
Status of Resources for Information Technology to Support Health
Information Exchange in Resource-constrained Settings
Andrew Alunyu Egwar
1,2
, Richard Ssekibuule
2
and Josephine Nabukenya
2
1
Department of Computer Engineering, Busitema University, Tororo, Uganda
2
Department of Information Systems, Makerere University, Kampala, Uganda
Keywords: eHealth, Communication Resources, Health System, ICT, LMICs.
Abstract: Various resources exist to support health information exchange (HIE). Both computerised and
uncomputerized communication resources continue to be used in resource-constrained environments, like the
Uganda health system to support HIE. Despite the rapid shift to the digital health environment, the resource
capabilities of health systems in LMICs to support robust HIE is unknown. This study surveyed the status of
resources for ICT to support ehealth communication in a resource-constrained setting. The study was
conducted in three districts, representing the urban, peri-urban and rural settings of Uganda. The qualitative
data collected was analysed with QSR NVivo 10. Results show major resource challenges including financial
constraints, funders restrictions, human resource limitations, isolated computer systems, lack of support from
management, legacy/outdated systems, intermittent/limited network bandwidth, limited hardware,
misuse/poor maintenance of the available hardware, and power outages among others. In addition, results
show a great disparity in their distribution across the healthcare sector. Therefore, we argue that much
improvement is needed if the benefits of ehealth are to be attained in LMICs. Recommendations include
specifying minimum resources for ICT required to support HIE, supervising implementation and monitoring
compliance to the standards, establish a mechanism for periodic review of the minimum standards, and finally,
align ICT funding within the mainstream funding for healthcare services. It should uniformly apply across
the board (i.e., facilities located in urban, peri-urban and urban) for the full benefits of ICT in health to be
achieved in LMICs.
1 INTRODUCTION
Low- and middle-income countries (LMICs) lag in
development and lack of resources for the wellbeing
of all (Andrews et al., 2012). The resource challenges
extend to shortages in the healthcare system.
However, ICT has found multiple applications in
LMICs as they attempt to alleviate current resource
shortages limiting service delivery in their healthcare
sector, transportation, and governance among others.
In fact, in their ICT policy document, Uganda’s
ministry of ICT identified applications of ICT for
sustainable development to span the fields of public
administration, business, education and training,
health, employment, environment, agriculture,
petroleum, science, oil and gas, as well as linguistic
and cultural diversity (Uganda’s MoICT, 2014).
Particular to this study, is the need to leverage
challenges in healthcare like high patient-physician
ratio, variable quality of care, limited medical
equipment, high cost of healthcare, corruption/fraud,
and patient monitoring problem (Lewis et al., 2012;
Madinah, 2016) by adopting ICT in support of health
information exchange (Peña-López, 2010).
According to Health ICT Industry Group, (2009)
ICT can help support Electronic Health Records
(EHR), Chronic Disease Management Systems,
Computerised Practitioner Order Entry (CPOE),
Clinical Decision Support, Electronic Transfer of
Prescription, Electronic Appointment Booking,
Personal Health Record, Telemedicine, and RFID and
Bar-coding. In fact, the use of ICT in healthcare are
categorised into health education, hospital
management system, health research, and health data
management (FrontEnders Healthcare Services Pvt.
Ltd, 2016; Lewis et al., 2012). These are geared
towards alleviating healthcare resource challenges, a
problem more pronounces in LMICs. Contrary to a
report by Lewis et al., (2012) that ranked sub-Sharan
Africa the third-best in use of technology-enabled
Egwar, A., Ssekibuule, R. and Nabukenya, J.
Status of Resources for Information Technology to Support Health Information Exchange in Resource-constrained Settings.
DOI: 10.5220/0008970004630471
In Proceedings of the 13th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2020) - Volume 5: HEALTHINF, pages 463-471
ISBN: 978-989-758-398-8; ISSN: 2184-4305
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
463

programmes as a percentage of all programmes, these
mostly LMICs continue to grapple with resource
shortages in Healthcare.
Central to the use of ICT to support health
(ehealth) is the communication infrastructure and
supporting resources. In fact, the use cases are
facilitated by a communication infrastructure with
resources suitable to meet the stringent requirements
in a healthcare environment. However, the ICT itself
continue to face challenges in LMICs including
resource limitations, security and privacy concerns
(Blantz, 2010; Dhital, 2018). These constraints on
ICT has a bearing on their application to healthcare.
According to Blantz (2010), the resource challenges
range from connectivity problems, power shortages to
human and other nontechnical challenges. Among
these are challenges specific to ehealth infrastructure
intended to support health data handling and or
information exchange. However, resource challenges
may not be uniform across the healthcare system.
Resources distribution in LMICs tends to be along
the urban, peri-urban and rural divide. No matter the
kind of resource, they are spread across the structural
divide, with better resources reducing from developed
to least developed countries, from urban to rural
settings (Henry, 2019; Jere et al., 2013; Kuntagod et
al., 2014). Therefore, the resources for the
communication infrastructure supporting ehealth
need to be investigated across the general resource
distribution divide. Our consideration of resources
stems from the summarised definition of resources by
Alvaro et al., (2010) from the conservation of
resource theory. They believe resources are objects,
conditions, personal characteristics, and energies that
are valued for survival or that serve as a means of
achieving these resources (Alvaro et al., 2010).
Mindful that health information exchange needs to
take place irrespective of the locality of the health
facility; adequate data communication resources that
span physical, structural and energy (Alvaro et al.,
2010) are required to support such exchanges.
According to Alvaro et al., 2010, the three major
concepts of Conservation of Resources (COR) theory
that apply to this study are; one, resources are
required for adaptation and change. Healthcare
systems need to adapt to the electronic transfer of
health data. Two, the threat of loss leads to the
protection of assets/resources in this case protection
of the CIT resources and data involved in the
exchange. Three, resources must be optimized for
adaptation. Given the resource-constrained, there is a
need to optimise the available resources to achieve
HIE in LMICs.
1.1 Health Information Exchange
It is the role of delivery systems and communities who
intend to exchange health information, to set up the
communication infrastructure (McCarthy et al., 2014)
for such exchange. Health information exchange (HIE)
is the secure, electronic movement of health-related
information in a standard format between disparate
sources and users (Williams et al., 2012). To facilitate
HIE, existing communication resources need to be
robust to be able to support healthcare processes and
data communication. In this regard, the
communication infrastructure both within and across
health facilities must be properly designed and
implemented to support healthcare processes and data
exchange. Thereby supporting HIE to improve clinical
decision-making and continuity of care, while reducing
unnecessary use of services (McCarthy et al., 2014).
1.2 Why eHealth Communication
Resources?
Other studies have used or identified among other
resources sufficient storage, transport capacity (data
communication bandwidth), state-of-art hardware as
required to support health data sharing/
communications (Dixon, 2016; Sewell, 2014). The
scarce telecommunication resources like the spectrum,
numbering, and rights of way (Uganda’s MoICT,
2014) may be considered per implementation of a
communication system. To meet the time requirements
of health data, the data communication system/network
needs to be robust. In addition, network availability
and performance are considered very critical in
healthcare (Juniper Networks, 2015). In fact, Sewell,
(2014) argues that sufficient network capacity and
speed are critical for supporting current and future
healthcare technologies and applications. In fact,
Dixon, (2016) argues strongly for sufficient storage as
well as transport capacity for data and or information
exchange. Therefore, we argue that the capacity of the
communication infrastructure is dependent on these
resources, i.e., storage, transport capacity/ bandwidth,
the spectrum, available hardware, and of course
associated software platforms. If the health data
communication infrastructure is to be robust, the
design and implementation of ICT systems used within
the healthcare facility, cabling and choice of cable
category, implementation of interfaces that request
access to health records, establishment of the modes of
information exchange, security, access privileges and
privacy, must follow strict guidelines.
To investigate the factor of resources that
influence implementation of ehealth in LMICs, the
HEALTHINF 2020 - 13th International Conference on Health Informatics
464

study sought to answer the research question of what
minimal communication resources are required to
support sharing of Health Information in resource-
constrained settings, the study explores the following
questions: (1) what is the perception of healthcare
practitioners in resource-constrained settings regards
role of ICT in health? (2) what ehealth
communication infrastructure resources are currently
available to resource-constrained settings? (3) what
healthcare processes can the current ICT resources
support? And (4) what are the recommended
improvements to communication resources to support
HIE in low resourced environments?
The rest of the paper is organised as follows:
Section 2 presents the methodology followed to
conduct the study. In Section 3, we present the results
of the survey of the current status of resources that
support electronic health communication
infrastructure in Uganda. Finally, we discuss the
results of the survey in Section 4 before presenting
the conclusions and future works in Section 5.
2 METHODS
This was a qualitative study of communication
resources that support HIE. The study involved, one,
a literature review of health informatics literature
from PubMed Central and Google scholar regards
resources for ehealth communication in LMICs or
developing countries. The literature review
considered both peer-reviewed and grey literature
that considered resources for ehealth communication
to support HIE. We also reviewed the state of ICT
resources that may support HIE in four LMICs.
Two, an exploration of communication resources
available to health facilities in Uganda’s health system
to understand their support for healthcare processes
and identify any resource limitations. Only health
facilities at the level of health centres IV, district
hospitals and regional referral hospitals were included
in the survey. Nine health facilities were purposively
chosen from the central, eastern and northern Uganda.
The basis of choice is, first, on the basis that they
handle a high volume of patients. Second, Uganda’s
ministry of health (MoH) and or implementing partners
have supplied all of them with one form of ICT or the
other. Third, representative of rural (05 health centres
IV), peri-urban (02 peri-urban health facilities – district
hospital and regional referral hospital) and urban
setting (02 urban health facilities).
Interviews were conducted among hospital
superintendents/directors, Incharges (an officer in
charge of a health facility) of health facility, ICT
administrators and records offices of the identified
facilities. However, out of the eighteen (18)
responses, only fifteen (15) were included in the
analysis. Three (03) records were excluded because
they had missing information. In order to identify the
emerging themes, QSR NVivo 10 was used in the
analysis of the qualitative data collected.
3 RESULTS
3.1 Review of Other Studies
Only nineteen (19) peer-reviewed and grey literature
were used in the review. The key results from their
synthesis regard the role of ICT in health, resources for
ehealth communication infrastructure available to
resource-constrained settings, minimal communication
resources required to support HIE and challenges to
use of ICT in low resourced environments are
summarised below in Table 1. These were the basis of
our survey of ICT resource that supports healthcare
processes in LMICs, a case of Uganda.
Table 1: Themes emerging from the literature review.
R
ole o
f
ICT in health
Support data collection, analysis and storage
Support for clinical decisions and diagnosis
Support for messaging and data sharing
R
esources
f
or eHealth CI/T
eHealth hardware
Application software/technologies
Mobile connectivity and Internet penetration
Access to Power/ Electricity
Literacy skills
Security /privacy
Challenges
Lack of affordable connectivity / bandwidth
Poor infrastructure
Deployment of inappropriate technologies
Technology literacy challenges
Improper involvement of key stakeholders
Limited supporting resources like power
Inadequate policies
3.2 Case Study of Uganda
Responses used in the analysis were obtained from key
stakeholders from healthcare settings at the level of
Health Centre IVs’ and above in the study districts of
Tororo and Lira in Uganda. The hospital/health facility
superintendents, directors, Facility Incharges, ICT
officers, records officers, and ICT users represent the
decision-makers, implementers and users of ICT at
Status of Resources for Information Technology to Support Health Information Exchange in Resource-constrained Settings
465
health facility levels in Uganda. Being the key
stakeholders, their response presents a realistic account
of the status of ICT at surveyed health
facilities/districts. The response was distributed among
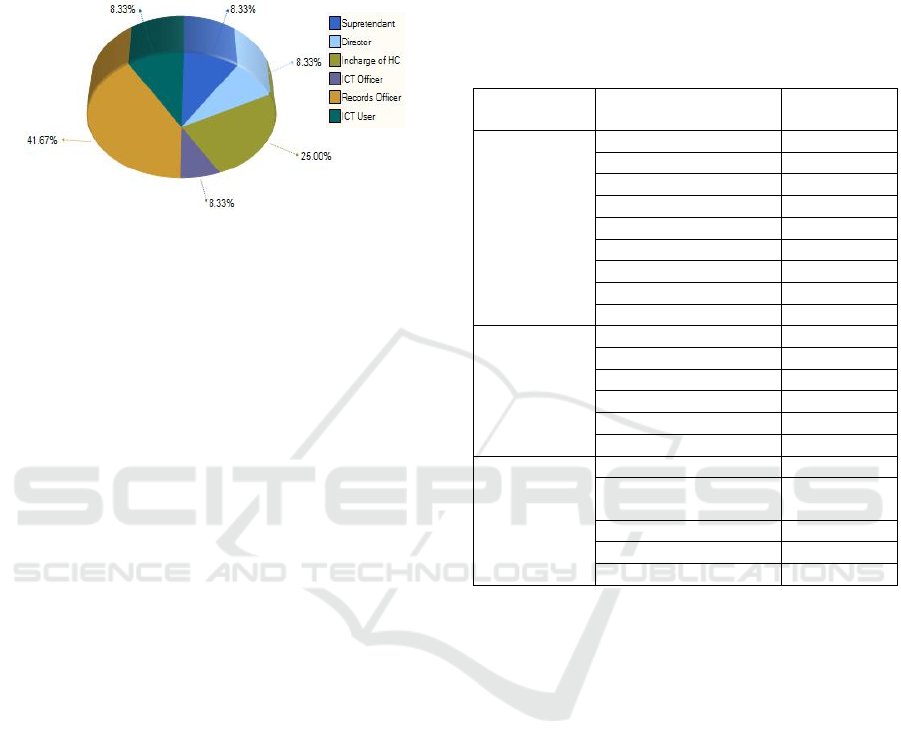
the respondent categories as shown in Figure 1.
Figure 1: Distribution of responses by relevant positions.
Qualitative analysis was carried out using QSR
NVivo 10. Emerging themes include use of ICT to
support healthcare processes especially data handling
and exchange, guidelines/standards for use, advantages
of incorporating ICT in healthcare processes, current
communication resources available in health facilities
in the study districts, existing challenges, and
recommended improvements. The results depict the
views of different facility-level stakeholders. Most of
whom were record officers (41.67%) who are the key
users of ICT in the healthcare process and Incharges
(25.0%), the decision-makers at facility levels. The rest
i.e., superintendents, directors, ICT officers and ICT
users, were equally represented at 8.33%.
3.2.1 Role of ICT in Healthcare
Results in Table 2 present the views of Uganda’s
health facility stakeholders on the role of ICT to
healthcare processes. With uses ranging from
administration, data storage, laboratory, monitoring,
ordering, records, reporting, and research; various
components of the ehealth CI/T are engaged to
support health data/information exchange. Reported
modes of health data exchange range from electronic
to paper-based transfer within the facility, across
facilities, or with the MoH headquarters.
They identified ICT use in healthcare that follows
appropriate rules of data handling and exchange to be
able to achieve the advantages of improved accuracy,
monitoring, tracking, reliability of healthcare
processes, and save on cost and time.
Hardware – the hardware (HW) resources include
disks/tapes for data backup; computers (both
desktops, laptops, portable digital assistants and
phones) for computational tasks and communication;
both local network and Internet resource to facilitate
communication and health data sharing; and attached
resources such as printers, scanners among others.
These hardware resources need to be dedicated and
robust to support data collection, processing, storage,
output, and communication. To emphasise this need,
a respondent called for “computers and tablets should
not be used to do anything else”.
Table 2: Role of ICT in health facilities.
Themes Sub-Themes
# of
respondents
Usage
Administration 2/15
Data storage 3/15
Laboratory 1/15
Monitoring 2/15
Ordering 2/15
Records 7/15
Reporting 6/15
Research 1/15
Others 2/15
Support for
Health
Information
Exchange
Electronic 9/15
Interfacility 3/15
Intra-facility 6/15
Mode of exchanges 6/15
Paper-based 1/15
Rules for exchange 3/15
Advantages
Improved accuracy 3/15
Improved monitoring and
tracking
2/15
Improved reliability 1/15
Saves Money 1/15
Time-saving 2/15
Software – the software (SW) systems and
technologies that were identified as in use by the
surveyed health facilities include simple database
systems, DHIS2, eHMIS, HIS, HR Biometric system,
Medical Records, mTrac, Staff Recruitment System,
and Tally Sheets.
Human Resources – respondents identified the
need for digitally enabled human resources for
healthcare. They strongly highlighted the need for in-
service training of staff and or recruitment of digital
health workers.
Electric Power – is required to ensure that the
available hardware resources are powered to
participate in data handling and communications. In
fact, it powers the ICT equipment to ensure they
function with a large meantime between failure.
Resources Challenges: the use of ICT in
different domains continues to experience challenges
including resource challenges. In a similar manner,
the ehealth communication infrastructure required to
facilitate health information exchange in low-
resourced settings experiences resource challenges.
HEALTHINF 2020 - 13th International Conference on Health Informatics
466
Among the identified challenges are financial
constraints, funders restrictions, HR limitations,
isolated systems-computers, lack of support from
management, legacy / outdated systems, limited
network bandwidth, and the intermittent Internet,
limited use-access, limited hardware, misuse and
poor maintenance of the available hardware, and
power outages. The number of respondents who
agreed on the existence of each of these challenges in
their facilities are summarised in Table 4.
Table 3: eHealth and supporting resources.
Resource type # of respondents
HW-Storage Hard disks/Tapes 1/15
Computers, laptops, PDAs, etc 9/15
Local area network & Internet 6/15
Printer 1/15
Scanner 2/15
SW-Systems & Technologies
Database 2/15
DHIS2 1/15
eHMIS 1/15
HIS 1/15
HR Biometric system 2/15
Medical Records 1/15
mTrac 2/15
Staff Recruitment System 1/15
Tally Sheets 1/15
HR -Available HR 2/15
- HR Training 4/15
Power 1/15
Table 4: Challenges to the use of ICT in Health Facilities.
Challenges # of respondents
Financial constraints 4/15
Funders interest 2/15
HR limitations 5/15
Isolated systems-computers 3/15
Lack of support from
management
2/15
Legacy / outdated systems 3/15
Limited BW-Internet 3/15
Limited HW 2/15
Limited use-access 3/15
Misuse & poor maintenance 2/15
Power 3/15
Others 6/15
Other challenges that may negatively influence
adoption and use of ICT in healthcare were identified
as missing technologies, the inexistence of the ICT
department, improper/unbalanced planning for the
ICT department, and limitation in the digital health
skills of their workers.
Security / Privacy Guidelines: there are various
threats to the electronic sharing of health data (11/13).
However, these threats can be minimised by a set of
guidelines on the use of ICT in healthcare. Among the
standards identified as required to regulate the use of
ICT in healthcare are access restrictions whether
physical, password, pin, unique patient or practitioner
codes and access logs (see Table 5). Management plays
a key role in the development and enforcement of such
guidelines.
Table 5: Current security and privacy guidelines for
handling health data in a digital environment.
Sub-Themes # of respondents
Threats 11/15
Privacy and security measures
Access-Log 1/15
Restrictions 6/15
Unique codes
Patient unique code 4/15
Practitioner unique code 3/15
Role of management 2/15
Suggestions for Improvement: table 6 present
views of respondents on how the use of ICT can be
improved to better serve healthcare processes. Their
views included the provision of data backup storage,
minimising ICT resource challenges that were
summarised in Table 4, better management, training
of staff in digital health skills, better stakeholders’
involvement, and adoption of user-friendly and
supportive technologies.
Table 6: General views on improving ICT for health.
Sub-Themes # of respondents
Data Storage 1/15
Improved resources 3/15
Management role 3/15
Training 5/15
Stakeholders 2/15
Supportive technologies 1/15
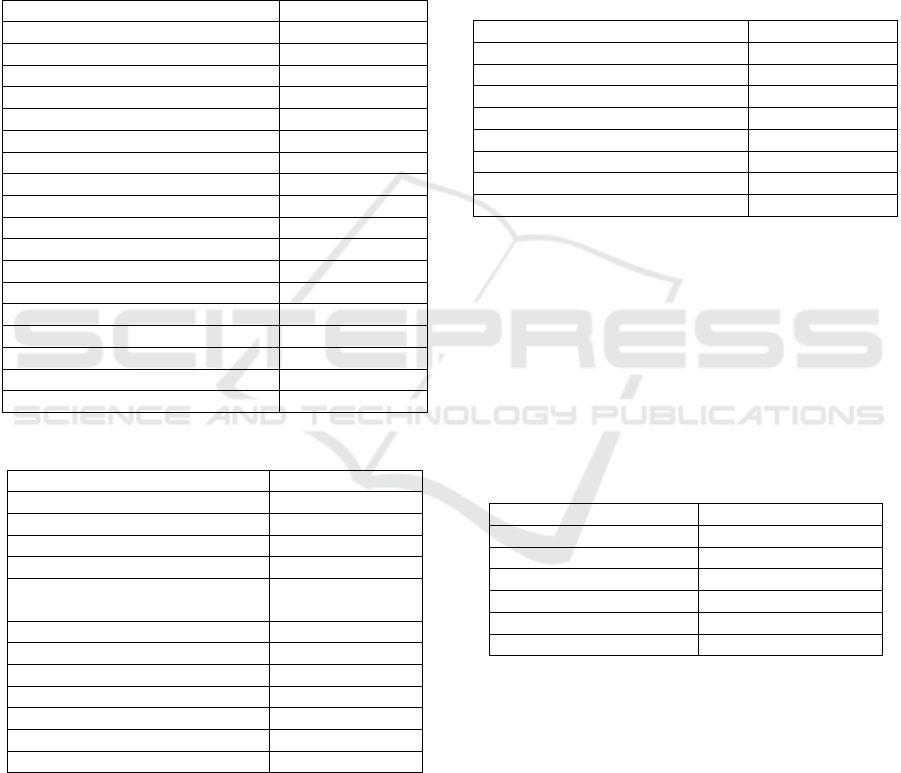
Further analysis was done, first, to examine the
distribution of the resources for ICT across the urban,
peri-urban and rural setting. Results show unequal
distribution as presented in Figure 2. The resources
are high in health facilities in urban settings and
decrease tremendously in rural settings. In fact,
similar resource categories in a rural setting are under
half those in urban settings. Second, to explore how
the responses vary by categorises of respondents.
Respondents were categorised into superintendents of
regional referral hospitals and directors of district
hospitals, medical officers who are in charge of
Status of Resources for Information Technology to Support Health Information Exchange in Resource-constrained Settings
467
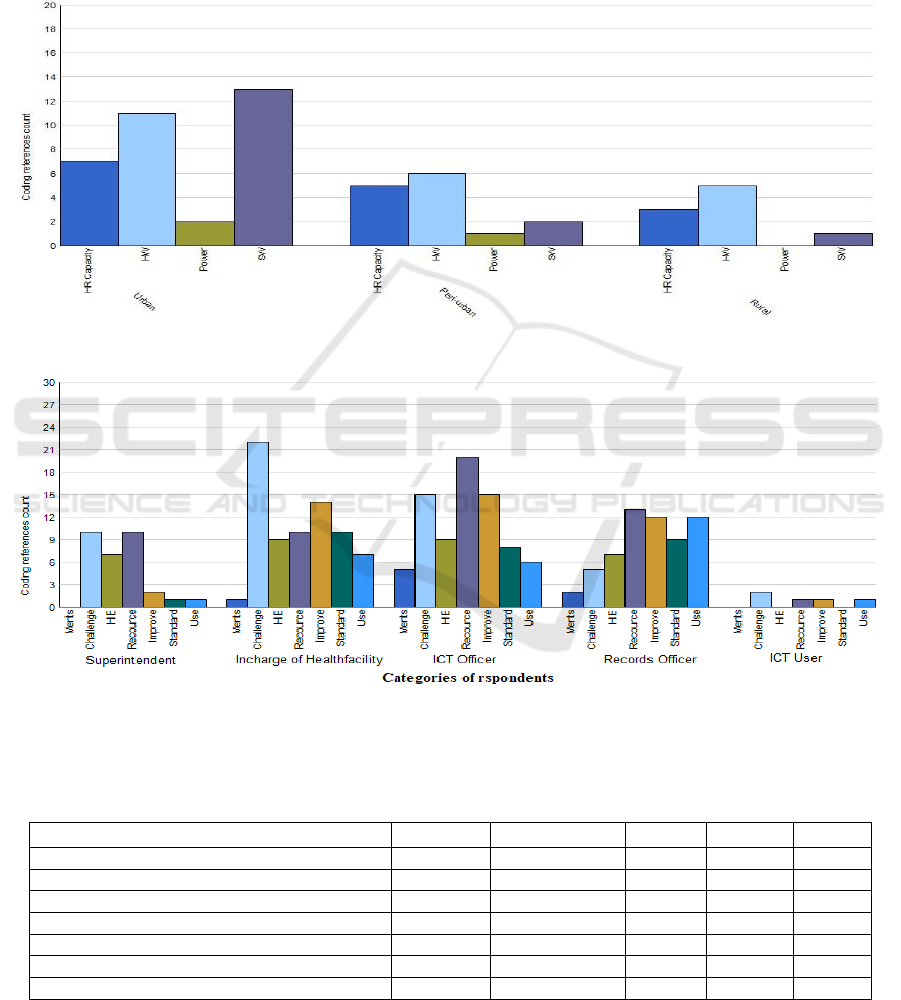
Health Centre IVs, officers in charge of ICT in the
respective referral and district hospitals, record
officers at the level of Health Centre IVs and district
hospitals, and ICT users at the surveyed health
facilities. The result presented in Figure 3 shows
strong views were expressed by the In charge of
health facilities, ICT officers and Records officers.
Counts in Figure 3 represents the number of times
respondents expressed strong views concerning the
identified themes.
Third, we compared results from the survey of
Uganda to those obtained from the literature review
of four other LIMCs in Africa. With the exception of
available bandwidth, the results presented in Table 7
show Uganda has similar or even better ICT resources
when compared to the four reviewed LMICs.
Figure 2: Urban, peri-urban and rural distribution of CIT resources.
Figure 3: Distribution of responses by respondent categories.
Table 7: Comparing the state of ICT resources in Uganda to other Four LMICs in Africa (ITU, 2019; WHO & ITU, 2015;
Asingwire, 2018; Bhatia et al., 2015; and Uganda’s MoICT, 2018).
Resources
Kenya South Africa Rwanda Tanzania Uganda
Average available Bandwidth (Mbps) 12.2 6.7 ─ ─ ─ ─ 4.0
Internet penetration ─ ─
─
Mobile Network connectivity ─ ─
─
Hardware resources
─
Security /privacy ─ ─ ─ ─ ─ ─
Literacy skills ─
─ ─
Access to Power ─ ─ ─
Key: =Very High (above 80%), ─=High (61%-80%), =Medium (41%-60%), ─=Low (21%-40%), =Very
Low (below 21%), ─ ─=Not sure/missing information.
HEALTHINF 2020 - 13th International Conference on Health Informatics
468

4 DISCUSSION
The hardware and software resources should be robust
enough to provide a reliable transport environment for
data sharing. Remembering that resources must be
optimized for adaptation (Alvaro et al., 2010), the
healthcare environment requires robust processing
power and communication capacity to meet the
stringent life-saving time requirements. The results
show a discrepancy in requirements for the resources
like the one suggested by HealthIT, (2013) and those
identified for Uganda. Whereas the practitioners
expressed aspiration for state-of-the-art CI resources,
the ministry recommended improved equipment,
existing resources for ehealth CI remains limited in
Uganda’s health system. These recommendations are
in line with the suggestions by respondents for
resource improvement, e.g., MoH “need to install
reliable internet service”, “provide power backup
sources”, and “Computers in all the departments and
these computers can be networked”. Not only are
appropriate resources for the CI required, but also a
proper design and implementation that furthers the
aims of healthcare delivery (McCarthy et al., 2014).
For HIE and interoperability to exist across the
healthcare system, the design and implementation of
such infrastructure need to follow agreed standards.
Whereas a previous study identified multiple
ehealth technologies in Uganda’s healthcare
environment (Huang et al., 2017), this survey only
identified nine software technologies. This could
partly be attributed to failure to sustain donor
technologies after the project duration, or lack of
skills to continue their use or financial constraints
among others. The initiative by Uganda’s MoH to
promote technologies like DHIS2 and mTrac in a
drive to promote standardisation of interoperable
systems could have also discouraged the use or
further adoption of diverse systems. Whatever the
software system / technology, it must be robust to
perform the required tasks as stated by a respondent
“All you need is very robust software systems, once
you have it the others can be automatic”. However,
network connectivity remains poor in rural areas.
This hampers HIE efforts. An earlier study on the
practical challenges for large-scale deployment of
mHealth solutions in LMICs confirms it, saying “for
always-on data, connectivity does not work when
deployed in rural…”(Kuntagod et al., 2014).
The disparity in the distribution of resources is
attributed to a lack of standards to guide the
establishment of the ehealth communications
infrastructure, financial limitations, and limited
support or improper prioritisation by management.
For example, whenever the mains power supply is
off, there is a lack of a fails-over power backup supply
in the form of no fuel to run the generators, or failed
solar installation, etc.
In fact, identified challenges to use of ICT
resources in health majorly centre around a limitation
in financial resources as summarised in this response:
“We have very limited budget, data, for example,
is not easily affordable. We normally take advantage
of partners who have interest in certain things and
avail data for this and this. Otherwise, our budget is
very limited. We can’t support the ICT sector
effectively. The hardware has wear and tear, the
maintenance cost is very high”.
Existing ICT resources are donor-funded,
confirming the arguments of Huang et al., (2017);
however, they come with stringent restrictions on use.
Sustainability tends to last for only the duration of the
funding. Technologies in use are able to improve
healthcare processes, for example, the monitoring and
supplies tracking system is able to expose corrupt
behaviours thereby saving on money. “Because you
can monitor all the vouchers and the transactions
from the stores and can count how many tablets were
used. This would help save a lot of money”.
As regards the role of ICT in healthcare, we argue
that, although ICT presents much promise to support
HIE, existing communication resources are still
inadequate in Uganda’s health system. Multiple-use
cases of ICT in healthcare have been highlighted in
these resource-constrained settings (Lewis et al.,
2012), however, the advantages are still restricted to
administrative tasks. There is a need to extend this to
HIE related processes. Similar dilemma including the
problem of the cross-system linkup, lack of
commonly defined and consistently implemented
standards, privacy/security concerns, cost of
implementation, and availability of necessary
infrastructure like power, Internet, among others
(Lewis et al., 2012; Peña-López, 2010) exist in other
resource-constrained healthcare settings.
In further analysis, first, we discovered that the
resource decreases uniformly from urban to the rural
healthcare settings, with power tending towards zero
in the rural health facility. This high-power outage
without an alternative source of power requires
immediate action as called for by a respondent
“Something must be done about this frequent power
interruption”. We acknowledge that respondents in
urban settings expressed the strong presence of
software resources (SW) above other resource
categories as represented in Figure 2. This is possible
because the first stopover for new technological
innovations is in urban health facilities and only a few
Status of Resources for Information Technology to Support Health Information Exchange in Resource-constrained Settings
469

scales over to rural settings. Also, the availability of
supporting resources like power, internet, technical
human resource, etc may be enabling factors.
Second, we realised that although ehealth users
were majorly from urban settings where there are
more ICT resources, they couldn’t state the
advantages of ehealth in facilitating healthcare
processes (see Figure 3). It was also surprising that
the interviewed superintendents and directors
couldn’t properly state the advantages of ehealth.
Overall, the facility managers and direct users of
ehealth technologies expressed little opinion on the
merits of the use of using ICT in healthcare as
compared to their counterparts, the Incharge of health
centre IVs, ICT officers and records officers. This
shows the managers are disengaged from decisions
regards acquisition and use and possibly ICT are
imposed on them by NGOs, implementing partners
and or governments. The users lack proper orientation
to adopt the use of ICT and therefore find it difficult
to use. This could explain why many respondents
recommend management support and training. “We
need training of staff. Some people might have not
been trained, so they find difficulty in handling it”.
Third, a comparison of the state of resources for
ICT in four other LMICs in Africa indicate that
Although Uganda has not yet achieved much progress
regards electronic HIE, her ICT resource environment
is similar or even better than some of the countries
that have made much progress. In fact, other LMICs
who are hesitant on adapting ehealth in support of
their healthcare services can learn from this
comparison.
5 CONCLUSIONS
The survey of ICT resources being used in health to
support ehealth communication in three regions of
Uganda revealed major challenges to the acquisition,
establishment, and management of the ehealth
communication infrastructure. Furthermore, the
resource distribution is unevenly spread across the
rural, peri-urban and urban settings. Both these
challenges and the uneven spread negatively
influence health information exchange both within a
health facility and across health facilities
respectively. Although the survey only involved three
districts in Uganda, we believe the findings from this
study are representative of the status of ehealth
communication resources in the whole country.
The findings of this study can inform Uganda’s
MoH (and any other resource-constrained LMIC) to
standardise the ehealth communication infrastructure
of their healthcare systems. Recommendations for
improvement include; (1) the MoH needs to specify
minimum resources for ICT required to support HIE,
both within and across healthcare organisations. This
includes standardisation of the design and
implementation of ICT systems to support HIE. The
technology systems at the healthcare facility level, the
cabling and cable category, interfaces, modes of
information exchange, security, access privileges and
privacy need to be standardised. (2) The MoH needs
to supervise implementation and monitoring
compliance to the standards. Changes to be
implemented may include those that create a uniform
enabling environment for HIE, for example, connect
all health facilities to the national backbone, provide
alternative power sources like solar power, etc. (3)
Establish a mechanism for periodic review of the
minimum standards for ICT supporting HIE. And
finally, (4) Align ICT funding within the mainstream
funding for healthcare services.
In another ongoing study, we are reviewing global
standards for ehealth CI/T to determine criteria for
selecting standards suitable to support HIE in LMICs.
We also intend to develop a structured process that
can be used by LMICs to adopt standards for ehealth
CI/T, monitor implementation and compliance with
such standards.
ACKNOWLEDGEMENTS
This study was funded in part by the Swedish
International Development Cooperation Agency
(Sida) and Makerere University under Sida
contribution No: 51180060.
REFERENCES
Alvaro, C., Lyons, R. F., Warner, G., Hobfoll, S. E.,
Martens, P. J., Labonté, R., Brown, E.R., 2010.
Conservation of resources theory and research use in
health systems. Implementation science 5, 79.
Andrews, C., Das, M., Elder, J., Ovadiya, M., Zampaglione,
G., 2012. Social Protection in Low Income Countries
and Fragile Situations: Challenges and Future
Directions. World Bank 59.
Asingwire, N., 2018. The high cost of mobile data in Sub-
SaharanAfrica [WWW Document]. SautiTech. URL
https://www.sautitech.com/telecom/uganda-has-the-
most-expensive-internet-in-east-africa-report/ (accessed
6.20.19).
Bhatia, M., Angelou, N., Soni, R., Portale, E., Fletcher, E.
R.., Susan Wilburn, Adair-Rohani, H., 2015. Access to
Modern Energy Services for Health Facilities in
HEALTHINF 2020 - 13th International Conference on Health Informatics
470

Resource-Constrained Settings: A Review of Status,
Significance, Challenges and Measurement. World
Health Organization and World Bank.
Blantz, E., 2010. 4 Key Challenges and Solutions to ICT
Deployments for Rural Healthcare. ICTworks. URL
https://www.ictworks.org/4-key-challenges-and-
solutions-ict-deployments-rural-healthcare/ (accessed
10.24.19).
Dhital, H., 2018. Opportunities and Challenges to Use ICT in
Government School Education of Nepal. International
Journal of Innovative Research in Computer and
Communication Engineering 3215–3220.
Dixon, B. E., 2016. What is Health Information Exchange?
In: Health Information Exchange : Navigating and
Managing a Network of Health Information Systems.
pp. 3–20.
FrontEnders Healthcare Services Pvt. Ltd, 2016.
Information Communication Technology in
HealthCare [WWW Document]. URL
https://www.frontenders.in/blog/information-
communication-technology-healthcare.html (accessed
10.21.19).
Health ICT Industry Group, 2009. ICT’s Role in Healthcare
Transformation.
HealthIT, 2013. What is the recommended bandwidth for
different types of health care providers? [WWW
Document]. URL https://www.healthit.gov/faq/what-
recommended-bandwidth-different-types-health-care-
providers (accessed 5.22.19).
Henry, L., 2019. Bridging the urban-rural digital divide and
mobilizing technology for poverty eradication:
challenges and gaps. University of the West Indies, St
Augustine, Trinidad and Tobago.
Huang, F., Blaschke, S., Lucas, H., 2017. Beyond pilotitis:
taking digital health interventions to the national level
in China and Uganda. Globalization and Health 13, 49.
https://doi.org/10.1186/s12992-017-0275-z
ITU, 2019. ICT Country Profile [WWW Document]. URL
https://www.itu.int/net4/itu-d/icteye/CountryProfile.
aspx#AsiaPacific (accessed 5.22.19).
Jere, N. R., Thinyane, M., Boikhutso, T., Ndlovu, N., 2013.
An assessment of ICT challenges in rural areas: ICT
experts vs rural users views: a case of the Siyakhula
Living Lab, in: Proceedings of the South African
Institute for Computer Scientists and Information
Technologists Conference. ACM, pp. 233–241.
Juniper Networks, 2015. Five Requirements for Building a
State-of-the-Art Healthcare Network from the Ground
Up 6.
Kuntagod, N., Paul, S., Kumaresan, S., Ganti, S., 2014.
Practical challenges for large-scale deployment of
mHealth solution insights from a field trial, in: IEEE
Global Humanitarian Technology Conference (GHTC
2014). IEEE, pp. 235–241.
Lewis, T., Synowiec, C., Lagomarsino, G., Schweitzer, J.,
2012. E-health in low-and middle-income countries:
findings from the Center for Health Market
Innovations. Bulletin of the World Health Organization
90, 332–340.
Madinah, N., 2016. Challenges and barriers to the health
service delivery system in Uganda. IOSR Journal of
Nursing and Health Science 5, 30–38.
McCarthy, D. B., Propp, K., Cohen, A., Sabharwal, R.,
Schachter, A. A., Rein, A. L., 2014. Learning from
Health Information Exchange Technical Architecture
and Implementation in Seven Beacon Communities.
EGEMS (Wash DC) 2. https://doi.org/10.13063/2327-
9214.1060
Peña-López, I., 2010. Improving health sector efficiency:
The role of information and communication
technologies.
Sewell, A., 2014. Meeting network infrastructure
challenges [WWW Document]. Healthcare Innovation.
URL https://www.hcinnovationgroup.com/policy-
value-based-care/article/13006987/meeting-network-
infrastructure-challenges (accessed 5.23.19).
Uganda’s MoICT, 2018. The National Broadband Policy.
Uganda’s MoICT, 2014. National Information and
Communications Technology Policy for Uganda.
WHO & ITU, 2015. Atlas of eHealth country profiles 2015:
The use of eHealth in support of universal health
coverage [WWW Document]. WHO. URL
http://www.who.int/goe/publications/atlas_2015/en/
(accessed 2.28.19).
Williams, C., Mostashari, F., Mertz, K., Hogin, E., Atwal,
P., 2012. From the Office of the National Coordinator:
the strategy for advancing the exchange of health
information. Health affairs 31, 527–536.
Status of Resources for Information Technology to Support Health Information Exchange in Resource-constrained Settings
471
