
A Framework for System-level Health Data Sharing
Mana Azarm
1
, Craig Kuziemsky
2
and Liam Peyton
1,*
1
Faculty of Engineering, University of Ottawa, 800 King Edward, Ottawa, Ontario, Canada
2
Office of Research Services, MacEwan University, 104 Avenue NW, Edmonton, Alberta, Canada
Keywords: System-level Health Data Sharing, Evaluation, Panel of Experts, Interoperability, Electronic Medical Record.
Abstract: Circle of care is the term that has been used to provide context for health data sharing that is allowed by
privacy regulation that occurs when a diverse team is collaborating to provide care to a patient. We introduce
the concept of system-level health data sharing to capture the totality of health data that exists for a patient in
a healthcare system across multiple health care organizations. MyPHR is a system-level health data-sharing
framework that guides any healthcare system to set up interoperable, patient-centred health data sharing. We
briefly introduce the components of MyPHR framework and then discuss its evaluation by a panel of experts
who reviewed a demonstration walkthrough of the interfaces and data sharing that the framework supports.
1 INTRODUCTION
Health data can be shared at three levels. First, it can
be shared within the boundaries of a single health care
organization (HCO). In this case, the HCO does not
interact with other HCOs so data is not shared outside
the HCO. Patients can be involved in their care
delivery through a HCO-specific portal that grants
access to their personal health data. We call this
single-HCO health data sharing (Azarm, Peyton,
Backman, & Kuziemsky, 2017).
Second, it can be shared within a group of HCOs
who agree to acquire and use a single system in order
to facilitate collaboration and data sharing. We call
this multi-HCO health data sharing. An example of
multi-HCO sharing is the TakeCare system (Cars, et
al., 2013) that a few hospitals in Stockholm use to
enable data, process, and contextual interoperability
(Kuziemsky, 2013) within this alliance. However, no
interaction is supported with HCOs outside of this
alliance.
Finally, at the third level there is HCO-
independent data sharing. Any HCO can share and
access health date through a medium that allows the
flow of data from and to the existing Electronic
Medical Record (EMR) systems. Although not as
successful as we would expect, Microsoft
HealthVault is an example of HCO-independent data
sharing. (Sunyaev, Kaletsch, & Krcmar, 2011).
*
https://engineering.uottawa.ca/people/peyton-liam
A framework for system-level health data sharing
offers the potential to support better patient-centred
care (Haux, 2006). A circle of care (Donga, Samavia,
& Topaloglou, 2015) refers to a patient and a team of
healthcare providers who are providing care to the
patient in order to address a common healthcare goal.
A system-level circle of care covers all healthcare
providers across an entire health system (Gaynor, Yu,
Andrus, Bradner, & Rawn, 2014) who are providing
care to a single patient to address multiple goals
without necessarily collaborating or being aware of
each other (Azarm, Backman, & Kuziemsky, 2019).
1.1 Interoperability
Interoperability can be defined as the ability to
exchange and use information across different
organizations, enabling cooperation between their
entities (Benson & Grieve, 2016). Three types of
healthcare interoperability have been defined: data,
process, and contextual (Kuziemsky, 2013). Data
interoperability refers to the syntactical level of data
and whether it is machine interpretable across different
systems. Process interoperability focuses on the system
users and the processes they engage in. Process
interoperability requires system users to be able to use
and interpret data across the various tasks of health care
delivery. Finally, contextual interoperability refers to
the political and social environment where the
514
Azarm, M., Kuziemsky, C. and Peyton, L.
A Framework for System-level Health Data Sharing.
DOI: 10.5220/0008986305140521
In Proceedings of the 13th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2020) - Volume 5: HEALTHINF, pages 514-521
ISBN: 978-989-758-398-8; ISSN: 2184-4305
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

healthcare providers operate and includes different
legislation and/or social norms that can help or hinder
the shared care provided to a patient when delivered
across different providers or settings.
1.2 Quadruple Aim
Berwick et al. introduced the Triple Aim framework
for improving the healthcare delivered to individuals
in a balanced manner. The triple aim- comprises three
principles: improving the individual experience of
care, improving the health of population, and
reducing per capital cost of care for population
(Berwick, Nolan, & Whittington, 2008). However,
the success of triple-aim principles is dependent on
effective healthcare organizations and healthcare
workforce (Sikka, Morath, & Leape, 2015).
Therefore, the quadruple aim framework emerged by
introducing a fourth principle of improving the
experience of providing care (Sikka, Morath, &
Leape, 2015). The fourth principle is about care of the
providers and enhancing the work life of providers to
address emerging issues such as physician burnout
(Bodenheimer & Sinsky, 2014). Through a
quantitative study, Quanjel et al. proved that how the
patient-perceived quality of care is improved by a
Primary Care Plus initiative in Netherlands. (Quanjel,
Spreeuwenberg, Struijs, & Baan, 2019).
1.3 Governance
Healthcare in Canada is legislated and funded by the
federal government and administered provincially
(Madore, 2005). Electronic health record (EHR)
governance models vary from country to country and
even from region to region. Various Scandinavian
countries, where health services are publicly funded,
have embarked on a successive path of regulating,
mandating and advancing use of electronic health
records. Their endeavours started in the 1990s to push
healthcare providers to deploy electronic health
record systems and continued until recent years when
they are moving towards the implementation of
national electronic health record systems. As an
example, Denmark published various national IT
strategies consisting of national action plans for
adoption of EHRs, pushing hospitals to employ HER
systems, and governing and harmonizing all EHR
systems in the country (Kierkegaard, 2015).
Although healthcare is delivered by the private
sector in the United States, the Health Information
Technology for Economic and Clinical Health Act
(HITECH) provisions of the American Reinvestment
and Recovery Act (ARRA) facilitated the adoption of
EHR systems by providing financial incentives for
those who succeed at digitizing their health data,
automation of their internal processes, and seamless
collaboration with other healthcare providers
(Marcotte, Kirtane, Lynn, & McKethan, 2014).
US hospitals embarked on a healthcare
automation journey from the 1960 with purchase of
mainframes to handle their administrative functions
(Collen & Ball, 2015). They continued purchasing
software to handle different business and admin
functions. In 1990s the hospitals were operating with
hospital information systems (HISs) and electronic
patient record (EPR) systems, when the
interoperability became an issue. With the new
vendors’ promise of better inter-organizational
interoperability, most hospitals could benefit from
exchange of information among their different
acquired software systems after 2010.
Multi-Hospital Information Systems (MHIS) -
systems serving three or more hospitals emerged in
late 1980s. They often entailed translation databases
and other technology to support the exchange of
information and forms across the organizations
involved (Collen & Ball, 2015). Meditech and Epic
are examples of EHR systems used worldwide.
2 MyPHR: A SYSTEM-LEVEL
HEALTH DATA SHARING
FRAMEWORK
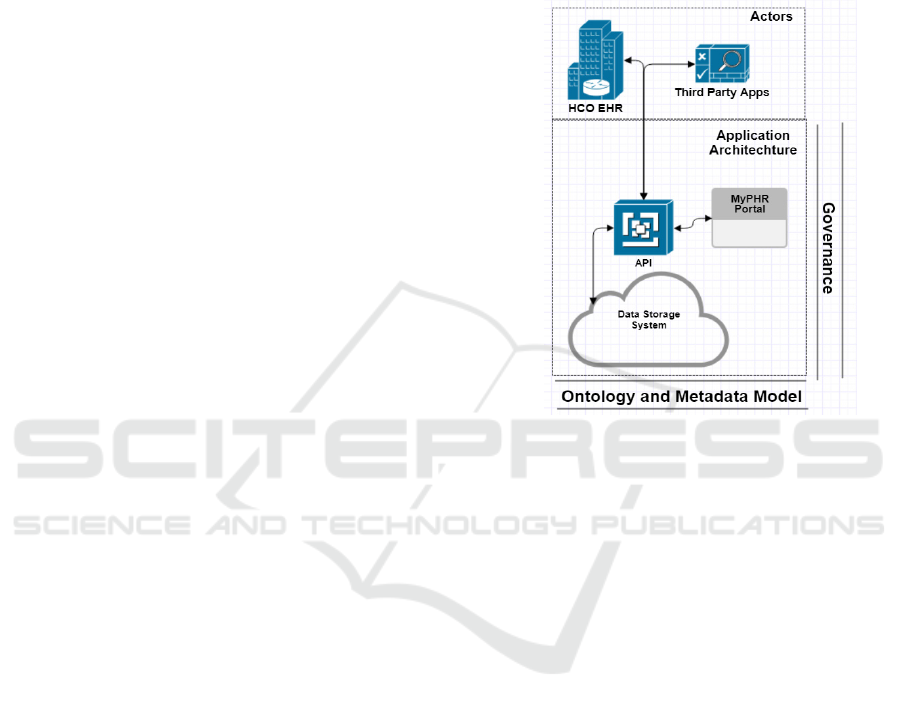
MyPHR is an application framework that guides a
healthcare system in setting up a system-level patient-
centered infrastructure so that they can have a
connected healthcare platform (Azarm, Backman, &
Kuziemsky, 2019). It has three components. First is
an information model that defines exactly what type
of information to share by everyone and in particular
has a simple definition of an episode so that all
stakeholders can understand what is shared without
being an expert. Second, it has an architecture that
defines a cloud hosted infrastructure like Gmail,
where the information can be stored and coordinated
amongst all people. And the final piece is the
governance model which defines who, how, and
when can access any piece of information in the
system, and who owns and maintains the system.
Healthcare systems in different political contexts
could use this framework to build a patient-centric
interoperable health information sharing platform.
MyPHR empowers patients to be more involved in
their care delivery, they have access to any piece of
information that’s shared on this platform about them,
A Framework for System-level Health Data Sharing
515
they can add/edit some information, and they can
always audit who and where has accessed their
information.
2.1 Demonstration Walkthrough
In order to test our proposed MyPHR architecture we
developed a prototype of the MyPHR portal pages as
well as a RESTful API that helps collect and share the
data that’s formatted in accordance with our proposed
ontology. Although, our ontology is mainly expressed
in a relational and schema-binding annotation, our
prototype data is stored in a No-SQL database
(Google Firebase). This speaks to the scalability of
our ontology.
Our MyPHR prototype web portal and API
include methods to facilitate the Client actions such
as viewing care history, updating health profile
information, view active practitioners, etc. The
prototype has methods that send updates to pull a
patient’s records from our API, collect information
entered by patients, and send them to the API for
permanent storage in a cloud environment. The API
has methods to register a patient with a healthcare
provider (through registering an episode), retrieve a
patient’s care history, update a patient’s care record
and terminate a patient’s episode of care with a
healthcare provider.
3 METHODOLOGY
Our research follows the guidelines of Design
Science Research (DSR) (Gregor, Müller, & Seidel,
2013) where we aim at improving the personal health
care experience through developing Health
Information Systems artifacts (Baskerville, Baiyere,
Gregor, Hevner, & Rossi, 2019). DSR is very relevant
when it comes to developing information system
artifacts that are innovative and solve real-world
problems (Hevner & Chatterjee, 2015). Our artifacts
include an architectural framework, web portal, API,
governance principles, and an ontology. Moreover,
through a literature review, we defined a customized
set of evaluation criteria for system-level healthcare
data sharing systems.
As per DSR guidelines, the project should start
with the specification of a problem/opportunity
(Baskerville, Baiyere, Gregor, Hevner, & Rossi,
2019). Therefore, through a Systematic Literature
Review (SLR) we aimed to identify the gaps in the
collaborative health care especially in Ontario, with
the possibility of finding a platform-independent
solution for interoperability (Azarm, Kuziemsky, &
Peyton, 2015). This step was achieved by studying
the current body of knowledge (Gregor, Müller, &
Seidel, 2013). At the end of the first iteration, we
proposed an architecture, defined a set of attributes
(minimum dataset) that flows through the proposed
architecture, and designed a web portal and an
underlying REST-full API.
Figure 1: MyPHR High Level Architecture.
In our second iteration of DSR, we honed in on
the idea of an ontology, and how we can make our
minimum data set more streamlined. Our ontology
was developed using an ontology development
methodology (Noy & McGuinness, 2001), and we
benchmarked HL7 FHIR (Azarm & Peyton, 2018).
Based upon Noy’s ontology development guidelines,
our benchmarking of the FHIR was to conform with
a popular health data standardization entity.
The third iteration was conducted to address
regulation, security and authorization concerns. We
focused on developing a set of data governance
principles in our third DSR iteration. We studied a
data sharing application that a group of researchers at
Elizabeth Bruyère hospital in Ottawa had developed
through a third party software company called NexJ.
We then studied their application (P2H) as a case with
regards to MyPHR framework to test our proposed
governance principles (Azarm, Backman, &
Kuziemsky, 2019). At the end of this iteration, we
came up with the concept of “system level circle of
care”.
Our fourth iteration involved prototyping the
architecture to pinpoint the actors and the interfaces.
We conducted a usability study through a Patient
Case Study that showcased our expectations from the
HEALTHINF 2020 - 13th International Conference on Health Informatics
516

prototype and how they were met. At the end of this
cycle, we conducted an evaluation with a
demonstration walkthrough reviewed by a panel of
experts (Agarwal, et al., 2016). We gathered a review
panel consisting of 5 experts in the healthcare
technology domain. This panel of experts included a
general practitioner, a nurse practitioner, two
healthcare technology directors, and a healthcare
management scholar and thought leader.
4 EVALUATION
4.1 Evaluation Criteria
We introduced a set of evaluation criteria to evaluate
frameworks and approaches in healthcare data
sharing. The evaluation criteria can be leveraged to
analyse any data sharing framework in the same
domain. We used the evaluation criteria to evaluate
our proposed application framework and compared it
against some related works.
The set of evaluation criteria identified in this
section were derived from:
1. Analysis of the related literature
2. Gap analysis of the current practices in hospital
and community care
3. Government regulations and industry norms and
concerns
4. Feedback from domain experts and practical
experience
5. Experiences we acquired while working through
our case studies.
We divided our evaluation criteria into 3 categories
depending on the domain and/or the source.
4.1.1 System-level Interoperability
System-level interoperability is our first set of
evaluation criteria where we discuss three aspects of
interoperability i.e. data, process, and context.
The main question in data interoperability is: Is
sharing of data available across various platforms?
With the patient’s care being transferred from one
HCO to another, there follows a need to transfer their
health data as fast as possible in a secure manner. The
systems that can enable their users to share data
regardless of their platform, will get a full score for
this criteria.
For process interoperability we ask: Are we able
to align and map processes across the boundaries of
organizations? When a system is not capable of
collaborating with other organizations and align their
processes with those of other healthcare providers,
they would get a NA; when the system has established
allegiance with a group of other healthcare systems
and they can all map their processes to each other,
they would be partially interoperable, hence a P is
assigned; Finally, when processes can be translated
and mapped within any organization, that system
would get an A.
Context interoperability investigates if a system
is capable of operating efficiently across different
political/legislative contexts? From this perspective,
a perfect system is capable of crossing various
political environments e.g. provinces or countries
without losing its cohesion and seamless integrity.
4.1.2 System-level Quality of Care
The Quadruple Aim framework that aims at
improving the healthcare experience for all
stakeholders is employed for this category of criteria.
The evaluation criteria in this category are also a
product of the Canadian Institute for Health
Information (CIHI) framework. Based on CIHI, a
care of quality is evidence-based, patient-centric,
timely, and safe (CIHI, 2011). The key to evidence-
based care is to be able to share previous experiments
and experiences. Below, we introduce the criteria in
this category.
Evidence-based: this metric comes from the
CIHI framework. It focuses on how easy it is to
support medical evidence or other processes across
different platforms? The perfect system supports
sharing of the evidence/process regardless of
platform type.
Right Level of Details: the fourth principle of the
quadruple aim framework is about improving the
experience of providing care. The amount of data we
gather in this day and age flood the healthcare
workers with enormous amount of information that
can leave them overwhelmed, and bear counter-
intuitive consequences. What can support many
healthcare workers is just the right amount of data at
the right time. Therefore, we will examine if the
framework under investigation can facilitate the
provision of just the right level of details in order to
support a healthcare worker in fulfilling their duties.
Patient-centric: this criterion crosses the two
frameworks of CIHI (patient-centric) and Quadruple
aim (patient’s care experience). It measures how
informed a patient is in their care delivery process.
However, it’s not only about the quantity of data, but
it’s also about the breadth of data, and the care
episodes and organizations. A perfect system would
enable the patients to access any piece of information
available on the data sharing platform.
A Framework for System-level Health Data Sharing
517
Timely: this criterion from CIHI framework
captures the essence of the two Quadruple Aim
principles of patient, and provider experience. If
required information is received in a timely manner,
this could have a positive impact on the experience of
the individuals on both ends of care delivery. It
assesses if system users (patients or providers) have
the means to autonomously access the information in
a timely manner. Here, the ideal system makes the
data available and accessible in real-time as they are
generated.
Cost: this criterion comes from the Quadruple
Aim criteria. It focuses on how the overall cost of
healthcare can be decreased. Therefore, the question
is if the system helps with any net savings. If the costs
of acquiring the system are less than the alternative
ways of solving the same problems, that health data
sharing system is regarded as successful.
Health: another Quadruple Aim criterion. Here
we talk about improving the health of the population.
Does the system under investigation help achieve this
goal in any way?
4.1.3 System-level Privacy and
Confidentiality
Within this category we introduce two criteria; one
for regulation compliance, and one for addressing
privacy concerns.
Regulations Compliant: in this section we
evaluate systems based on how complaint or
adaptable they are to health regulations. If a system
would not pass regulations without major
modifications, it is deemed as a failure.
Privacy: personal health information is
considered one of the most confidential type of
information. Therefore, it’s important that the system
we employ, keeps the integrity and confidentiality
requirements on the forefront of their specifications.
4.2 Panel of Experts Review
We gathered 5 experts to review a prototype of
MyPHR framework. In order to provide context for
the demo, we first gave an overview of MyPHR
framework and its three major components:
Ontology, Governance and architecture. Then, we
walked them through a demo of a MyPHR
framework-compliant prototype software application.
During the framework overview and demo
walkthrough there was much free-form discussion
and feedback. At the end of the session we asked the
experts to give us more structured feedback, using the
evaluation criteria we have set as the “objectives to
meet” for our research. For each criterion, we gave a
rubric that helped quantify the evaluation of the
criterion. The experts were also encouraged to give us
comments and free form feedback, either specific to
a criterion, or not.
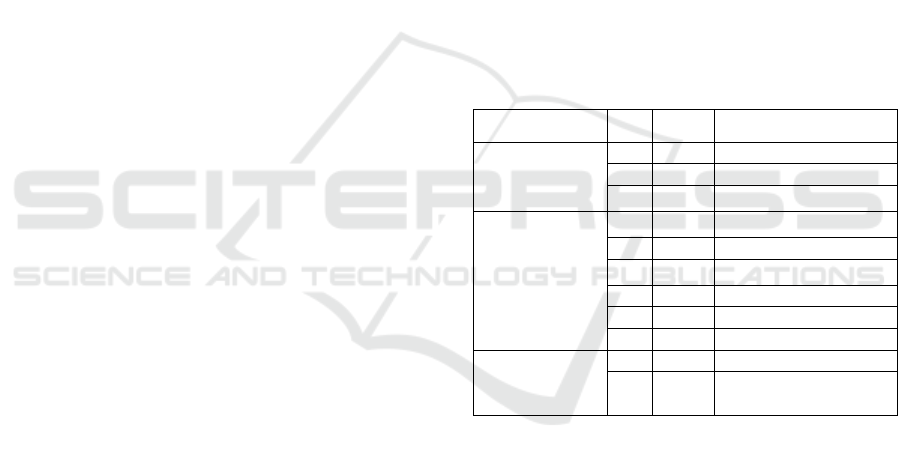
4.2.1 Evaluation Rubric
Our evaluation rubric lists the evaluation criteria that
we laid out in section 4.1. We asked each expert to
rate our framework against our evaluation criteria
using a 5-point scale with the following values: Not
Satisfactory, Below Average, Average, Above
Average, or Satisfactory. To quantify our score
levels, we added a numerical scale (1-10) to our 5-
point scale of “Non-Satisfactory” to “Satisfactory”
levels. For example, a non-satisfactory evaluation of
a criterion could bear a numeric score of 1 or 2. We
also invited our experts to add any additional
comment in a free text and descriptive format. Our
evaluation rubric is shown in Table 1.
Table 1: Evaluation rubric.
Domain ID Weight Criteria
System-Level
Interoperability
I1 5 Data interoperability
I2 3 Process interoperability
I3 1 Context interoperability
System-Level
Quality of Care
Q1 1 Evidence-based
Q2 1 Right level of details
Q3 5 Patient-centric
Q4 5 Timely
Q5 1 Cost
Q6 1 Health
System-Level
Privacy and
Confidentiality
P1 1 Privacy
P2 5 Regulations compliance
4.2.2 Expert Feedback
During the sessions and through written comments,
we received some valuable insights and suggestions
that we have summarized below:
1. There shall be a patient identification and
matching logic. In Ontario, OHIP number does
not include individuals from RCMP and the
military.
2. Experts were interested in seeing a place for
smart devices in our proposed architecture.
3. Experts were interested in seeing how
appointments fit into the Episode concept e.g. a
list for appointments that is separate from the list
of episodes.
4. Experts were interested in a different
presentation format for the health data. For
HEALTHINF 2020 - 13th International Conference on Health Informatics
518

example: Diagnoses in reverse chronological,
and with a short label/comment.
5. Caregiver information was not clear about
connotations such as power of attorney for
personal care; hierarchy of substitute decision
makers; primary care giver.
6. The data points that should be editable by the
Clients? e.g. diet, advanced directives.
7. The information presented on the prototype
portal such as dates did not always follow a
consistent format.
8. Experts were interested to see practitioners’
qualification/speciality level of primary
physician on the prototype portal.
9. Experts were looking for more clarification
around service language as it can be assumed
any of the following: preferred service
language, mother tongue, actual language of
service.
10. Experts were not certain where user comments
can be placed.
11. Experts needed more clarity on meta-data.
12. The governance principles around HICs’
visibility on patient data was discussed. Experts
suggested to allow HICs’ access to patient data
to be beyond the active status of their episodes.
13. Experts identified an opportunity for new and
improved functionalities that can be added to
HCO electronic record systems. They thought
the framework as presented likely encounters
few technical hurdles, and provides for a
platform agnostic approach for sharing data
across multiple healthcare information systems.
14. The experts suggested that while the framework
and API approach would provide a near real-
time solution, the various HCOs may determine
to interact with the data in either a batch mode
or the preferred triggers to flow information
across. Each HCO may also make
determinations as to which episodes of care
would be included in the information flow,
potentially causing inconsistency in the
frameworks picture of the patient/client.
15. The adoption barriers identified by experts
were: Financial barriers for HCOs to invest in
building the interfaces and rules to submit data
through to the API; Political barriers in
determining where the primary Health
Authority role, at a patient-centric service,
should lie; Perception of the shared data and
what it is providing, i.e. some HCOs will want
to increase the scope of what is shared, while
others may not be willing to participate; Privacy
controls may need to be enhanced, in that the
clients and/or HCOs will want to have some
control as to which episodes of care are visible
across all partners in the system, or just to some.
16. Experts also identified a few barriers to
implementation: Political barriers, where a
centralized Health Authority to host the
framework and centralized/consolidated data
needs to be determined. Within some regions,
the pendulum swings as to whether a centralized
or decentralized approach to a Health Authority
that would hold client level data, would be put
in place. HCOs, particularly individual family
physicians and Family Health Groups, may be
reluctant to participate, most likely out of cost.
The cost to update their systems to interface
with the API would be imposed to the individual
practices in many regions, if this would be a
mandated system to be used. To solve this, the
Health Authority may need to help fund vendors
to build interfaces, and thus help bring in the
smaller HCOs.
17. Some experts were not sure if the criterion “right
level of detail” is from patients point of view,
physicians, HCOs or the regulator.
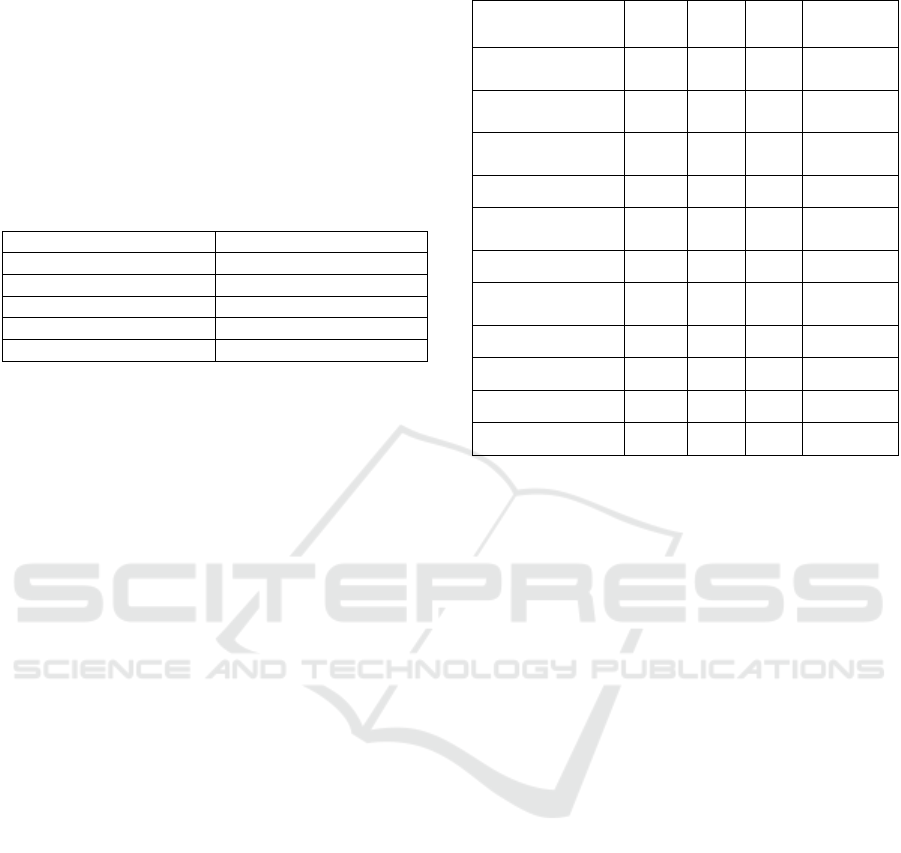
4.2.3 Evaluation Results
After the Panel of Expert Review Session, we
reviewed both the structured and unstructured
feedback. The unstructured feedback consisted of the
verbal comments made during the session (notes were
taken) and the written comments appended to the
structured feedback that was laid out in section 4.2.2.
We categorized the comments into 5 groups. In
the review session, we had presented 4 components to
the experts: the demo data, the look and feel of the
prototype application, the MyPHR framework, and
our proposed evaluation criteria. Naturally, we
wanted to identify and isolate the comments related
to each of the 4 aforementioned review session
components. Therefore, we created 4 categories of
usability (for prototype application), demo data,
framework, and criteria. Furthermore, we noticed that
some expert feedback bore some degree of
misunderstanding or communication problems.
Therefore, we added a fifth category that
encompasses the comments entailing a
misunderstanding of a notion.
1. Prototype Usability: Feedback on the prototype
application (look and feel and organization)
2. Demo data: Feedback on the demo data used in
the presentation
3. Framework: Feedback on the elements of
MyPHR framework
A Framework for System-level Health Data Sharing
519
4. Criteria: Feedback on the appropriateness,
relevance or poor definition, or
misunderstanding of the criteria we had
specified to use for evaluation
5. Misunderstanding: The comments that indicated
certain aspects of the framework overview or
demo were either not properly communicated or
not properly understood in terms of the context,
or objectives.
Table 2: Comment categories.
Category
Comment ID
Prototype Usability 7,8
Demo Data 3,4, 6,8,9,10
Framework 1,2,11,12,13,14,15,16
Criteria 17
Misunderstanding 5
Then, we analyzed the scores given to each
criterion by experts. As for the scores given, of all the
scores we received from the filled evaluation rubrics
(Table 1), the experts rated the prototypes 67% of the
times “above average”, 19% of the times “average”,
and 14% of the times “below average”.
When a criterion had a score variability (i.e.
difference between the highest score and the lowest
score given) of less than 4 among experts, we deemed
that criterion as having experts’ consensus, and when
there was 4 or more score variability, we deemed that
as divergent opinions about that criterion. We should
point out that when the score variability was between
3 and 5, we manually inspected the results to see
where the majority of the experts landed. As
summarized in Table 3, experts had consensus on 5
criteria and had divergent opinions on the other six.
Based on score averages, the experts scored MyPHR
average or above average on all criteria.
We can conclude from the evaluation results that
MyPHR appeared very strong on I1-Data
Interoperability, Q3-Patient Centric, Q4-Timely, and
P2-Regulations compliance, whereas I3-context
interoperability, and P1-privacy were not as strong.
Although our evaluation criteria touch on various
aspects of interoperable, patient-centric and
successful healthcare platforms, we did not put our
focus equally on all of them. We decided to
concentrate more on developing a patient-centric
framework that allows all healthcare stakeholders to
communicate their data in a timely and cost-efficient
manner. Therefore, not all our evaluation criteria have
the same weight for us. To address that issue we
created a three-scale numeric weight (1, 3, 5) based
on how influential they were in our research.
Table 3: Expert scores.
Criteria AVG Min Max Overall
Data
interoperability
7.9 6 9.5 consensus
Process
interoperability
6.5 4 8 divergent
Context
interoperability
5.0 4 6 consensus
Privacy 5.9 4 9.5 divergent
Regulations
compliance
8.9 8 9.5 consensus
Evidence-based 6.0 4 8 divergent
Right level of
details
6.6 4 8 divergent
Patient-centric 8.7 8 9.5 consensus
Timely 8.6 7 9.5 consensus
Cost 6.6 5 9.5 divergent
Health 6.6 2 8 divergent
5 CONCLUSIONS AND FUTURE
WORK
In this paper we evaluated a system-level patient-
centric health data sharing framework that we had
developed previously. One of the methods used for
this evaluation was a review by a panel of experts.
The review produced structured and unstructured data
that was analysed to improve our framework.
The reviewers also suggested features that can be
considered for the future work. Developing a
universal client matching algorithm and identification
system instead of using patient health card number
would perfectly fit in the next step agenda. Enabling
the flow of information from the personal smart
devices and the changes it would impose on our
proposed ontology is another good area for future
work. Furthermore, inclusion of richer metadata
would enable better patient-specific privacy and
security settings when it comes to setting proper and
access levels for different users. This is an area that
can be easily added to our existing ontology. Another
enhancement we may tap into is to open up HICs’
access to client information to beyond their active
status in the system-level circle of care, i.e. once a
healthcare provider takes on a client, they have
persistent access to that client’s information without
time constraints.
In the context of the structured review results, and
through factoring the weights into the scores we
HEALTHINF 2020 - 13th International Conference on Health Informatics
520

received from our experts, we came to a GPA of 70%
for all criteria considered. This figure tells us that our
proposed framework is viable, although there is a lot
of room for improvement. The proposed framework
is perceived to improve the current situation.
ACKNOWLEDGEMENTS
This research was funded by NSERC and OGS.
REFERENCES
Agarwal, S., LeFevre, A. E., Lee, J., L’Engle, K., Mehl, G.,
Sinha, C., & Labrique, A. (2016). Guidelines for
reporting of health interventions using mobile phones:
mobile health (mHealth) evidence reporting and
assessment (mERA) checklist. the bmj, 352-362.
Azarm, M., & Peyton, L. (2018). An Ontology for a Patient-
Centric Healthcare Interoperability Framework.
IEEE/ACM International Workshop on Software
Engineering in Healthcare Systems (SEHS).
Gothenburg, Sweden: IEEE Xplore.
Azarm, M., Backman, C., & Kuziemsky, C. (2019). System
Level Patient-Centered Data Sharing. 2019 IEEE/ACM
1st International Workshop on Software Engineering
for Healthcare (SEH) (pp. 45-48). Montreal: IEEE.
Azarm, M., Kuziemsky, C., & Peyton, L. (2015). A Review
of Cross Organizational Healthcare Data Sharing. The
5th International Conference on Current and Future
Trends of Information and Communication
Technologies in Healthcare (ICTH-2015). 63, pp. 425-
432. Berlin: Elsevier.
Azarm, M., Peyton, L., Backman, C., & Kuziemsky, C.
(2017). Breaking the Healthcare Interoperability
Barrier by Empowering and Engaging Actors in the
Healthcare System. Procedia Computer Science. 113,
pp. 326-333. Lund, Sweden: Elsevier.
Baskerville, R., Baiyere, A., Gregor, S., Hevner, A., &
Rossi, M. (2019). Design Science Research
Contributions: Finding a Balance between Artifact and
Theory. Journal of the Association for Information
Systems, 358-376.
Benson, T., & Grieve, G. (2016). Principles of Health
Interoperability SNOMED CT, HL7 and FHIR (Third
ed.). (T. Benson, Ed.) London, UK: Springer.
Berwick, D. M., Nolan, T. W., & Whittington, J. (2008).
The Triple Aim: Care, Health, And Cost. Health
Affairs, 27(3).
Bodenheimer, T., & Sinsky, C. (2014). From triple to
quadruple aim: care of the patient requires care of the
provider. Ann Fam Med, 573-576.
Cars, T., Wettermark, B., Malmstrom, R., Ekeving, G.,
Vikstrom, B., Bergman, U., ... Gustafsson, L. (2013).
Extraction of Electronic Health Record Data in a
Hospital Setting: Comparison of Automatic and Semi-
Automatic Methods Using Anti-TNF Therapy as
Model. Basic & Clinical Pharmacology & Toxicology,
112, 329-400.
CIHI. (2011). Learning From the Best: Benchmarking
Canada’s Health System. Canadian Institute for Health
Information.
Collen, M. F., & Ball, M. J. (2015). The History of Medical
Informatics in the United States. Baltimore , MD , USA:
Springer-Verlag London.
Donga, X., Samavia, R., & Topaloglou, T. (2015). COC:
An Ontology for Capturing Semantics of Circle of Care.
Procedia Computer Science. 63, pp. 589-594. Elsevier.
Gaynor, M., Yu, F., Andrus, C. H., Bradner, S., & Rawn, J.
(2014, March). A general frame work for
interoperability with applications to health care. Health
PolicyandTechnology, 3(1), 3-12.
Gregor, S., Müller, O., & Seidel, S. (2013). Reflection,
abstraction, and theorizing in design and development
research. Proceedings of European Conference on
Information Systems, (p. 74). Utrecht, The Netherlands:
ECIS.
Haux, R. (2006). Health information systems : past, present,
future. nternational journal of medical informatics ,
75(3), 268-281.
Hevner, A. R., & Chatterjee, S. (2015). Design Science
Research in Information Systems. Association for
Information Systems (AIS).
Kierkegaard, P. (2015). Governance structures impact on
eHealth. Health Policy and Technology, 4, 39-46.
Kuziemsky, C. (2013). Interoperability, A Multi-Tiered
Perspective on Healthcare. In M. Ángel Sicilia, & P.
Balazote, Interoperability in Healthcare Information
Systems Standards Management and Technology. IGI
Global.
Madore, O. (2005, May 17). Parliament of Canada.
Retrieved February 11, 2017, from http://www.lop.parl.
gc.ca/content/lop/researchpublications/944-e.pdf:
http://www.lop.parl.gc.ca/content/lop/researchpublicat
ions/944-e.pdf
Marcotte, L., Kirtane, J., Lynn, J., & McKethan, A. (2014).
Integrating Health Information Technology to Achieve
Seamless Care Transitions. Journal of Patient Safety.
Noy, N. F., & McGuinness, D. L. (2001). Ontology
Development 101: A Guide to Creating Your First
Ontology. Stanford University, Knowledge Systems
Laboratory Tech report KSL-01-05. Palo Alto: Stanford
University.
Quanjel, T., Spreeuwenberg, M. D., Struijs, J. N., & Baan,
C. A. (2019, May). Substituting hospital-based
outpatient cardiology care: The impact on quality,
health and costs. Plus One, 14(5).
Sikka, R., Morath, J. M., & Leape, L. (2015). The
Quadruple Aim: care, health, cost, and meaning in
work. The BMJ, 608-610.
Sunyaev, A., Kaletsch, A., & Krcmar, H. (2011).
Comparative Evaluation of Google Health API vs.
Microsoft Healthvault API. Proceedings of the Third
International Conference on Health Informatics
(HealthInf 2010) (pp. 195-201). Valencia, Spain:
SSRN.
A Framework for System-level Health Data Sharing
521
