,
, ∧
,
,
ℎ
Figure 2: Tree of predicted health states.
5 CASE STUDY
In this section, we present a case study to exemplify
the functioning of the proposed system.
Architecture Description. We assume that the su-
pervised patient suffers from heart failure and dia-
betes. To this end, the WBAN should at least include:
a) Two medical devices: an Insulin Pump (InsP) to
supervise and control diabetes by regulating the blood
glucose level (bgl); and an Implantable Cardiac De-
fibrillator (ICD) to treat the heart failure disease by
reacting to the occurred arrhythmia. These two de-
vices are currently available in the market; b) A set
of biomedical sensors, which are available in the mar-
ket, including glucose, heart rate, ECG, and potas-
sium sensors; and c) A central node which integrates
in its knowledge base a set of hypothesis and infer-
ence rules to control diabetes and heart failure. We
assume that knowledge base includes at least: hypoth-
esis, medical rules and decision rules detailed in Ta-
bles 2, 3 and 4, respectively. Some of the medical
rules presented in Table 3 were inspired from the re-
search work developed in (Ellouze et al., 2017).
Forward Chaining for the Early Detection of Crit-
ical Health Status. At the instant t
i
, the data pro-
cessing and analysis module generates and stores
a health record H
i
(Table 5) in the health sta-
tus database, and notifies the multi-engine inference
module . Then, the latter executes the forward rea-
soning starting from H
i
.
Starting from H
i
, which showed the decreased
blood glucose level, the multi-engine inference mod-
ule retrieves the rule MR
1
and executes it in forward,
since its premises corresponds to s
4
part of H
i
. After
that, it retrieves the rules MR
2
, MR
3
, MR
4
and DR
1
,
and then executes them. By executing DR
1
, the multi-
engine inference module sends an alert to the RSS to
notify it about predicted anomaly and the decisions it
generates. After receiving decisions validation, it or-
ders the Insulin Pump to stop insulin injection. Later,
A Smart Healthcare: Methods based on WBAN and Multi-engine Artificial Intelligence
189
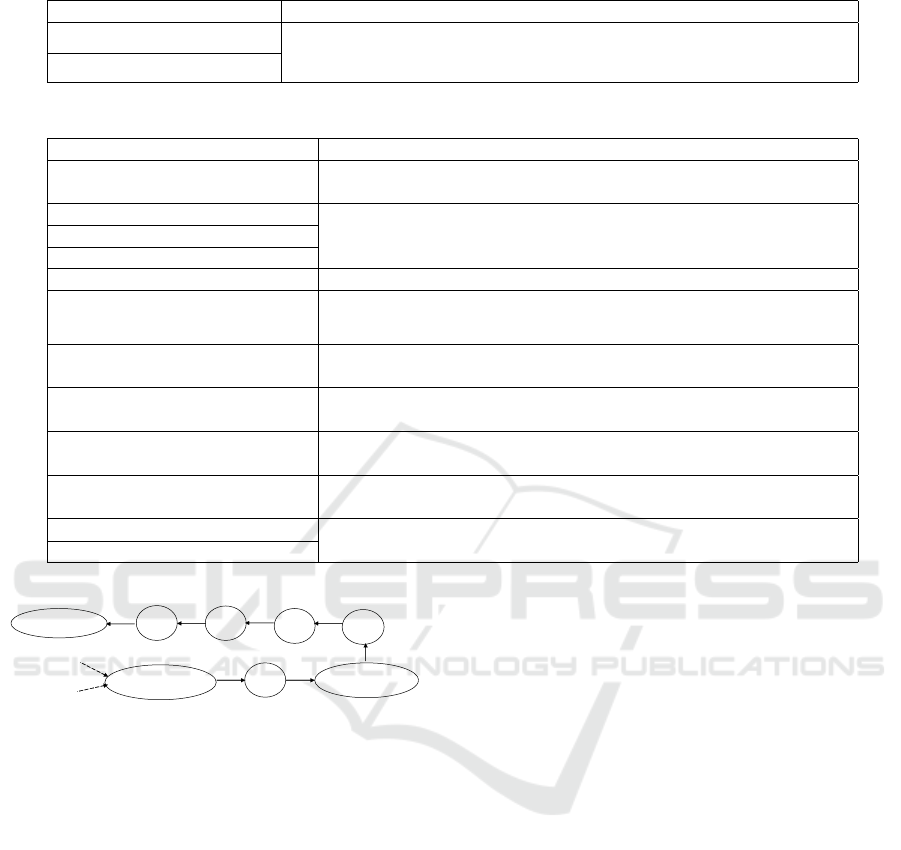
Table 2: Example of Hypothesizes.
Hypothesizes Descriptions
(Ht
1
) : DM
High risk o f
→ Hypo (Ht
1
) and (Ht
2
) state that a patient suffering from Diabetes Mellitus (DM)
or Type 1 Diabetes (T 1D) has a high risk of Hypoglycemia (Hypo).
(Ht
2
) : T 1D
High risk o f
→ Hypo
Table 3: Examples of heterogeneous medical rules.
Medical Rules Descriptions
(MR
1
) :& bgl →
T
Hypo
(MR
1
) states that the decrease of the blood glucose level (& bgl),
leads to Hypoglycemia (Hypo), within avperiod T.
(MR
2
) : Hypo →
T
& K
+
(MR
2
), (MR
3
) and (MR
4
) state that Hypo leads to the decrease of the
serum potassium concentration (& K
+
), the increase of Heart Rate
(% HR), or Brain Death (BD), respectively, within a period T .
(MR
3
) : Hypo →
T
% HR
(MR
4
) : Hypo →
T
BD
(MR
5
) :& K
+
→
T
Hypokalemia (MR
5
) states that & K
+
leads to Hypokalemia, within a period T .
(MR
6
) : Hypokalemia →
T
QT prolong
(MR
6
) states that the occurrence of Hypokalemia leads to the
prolongation of the QT interval (QT prolong) within a time period T .
(MR
7
) :% HR →
T
QT prolong
(MR
7
) states that an increased heart rate leads to the prolongation of
the QT interval within a given period of time T .
(MR
8
) : QT prolong →
T
% Ca
2+
(MR
8
) states that the occurrence of a QT prolongation induces the
increase of the intracellular Ca
2+
within a period of time of length T .
(MR
9
) :% Ca
2+
→
T
VA
(MR
9
) states that an increased intracellular Ca
2+
leads to the
occurrence of Ventricular Arrhythmia (VA), within a period T .
(MR
10
) : VA →
T
VA (MR
10
) states that the occurrence of a VA leads to the occurrence of
another VA within a period of time of length T .
(MR
11
) : VA →
T
Death (MR
11
) and (MR
12
) state that the occurrence of a fatal VA or BD,
respectively, induces the patient’s death within a time period T .(MR
12
) : BD →
T
Death
ƌĂĚLJĐĂƌĚŝĂ
ଵ
ଵ
ଵ
↑
ଶ
ା
ଽ
,LJƉŽŐůLJĐĞŵŝĂ
↑
Yd
ƉƌŽůŽŶŐĂƚŝŽŶ
ଷ
଼
dϭ
D
Figure 3: Medical explanation of Bradycardia occurrence.
it retrieves the rules MR
5
, MR
7
, and MR
12
and ex-
ecutes them, since their premises corresponds to the
consequences of the rules MR
2
, MR
3
and MR
4
, re-
ceptively. After the execution of MR
6
, MR
8
and MR
9
,
the rules MR
10
, MR
11
, and DR
2
are executed. To ap-
ply the decisions of DR
2
, the multi-engine inference
module sends a notification to the ICD and the RSS to
notify them about the occurrence of VA. The forward
reasoning results is depicted in Figure 2.
Medical Explanations of an Occurred Health
Anomaly. To exemplify the reasoning allowing the
provision of medical explanations of an occurred
anomaly, we use an example of health status progres-
sion from hypoglycemia to Bradycardia, which was
showed in (Reno et al., 2013). We assume that this
health progression occured within a supervised pa-
tient. When receiving an alert related to Bradycar-
dia detection from the central node (more precisely
from the multi-engine inference module), the physi-
cians request medical explanations through the deliv-
ery of a specific request. Upon request reception, the
multi-engine inference module collects health records
H =
{
H
1
, H
2
, H
3
, H
4
, H
5
, H
6
, H
7
}
from the health sta-
tus database, where H
7
is the record showing Brady-
cardia, and H
1
is the oldest record in the database.
Table 2 details the contents of collectd records. After
that, the multi-engine inference module executes the
backward reasoning. Starting from H
7
, it retrieves the
rule MR
10
from the knowledge database and executes
it in backward three times, since the consequences
and the premises of this rule correspond to Bradycar-
dia, PVCs, and ST, which are three types of VA oc-
curred in H
7
, H
6
,H
5
, and H
4
. Since ↑ Ca
2+
is an unob-
servable state that cannot observed in health records,
the inference module executes MR
9
in backward. Af-
ter that, it retrieves and executes MR
8
, as its premises
corresponds to a QT prolongation which occurred in
H
3
. Later, since an increased heart rate was occurred
in H
2
, the rule MR
7
is executed. Finally, the multi-
engine inference module executes MR
3
, since hypo-
glycemia, which is its premises, occurred in H
1
. To
explain hypoglycemia occurrence, hypothesizes Ht
1
and Ht
2
are used. Upon completing the construc-
tion of the medical explanations (Figure 3), the multi-
engine inference module sends it to the physicians as
a response to the received request.
BIODEVICES 2020 - 13th International Conference on Biomedical Electronics and Devices
190
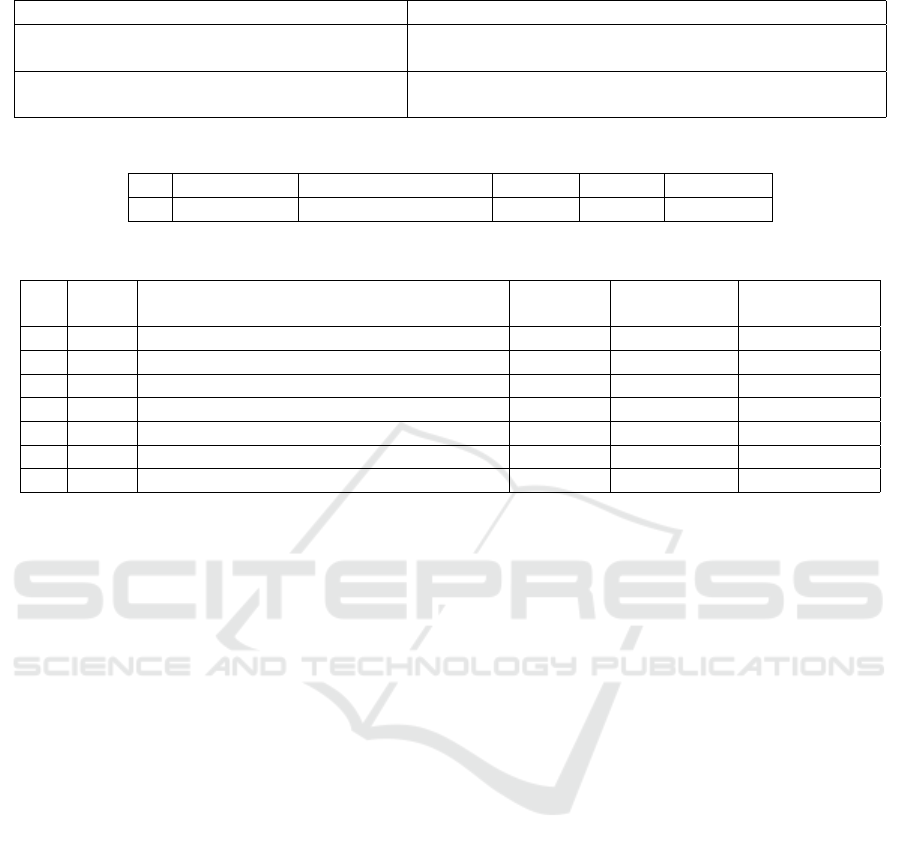
Table 4: Examples of decision rules.
Decision rules Descriptions
DR
1
: Hypo →
(Alert
Hypo
, RSS) ∧ (STOP, InsP)
When Hypoglycemia occurs, sends an alert to the RSS
and then orders Insulin Pump to stop insulin injection.
DR
2
: VA → (Alert
VA
, ICD) ∧ (Alert
VA
, RSS) When VA occurs, sends an alert to the ICD and to the
RSS to notify them about VA occurrence.
Table 5: Part of health records collected at the instant t
i
.
Time stamps s
1
(ECG) s
2
(HR) s
3
(QT) s
4
(bgl)
H
i
t
i
Normal sinus rhythm Normal Normal Decreased
Table 6: Part of health records collected after the instant t
7
.
Time
stamps
s
1
(ECG) s
2
(HR) s
3
(QT) s
4
(bgl)
H
1
t
1
Normal sinus rhythm Normal Normal Hypoglycemia
H
2
t
2
Normal sinus rhythm Increased Normal Hypoglycemia
H
3
t
3
Premature Atrial Contractions (PACs) Increased Prolongation Hypoglycemia
H
4
t
4
Premature Ventricular Contractions (PVCs) Increased Prolongation Hypoglycemia
H
5
t
5
Sinus Tachycardia (ST) Increased Prolongation Hypoglycemia
H
6
t
6
PVCs Increased Prolongation Hypoglycemia
H
7
t
7
Bradycardia Increased Prolongation Hypoglycemia
6 CONCLUSION
In this paper, we focused on the design of a Smart
Healthcare System carried by a WBAN which allows
managing multiple types of chronic diseases. The
proposed architecture of the healthcare system inte-
grates heterogeneous components to promote the su-
pervision of multiple types of diseases. It is also
equipped by a certain extent of intelligence related to
multiple discipline allowing it to appropriately diag-
nosis anomalies and react to them. In particular, a set
of inference rules and hypothesizes together with two
reasoning methods are used. A case study to exem-
plify the functioning of the proposed healthcare sys-
tem were also detailed.
REFERENCES
Alfian, G., Syafrudin, M., Ijaz, M. F., Syaekhoni, M. A.,
Fitriyani, N. L., and Rhee, J. (2018). A personalized
healthcare monitoring system for diabetic patients by
utilizing ble-based sensors and real-time data process-
ing. Sensors, 18(7):2183–2208.
AlMusallam, M. and Soudani, A. (2019). Embedded solu-
tion for atrial fibrillation detection using smart wire-
less body sensors. IEEE Sensors Journal, Early Ac-
cess.
Ellouze, N., Rekhis, S., Boudriga, N., and Allouche, M.
(2017). Cardiac implantable medical devices foren-
sics: Postmortem analysis of lethal attacks scenarios.
Digital Investigation, 21:11–30.
Reno, C. M., Daphna-Iken, D., Chen, Y. S., Vander-
Weele, J., Jethi, K., and Fisher, S. J. (2013). Severe
hypoglycemia-induced lethal cardiac arrhythmias are
mediated by sympathoadrenal activation. Diabetes,
62(10):3570–3581.
Rizwan, A., Zoha, A., Zhang, R., Ahmad, W., Arshad, K.,
Ali, N. A., Alomainy, A., Imran, M. A., and Ab-
basi, Q. H. (2018). A review on the role of nano-
communication in future healthcare systems: A big
data analytics perspective. IEEE Access, 6:41903 –
41920.
Sahoo, P. K., Thakkar, H. K., Lin, W.-Y., Chang, P.-C.,
and Lee, M.-Y. (2018). On the design of an efficient
cardiac health monitoring system through combined
analysis of ecg and scg signals. Sensors, 18(2):379–
407.
Teshome, A. K., Kibret, B., and Lai, D. T. H. (2018).
A review of implant communication technology in
WBAN: Progress and challenges. IEEE Reviews in
Biomedical Engineering, 12:88–99.
Valenza, G., Nardelli, M., Lanata, A., Gentili, C., Bertschy,
G., Kosel, M., and Scilingo, E. P. (2016). Predicting
mood changes in bipolar disorder through heartbeat
nonlinear dynamics. IEEE Journal of Biomedical and
Health Informatics, 20(4):1034–1043.
A Smart Healthcare: Methods based on WBAN and Multi-engine Artificial Intelligence
191
