
Applying Agile Principles to Collaborative Healthcare Teams
Rubina Lakhani, Benjamin Eze and Liam Peyton
Faculty of Engineering, University of Ottawa, 800 King Edward Street, Ottawa, Canada
Keywords: Collaborative Healthcare Teams, Performance Management, Agile, Treatment Plan, Dashboard, ADHD.
Abstract: In this paper, we demonstrate how agile principles can be applied to collaborative healthcare teams. We
provide a generic Agile Healthcare Process, and two associated artifacts, the Agile Treatment Plan, and the
Agile Dashboard using a theoretical Attention Deficit Hyperactivity Disorder case study. The paper describes
these in detail and shows how healthcare teams can measure the success of their collaboration through
actionable metrics. Our hypothesis is that providing a process in which collaboration factors are identified
and associated with specific performance metrics that can be collected and analyzed, can improve
coordination of collaborative healthcare teams. We demonstrate how agile methodology can be applied to
manage the treatment of chronic conditions such as ADHD. Our approach anchors around the Agile Treatment
Plan and the Agile Dashboard. We show how the KPIs associated with these artifacts can be used to quantify
healthcare team collaboration and performance.
1 INTRODUCTION
Medical errors – from poor communication,
misdiagnosis, poor judgement, and inadequate skills
- account for 30% of patient deaths in the US
(Anderson & Abrahamson, 2017; Makary & Daniel,
2016). Medical errors can be systematic or linked to
individual care providers, but approximately 75% of
these errors are the result of teamwork failures (Mayo
& Woolley, 2016). While most medical errors are
unintended, the negative impact on quality of care can
be very significant and sometimes result in the death
of the patient.
Chronic health conditions like Attention Deficit
Hyperactivity Disorder (ADHD) pose a huge
challenge since managing the condition requires
collaboration and coordination between healthcare
professionals, school authorities, community support
and caregivers (Carpentier, 2012). These long-term
chronic conditions are most susceptible to medical
errors because of the number of different individuals
involved in patient care. Therefore, the high incidence
of chronic health conditions and the associated
benefits of team-based care delivery is one of the
major drivers for collaboration (Kuziemsky, 2016).
Collaboration can be especially challenging. In
addition to clinical domain complexity, care team
members tend to have very different roles,
perspectives and training (family health, mental
health, community health, and therapies) (Ezziane et
al., 2012). Additionally, healthcare policy and
regulation pose challenges to team collaboration. In
general, healthcare collaboration is complex, which
can make coordination, cooperation and
communication difficult. These factors make
measuring teamwork performance particularly
challenging (Sicotte, D’amour, & Moreault, 2002).
In this paper, we discuss performance
management for collaborative healthcare teams by
using a theoretical ADHD case study. The case study
is developed using empirical observation, theoretical
research and consultation with experts. We establish
the advantages of treating healthcare processes as
agile processes guided by an agile treatment plan and
dashboard that is managed across the healthcare team,
and 2) show that healthcare teams can measure the
success of their collaboration through actionable
metrics.
It is our hypothesis that if we provide a framework
in which a holistic set of collaboration factors and an
associated set of specific performance metrics is
collected, analysed and communicated effectively,
then, care teams will be more effective in
coordinating care. This should result in outcome
improvements to quality of care that will exceed those
from traditional practice.
506
Lakhani, R., Eze, B. and Peyton, L.
Applying Agile Principles to Collaborative Healthcare Teams.
DOI: 10.5220/0008984105060513
In Proceedings of the 13th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2020) - Volume 5: HEALTHINF, pages 506-513
ISBN: 978-989-758-398-8; ISSN: 2184-4305
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
2 BACKGROUND
Managing chronic disease conditions is complex, long-
term, and requires multifaceted responses from multi-
disciplinary healthcare teams comprised of doctors,
nurses, social workers, physiotherapists and other
health professionals that provide collective
intelligence, over multiple domains for the purposes of
diagnosis and treatment (Nolte, Knai, & McKee,
2008). While team collaboration has the potential to
improve patient care, in many instances it can have the
opposite effect if the teams do not collaborate
effectively (Havyer et al., 2014; Zwarenstein,
Goldman, & Reeves, 2009). Further, there is a great
focus on integrating clinical workflows, with less
emphasis placed on team-based collaboration (Eikey,
Reddy, & Kuziemsky, 2015).
(Eikey et al., 2015) develop a Collaboration Space
Model that is based on four main concepts:
1) Technology - used by care providers,
2) Context – refers to the collaborating teams,
3) Processes – refers to collaborative processes,
workflows, communication, and information
exchange, and
4) Outcomes – represent the goals for achieving the
desired patient outcomes. While collaboration must be
designed to incorporate these four concepts, there is the
gap to ensure that outcomes are in line with the desired
patient outcomes.
Agile methodology encompasses well-defined
methods for organizing collaborative work processes
and for measuring performance in software
engineering and other fields. Agile methodology is
heavily used in managing software development
projects and teams (Duka, 2013). It involves breaking
up development activities into vertical slices that allow
for the incremental release of software to the customer
at the end of each sprint (Agile Methodology, 2008;
Upadrista, 2015). The strength of agile methodology is
that it enables continuous, measurable feedback that
gets communicated back to the teams, so priorities and
goals are constantly adjusted to be in congruence with
the customer needs.
Some early results in the literature show the
potential benefits of applying this approach to the
healthcare domain (Mayo & Woolley, 2016)
(Williams, 2016). Applying agile methodology
principles to collaborating healthcare teams means that
patient outcomes are continuously evaluated by the
collaborating teams. Feedback from the patient and
caregivers is received in a timely manner by the teams
so medical errors are minimized while the feedback
from the patient results in tuning treatment plans to
meet the desired patient outcomes. Based on the work
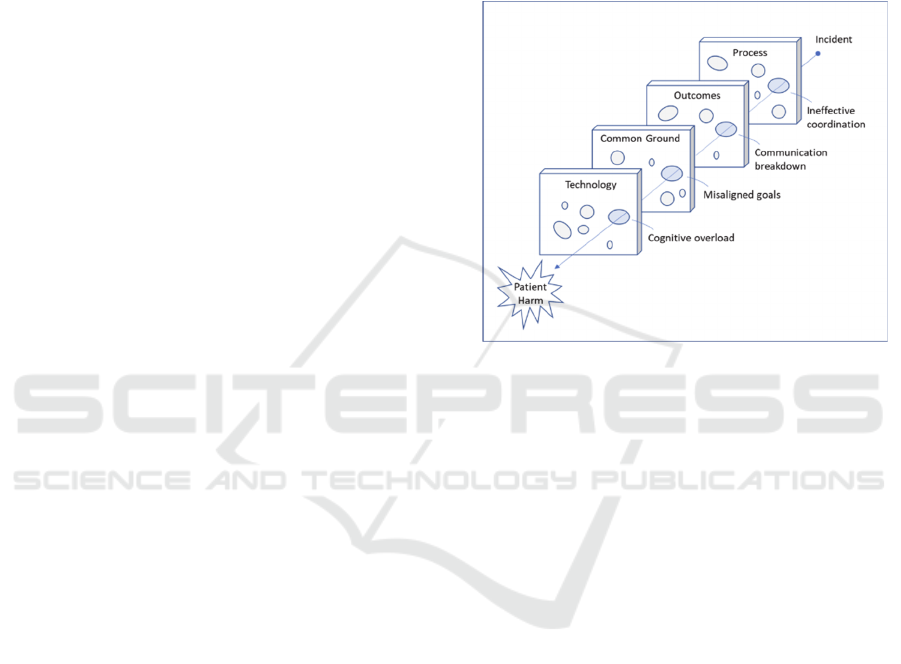
of James Reason (Reason, 2000), Figure 1, shows that
each of the collaboration space model concepts is
affected by various issues like cognitive overloads,
misaligned goals, communication breakdown, and
ineffective coordination. These dark (active) holes
constitute negative incidents or errors, while the others
are latent. When several active holes line up, patient
harm occurs through a cascade of these errors.
Figure 1: Swiss Cheese Diagram of Collaboration Failure
(Reason, 2000).
A key component of agile methodology is the
ability to provide measurable outcomes. This requires
collaborating healthcare teams to define metrics for
measuring success in forms of Key Performance
Indicators (KPIs)
In order to monitor care processes, data must be
collected and reported to measure how well they are
meeting quality of care goals dictated by
organizational, governmental, and accreditation
regulations. These measures need to be presented and
reported to care teams in a simple format such as a
dashboard or report that assists them in decision
making (Azvine, Nauck, & Ho, 2003).
Shared outcomes and goals for patient health are
measured and evaluated in a methodical manner and
inform the accountability and efficiency of the team.
The agile mindset encompasses values, goals and
attitudes for the benefit of the customer, as opposed to
the benefit of the bottom line (Denning, 2016). It
involves continuous improvement and transparency on
an ongoing and daily basis. The communication is
egalitarian, open and conversational and occurs
independently of hierarchy or position within the
organization. The workplace, including the physical
workspace, is open and lends itself to collaboration
(Denning, 2016)
Applying Agile Principles to Collaborative Healthcare Teams
507
3 A GENERIC AGILE PROCESS
FOR COLLABORATIVE
HEALTHCARE TEAMS
Agile methodology may be applied to situations
where complexity and uncertainty are high. This
uncertainty can be related to the scope or even
whether a product or service meets customer and
market needs (Samaniego & Deters, 2016). Agile
methodology can be applied to many aspects of
healthcare service delivery involving multiple
collaborative healthcare teams. For example, teams
within a department in a hospital may work very
efficiently. However, when they are required to
interact with the greater community (inside and
outside the hospital), there is a higher likelihood of
issues. (Tolf, Nyström, Tishelman, Brommels, &
Hansson, 2015) describe three types of environmental
uncertainties that face hospitals, which can be
generalized to healthcare organizations: 1) general
uncertainties that deal with changing demographics,
technology, political and socioeconomic realities; 2)
task uncertainties related interaction with other care
organizations or individuals such as community care,
social care, patients and suppliers; and 3) work
uncertainties that describe scientific elements related
to the nature of care itself such as certainty of
diagnoses, and the ability to routinize diagnoses.
Our generic agile process for collaborative teams
leverages agile artifacts as shown in the list below.
This list summaries some of the mappings between
the terminologies used by collaborative healthcare
teams and agile methodology.
• Sprint Planning: Sprint Planning
• Agile Treatment Plan: Project Backlog
• Intervention/Action: Task
• Ongoing Collaboration: Daily Stand-up
Meeting
• Final Case Conference: Sprint Retrospective
• Agile Dashboard: Agile Dashboard
In order to illustrate the agile process for
collaborative healthcare, we will assume that the
patient has been diagnosed with ADHD, and the team
is in the process of determining the drug of choice, as
well as implementing behavioural modification
strategies for learning.
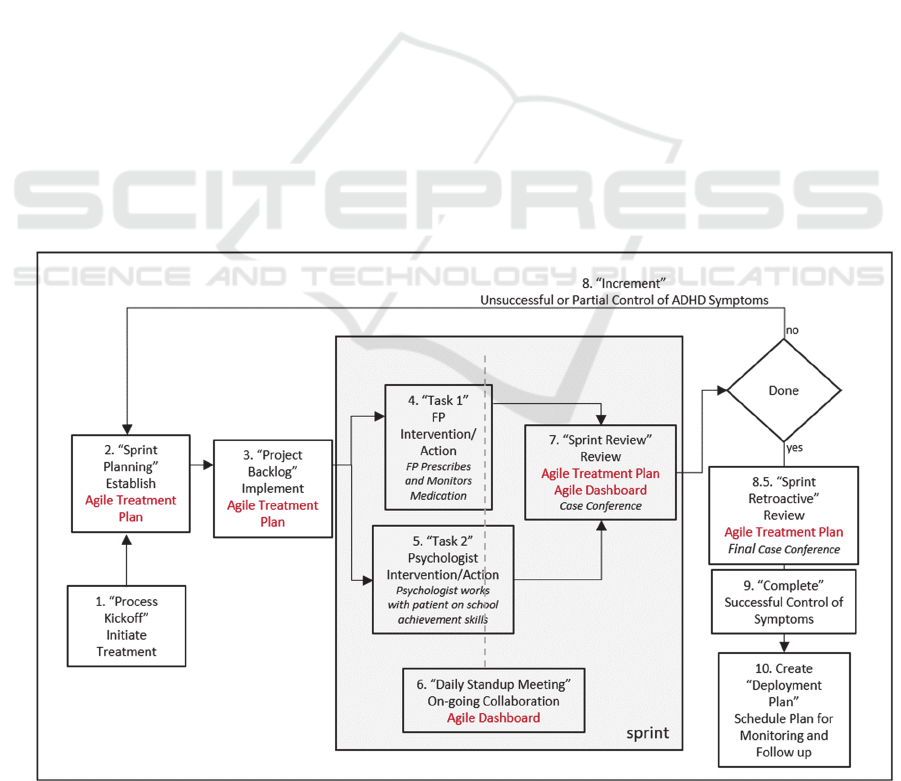
Figure 2 shows how an agile process would see
the creation of a virtual team consisting of the
physician and psychologist. The teams would create
the activities that are part of their treatment as user
stories to a scrum backlog. The team would agree on
an initial treatment plan at a “Sprint Planning
Meeting”, by moving activities from the cross-team
“Project Backlog” into the current sprint or Agile
Treatment Plan (ATP).
Figure 2: Agile Process.
HEALTHINF 2020 - 13th International Conference on Health Informatics
508

This initial meeting could include other players
such as the patient and parents. At the end of the sprint
planning meeting, a treatment plan for the sprint is
produced reflecting a commitment made by all teams
involved. This plan would organize and prioritize
specific interventions related to the broad areas of a
patient’s life, for example, home, school, friends and
peers.
In our example (Figure 2), we focus on learning at
school. The treatment plan includes medication
which would help reduce the symptoms of ADHD.
Therapy is prescribed to help with coping strategies,
as well as possibly tutoring help with schoolwork. A
variety of interventions would be articulated in the
treatment plan to help with the child’s development
(Jellinek & Mcdermott, 2004).
4 ADHD CASE STUDY
Dysfunction of the cerebellar-striatal/adrenergic-
prefrontal brain results in the core symptoms of
ADHD which involve developmentally inappropriate
and functionally impairing inattentiveness and
hyperactivity-impulsivity (Solanto, Arnsten, &
Castellanos, 2001). ADHD is difficult to diagnose
because the core and secondary symptoms of ADHD
are exhibited in many childhood disorders.
Additionally, many view ADHD symptoms as a kind
of variation of normal childhood development.
(Rapport, Timko, & Wolfe, 2006). Whatever the
etiology, the prevalence of the diagnosis of
ADHD/ADD has exploded over the past two decades.
Parents become aware of behavioural issues that
manifest in a child’s or adolescent’s education or
social interactions and, justifiably, look for solutions
to help them.
In current practice, the healthcare team for a child
who has been diagnosed with ADHD is the primary
care physician, parent(s), teacher, and if possible, the
child. Each of these team members plays a role that
yields the most effective outcomes for the child.
The role of the physician is to diagnose, prescribe
medication, recommend community resources for
behaviour and support (such as psychologists), and
on-going monitoring of the child’s progress
(Canadian ADHD Practice Guidelines, Third
Edition, 2011).
The role of the educator is to implement, enforce
and document academic and behavioural strategies
during school hours. Once ADHD is successfully
diagnosed, there is strong evidence that treatments
with high acceptability and adherence yield the best
outcomes for school-aged children with ADHD.
ADHD is a disorder that is best treated with a
combination of drugs and behavioural therapy (MTA
Cooperative Group, 1999; Subcommittee on
Attention-Deficit/Hyperactivity Disorder & Steering
Committee on Quality Improvement and
Management, 2011).
The role of the parent is to execute
recommendations of the family physician and
psychologist, to monitor the effectiveness of the
administered medication, to act as an intermediary
between the school and the healthcare system, to
advocate for the child, and to be a contributing
member of the agile team.
The team in this scenario includes the family
physician Dr. Jones, the psychologist, Dr. Martin,
Mary Smith, the patient, and Mary’s mother. The
educator has been excluded for simplicity.
Due to the collaborative nature of treatment,
ADHD is used as a case study to elaborate on our
model and validate its applicability. We aim to
assess/evaluate whether or not care teams will be
more effective in coordinating care if they adopt or
generic agile process for collaborative care.
4.1 Agile Treatment Plan
The Agile Treatment Plan (ATP) is a document that
establishes the roles and responsibilities of each team
member. This helps in clarifying the importance of
the role of the patient in the process and set
expectations. For example, if the patient is not
compliant in taking the medications, then the process
is deemed a failure and will not be marked as
complete – allowing the team to try a different
approach in subsequent sprints. In addition, an ATP
would specifically outline what drug is being titrated,
as well as the expected reaction to the drug. It could
also specify a meeting plan which would be agreed
upon by all team members.
A sample Agile ADHD Treatment Plan is shown
in Figure 3. In a typical Agile Scrum sprint, the “Daily
Stand-up Meeting” takes place every day for 15
minutes; however, this is highly unfeasible.
Therefore, we adapt the process for the team to meet
on a regular basis at a mutually agreed-upon time, for
a short duration (15 min), to answer three agile-based
questions as needed:
a.What did you do previously?
b.What are you doing currently?
c.Are there any impediments in your way?
Each member of the team provides information or
other assistance to help with impediments as needed.
The team is flexibly agile and governs itself around
the treatment needs of the patient. It should be noted
Applying Agile Principles to Collaborative Healthcare Teams
509
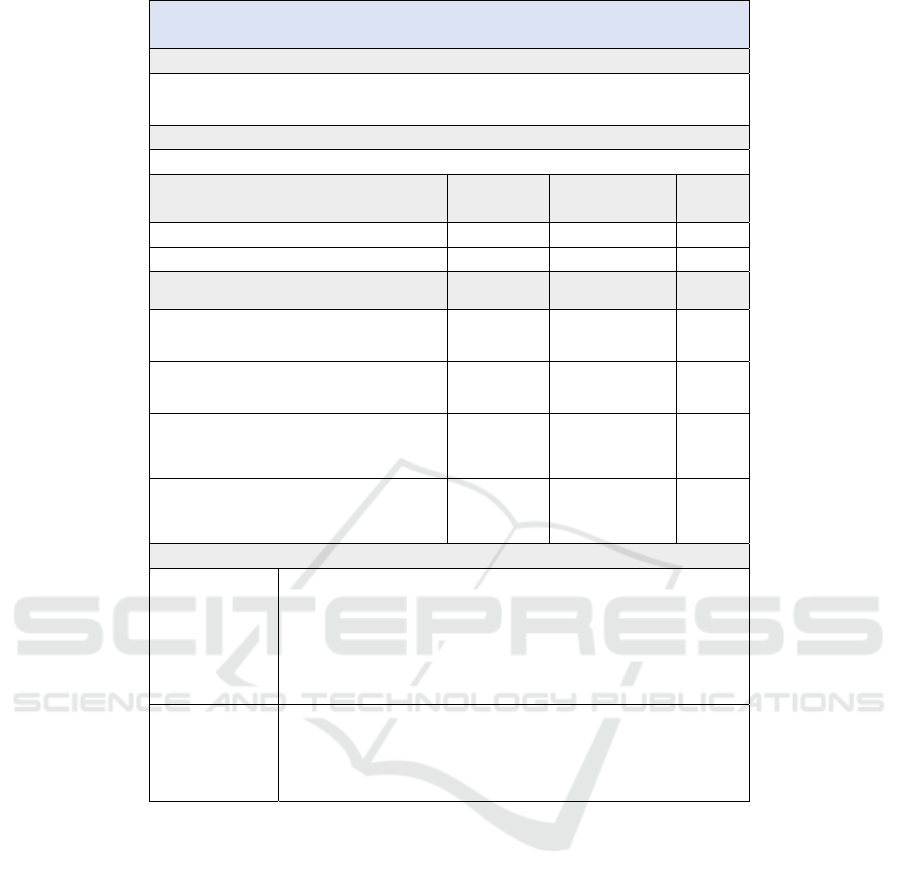
Figure 3: Agile ADHD Treatment Plan.
that each member of the team becomes a source of
expertise in their own discipline, with a recognition
that success can only occur when all members are
fulfilling their responsibilities. The treatment plan is
updated according to feedback from the regular
meetings as necessary. Because of regular sprint-like
meetings, the team becomes agile and can be
responsive to issues that arise from drug
incompatibility for example. Iteration may occur, and
once successful, a final case conference will be held
where there will be an agreement regarding the
outcomes and next steps.
4.2 Agile Dashboard
The objective of this artifact is to provide a snapshot
status at any time before, during or after a sprint. The
elements of the dashboard are the iteration number,
the sprint number and the status of each
Intervention/Action of the current sprint. Figure 4
shows an example of the beginning and middle of a
sprint. The status of the intervention is indicated by
red=fail, yellow=jeopardy, and green=good.
The Agile Dashboard (AD) provides a
mechanism to monitor the status of all the KPIs
associated with the overall treatment plan. It provides
not only the quick operational summary of the
treatment, but it also flags the risks, and blockers so
early intervention can be put in place to mitigate
against those.
Agile Treatment Plan
Name: Mary Smith DOB: July 1, 2006 Current Date: October 11, 2019
Problem/Symptom:
Current symptoms of ADHD include periods of inattentiveness, frustration, irritability and poor self esteem. In addition, over the past few
months Mary has had difficulty coping with stressors; she has reacted to stressors with a brief increase in depressive symptoms, including
increased sleep, suicidal thoughts, and loss of interests.
Long Term Goal:
Symptoms of ADHD will be significantly reduced and will no longer interfere with Mary’s functioning at school.
Short Term Goals/Objectives:
Date Established
Projected Completion
Date
Date
Achieved
1. Alleviate physiological symptoms of ADHD September 1, 2019 June 1, 2019
2. Help Mary be successful at school for current school year September 1, 2019 June 30, 2019
Intervention/Action:
Responsible Person
Short Term
Goals/Objectives:
Status of
Intervention
1. Determine best medication for Mary and monitor her
progress.
Dr. Jones
1. Alleviate
physiological
symptoms of ADHD
Ongoing
2. Mary will take medications on a regular basis as prescribed
and report on how she is feeling.
Mary’s Mother
1. Alleviate
physiological
symptoms of ADHD
Ongoing
3. Dr. Martin will outline and execute a plan to help Mary
success at school.
Dr. Martin
2. Help Mary be
successful at school
for current school
year
Ongoing
4. Mary will work with Dr. Martin and diligently apply the
recommendations from Dr. Martin.
Dr. Martin
2 Help Mary be
successful at school
for current school
year
Ongoing
Review Meetings:
Date: Oct. 11, 2019
Reported by: Dr. Martin
Short Term Goals/Objectives: 1
Intervention/Action: 3,4
STATUS: YELLOW
Mary has not been responding well to current therapy. As a result, I am initiating a new assessment to
determine if there are any underlying issues. At the current time, I recommend a case-conference be held
with Mary’s parents as well as her teacher and guidance councillor. I believe that an Individual Education
Plan (IEP) should be initiated in order to help Mary access the curriculum.
Date: Oct. 11, 2019
Reported by: Dr. Jones
Short Term Goals/Objectives: 2
Intervention/Action: 1,2
STATUS: YELLOW
Mary has demonstrated no change in symptoms. I am increasing titration to 15mg methylphenidate.
HEALTHINF 2020 - 13th International Conference on Health Informatics
510
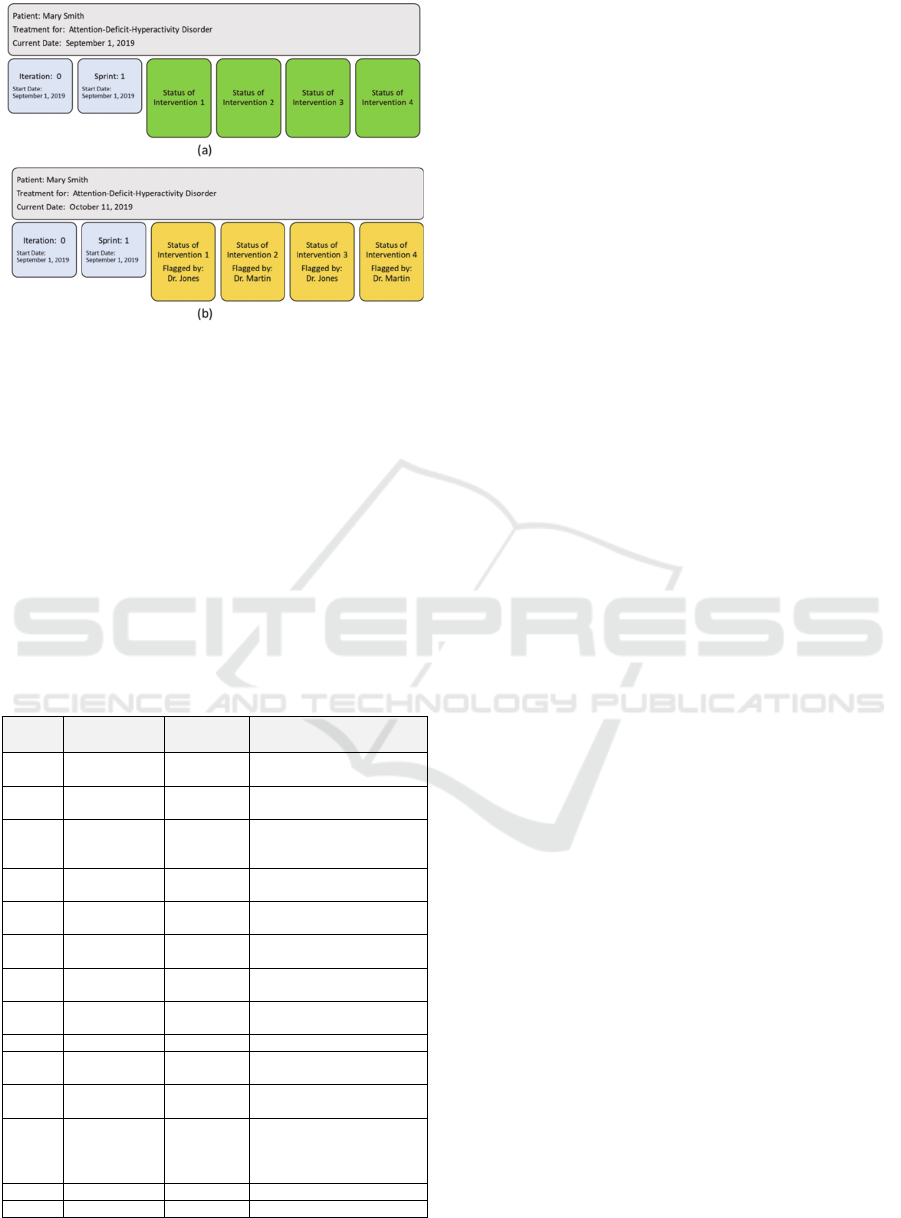
Figure 4: Agile Dashboard at the Beginning (a) and Middle
(b) of a Sprint.
5 PERFORMANCE
MANAGEMENT OF
HEALTHCARE
COLLABORATIVE TEAMS
The Agile Treatment Plan and Agile Dashboard are
useful
tools
for
enabling,
standardizing
and
automating communication between the different
actors in the collaborative healthcare team.
Table 1: Healthcare Agile KPIs.
KPI Description Unit Example
WoS Workflow on
Schedule
Yes Team is meeting as agreed
u
p
on
No Team is not meeting as
a
g
reed u
p
on
Jeopardy There is a risk that the team
is not meeting as agreed
u
p
on
Unknown Schedule not updated due
to technolo
gy
failure
Mod Modality % self Patient administering care
to self
% in
p
erson
Care being given by the
p
arent
% remote Care being monitored by
p
h
y
sician
SS Success
Status
Green Task complete and
successful
White Task incomplete
Yellow Task incomplete – in
j
eo
p
ard
y
Red Task complete and
unsuccessful
DB Dashboard Mixed All KPIs would be shown
on the dashboard in
addition to technology
effectiveness
TEC Technolo
gy
Success Tools workin
g
Fail Tools not workin
g
.
The data from these artifacts can be useful for
performance management of Healthcare
Collaborative teams. Performance management in
this context would help professionals analyse how
effective their interventions/actions are for the
individual as well as over a large swath of patients,
without actually monitoring their actual treatment.
Accordingly, performance metrics are related to team
collaboration, and not individual team member
performance. Some examples are shown in Table 1.
We specifically chose KPIs related to
collaboration, while avoiding those related to specific
areas of clinical expertise such as “appropriate
diagnosis” or “effective medication” for example.
The objective is to measure key aspects of team
performance such as whether they were meeting
regularly, how are they meeting (in person or
remotely), whether they thought they were being
successful and whether the technology they are using
is working for them. Other KPIs can include whether
the workflow is on schedule, how often the
technology breakdown and causes problems.
6 DISCUSSION AND FUTURE
WORK
In this paper, we have shown how agile methodology
can be applied to making collaborative healthcare
teams more effective. Our approach revolves around
the Agile Treatment Plan and the Agile Dashboard.
The application of agile principles results in
several improvements. For example, team members
are aware on a daily basis of patient status in terms of
what is being done (Agile Treatment Plan) and how
the patient is progressing (Agile Dashboard). Rather
than each individual team member having their own
treatment plan, and ad hoc measurements of
indicators for progress, this approach provides
conformity and continuity between modalities and
treatments. Team consensus is established at the
beginning of what the goals are and how they will be
measured (dashboard) in a formalized way.
Importantly, the process of care follows a simple
structured template rather than being ad hoc and
adverse event-driven. Another important factor is
that the composition of the team is flexible and
configurable (for example, the patient, parent or
teacher or pharmacist can be part of the team).
Different members with different roles and
knowledge can easily plugin. Finally, performance
management is now enabled and quantifiable.
Applying Agile Principles to Collaborative Healthcare Teams
511

There are several challenges to the application of
an agile methodology to healthcare processes. For
example, the ATP represents yet another form for
practitioners to be concerned with. An Agile
Dashboard will have the same issue since there are
several support tools. Hence the adoption of these
artifacts may be an issue due to cognitive overload,
management of information, hosting and other IT
issues. A further issue is on reaching agreement on
KPIs, their meaning and use.
An area of the agile methodology that would
improve collaboration is a common language and
terminology. There are several ways that this could be
achieved. Firstly, placing an emphasis on the
functionality of the patient, rather than the disease,
may be an effective way to enable common ground
through common language use. This would also shift
the emphasis from treatment to management and
creation of healthy living within the context of illness.
Secondly, in order to further create a common
understanding, we believe that an ontology for
collaborative healthcare that consists of actors, their
relationships, how communication occurs, what
information is communicated, and what is done with
this information, be developed.
7 CONCLUSION
In this paper, we have shown how agile methodology
can be applied to manage the treatment of chronic
conditions such as ADHD. Our approach anchors
around the Agile Treatment Plan and the Agile
Dashboard. We have shown how the KPIs that form
these artifacts can be used to quantify healthcare team
collaboration and performance. We also articulated
some areas of improvement that could be evident
should if an agile approach is used. Finally, we
articulated some challenges and the need for an
ontology and common communication based on
functionality, rather than ailment or disease.
In summary, the application of Agile
methodology to healthcare would require
managers/administrators to empower knowledge
workers to find solutions, rather than control the
team. It requires healthcare teams to become self-
organizing, autonomous, and have the ability to
function as a network of teams. Coordination of work
would occur in an iterative manner, free of
bureaucracy, while at the same time being structured.
Practices would be customer-focused, and mission-
critical.
REFERENCES
Anderson, J. G., & Abrahamson, K. (2017). Your health
care may kill you: Medical errors. Studies in Health
Technology and Informatics. https://doi.org/10.3233/
978-1-61499-742-9-13
Azvine, B., Nauck, D., & Ho, C. (2003). Intelligent
business analytics-a tool to build decision-support
systems for eBusinesses. BT Technology Journal,
21(4), 7. https://doi.org/10.1023/A:1027379403688
Canadian ADHD Practice Guidelines, Third Edition.
(2011). Toronto.
Carpentier, P. J. (2012). ADHD. In Drug Abuse and
Addiction in Medical Illness: Causes, Consequences
and Treatment. https://doi.org/10.1007/978-1-4614-
3375-0_22
Denning, S. (2016). How to make the whole organization
“Agile.” Strategy and Leadership, 44(4), 10–17.
https://doi.org/10.1108/SL-06-2016-0043
Dabak, A. 2016. “APC Key Performance Indicators.” In 1st
ISA UAE Automation Conference and Exhibition
2016.
Duka, D. (2013). Adoption of agile methodology in
software development. 2013 36th International
Convention on Information and Communication
Technology, Electronics and Microelectronics, MIPRO
2013 - Proceedings.
Eikey, E. V., Reddy, M. C., & Kuziemsky, C. E. (2015).
Examining the role of collaboration in studies of health
information technologies in biomedical informatics: A
systematic review of 25 years of research. Journal of
Biomedical Informatics, 57, 263–277.
https://doi.org/10.1016/j.jbi.2015.08.006
Ezziane, Z., Maruthappu, M., Gawn, L., Thompson, E. A.,
Athanasiou, T., & Warren, O. J. (2012). Building
effective clinical teams in healthcare. Journal of Health
Organization and Management, 26(4), 428–436.
https://doi.org/10.1108/14777261211251508
Havyer, R. D. A., Wingo, M. T., Comfere, N. I., Nelson, D.
R., Halvorsen, A. J., McDonald, F. S., & Reed, D. A.
(2014). Teamwork Assessment in Internal Medicine: A
Systematic Review of Validity Evidence and
Outcomes. Journal of General Internal Medicine,
29(6), 894–910. https://doi.org/10.1007/s11606-013-
2686-8
Jellinek, M. S., & Mcdermott, J. F. (2004). Formulation:
Putting the Diagnosis Into a Therapeutic Context and
Treatment Plan. J. AM. ACAD. CHILD ADOLESC.
PSYCHIATRY, 43(7), 913–916.
https://doi.org/10.1097/01.chi.0000125090.35109.57
Kuziemsky, C. (2016). Decision-making in healthcare as a
complex adaptive system. Healthcare Management
Forum, 29(1), 4–7. https://doi.org/10.1177/084047
0415614842
Makary, M. A., & Daniel, M. (2016). Medical error-the
third leading cause of death in the US. BMJ (Online).
https://doi.org/10.1136/bmj.i2139
Mayo, A. T., & Woolley, A. W. (2016). STATE OF THE
ART AND SCIENCE Teamwork in Health Care:
Maximizing Collective Intelligence via Inclusive
HEALTHINF 2020 - 13th International Conference on Health Informatics
512

Collaboration and Open Communication. AMA Journal
of Ethics Journal of Ethics ®, 18(9), 933–940.
https://doi.org/10.1001/journalofethics.2016.18.9.stas2
-1609
MTA Cooperative Group. (1999). A 14-Month
Randomized Clinical Trial of Treatment Strategies for
Attention-Deficit/Hyperactivity Disorder. Archives of
General Psychiatry, 56(12), 1073. https://doi.org/
10.1001/archpsyc.56.12.1073
Nolte, E., Knai, C., & McKee, M. (2008). Managing
chronic conditions. Experience in eight countries. In
Observatories Studies Series N˙15. https://doi.org/
ISBN 978 92 890 4294 9
Rapport, M. D., Timko, T. M., & Wolfe, R. (2006).
Attention-Deficit/Hyperactivity Disorder. In M. Hersen
(Ed.), Clinician’s handbook of child behavioral
assessment (pp. 401–435). Elsevier Academic Press.
Reason, J. (2000). Human error: models and management.
British Medical Journal, 320, 768–770.
https://doi.org/10.1136/bmj.320.7237.768
Samaniego, M., & Deters, R. (2016). Blockchain as a
Service for IoT. 2016 IEEE International Conference
on Internet of Things (IThings) and IEEE Green
Computing and Communications (GreenCom) and
IEEE Cyber, Physical and Social Computing
(CPSCom) and IEEE Smart Data (SmartData), 433–
436. https://doi.org/10.1109/iThings-GreenCom-
CPSCom-SmartData.2016.102
Sicotte, C., D’amour, D., & Moreault, M.-P. (2002).
Interdisciplinary collaboration within Quebec
community health care centres. In Social Science &
Medicine (Vol. 55). https://doi.org/10.1016/S0277-
9536(01)00232-5
Solanto, M. V., Arnsten, A. F. T., & Castellanos, F. X.
(2001). Stimulant drugs and ADHD : basic and clinical
neuroscience. New York: Oxford University Press.
Subcommittee on Attention-Deficit/Hyperactivity
Disorder, & Steering Committee on Quality
Improvement and Management. (2011). ADHD:
Clinical Practice Guideline for the Diagnosis,
Evaluation, and Treatment of Attention-Deficit/
Hyperactivity Disorder in Children and Adolescents.
Pediatrics, 128(5), 1007–1022. https://doi.org/10.1542/
peds.2011-2654
Tolf, S., Nyström, M. E., Tishelman, C., Brommels, M., &
Hansson, J. (2015). Agile, a guiding principle for health
care improvement? International Journal of Health
Care Quality Assurance, 28(5), 468–493.
https://doi.org/10.1108/IJHCQA-04-2014-0044
Upadrista, V. (2015). Agile Methodology. In The Art of
Consultative Selling in IT. https://doi.org/10.
1201/b18065-15
Williams, S. J. (2016). Delivering Agile and Person-centred
Care. In Improving Healthcare Operations (pp. 45–56).
https://doi.org/10.1007/978-3-319-46913-3_4
Zwarenstein, M., Goldman, J., & Reeves, S. (2009).
Interprofessional collaboration: effects of practice-
based interventions on professional practice and
healthcare outcomes. Cochrane Database of Systematic
Reviews, (3). https://doi.org/10.1002/14651858.
CD000072.pub2
Applying Agile Principles to Collaborative Healthcare Teams
513
