
Clinical Value of Functional MRI in the Diagnosis of Cognitive
Disorders in Patients with Arteriovenous Malformations
N. V. Korno
1
, N. E. Ivanova
1
, A. Yu Ivanov
2
, G. E. Trufanov
1
, N. N. Semibratov
1
, D. N. Iskhakov
1
,
A. V. Sokolov
1
, A. S. Lepekhina
1
and A. Yu Efimtsev
1
1
Almazov National Medical Research Centre, Akkuratova Str. 2, Saint-Petersburg, Russia
2
St.-Petersburg State Pediatric Medical University, Litovskaya Str. 2, Saint-Petersburg, Russia
Keywords: Functional Magnetic Resonance Imaging, Arteriovenous Malformations, Bold Contrast, Cognitive
Impairment.
Abstract: Cognitive impairment that develops in acute and chronic cerebral pathology, including arteriovenous
malformations, is one of the most frequent and prognostically unfavorable complications. Late detection of
severe forms of cognitive impairment, including dementia, leads to a lack of early preventive and therapeutic
correction, a decrease in the effectiveness of rehabilitation and the quality of life of patients with AVM. A
comprehensive assessment of cognitive impairment may be a diagnostic criterion for assessing the severity
of neurological symptoms at the endovascular treatment stages. A significant contribution to the study of the
pathophysiology of CN formation in patients with AVM is made by fMRI, providing knowledge about the
functional organization of the brain. The results of functional mapping of the brain in 11 patients with
arteriovenous malformations are presented. The structure of cognitive impairment was evaluated using
advanced neuropsychological testing and structural-functional restructuring in the cerebral cortex using fMRI.
To obtain images, an echoplanar tomography technique using BOLD contrast was used. The data obtained
indicate complex neurodynamic disorders of the cognitive sphere in patients with AVM in several areas of
both the right and left hemisphere: dorsal, ventral and medial front-striatal thalamic and fronto-parietal
cerebellar networks.
1 INTRODUCTION
Cerebral arteriovenous malformations (AVM) are a
malformation of cerebral vessels belonging to the
group of congenital and progressive vascular diseases
of the central nervous system (Robert,2007; Berman,
2007; Lin et al, 2012).
AVMs are a significant source of disability and
mortality in the working age population among
various forms of cerebrovascular abnormalities. Up to
4% of all intracranial volume formations, 9% are
causes of non-traumatic subarachnoid hemorrhages,
1% are ischemic strokes (Robert, 2017).
Information on the frequency of occurrence of
cerebral AVM in the population is contradictory and
depends on the sources of information. Some studies
indicate that the prevalence of the disease in the adult
population is 19 per 100,000 people, and the
frequency of surgical interventions for AVM of the
cerebral vessels is 0.9 per 100 thousand of the
population per year (Laakso et al., 2010; Lunsford,
2009; Laakso et al. A2012).
The clinical manifestation of AVM most often
occurs in people 20-50 years old, and the long-term
prognosis without surgical treatment is unfavorable:
23% of patients die, in 48% the disease leads to
disability, which indicates the social significance of
this problem (Robert, 2017).
One of the most frequent and maladaptive
manifestations of AVM is cognitive impairment (CI)
(Marshall et al., 2003; Steinvorth et al., 2002, Lazar
et al. 1996; Steinvorth, 2002; Andrea et al.,2014;
Buklina, 2001).
Considering that AVM is a congenital pathology,
CI at the stage of mild disorders often remain
underestimated, thereby transforming into more
severe forms, leading to significant limitations in
work, the social sphere, and patient self-care (Ernst et
al.,2017; Charidimou et al., 2017)
The cerebral cortex is a complex integrated
system that combines a large number of different
parts of the nervous system, each of which performs
Korno, N., Ivanova, N., Ivanov, A., Trufanov, G., Semibratov, N., Iskhakov, D., Sokolov, A., Lepekhina, A. and Efimtsev, A.
Clinical Value of Functional MRI in the Diagnosis of Cognitive Disorders in Patients with Arteriovenous Malformations.
DOI: 10.5220/0008973003790386
In Proceedings of the 13th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2020) - Volume 1: BIODEVICES, pages 379-386
ISBN: 978-989-758-398-8; ISSN: 2184-4305
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
379

a specific function. At the same time, these
departments interact with each other, participating in
the implementation of one or another program, in the
framework of which the information entering the
brain is constantly processed by centers structurally
and functionally interconnected (Yakhno et al., 2014;
Luria, 2000, Mendoza et al., 2014)
The quantitative and qualitative characteristics of
cognitive impairment are extremely important in the
diagnostic work of neurologists, neurosurgeons,
therapists and doctors of other specialties. The
identification and clinical analysis of the cognitive
impairment features in patients with AVM is
necessary for the correct syndromal and topical
diagnosis, for assessing the severity of neurological
symptoms at the stages of endovascular treatment of
AVM. Extensive neuropsychological testing and
conventional neuroimaging are not enough to
describe the general picture of AVM, because even if
it can provide accurate anatomical localization, it
does not provide any information about the functional
organization of the brain.
A significant contribution to the study of the
pathophysiology of cognitive impairment formation
in patients with AVM is made by modern methods of
neuroimaging, one of which is fMRI, because it
allows you to simultaneously obtain data on
metabolism, blood flow and structural and functional
characteristics of the brain (Ellis, 2016).
The first work on the use of fMRI in brain
research appeared in 1992 (Bandettini, 1992). FMRI
has become the standard for determining the activity
of brain neurons in humans, since it is a non-invasive
method, has reliable localization of responses, and
high spatial resolution, compared to the earlier
developed technologies, such as positron emission
tomography (PET) (Odinak, 2006; Lazar et al., 2010).
Considering that the hemodynamic characteristics
of AVM is a decrease in pressure in the arteries
involved in the blood supply to AVM, a unified
system of blood circulation equilibrium is being
displaced, and as a result — arteriovenous bypass
surgery has a damaging effect on the cerebral cortex.
According to the mechanism of intensive venous
discharge, areas of reduced microcirculation are
formed, both in the affected vascular pool and in the
opposite hemisphere. Due to the structural and
functional reorganization of the cerebral cortex, that
occurs against the background of insufficient blood
circulation, cortical functions from certain parts of the
brain are rearranged to adjacent parts of the brain,
which leads to their later manifestation in patients
with AVM (Ishikawa et al., 2017; Moretti et. Al.,
2017).
Functional magnetic resonance imaging is
considered as a way of studying the "functional
architecture" of the brain. The most widely used
fMRI technique is based on the sensitivity of the pulse
sequence of the gradient echo to changes in the
oxygenation of brain tissue - the BOLD effect
(Barbay et. al., 2017, Keefe et. al., 2017).
With this sequence, changes in the magnetic
resonance signal in the same part of the brain under
conditions of rest and activation occur due to
differences in the paramagnetic properties of
deoxyhemoglobin and oxyhemoglobin. It is believed
that when exposed to an irritant, the degree of
increase in regional blood flow exceeds the tissue's
oxygen demand, which leads to local hyperoxemia
and, consequently, to a decrease in the concentration
of deoxyhemoglobin. Due to a decrease in the degree
of local inhomogeneity of the magnetic field, an
increase in the magnetic resonance signal occurs.
Areas that change the signal intensity in accordance
with the shape and duration of the stimulus are
detected using special statistical processing, are
selected in the form of activation maps and combined
with anatomical images of the brain.
Regarding the study of the cognitive status of
patients with AVM, there are only a few studies. In
2013, a team of researchers led by R.L. Piana showed
how the combined use of different imaging
techniques can be useful in understanding
neuroplasticity and hemodynamics in patients with
AVM at the endovascular treatment stages. Valuable
information in this case is that the structural and
functional organization of the brain in patients with
complex AVMs has a number of features, and it can
be obtained using a more systematic and extensive
imaging protocol that combines perfusion with
complex analyzes of functional MRI (fMRI) and
anatomical MRI for the purpose of mapping brain
activations at the stages of endovascular treatment of
vascular abnormalities (Roberta La Piana, 2013).
In the works of J.C. Lin, T.H.Le described cases
of regression of neurological deficit after
microsurgical removal of malformation due to
compensatory rearrangement of cortical functions.
A study conducted in Japan between 1977 and
1994 described dynamic changes in activation zones
for stimulus tasks. This pattern was presumably
associated with either hemorrhage or ischemic
disorders that correlated with changes in MRI
(hemosiderin deposition, hypoperfusion zones
associated with the “robbery phenomenon”) (Kida,
1994).
A number of foreign fMRI studies have shown
that the functional activity of the cerebral cortex is
NDNSNT 2020 - Special Session on Non-invasive Diagnosis and Neuro-stimulation in Neurorehabilitation Tasks
380

specifically impaired in patients with depressive and
anxiety disorders (Bremner et al., 2002; Cotter et al.,
2001).
Using fMRI methods, Russian researchers have
demonstrated the effects of activation of
neuroplasticity under the influence of
neuroelectrostimulation in patients with depressive
disorder. The use of modern methods of data analysis
of fMRI revealed a significant improvement in the
functioning of the basic working network and brain
connectivity in the studied patients (Kublanov, 2018;
Kublanov, 2019).
To assess cognitive impairment in patients with
AVM, a comprehensive examination is necessary,
including not only the identification of structural
changes using modern neuroimaging methods, but
also a qualitative analysis of integrative changes
using neuropsychological examination. In routine
practice, CI in patients with AVM often remains
unrecognized due to the lack of a standard
examination protocol and the possibility of long-term
monitoring of this category of patients (Skrobot et al.,
2018; Behrman, 2017).
2 PURPOSE
The aim of our study was to assess the clinical
significance of modern functional neuroimaging in
the diagnosis of cognitive impairment in patients with
arteriovenous malformations of the brain, who
underwent embolization of the AVM with the non-
adhesive ONYX composition.
3 MATERIALS AND METHODS
3.1 Study Population
The main criterion for inclusion in the study was the
presence of AVM of supratentorial localization,
confirmed by the history, neurological examination,
and the results of a routine neuroimaging
examination. The study included 11 patients with
arteriovenous malformations of the brain who have
been treated at the Russian National Pedagogical
Institute. prof. A.L. Polenova from January 2014 to
December 2017, who performed embolization of the
AVM with the non-adhesive ONYX composition,
and 18 healthy right-handed volunteers (healthy
controls), who were stratified by gender and age. The
average age of patients with AVM was 36.6 years.
Analysis of the results was made with a maximum
follow-up of 12 months. The structure of cognitive
impairment was evaluated using advanced
neuropsychological testing and structural and
functional restructuring in the cerebral cortex using
fMRI. To activate various areas of the cerebral cortex
during fMRI, patients were asked to perform special
tasks-paradigms. The following were used: the
standard speech block paradigm (speech test), the
generation of counting operations according to the
indifferent counting series presented with the help of
headphones (counting test), the activation of optical-
spatial functions and visual memory using simple
(non-plot) pictures presented on the screen (visual
stimuli).
3.2 MR Imaging Protocol
To obtain images, we used the echoplanar
tomography technique using BOLD contrast.
Postprocessing included the elimination of artifacts,
statistical analysis of BOLD signals, the construction
and combination of t-maps of activation zones with
T1 of the brain and their transformation into the MNI
coordinate space (Montreal Neurological Institute -
Montreal Neurological Institute). The study was
performed using 1.5 Tesla MR scanner. The
observations were dominated by the epileptic type of
course - 8 (41.1%), hemorrhagic type was found in 3
patients (33.56%).
The majority of patients with AVM in the amount
of 6 (54.5%) cases were assigned to Spetzler-Martin
Grade III and V, with the exception of 1 (9.1%)
patient of Grade IV. In the studied group of patients,
AVM localization in the left hemisphere prevailed - 6
(54.5%) patients. Of these, in an amount of 4 (36.4%)
in the left parietal lobe, temporal lobe -1 (9.1%), in
the left occipital lobe -1 (9.1%). In the right
hemisphere, the main localization of the AVM is in
the parietal lobe and occipital lobe 2 (18.2%), in one
case (9.1%) in the frontal lobe.
The principle of multi-stage, complex treatment
was used in all patients - the maximum possible AVM
fragments were embolized during one surgical
intervention (60% approx. of the whole volume of
AVM).
3.3 Results
When performing intragroup analysis (healthy
volunteers) at the stages of interaction of neuronal
structures for recognizing the presented images, a
decrease in activation was detected in the prefrontal
cortex, the Broadman area (BA) 10, as well as in the
projection of BA17 and BA18 (MNI coordinates: -36 -
Clinical Value of Functional MRI in the Diagnosis of Cognitive Disorders in Patients with Arteriovenous Malformations
381
90 14). At the same time, an increase in activation was
observed in the isthmus of the cingulate gyrus - BA31
(MNI coordinates: 6 -62 32), in the insula (MNI
coordinates: 4 40 38) and the parahippocampal gyrus
(MNI coordinates: 32 -36 -12). Local patterns of
processing visual information, recognizing visual
images and transmitting information to other
departments of the visual analyzer that are involved in
providing emotional-volitional decisions, the
formation of motivation, cognitive flexibility, short-
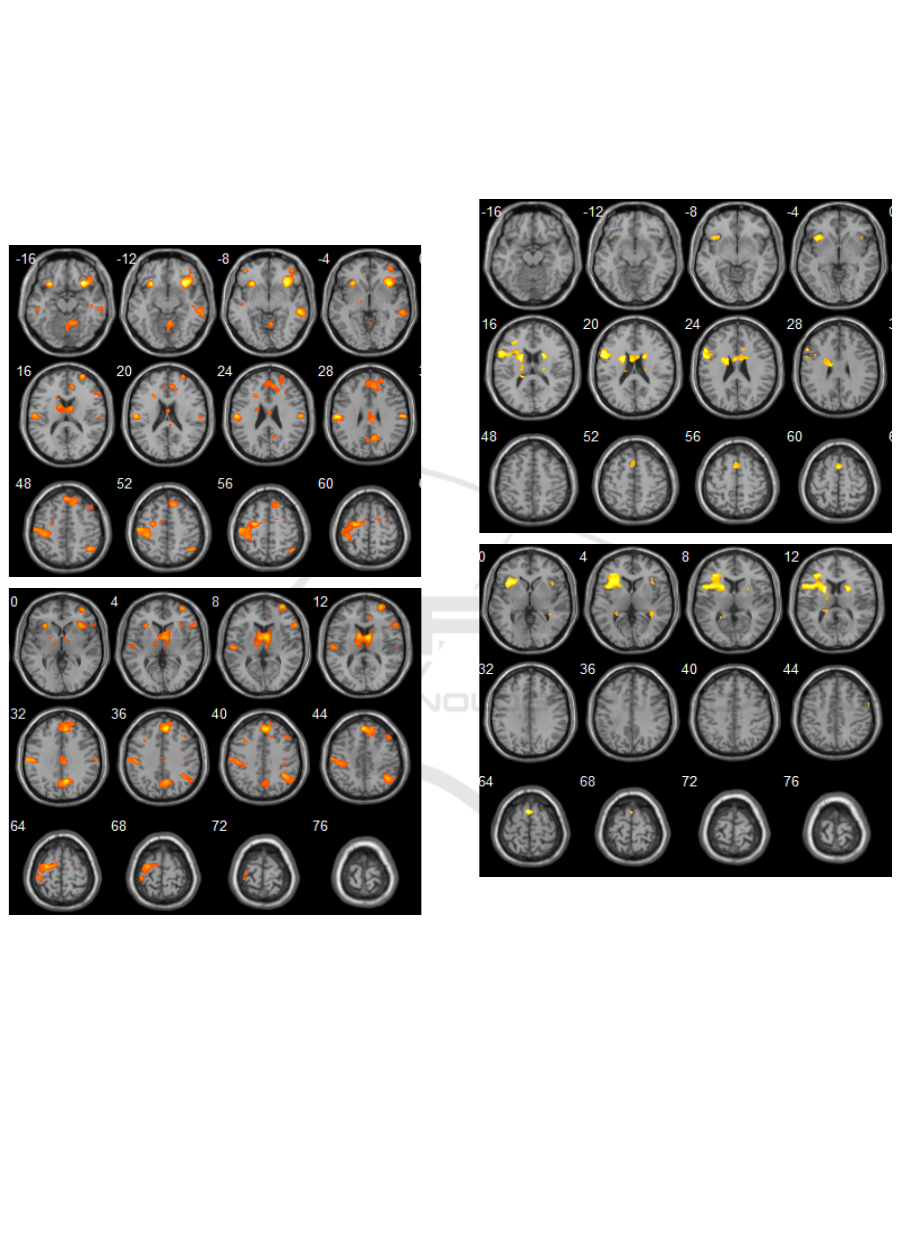
Figure 1: The control group. Activation sites (response to a
visual stimulus) in the projection of brain structures: the
isthmus of the cingulate gyrus, insular cortex,
parahippocampal gyrus, Broca and Wernicke areas —
bilaterally.
term memory and neurodynamics, which is the main
function of the thalamo lenticular complex (Figure 1),
were found. The topical importance of the
parahippocapal complex is to create complex cognitive
patterns, form short-term memory, while being the
basis of neurodynamic thinking, forming connections
with cortical, subcortical, stem formations of the brain.
As it can be seen in Figure 2, when performing a
speech test, there were activations in the region of the
parahippocampal complex in the projection of the
fusiform gyrus (MNI coordinates: 30 -34 20), upper
and lower temporal gyri on the right (MNI coordinates:
52 64 22; 54 -18 -22), upper frontal gyrus on the right,
caudate nuclei (MNI coordinates: 6 8 -6), insular lobes
(MNI coordinates: 34 -22 10).
Figure 2: The control group. Activation sites (response to a
speech test) in the projection of brain structures: the isthmus
of the cingulate gyrus, insular lobes and parahippocampal
gyri.
Presenting a ”count” stimuli resulted in activation areas
in the projection of the middle frontal gyri bilaterally,
insular cortex on the right (MNI coordinates: 40 - 14
8), the upper frontal gyrus on the left (MNI
coordinates: -14 48 48), precentral gyrus bilaterally
(MNI coordinates: 38 -14 50; -24 -24 62). All these
zones are parts of the working network of the brain
at rest and carry out complex, including logical,
processing of information of various nature, are
responsible for short-term and long-term memory,
fluency of speech, neurodynamics, and error control
NDNSNT 2020 - Special Session on Non-invasive Diagnosis and Neuro-stimulation in Neurorehabilitation Tasks
382
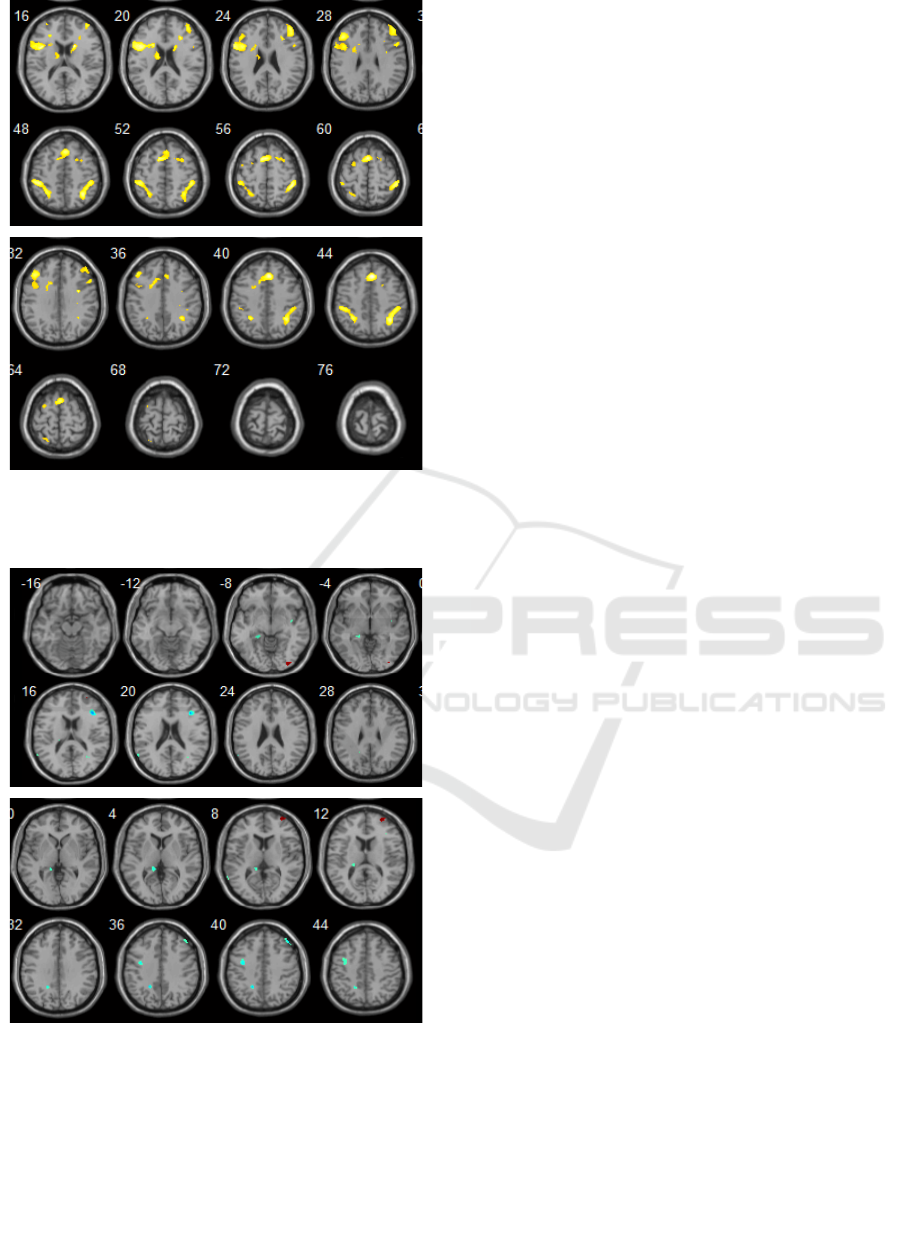
Figure 3: The control group. Activation sites (response to a
count test): in the projection of brain structures: medial
prefrontal cortex, BA9, BA46, BA31, BA32.
Figure 4: Results of intergroup analysis. Activation sites
(response to the visual stimuli) presented in the patient
group compared to the control group. Increased severity
(blue): in the projection of PB 6, PB 10, parietal cortex,
prefrontal and cingulate cortex, (p <0.001).
(Figure 3).
The dynamical intergroup analysis was aimed to
establishing statistically significant differences
between the volume of activations to compare
functional changes in the cerebral cortex in patients
with AVM and healthy volunteers. In patients with
AVM, fewer activation sites were detected in
response to certain cognitive tasks. Recognition of the
presented images, storing and fixing of repeated
images on the images presented on the screen
revealed an increase in the activation of the following
areas of the brain in patients with AVM: on the left is
the region of the central gyrus, subcortical structures
BA6 (MNI coordinates: -2 8 -25), BA10 (MNI
coordinates: 23 55 7); parietal cortex (MNI
coordinates: 23 -38 52), on the right - the lower
parietal cortex (MNI coordinates: -24 -50 -40), the
prefrontal cortex (MNI coordinates: 17 44 2) and the
cingulate cortex (MNI coordinates: 4 23 22), p
<0.001, (Figure 4).
When performing a speech test, in patients,
comparing to the control group, a decrease in
activation was found in the following areas: lower
parietal lobe bilaterally, insular lobules on the left
(BA13, MNI coordinates: -42 4 -1), lower frontal
gyrus on the left (MNI coordinates: -32 47 -1),
caudate nucleus (MNI coordinates: 14 10 11) on the
left, parahippocampal gyrus on the left (MNI
coordinates: 24 -9 -4). There was also a statistically
significant increase in activation in the projection of
the superior frontal gyrus on the left (BA 10, MNI
coordinates: 12 49 4), the medial prefrontal cortex
and the anterior cingulate gyrus, p <0.001, (Figure 5).
The main functions of these zones are organization of
complex cognitive circuits, the substrate of short-term
memory, the basis of neurodynamic thinking. They
form connections with cortical, subcortical, stem
structures in the brain.
When performing count test (repeated count
operations), in patients, comparing to the control
group, a statistically significant increase in
activations was established in the following areas:
inferior parietal lobe, BA32 bilaterally (MNI
coordinates: -10 46 11; 14 40 11) , BA7 (MNI
coordinates: 23-60 60), BA9 on the right (MNI
coordinates: 35 39 31), insula (MNI coordinates: 44 4
10), middle frontal gyrus (MNI coordinates: 30 47
11), waist gyrus on the left (MNI coordinates: -3 36
11), p <0.001, (Figure 6).
In the structure of cognitive impairment within the
group of patients with AVM at the stages of
endovascular treatment (ONYX embolization),
cognitive impairments of a mixed structure
(dysfunction of the fronto-subcortical formations of
the brain; structures of the hippocampal circle;
temporal-parietal-occipital region) were revealed -
90%; dysfunction of the structures of the hippocampi
- 10%. In 70%, cognitive impairment was noted at the
Clinical Value of Functional MRI in the Diagnosis of Cognitive Disorders in Patients with Arteriovenous Malformations
383
Figure 5: Intergroup analysis results. Activation sites
(response to the presented speech test) in the patient group
compared to the control group. Increased (blue): in the
projection BA10 on the left. Decrease (red): in the
projection of the lower frontal gyrus on the left, the insula
on the left, the caudate nucleus, the parahippocampal gyrus
on the left (p <0.001).
level of the first functional block (block of regulation
of brain activity) - nonspecific structures of the brain
(thalamo-reticular complex) and the third functional
block (level of regulation, control of activities). In all
patients in the group with AVM, a defeat of the
second functional block (block of reception,
processing and storage of ectoceptive information
(modally specific processes) was noted. Focal
neurological symptoms in the form of oculomotor
disorders, homonymous hemianopsia and
coordinating disorders were revealed in 60% of cases.
About 30% of patients showed mild hemiparesis and
pyramidal symptoms, and 20% had Vincent's
symptom (BA4, BA6) and mild sensitive disorders.
Figure 6: Intergroup analysis results. Activation sites
(response to the presented sample test) in the patient group
compared to the control group: Increased (blue): in the
projection, left inferior parietal lobe BA9, left middle
frontal gyrus (p <0.001).
4 CONCLUSIONS
The clinical significance of modern functional
neuroimaging plays an important role in the diagnosis
of cognitive impairment. The results of our fMRI
study in patients with AVM using the diagnostic
algorithms indicate complex neurodynamic disorders
of the cognitive sphere in several areas, such as the
right and left hemispheres of the dorsal, ventral and
medial fronto-striato-thalamic and fronto-parieto-
cerebellar networks, responsible for control,
attention, reaction speed of choice. In addition, there
is growing evidence of a decrease in activation in
patients with AVM at the endovascular treatment
stages in the prefrontal and limbic regions, which
provide motivation and control of emotions.
Pathogenetic features of cognitive impairment,
assessment of modern methods of neuroimaging and
diagnosis using advanced neuropsychological testing
are currently a promising area. However, features in
the field of correlation between functional research
methods and early identification of cognitive
impairment using advanced neuropsychological
testing have not been investigated. The study of the
structure of cognitive impairment using fMRI in
combination with neuropsychological testing can
help take a fresh look at the vast neuronal
relationships in the central nervous system. The
NDNSNT 2020 - Special Session on Non-invasive Diagnosis and Neuro-stimulation in Neurorehabilitation Tasks
384

inconsistency of numerous literature data confirms
the relevance of this technique to improve the
diagnosis of cognitive impairment in patients with
AVM in order to optimize the therapeutic effect.
CONFLICT OF INTERESTS
The authors declare no conflict of interest.
REFERENCES
Robert M. Friedlander, M.D. Arteriovenous Malformations
of the Brain N Engl J Med 2007;356:2704-2712.
Berman MF, Sciacca RR, Pile-Spellman J, Stapf C et.al.
The epidemiology of brain arteriovenous
malformations. N Engl J Med. 2007;356(26):2704-12.
Lin N, Zenonos G, Kim AH, Nalbach SV, Du R, Frerichs
KU, Friedlander RM et al.. Angiogram-negative
subarachnoid hemorrhage: relationship between
bleeding pattern and clinical outcome. Neurocrit Care.
2012;16(3):389-98. DOI 10.1007/s12028-012-9680-6.
Robert A. Solomon, M.D., E. Sander Connolly, Jr., M.D.
Arteriovenous Malformations of the BrainN Engl J
Med. 2017;376:1859-1866 DOI: 10.1056/NEJMra16
07407
A. Laakso, R. Dashti, S. Juvela, M. Niemela, J.
Hernesniemi Natural history of arteriovenous
malformations: presentation, risk of hemorrhage and
mortality. Acta Neurochir Suppl. 2010;107:65-69.
L.D. Lunsford, D. Kondziolka Radiosurgery Practice
Guideline Initiative Stereotactic Radiosurgery for
Patients with Intracranial Arteriovenous Malformations
(AVM). Radiosurgery Practice Guideline. 2009; Report
№2-03. March.
Laakso A., Hernesniemi J. «Arteriovenous malformations:
epidemiology and clinical presentation». Neurosurg.
Clin. N Am. 2012; 23:1–6.
Marshall G.A., Jonker B.P., Morgan M.K., and Tailor A.J.
Prospective study of neurophysiological and
psychological outcome following syrgical excision of
intracerebral arteriovenous malformations. Jornal of
Clinical Neuroscience. 2003;10:42-47.
Mahalick D.M.,Ruff R.M., Heary R.F. Preoperative versus
postoperative neurophysiological sequelae of
arteriovenous malformations. Neurosurgery. 1993;
33:563-570.
Steinvorth and all, Temporal lobe arteriovenous
malformations: Surgical management and outcome.
Surgical Neurology. 2002;46:106-114.
Lazar R.M., Connaire K., Marshall R.S. et al.
Developmental deficits in adults patients with
arteriovenous malformations. Arhives of Neurology.
1996;56:103-106.
Steinvorth S., Wenz F., Wildermuth S. et. al. Cognitive
function in patients with cerebral arteriovenous
malformations after radiosurgery: prospective long-
term follow-up. Int J Radiat Oncol Biol Phys.
2002;54(5):1430-7.
Andrea L. Murray, Michael Dally, Aimee Jeffreys, Peter
Hwang «Neuropsychological outcomes of stereotactic
radiotherapy for cerebral arteriovenous malformations»
Journal of clinical neuroscience; 2014; 21(4):601–606.
Buklina S.B. Clinical and neuropsychological syndromes of
arteriovenous malformations of the deep structures of
the brain: Dis. PhD, 2001.
Ernst M, Boers AMM, Aigner A, Berkhemer OA, et al.
Association of computed tomography ischemic lesion
location with functional outcome in acute large vessel
occlusion ischemic stroke. Stroke. 2017;48(9): 2426–
2433.
Charidimou A, Boulouis G, Gurol ME, Ayata C, et.al.
Emerging concepts in sporadic cerebral amyloid
angiopathy. Brain. 2017;140(7):1829–1850.
Yakhno N.N., Levin O.S., Damulin I.V. Cognitive
impairment in the practice of a neurologist. Neurology,
neuropsychiatry, psychosomatics. 2014;(3):32-37.
Luria A.R. Higher cortical functions of a person and their
disturbances in local brain lesion. M.: Academic
project, 2000.— 512 p.
Mendoza G., Merchant H. Motor system evolution and the
emergence of high cognitive functions. Prog Neurobiol
2014;122:73-93. doi: 10.1016/j.pneurobio.2014.09.00
1.
Ellis MJ, Ryner LN, Sobczyk O, Fierstra J. et. al.
Neuroimaging Assessment of Cerebrovascular
Reactivity in Concussion: Current Concepts,
Methodological Considerations, and Review of the
Literature. Front. Neurol. 2016;7:61. doi:
10.3389/fneur.2016.00061
BP. Bandettini, E. Wong, R. Hinks, R. Tikofsky, J.
HydeTime course EPI of human brain function during
task activation Magn. Reson. Med., 25 (1992), pp. 390-
397
Emelin A.Yu. Structural neuroimaging in the differential
diagnosis of vascular cognitive impairment. Russian
military medical academy. 2010;3(31):97–102.
Odinak M.M. Functional neuroimaging in the diagnosis of
dementia. M.M. Odinak, A.Yu. Emelin, A.V.
Pozdnyakov, L.A. Tyutin, G.E. Trufanov, V.A. Fokin,
V.V. Dean, V.Yu. Lobzin. Russian military medical
academy. 2006;1(15):101–11
Lazar R.M., Marshall R.S., Pile-Spellman J., et al. 1997;
Geibprasert S., Pongpech S., Jiarakongmun P., et al.
2010.
Ishikawa M, Kusaka G, Terao S et. al. Improvement of
neurovascular function and cognitive impairment after
STA-MCA anastomosis. J Neurol Sci. 2017;373:201–
207.
Moretti DV, Pievani M, Pini L. Cerebral PET glucose
hypometabolism in subjects with mild cognitive
impairment and higher EEG high-alpha/low-alpha
frequency power ratio. Neurobiol Aging. 2017;58:213–
224.
Barbay M, Taillia H, Nedelec-Ciceri C, Arnoux A, et. al.;
GRECOGVASC Study Group. Vascular cognitive
Clinical Value of Functional MRI in the Diagnosis of Cognitive Disorders in Patients with Arteriovenous Malformations
385

impairment: Advances and trends. Rev Neurol (Paris).
2017;173(7-8): 473–480. 39.
Keefe RSE, Davis VG, Harvey PD, Atkins AS, et.al.
Placebo response and practice effects in schizophrenia
cognition trials. JAMA Psychiatry. 2017;74(8):807–
814.
Roberta La Piana, Samuel Bourassa-Blanchette, Denise
Klein, Kelvin Mok et. al. «Reorganization after
Endovascular Treatment in a Patient with a Large
Arteriovenous Malformation: The Role of Diagnostic
and Functional Neuroimaging Techniques» Interv
Neuroradiol. 2013;19(3):329–338. Published online
2013 Sep 26. doi: 10.1177/159101991301900310.
PMCID: PMC3806008 PMID: 24070082;
Kida Y, Kobayashi T, Tanaka T, Oyama H, Iwakoshi T.
Clinical presentations and MRI findings of
angiographically occult vascular malformations.
Article in Japanese. No Shinkei Geka. 1994
Feb;22(2):141-5.
Bremner, J.D., Vythilingam, M., Vermetten, E. et.al.
Reduced volume of orbitofrontal cortex in major
depression. Biol. Psychiatry 2002;51:273–279.
Cotter, D., Mackay, D., Landau, S., Kerwin, R., Everall, I.
Reduced glial cell density and neuronal size in the
anterior cingulate cortex in major depressive disorder.
Arch. Gen. Psychiatry 2001;58:545–553.
Kublanov, V., Dolganov, A., Aftanas, L., Petrenko, T.,
Danilenko, K., Maria, R., Efimtcev, A., Babich, M.,
Sokolov, A., 2018. Investigation of the
Neuroelectrostimulation Mechanisms by Means of the
Functional MRI: Case Study. In: Proceedings of the
11th International Joint Conference on Biomedical
Engineering Systems and Technologies - Volume 3:
NENT (BIOSTEC 2018). Presented at the Special
Session on Neuro-electrostimulation in
Neurorehabilitation Tasks, pp. 319–324.
doi.org/10.5220/0006712203190324
Kublanov V.S., Petrenko T.S., Efimcev A.A. Application
of Multichannel Electrical Stimulation of the Neck
Nervous Structures in Patients with Depressive
Disorders: An fMRI Case Study. BIOSTEC–2019:
Proceedings of the 12th International Joint Conference
on Biomedical Engineering Systems and Technologies,
Prague, Czech Republic, 22-24 February 2019 /
Portugal: SCITEPRESS, 2019, Vol.5: NNSNT. P. 564–
571. doi.org/10.5220/0007681705640571
Skrobot OA, Black SE, Chen C, DeCarli C, Erkinjuntti T,
Ford GA, Kalaria RN, O’Brien J, Pantoni L, Pasquier
F, et al. Progress toward standardized diagnosis of
vascular cognitive impairment: Guidelines from the
vascular impairment of cognition classification
consensus study. Alzheimers Dement. 2018;14(3):280–
292.
Behrman S, Valkanova V, Allan CL. Diagnosing and
managing mild cognitive impairment. Practitioner.
2017;261(1804): 17–20
NDNSNT 2020 - Special Session on Non-invasive Diagnosis and Neuro-stimulation in Neurorehabilitation Tasks
386
