
Patients to Mobilize Their Data: Secure and Flexible mHealth
Delegation
Rafael Almeida
a
, Pedro Vieira-Marques
b
and Ana Ferreira
c
CINTESIS - Centro de Investigação em Tecnologias e Serviços de Saúde, Faculty of Medicine of Porto, Porto, Portugal
Keywords: Access Control, Delegation, Data Sharing, mHealth, Token-based Authentication, mHealth App.
Abstract: This work describes the development of a prototype of a secure and flexible delegation architecture, to be
applied to an mHealth scenario where a mobile app is used for monitoring and coaching asthma patients. The
motivation is the fact that mHealth apps are not security prepared and patients still have no trust in using them,
on a regular basis. Nonetheless, patients can acknowledge mHealth potential and see the relevance of
sharing/delegating health data to others, e.g., healthcare professionals, depending not only on the necessity
and security, but also on the level of control they can have over it. This proposal empowers the patient to
control, in a flexible, easy and secure way, fine-grained delegation features within a real mHealth setting.
1 INTRODUCTION
Research has confirmed that mobile app users have
security and privacy concerns when using mHealth
apps in their daily lives (Zhou, 2019) (Kotz, 2016),
something that can help justify their low usage and
adherence (Papageorgiou, 2018). Zhou et al.
concluded that mHealth users want to know how
health care providers apply access control to their
data and suggest the development of strong, but easy-
to-use security features, with clear privacy policies, to
encourage mHealth apps’ use (Zhou, 2019).
But this is just one step in the mobile security
chain. Patients should not only trust that authorized
people access their records, but they also need to be
able to securely share and delegate access whenever
and to whomever is necessary. Prasada et al.
identified that patients’ ability to share their personal
data collected via mHealth devices, with their friends,
family, third parties and the public, could limit their
willingness to use mHealth apps and reduce their
adherence and long-term use (Prasad, 2012). On
another study, many participants were reluctant to
share personal information because people
considered health-related information such as
exercise and dietary patterns, as private matters
a
https://orcid.org/0000-0002-5488-8450
b
https://orcid.org/0000-0003-4174-2820
c
https://orcid.org/0000-0002-0953-9411
(Peng, 2016). Although most of the participants were
not favourable to sharing personal information, they
would do it, depending on the necessity, security and
proper mechanisms to control what data and with
whom they would share them (Peng, 2016).
As delegation is needed to meet the requirements
for flexible and responsive access to resources
(Rabehaja, 2019), developers must consider that
mHealth users may change their sharing decisions
over time, as their privacy concerns are not static.
Current research must focus on sensible default
settings and flexible privacy controls for different
recipients (Prasad, 2012), and provide incentives to
foster continued use (Peng, 2016).
The main contribution of this work is a prototype
of a secure and flexible delegation architecture,
applied to a real mHealth setting for controlling and
coaching asthma patients, namely AIRDOC. Patients
can delegate their data with professionals in a simple
yet secure and fine-grained way, providing patient
empowerment to control who accesses what, in terms
of delegation needs.
552
Almeida, R., Vieira-Marques, P. and Ferreira, A.
Patients to Mobilize Their Data: Secure and Flexible mHealth Delegation.
DOI: 10.5220/0008972905520560
In Proceedings of the 6th International Conference on Information Systems Security and Privacy (ICISSP 2020), pages 552-560
ISBN: 978-989-758-399-5; ISSN: 2184-4356
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
2 RELATED WORK
Delegation is a concept that simply translates into
sharing or delegating tasks, duties, or roles
(delegator) to another subject (delegatee) (Schaad,
2002), who will act on behalf of the delegator.
Usually, the delegatee is a third-party outside the
realm of the access control policy defined for that
system. This is why delegation provides flexibility
and dynamism to a fixed access control policy. In
healthcare, delegation can be a necessity, for instance,
for a professional to consult a colleague’s opinion on
a patient’s diagnosis or to verify continuous
monitoring of a chronic patient. Proper security and
privacy must be provided for the patient to trust that
transaction, or the patient’s health outcomes could be
seriously compromised (Boulos, 2014).
The authors did not find in the literature the
implementation of delegation in real mHealth
scenarios. Most delegation works focus on the formal
metamodeling and/or the theoretical extension of
existing access control models (Schefer-Wenzl,
2014). A general overview of the literature for the
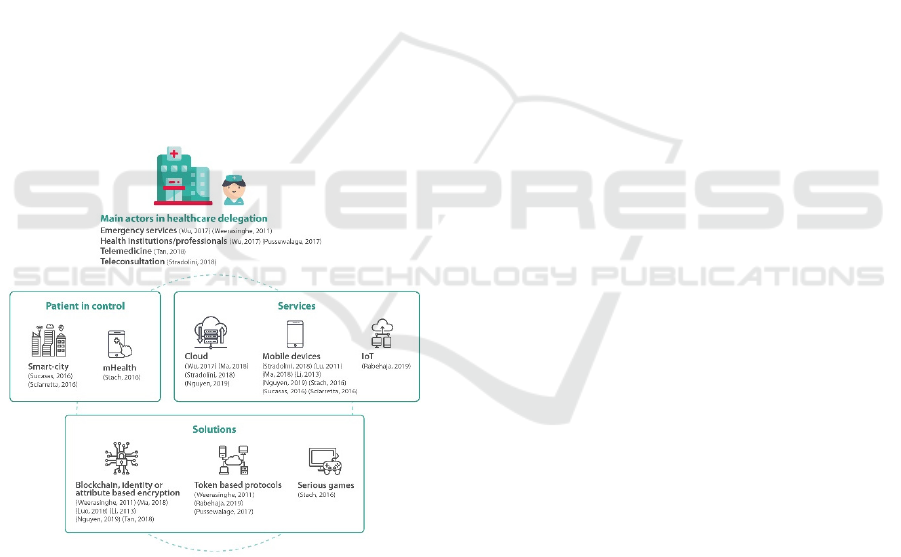
past ten years is shown in Figure 1.
Figure 1: Healthcare delegation actors, used services,
solutions and patient in control – review of last 10 years.
In terms of delegation architectures, those
described in the most recent literature commonly
include cloud services that comprise authentication,
processing and storage services, and constitute also a
middleware to connect both end points (e.g., an EHR
with emergency medical services (Wu, 2017) or
healthcare providers (Weerasinghe, 2011)).
However, using cloud services can hinder a
transparent view on the security controls that are (or
are not) used (Stradolini, 2018). Most cloud privacy
relies on cryptographic protocols but these may not
be used for all services in the cloud system (Li, 2013).
For authentication of the parties and establish
secure and trustable communications, the most used
protocols are OAuth2 (OAUTH 2, 2019) (Sucasas,
2016) (Sciarretta, 2016) (Ferretti, 2017) and token-
based. Since OAuth2 is a tested, light and still reliable
protocol, together with token-based features, this can
be a simple solution to establish a one-time secure
communication channel for temporary delegation
purposes (Weerasinghe, 2011).
For the works which empower the patient to
control what data are shared to other parties, Stach et
al. claims that the user defines what data and how
accurate they are, can be shared with the game,
providing a fine-grained and extendable permission
system (Stach, 2016). However, the patient (children
with diabetes) may not have the dexterity/experience
to decide on what should be shared and how
(especially in sharing their location as provided by the
game features). Another work allows the citizen/user
to authorize the mobile app to access protected
resources, on their behalf (Sucasas, 2016). This work
is not used in practice. Work (Sciarretta, 2016) does
not focus on mHealth, but presents a delegation
mechanism for Smart City mobile apps, which is used
in practice. The solution is based on OAuth2, with a
strong security assessment but with flat grant/deny
delegation options for fixed situations.
Our delegation architecture reuses available and
tested solutions and protocols such as OAuth2 and
openID, with token-based authentication, so it does
not rely on a cloud-based architecture, and is
implemented in a real mHealth setting.
3 METHODS
A literature review was performed to find techniques
used to implement delegation and retrieve the
requirements that could be applied to our use case
scenarios. The search was performed in July 2019 in
the IEEE Xplorer, ACM and Scopus online databases,
of articles published after 2009 (last ten years) with
search terms such as: “sharing or delegation patient
and health professional mobile app”; “delegation
mobile”; “delegation mobile health”. Titles and
abstracts were reviewed by one researcher and those
which referred to sharing and/or delegation of
mHealth (mobile and/or IoT) data with professionals
or other health related entities, were included. Twenty
papers were selected to be read fully and, after the
Patients to Mobilize Their Data: Secure and Flexible mHealth Delegation
553
analysis, a total of 14 papers were included in the
review for further perusing secure delegation
architectures to identify necessary requirements (2
papers were not directly related to the subject; 2 were
similar from the same authors but published on
different places; and 2 others were not describing
delegation schemes but analysed mHealth and
sharing perceptions and needs).
The following step was to define personas
associated with the main use cases for the domain
where those were going to be applied (section 4).
Then a new delegation approach was defined to
face the specific AIRDOC requirements. A prototype
was implemented and tested within a mobile app
simulation (sections 4 & 5).
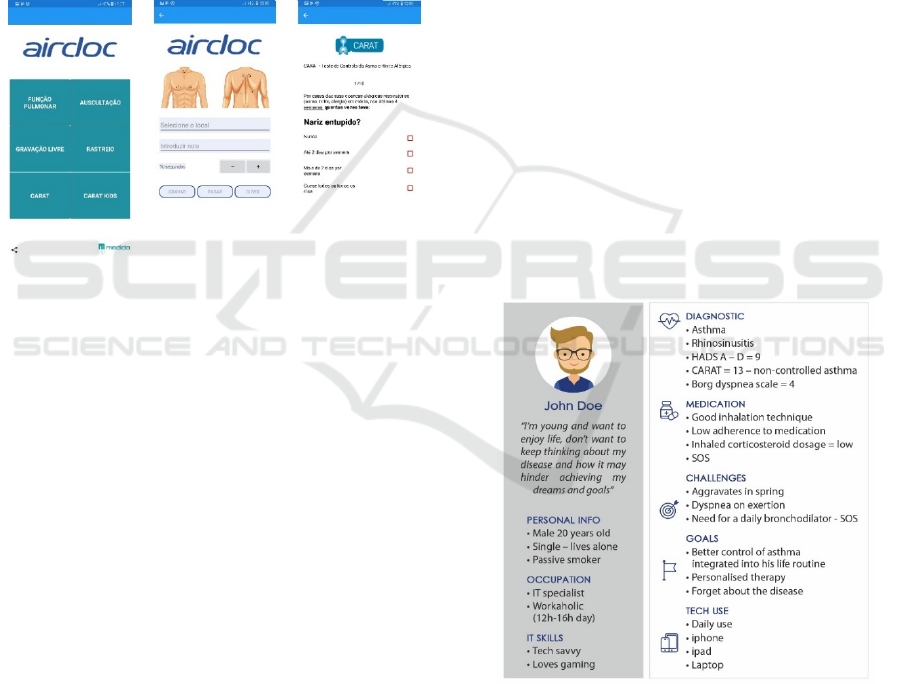
Figure 2: AIRDOC mHealth app screenshots: first menu
page, symptoms location and CARAT survey (left to right).
4 AIRDOC – THE mHEALTH APP
4.1 AIRDOC - The Project
The project AIRDOC aims to develop a Smart Mobile
Application for Individualized Support and
Monitoring of the Respiratory Function and Sounds
of Chronic Obstructive Patients (CORD) (AIRDOC,
2018). Current tools for CORD self-monitoring and
self-managing are complex, unattractive, not
individualized and require laborious analysis by
health professionals, discouraging their use and
integration. AIRDOC wants to make use of the
ubiquitous presence of smartphones in everyday life,
their embedded sensors (e.g., microphone) as well as
their processing and communication abilities.
AIRDOC aims also to focus on security, privacy and
interoperability requirements to impact on the
innovation of CORD healthcare, with increased
patient involvement and empowerment (Figure 2).
4.2 Use-Case Delegation Scenario
The success of the AIRDOC project mostly depends
on the simple, but also, secure and private integration
and communication between patients, health
professionals, family and friends, for supporting the
patient in their daily health monitoring capabilities.
For this, the functionality of delegation is one of the
first to be integrated within its access control model.
This section presents a use-case of a persona who
needs to use the AIRDOC mHealth application
(AIRDOC app) as a self-monitoring device and
shares data with his/her health professional.
4.2.1 Persona
For applications to be more successful and used on a
daily basis, they need to represent the users that are
going to be engaged and benefit from the application,
and not what the developers think is needed. A
persona puts a face and personal contextual attributes
to that user (all fictitious), who represents the target
population (Platt, 2016). A photograph and
demographic data - such as name, age, gender, marital
status, occupation, education, IT skills, health history
and how the mHealth application might achieve their
goals - are associated to the persona. Figure 3 presents
the persona for our use case (Section 4.2.2).
Figure 3: Persona describing a patient use-case for the
AIRDOC mHealth application.
4.2.2 Use-Case Description
The persona is an Asthmatic who wants to delegate
access to his health monitoring data, stored within the
AIRDOC app, to the professional who has been
treating him or to another professional, not directly
ICISSP 2020 - 6th International Conference on Information Systems Security and Privacy
554
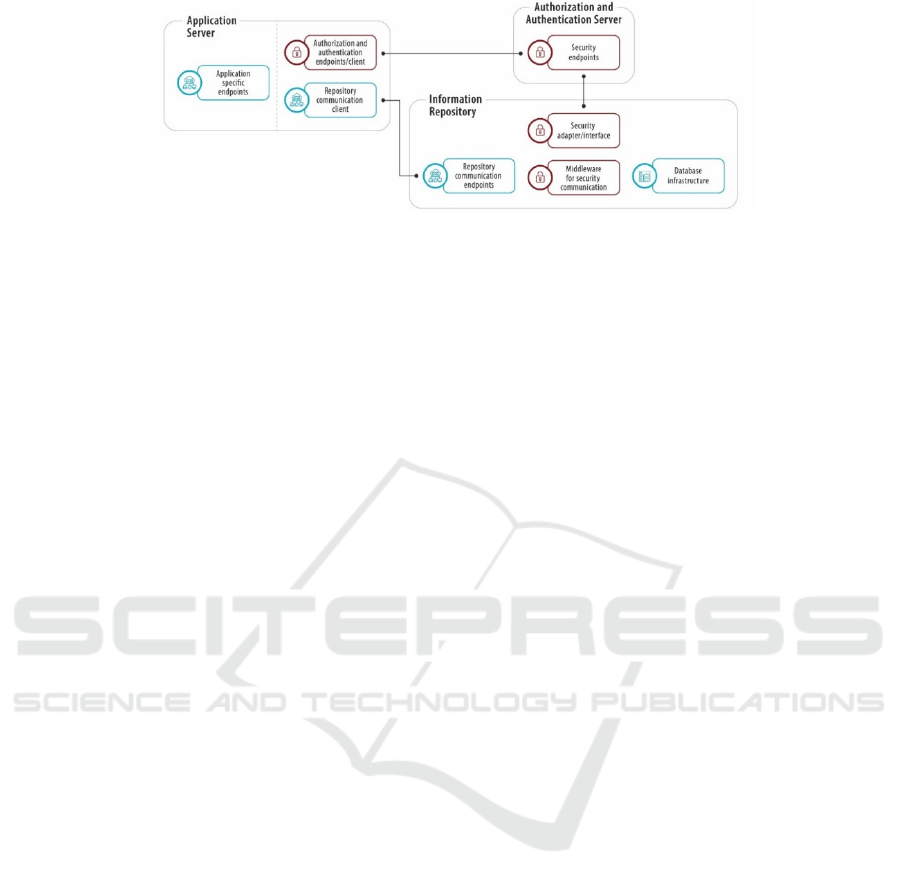
Figure 4: Architecture of the mHealth delegation AIRDOC prototype.
related to his treatment, but who can be helpful, at a
certain moment, about his condition (Figure 3).
Delegation Scenario: John is having trouble
controlling asthma symptoms lately so he is going for
a consultation with another specialist recommended
by a friend. At the consultation, the doctor verifies
that John can probably beneficiate from a tool that can
be integrated into his routine activities and use of
technology, in order to closely control symptoms,
medication adherence and improve recommendations
at any moment. She tells John to install the AIRDOC
app, an asthma coaching mHealth app to help him
follow medication plans and adopt suggested
behaviours for controlling asthma. In order for the
doctor to closely monitor the first months of
Johns’new therapy, John installs the app and decides
to activate the delegation feature:
1. John opens and accesses the AIRDOC app, and
starts the delegation functionality to delegate his
data to a “related” professional, someone who is
following him at the moment
2. John must insert a code in the app, given by the
doctor, as a means to securely identify John to
that doctor
3. Doctor’s AIRDOC app asks if she accepts to
receive data from that patient
4. The doctor accepts
5. A message is sent to both John and the doctor
asking them to revise and confirm the data that
are going to be shared, and with what parties
6. John and the doctor must agree to delegation
terms and conditions to finalize the delegation
process
7. Authentication messages and/or tokens are
exchanged, and access to John’s data is delegated
to the doctor
8. Secure communications are established and
delegation is set for a pre-defined period of time,
or until any of the parties revoke the request.
5 DELEGATION PROPOSAL
5.1 Delegation Architecture
Figure 4 presents the main components of the
developed architecture delegation prototype. These
comprise an: 1) Application Server, responsible for
supplying the application with the necessary request
resources and/or information; 2) Authorization and
Authentication Server, the main responsible for
security communications of the whole architecture;
and 3) Information Repository.
The authentication procedure is implemented with
the OAuth2 protocol together with the Authorization
and Authentication Server, using a hybrid flow,
which is a combination of implicit and authorization
flow. This server contains basic user and role
information (login/pass), as well as an identifier for
user identification, authentication and authorization
to the AIRDOC app. The Information Repository
contains all medical and personal data.
When a request is received from the app, it is
intercepted by the “Middleware for security
communication” component, which directs the: a)
authorization token, b) the type of CRUD action (e.g.,
create, read, update, delete, or other), c) the type of
accessed resource, d) the resource identifier and e)
any parameters on the request query, onto the
“Security adapter/interface”. This component
contains: a) a client to communicate with the security
server using introspect endpoints which validate the
security token, and retrieve the user’s ID and role; b)
configurable role permissions; and c) the
ownership/delegation verification pipeline process.
Security server information is used to setup the
client and the general role permissions, using a Role
Based Access Control model, by validating the
retrieved user’s role and intended action. This is
required to implement the interfaces of the methods
used during the ownership/delegation verification
pipeline process, in order to tell the system how to
Patients to Mobilize Their Data: Secure and Flexible mHealth Delegation
555
search for user’s security details. This verification
uses context specific implementations to determine
who is the data owner, and if there is any delegation
using that same data, in the repository.
5.2 Delegation Prototype
Specific to the delegation prototype, the described
components comprise various technologies:
Authorization and Authentication Server: uses
the Identity4 framework, which includes both
OAuth2 and
openID protocols. This is used to create
our own identity server to contain core user
information and recognized roles to be applied during
the authorization process;
Application Server: a simple NodeJS stub server
was used to simulate the OAuth2 protocol steps and
perform information requests to verify ownership and
delegation;
Information Repository: most of the work was
implemented here for the storage needs of the
repository to comply with the prototype goals, which
the application server could request, as well as keep
track of user’s relations (where applicable), and
between stored information. It also maintains a
register of all the delegation processes.
All of these characteristics and requirements led
to the decision of using the FHIR standard (FHIR,
2011). This standard allows the information regarding
user, and associated roles to be stored on FHIR
resources called Person, Patient, Related Person and
Practitioner. To implement the delegation
functionality and store related data on FHIR, a
resource named Consent is created. This resource was
designed to formally describe a given authorization
by a resource owner, to another actor in the system,
detailing what information is shared and what type of
access is given. For the actual prototype
implementation, the HAPI-FHIR framework (HAPI-
FHIR, 2014) was chosen because it introduces most
required functionalities to build a working prototype
in JAVA language. As for the database, considering
that FHIR naturally allows the use of JSON to
describe and communicate data, we decided to use the
nosql database MongoDB, in which JSON documents
can be directly stored, with no extra processing work.
5.2.1 Generic Communication Flow
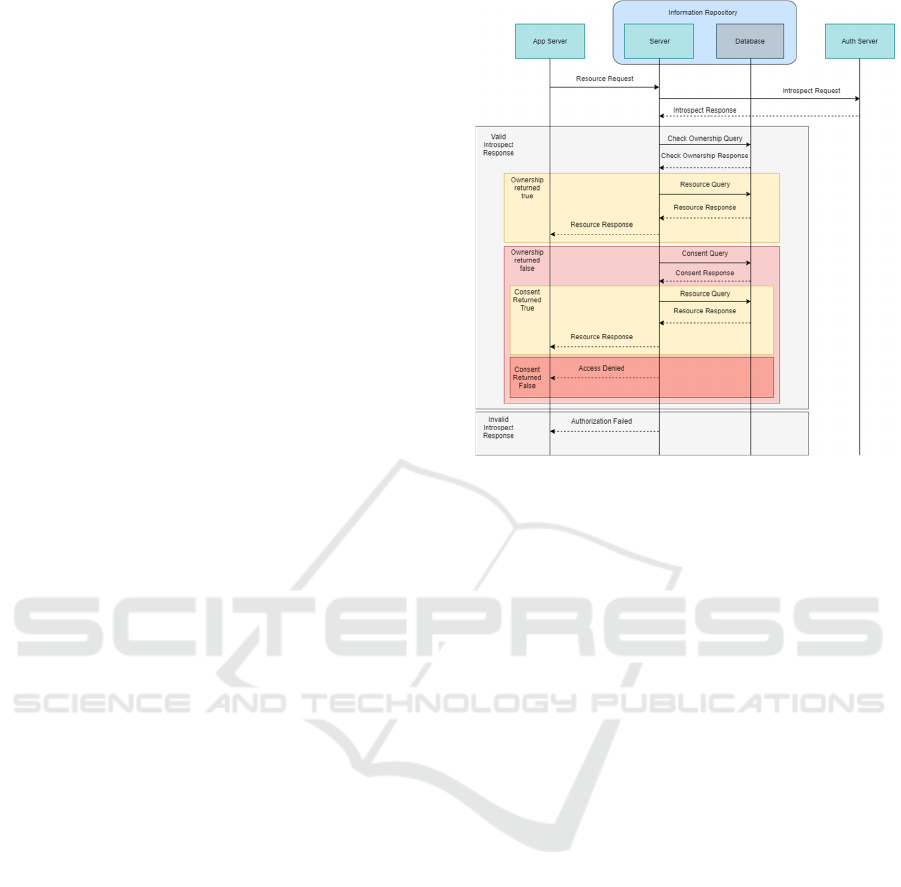
Figure 5 shows the communication flow and queries
performed between the components of the
architecture, to generally execute a resource request,
as well as what differs in the communication, when
the request is a delegation request (pink rectangle).
Figure 5: Generic activity diagram to perform the use-case
delegation procedure described in section 4.
Steps for this execution are the following:
• Resource Request: the user accesses the
AIRDOC app and requests access to resources – since
it is using REST standard, it should contain the
resource(s) ID and type, along with the security token
created earlier for the user;
Introspect Request: request for the security
token validation, user (security) id and role
information;
Check Ownership Query: an implemented
interface method which asks the information
repository for the internal and security ID of the
owner. If retrieved security ID is the same as the one
retrieved from the introspect request, we can assume
it is indeed the owner and proceed with the resource
request. Otherwise it is required to check for
delegation consent;
Consent Query: another implemented interface
method which uses the resource request security ID,
retrieves the system ID of the user, to be used with the
resource owner system ID, to verify the existence of
any active delegation consent. If such consent exists,
the resource request may proceed. Otherwise an
unauthorized access should be issued. Later work
should be done to parse the consent for specific
content details authorization.
5.2.2 Delegation Communication Flow
For the delegation process to be possible, both entities
(Actor A and Actor B – Figure 6) need to already be
ICISSP 2020 - 6th International Conference on Information Systems Security and Privacy
556
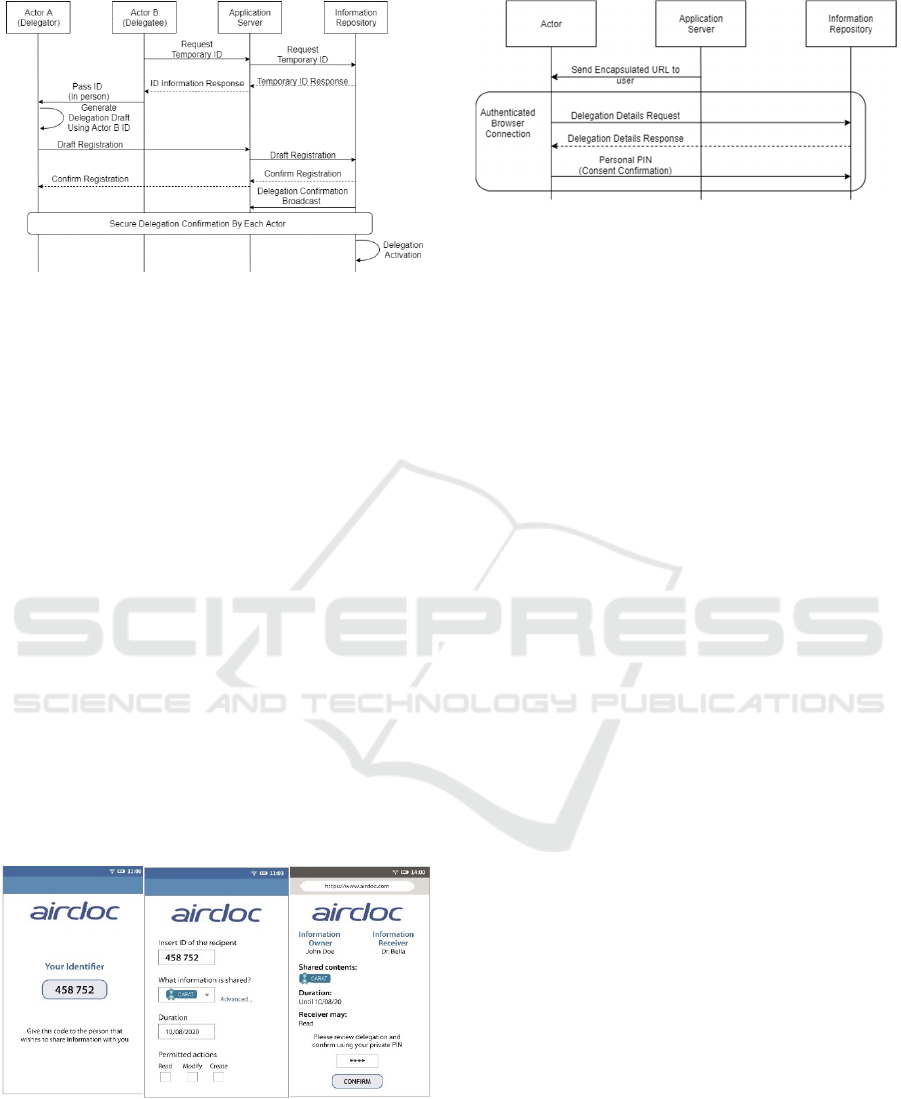
Figure 6: Activity diagram - delegation request.
recognized on the information repository, which in
the context of the prototype, means to already have a
Person resource created for each actor, ready to be
used for delegation rights assignment. For most of
this process, the application server acts only has a
middlelayer, passing the requests received from the
application onto the information repository.
To start the delegation process, Actor B, or the
delegate, the health professional, henceforward called
Doctor Bella, requests a temporary ID to be issued
from the application server. This ID should be human
readable, since, when received by Doctor Bella, it is
passed, in person, to actor A, or the delegator, in this
case the patient, John Doe (Figure 7 - left). With that
temporary ID, John can build a delegation draft where
he gives the required permissions to the ID, given to
him by the Doctor, but still, for the moment,
unrecognized by the application (Figure 7 - middle).
The delegation draft is then communicated to the
information repository via the application server.
Once on the repository, the temporary ID is replaced
by Doctor Bella’s formal ID and the draft is stored in
the database, waiting for confirmation.
Figure 7: AIRDOC app - Doctor Bella’s temporary ID,
passed on to John (left); the patient drafts the delegation
consent for Doctor Bella (middle); delegation consent draft
sent to all delegation parties, for confirmation with a
personal PIN, previously set (right).
Figure 8: Activity diagram – delegation confirmation.
To perform the confirmation (Figure 7 - right), an
URL address pointing to the delegation draft is passed
onto the application server, which is responsible to
broadcast that draft to the mobile application of all the
actors involved. The application should pass the URL
onto the device’s browser which opens a view to the
delegation draft and a confirmation box to allow both
the patient and the health professional to confirm or
deny the operation. To do this, they use a personal
pin, which allows them to validate their identities
using a communication channel directly from the
device, to the information repository (Figure 8). This
part of the process is similar to existing OAuth2 flows
of authentication, while additional security methods
can also be included in this process.
6 DISCUSSION
As previous research has shown, users want more
control over who accesses their health data, as well as
easy to use, but also strong security features to
accomplish that. The same applies to delegation
situations, which are increasing in the world of
mobile app with anytime/anywhere accesses.
However, there is concern in not sharing out their
health data to third parties, and even family and
friends, by default. There is evidence that patients
will want to do it, but want to delegate their data
whenever they see necessary, and in a controlled
manner, always verifying what and to whom they will
share them with (Peng, 2016).
Most existing research in the area of mHealth
delegation is just proof of concept and very few cases
are tested in real scenarios. Our work is being
developed in the ambit of a project which aims to
implement and make use of a mobile app for
monitoring and coaching chronic patients with
respiratory diseases. The developed app will be
available in online stores for download and use, and
several studies with real patients from various
healthcare organizations, will be performed within
the timeframe of the project’s duration.
Patients to Mobilize Their Data: Secure and Flexible mHealth Delegation
557

In terms of architecture and technologies used,
most are reused from existing well tested
technologies, e.g., OAuth2 and openID for
authentication and authorisation, which introduces
the use of token-based authentication. The main
advantage of token-based authentication is allowing
to use a reduced amount of credentials. It does this by
utilizing a single point for logging in, which generates
access tokens accordingly, to be used by the
application server to access the secured information
repository. This is done with authorization from the
user, the owner of the information, and also
refreshing tokens to maintain sessions, without the
use of credentials. Another advantage is the ease to
make identified third-party servers communicate with
the secured repository. An example is the hybrid flow
which is designed to force the application server to be
registered as a client in the OAuth2, implying that the
user would still have to use the credentials directly
with the OAuth2 server, and explicitly authorize the
third-party server, to perform requests in their name.
Meanwhile, the use of openID frameworks,
permits the creation of an identity server to be used
alongside the OAuth2 protocols, adding information
such as the user role in the system. Furthermore, and
since interoperability in healthcare is a must
requirement, FHIR, an already developed and
implemented standard for health information, is used
to store and communicate clinical related data. This is
a step forward to communicate with other clinical
information repositories, such as the ones used in
hospitals, or similar health related applications, while
also helping in the dissemination of standardized
clinic information. Being a well-known and
increasingly used standard, there is significant
previous work in the stability of the standard and on
the structures to contain as much as relevant and
organized information, as possible.
As for the delegation process, some analysis on
the security requirements and properties defined
during the work, is necessary. In order to start the
delegation, it is required that both parties can identify
each other. Although at the beginning of the process
an anonymous ID is used to link them, prior to the
confirmation step, the information repository is able
to replace the anonymous ID with an identification
used within the system, related to the person that
requested that ID. This method allows the patient for
later confidently identify the person/delegatee to
whom he is going to share information with. This
way, there is no need to depend on sharing permanent
IDs during all these communications, which could be
reused on, for example, a replay attack.
Afterwards, there is the problem of allowing all
parties relevant to the delegation process to confirm
the delegation consent and its contents. We used a
native property on FHIR resources that allows to
define the active state of each instantiated resource as:
draft, proposed, active, rejected, inactive or entered-
in-error. At this stage, we were studying the
possibility of using the draft state for when a consent
defining a delegation permission is uploaded into the
information repository. After this upload, we would
mark the draft in the waiting state, until all involved
parties confirm their authorization regarding the
consent contents, which would then imply changing
it to the active or rejected state. However, the
confirmation step should not be performed using the
application server, since confirmation of identity and
authorization is critical, so it should be as secure as
possible. Our proposed solution is based on how the
OAuth2 protocol works, where a similar method is
used in which a URL address is transmitted to the
users, with the same intent as when the application
server redirects authentication requests to the OAuth2
server. In practice, this opens an HTTPS connection
with the information repository, which can be
considered a secure channel for the user to review the
consent, validate it and confirm the authorization
using a previously registered PIN to confirm their
identity.
Limitations. A limitation of this work is the small
number of related research with applied mHealth use-
cases, available for comparison and discussion. Also,
due to the lack of space, it was not possible to show
varied use-cases, with different personas, and more
fine-grained delegation features. Finally, this work is
still in the prototype phase and requires usability and
reliability tests with end users, for its final evaluation.
However, this limitation will be overcome within the
lifetime of the project (AIRDOC, 2018), as already
described, tests will be performed with real patients,
enrolled in various healthcare organizations, before
the AIRDOC app goes online.
7 CONCLUSIONS
The presented delegation prototype sets the path for a
more flexible, easy and empowered way to provide
secure delegation to patients, in real mHealth settings.
This is a very relevant requirement with chronic
disease patients, to securely share/delegate their
continuous monitoring data to healthcare
professionals, or others who can support them. The
goal is to improve patients’ adherence to medication
and therapeutics to achieve better healthcare
outcomes. Our solution can be applied in any similar
ICISSP 2020 - 6th International Conference on Information Systems Security and Privacy
558

mHealth scenario as the security framework was
developed in a modular and independent way, using
available and well tested standards and technologies.
As future work, the solution will be validated for
its content, usability as well as legislation and privacy
requirements, and will integrate into the SoTRAACE
model (Moura, 2017). SoTRAACE allows to include
features that take into account a risk-based
personalized and contextual based decision, adapted
to every mHealth interaction. Delegation can be one
of those useful features on the way to a more patient
empowered, dynamic, usable and secure mHealth.
ACKNOWLEDGEMENTS
This work is supported by project NORTE-01-0247-
FEDER-033275, financed by the North Portugal
Regional Operational Programme (NORTE 2020),
under the PORTUGAL 2020 Partnership Agreement,
and through the European Regional Development
Fund (ERDF). A. Ferreira is also with TagUBig -
Taming Your Big Data (IF/00693/2015) from
Researcher FCT Program funded by National Funds
through FCT.
REFERENCES
AIRDOC, 2018. AIRDOC - Smart Mobile Application for
Individualized Support and Monitoring of the
Respiratory Function and Sounds of Chronic
Obstructive Patients. Available at:
http://cintesis.eu/en/portfolio-items/airdoc/ (Accessed:
September 2019).
Boulos, M., Brewer, A., Karimkhani, C., Buller, D.,
Dellavalle, R., 2014. Mobile medical and health apps:
state of the art, concerns, regulatory control and
certification. Online J Public Health Inform, 5, pp. 229-
229.
Ferretti, L., Marchetti, M., Colajanni, L., 2017. Verifiable
Delegated Authorization for User-Centric
Architectures and an OAuth2 Implementation. In IEEE
41st Annual Computer Software and Applications
Conference (COMPSAC), pp. 718-723.
FHIR, 2011. Fast Healthcare Interoperability Resources.
Standard for health care data exchange, published by
HL7®. Available at: https://www.hl7.org/fhir/
(Accessed October 2019).
HAPI-FHIR, 2014. Open-source implementation of the
FHIR specification in Java. Available at:
https://hapifhir.io/. (Accessed October 2019).
Kotz, D., Gunter, C., Kumar, S., Weiner, J., 2016. Privacy
and security in mobile health: a research agenda.
Computer, 49(6):22-30.
Li, L., Huang, D., Shen, Z., Bouzefrane, S., 2013. A Cloud
based Dual-Root Trust Model for Secure Mobile Online
Transactions. In IEEE Wireless Communications and
Networking Conference (WCNC), pp. 4404-4409.
Lu, J., Zhou, J., 2011. Preventing delegation-based mobile
authentications from man-in-the-middle attacks.
Computer Standards & Interfaces, 34, pp. 314-326.
Luo, J., Dong, Q., Huang, D., Kang, M., 2018. Attribute
Based Encryption for Information Sharing on Tactical
Mobile Networks. In IEEE Military Communications
Conference (MILCOM), pp. 1-9.
Ma, H., Zhang, R., Yang, G., Song, Z., He, K., Xiao, Y.,
2018. Efficient Fine-Grained Data Sharing Mechanism
for Electronic Medical Record Systems with Mobile
Devices. In IEEE Transactions on Dependable and
Secure Computing, pp. 1-1.
Moura, P., Fazendeiro, P., Vieira-Marques P., Ferreira, A.,
2017. SoTRAACE — socio-technical risk-adaptable
access control Model. In 2017 International Carnahan
Conference on Security Technology (ICCST), pp. 1–6.
Nguyen, D., Pathirana, P., Ding, M., Seneviratne, A., 2019.
Blockchain for secure EHRs sharing of mobile cloud
based ehealth systems. IEEE Access, 7, pp. 66792-
66806.
OAUTH 2, 2019. OAuth 2.0 [online]. Available at:
https://oauth.net/2/ (Accessed: August 2019).
Papageorgiou, A., Strigkos, M., Politou, E., Alepis, E.,
Solanas, A., Patsakis, C., 2018. Security and privacy
analysis of mobile health applications: the alarming
state of practice. IEEE Access, 6:9390-9403.
Peng, W., Kanthawala, S., Yuan, S., Hussain, S., 2016. A
qualitative study of user perceptions of mobile health
apps.
BMC Public Health, 16.
Platt, D., 2016. The Joy of UX – User Experience and
Interactive Design for Developers. Addison-Wesley.
Prasad, A., Sorber, J., Stablein, T., Anthony, D., Kotz, d.,
2012. Understanding sharing preferences and behavior
for mHealth devices. In Proceedings of the 2012 ACM
workshop on Privacy in the electronic society, pp. 117-
128.
Pussewalage, H., Oleshchuk, V., 2017. Attribute based
access control scheme with controlled access
delegation for collaborative E-health environments.
Journal of Information Security and Applications, 37,
pp. 50-54.
Rabehaja, T., Pal, S., Hitchens, M., 2019. Design and
implementation of a secure and flexible access-right
delegation for resource constrained environments.
Future Generation Computer Systems, 99, pp. 593-608.
Schaad, A., Moffett, J., 2002. Delegation of Obligations. In
Proc. of the 3rd International Workshop on Policies for
Distributed Systems and Networks, pp. 25-35.
Schefer-Wenzl, Sigrid., Bukvova, H., Strembeck, Mark.,
2014. A Review of Delegation and Break-Glass Models
for Flexible Access Control Management. Lecture
Notes in Business Information Processing, 183.
Sciarreta, G., Carbone, R., Ranise, S., 2016. A delegated
authorization solution for smart-city mobile
applications. In IEEE 2nd International Forum on
Patients to Mobilize Their Data: Secure and Flexible mHealth Delegation
559

Research and Technologies for Society and Industry
Leveraging a better tomorrow (RTSI), pp. 1-6.
Stach, C., 2016. Secure Candy Castle - A Prototype for
Privacy-Aware mHealth Apps. In 17th IEEE
International Conference on Mobile Data Management
(MDM), pp. 361-364
Stradolini, F., Tamburrano, N., Modoux, T., Tuoheti, A.,
Demarchi, D., Carrara, S., 2018. IoT for Telemedicine
Practices enabled by an Android™ Application with
Cloud System Integration. In IEEE International
Symposium on Circuits and Systems (ISCAS), pp. 1-5.
Sucasas, V., Mantas, G., Radwan, A., Rodriguez, J., 2016.
An OAuth2-based protocol with strong user privacy
preservation for smart city mobile e-Health apps. In
IEEE International Conference on Communications
(ICC), pp. 1-6.
Tan, Z., 2018. Secure Delegation-Based Authentication for
Telecare Medicine Information Systems. IEEE Access, 6,
pp. 26091-26110.
Weerasinghe, D., Muttukrishnan,R., et. al., 2011. Secure
Trust Delegation for Sharing Patient Medical Records
in a Mobile Environment. In Proceedings of 7th
International Conference on Wireless
Communications, Networking and Mobile Computing,
pp. 1-4.
Wu, X., Dunne, R., Yu, Z., Shi, W., 2017. STREMS: A
Smart Real-Time Solution toward Enhancing EMS
Prehospital Quality. In IEEE/ACM International
Conference on Connected Health: Applications,
Systems and Engineering Technologies (CHASE), pp.
365-372.
Zhou, L., Bao, J., Watzlaf, V., Parmanto, B., 2019. Barriers
to and Facilitators of the Use of Mobile Health Apps
From a Security Perspective: Mixed-Methods Study.
JMIR Mhealth Uhealth, 7(4): e11223.
ICISSP 2020 - 6th International Conference on Information Systems Security and Privacy
560
