
A Patient’s Perspective on Decision-making for the Adoption of
Digital Care Pathways
Raja Manzar Abbas
1
, Noel Carroll
1,2
and Ita Richardson
1,3
1
Lero - The Irish Software Research Centre, Ireland
2
Business Information Systems, NUI Galway, Galway, Ireland
3
ARC – Ageing Research Centre, HRI - Health Research Institute, University of Limerick, Limerick, Ireland
Keywords: Patient-centred Care, Healthcare Information Systems, Digital Care Pathway, Decision-making, Adoption.
Abstract: Healthcare Information Systems (HIS) are implemented to provide high-quality, patient-centred care. Yet,
there is little evidence about the decision-making role patients play for the adoption of HIS nor what factors
patients deem essential in the adoption of HIS. To guide healthcare practitioners in decision-making for the
adoption of HIS, this study reports on the key factors which influence patients’ perception and use of HIS.
Specifically, a qualitative study was conducted with 15 patients to understand the phenomenon of patient
decision-making for the adoption of HIS. Our findings identify the concept of ‘Digital Care Pathways’ and
indicate that there are four primary decision factors which influence the adoption of HIS: (i) trust; (ii) fear;
(iii) ease of use; and (iv) accessibility. To synthesise the findings, we present the patients decision-making
framework for digital care pathways as a first step to encapsulate the patients’ perspective of decision-making
factors associated with adopting innovations for digital care pathways.
1 INTRODUCTION
Healthcare delivery systems throughout the world
have been made possible by the advancement of
Information System (IS). Increasing attention has
been given to implementing healthcare information
systems (HIS) in hospitals, particularly regarding the
need to consider the acceptance and usage of HIS
among healthcare professionals (Ismail et al., 2015).
We coin the phrase ‘Digital Care Pathways’ to
refer to online services provided by hospitals. Digital
Care Pathways can provide a digital solution to the
patients, and it may bring other benefits, such as
standardized care and greater control over the delivery
of care. HIS is one of the applications that can be used
to provide a digital solution for patients. By adopting
HIS applications, hospitals also gain significant
benefits, ranging from improved diagnosis, thereby
delivering better patient care and improved the
support of clinical decision-making. This enhances
hospital productivity, lowers costs, and reduces
medication errors (Aron et al., 2011). Technological
advancements made in medical science have offered
new choices which are upgrading outcomes of care,
yet it has inadvertently dissociated clinicians from the
patients. Therefore, a healthcare environment has
been established where, often, patients and their
families are not involved in their significant treatment
decisions and discussions. Patients can be left in
obscurity about how their issues are being handled
and further on how to direct the profound range of
diagnostic choices accessible to them (Epstein et al.,
2011).
1.1 Patient-centred Care
The term, “patient-centred care”, was introduced by
the Picker/Commonwealth Program for Patient-
Centred Care (now the Picker Institute) to present the
significance of having a better understanding by
clinicians of the patient and family experience of
illness. Additionally, patient-centred care should
support patients’ needs during their time in a very
difficult and often complex care delivery system
(Barry and Edgman-Levitan, 2012). Over the past few
decades, renewed focus had emerged around patient-
centred care as an attempt to avert the trend away from
focusing on diseases and reverting back to the
patient’s needs and satisfaction (Gerteis et al., 1993).
The most significant characteristic of patient-
centred care is the dynamic commitment of patients
when healthcare choices must be made — moreover,
Abbas, R., Carroll, N. and Richardson, I.
A Patient’s Perspective on Decision-making for the Adoption of Digital Care Pathways.
DOI: 10.5220/0008967704470454
In Proceedings of the 13th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2020) - Volume 5: HEALTHINF, pages 447-454
ISBN: 978-989-758-398-8; ISSN: 2184-4305
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
447

when an individual patient lands at an intersection of
medicinal possibilities, diverging pathways have
extraordinary and significant results with lasting
ramifications. These include, for instance, decision-
making in major surgeries, prescriptions to be taken for
the rest of a patient’s life, and screening and
symptomatic tests that can trigger upsetting
interventions. The procedure by which the optimal
decision might be reached regarding a patient is termed
as shared decision-making. It includes, at least, a
clinician and the patient, while other members from the
medical team or households might be allowed to
participate. Every member is in this way outfitted with
a better comprehension of the pertinent factors and
wisely shares responsibility in the choice about how to
pursue treatment (Delbanco and Gerteis, 2012).
The adoption of HIS is similarly an essential
decision in a hospital, and central to this is the
decision-making process. However, despite an
accumulation of best practices, frameworks and
research which has identified success factors, the
function of hospital decision-makers, especially
patients, in the adoption process of new technologies
remains unreported (Yang et al., 2013).
1.2 Problem Statement
The objective of this paper is to report on an empirical
study conducted with patients on the role they play in
decision-making for the adoption of HIS. We look
particularly at the assumptions around ‘patient-
centric’ technology and the role of patients in
decision-making.
There is an apparent lack of insight into what role
patients play in the decision-making for the adoption
of HIS and whether they should be involved in the
decision-making process. To address these gaps, we
formulate the following research questions:
RQ1. What role do patients have in decision-
making for the adoption of HIS?
RQ2. From the patient’s perspective, what are
the decision-making factors for the adoption of
HIS?
2 BACKGROUND
2.1 Patient-centred Care
The Institute of Medicine (IOM) defined patient-
centred care as “care that is respectful of and
responsive to individual patient preferences, needs,
and values” by thus ensuring “that patient values
guide all clinical decisions” (Barry and Edgman-
Levitan, 2012). This definition highlights the
importance of clinicians and patients working
together to produce the best outcomes possible.
Patient-centred care depends on the nature of
individual, professional and organizational
connections. In this manner, endeavours to advance
patient-centred care ought to consider the patient-
centeredness of patients (and their households),
clinicians, and wellbeing systems (Epstein, 2010,
Epstein et al., 2011). Helping patients to be
progressively dynamic in consultations changes years
of doctor-commanded communications to those that
draw in patients as active about what patient-centred
care truly implies, however, can create endeavours
that are specious and implausible.
Despite the discussions around patient-
centeredness, hospitals have been adopting
technologies without having discussions with the
patients (Barry and Edgman-Levitan, 2012). Besides,
while adopting technologies may upgrade the patient's
experience, they have failed to accomplish the
objectives of patient-centred care. Calls for patient-
centred care have frequently stressed the execution of
infrastructural changes (Epstein et al., 2011). These
changes, such as adopting HIS, may be necessary to
move medical care into the 21st century, but they
should not be conflated with achieving patient-centred
care. Simply implementing HIS in itself is not patient-
centred unless it strengthens the patient-clinician
relationship, promotes communication about things
that matter, helps patients know more about their
health and facilitates their involvement in their care
(Epstein and Street, 2011).
2.2 Impact of HIS
Lippeveld et al., (2000) defines HIS as “a set of
components and procedures organized to generate
information which will improve healthcare
management decisions at all levels of the health
system”. HIS has the potential to address many of the
challenges that healthcare is currently confronting.
For example, it can improve information
management, access to health services, quality and
safety of care, continuity of services, and costs
containment (Lippeveld et al., 2000).
Technological advances have encouraged the
development of new technologies that drive
connectivity across the healthcare sector such as
software apps, gadgets and systems that personalise,
track, and manage care using just-in-time information
exchanged through various patient and community
connections (Leroy et al., 2014; Carroll, 2016). This
paradigm shift has contributed to advancing healthcare
HEALTHINF 2020 - 13th International Conference on Health Informatics
448

practice, highlighting our growing reliance and need of
digital care pathways to support healthcare decisions.
However, without involving patients in the decision-
making process, it may impact how patient-centred
care is received (Epstein and Street, 2011).
Digital care pathways provide the opportunity for
healthcare providers to meet the demands of high-
quality patient care and makes all-encompassing
healthcare support possible, thereby playing a
dominant role in improving health processes and in
the provision of patient care services worldwide.
2.3 Involvement of Patients in
Decision-making – Does it Matter?
Policies to encourage shared decision-making have
become prominent in the United States, Canada, and
the United Kingdom (Elwyn et al., 2010). This is partly
because of a recognition of the ethical imperative to
properly involve patients in decisions about their care
(Mulley, 2009). Shared decision-making is an approach
where clinicians and patients make decisions together
using the best available evidence. By doing so, they
likely know the benefits or harms of each so that they
can communicate their preferences and help select the
best course of action for them. Shared decision-making
respects patient autonomy and promotes patient
engagement (Elwyn et al., 2014).
Despite considerable interest in shared decision-
making, implementation has proved difficult and slow
(Légaré et al., 2008). At the minimum, three
conditions must be set up for shared decision making
to be part of mainstream clinical practice: provide
access to evidence-based information about
medication choices; direction on the best way to
weigh up the impact of various choices; and a strong
clinical culture that may encourages patient
involvement (Elwyn et al., 2010). In addition, Carroll
et al. (2016) outlined the importance of community
care and the need for more patient-centric focus in
decision-making. These authors outline some options
for creating a sustainable decision support platform
for patients that may facilitate wider adoption of
shared decision making in clinical practice.
2.4 Need for Patients Decision-making
Framework for Digital Care Pathways
According to Baker et al. (2002) “decision-making is
regarded as the cognitive process resulting in the
selection of a belief or a course of action among
several alternative possibilities”. Technology
adoption decisions in hospitals may occur through
planned acquisitions or uncontrolled changes in
medical practice. They reflect a complex set of
dynamics and incentives (Gelijns, 1992).
There are different decision-making models and
theories used to define a hospital’s decision to adopt
the technology. The first set of models include the
profit-maximization model (Focke and Stummer,
2003), and the fiscal managerial system (Lennarson
Greer, 1985). These theories presume that hospitals
assess new advancements from the viewpoint of
clinical gains, and advances obtained when the
estimated regular estimation of income surpasses the
expected expense over the valuable lifetime of the
item. Hospitals embrace capital-concentrated
advancements unrelated to their expense to
accomplish technological prevalence and to upgrade
their reputation. It helps hospitals as pioneers in the
technical domain, tempting patients, doctors, and
scientists (Anderson et al., 1994).
Nonetheless, medical administrators may often
choose to put resources into monetary loss activities
that can enhance medical exposure and draw in patients
for other parts of the hospitals (Teplensky et al., 1995).
The medical-unorthodox viewpoint (Lennarson Greer,
1985) centres around the delivery of services as per the
requirements of doctors or medical administrations. Its
likelihood depends on elementary presumptions that
the doctors and the clinic receive new technologies
dependent on the medical needs of the population they
serve, regardless of whether monetary limitations,
competition, or estimation of hospital repute
recommend alternative conducts. In contrast, hospitals
do not embrace innovation, regardless of its
exceptionally beneficial nature, if patients cannot
procure significant advantages from it.
Several other theories such as Technology–
Organization–Environment (TOE) framework
(Tornatzky et al., 1990), and Human-Organization-
Technology–fit (HOT-fit) (Yusof et al., 2008) have
been suggested to describe hospital behaviour and
adoption of new technology, yet none of these
perspectives has tried to explain technology adoption
decisions from the patient’s perspective or has
considered patients as a stakeholder (Yang et al., 2013).
3 METHODOLOGY
This study aimed to comprehensively analyse the
decision-making factors on the adoption of digital care
pathways in a hospital setting. For this purpose, we
performed a literature search, which focused on the
decision-making about the adoption of IS in general
and HIS in particular. The detailed protocol and results
of the literature review are available in our technical
A Patient’s Perspective on Decision-making for the Adoption of Digital Care Pathways
449

report (Abbas et al., 2019). Following the literature
review, we conducted exploratory interviews with
fifteen patients who were undergoing treatment in the
hospital and using HIS as part of their care pathway.
The hospital we studied is the second largest
maternity hospital in Ireland, with an average of 5,000
births per year and the sole provider of obstetrical,
midwifery and neonatal intensive care to the Mid-
West region. It is managed by the Irish Government’s
Health Service Executive (HSE) within a hospital
group. This hospital moved from phone consultation
for diabetic pregnant patients to virtual clinics which
includes video consultation with patients.
We used the methodical approach of qualitative
semi-structured interviews since they not only provide
an interviewing process that targets the identification
of the relevant determinants of the role patients can
play in the decision-making process, but it also allows
new viewpoints to emerge freely (Britten, 1995).
All the 15 interviews were recorded and
subsequently transcribed. Interviews were conducted
between February 2019 and August 2019. The ethical
approval was granted for these interviews through the
ethics committee.
Data analysis was undertaken using thematic
analysis (Guest et al., 2011). Initially, in thematic
analysis, we coded data according to key themes and
its various subcategories. All the interview transcripts
were analysed and coded, according to the guidelines
suggested by Saldaña (2015).
In the first cycle, the entire transcript was read in
detail line-by-line. We performed descriptive coding,
bearing in mind our research questions. This was
followed by relating categories to their subcategories.
We then mapped our findings according to the
literature while remaining open to the identification of
alternative and new categories of concepts. Once a
relationship was determined, the focus returned to the
data to question the validity of these relationships to
decision-making factors. Thus, by blending the
strengths of our analysis and coupling them with our
literature review, concept mapping offered a way to
represent meaning to the decision-making concept.
4 PATIENT DECISION-MAKING
FRAMEWORK FOR DIGITAL
CARE PATHWAYS
Lennarson Greer (1985) suggests that that the
clinicians and the hospital adopt new technologies
based on the clinical needs of the patients. While the
decision to adopt healthcare technology is based on
patients need is described, the patients are not
involved in the decision-making process. As a first
step for involving patients in the decision-making
process for the adoption of HIS, we developed the
‘Patient Decision-Making Framework for Digital
Care Pathways’ (Figure 1) that captures different
decision-making factors from the patient’s
perspective. Central to this is the idea that patients
need to be aware of the advancements in Digital Care
Pathway and how it helps them in improving their
care. In the norm, a Digital Care Pathway does not
alter how healthcare is delivered to the patients but
alters the medium of the care.
Based on the interviews, we identify patients’ key
decision-making factors for the adoption of digital care
pathways and present them through our framework.
The main contribution from our framework is that we
have identified four main patients’ decision-making
factors for the adoption of digital care pathways - trust
in the adoption of the digital care pathways, fear of
privacy and safety, ease of use of the digital care
pathways, and accessibility to healthcare. As described
earlier, there is a growing consensus that hospitals are
setup with a view to patient-centred care and one
should involve the patients in the decision-making. Yet,
we have observed a lack of involvement of patients in
decision-making for digital care pathways. Our
framework and the four factors provide an approach to
define the context of digital care pathways adoption to
support patients’ decision-making. We describe each of
the four factors and how literature supports our
framework.
4.1 Trust in Adoption of Digital Care
Pathways
Trust in technology influences the use or adoption of
a technology (Abbas et al., 2017). Trust is defined by
Amoroso et al. (1994) as a “level of confidence or
degree of confidence” and trust in technology is
defined as a “degree of confidence that the technology
satisfies its requirements”. Since the definition is
expressed as a “degree of confidence”, Amoroso et al.
illustrate that trust is dependent upon management
and technical decisions made by individuals or groups
of individuals evaluating the technology. Trust in
digital care pathways is expressed in terms of a set of
requirements, where the ‘set’ is variable. For
example, HIS trust may be dependent on the set of
functional requirements or maybe a critical subset of
functional requirements, or it may be some set of
requirements that include non- functional assurance
requirements like accuracy or reliability (Amoroso et
al., 1994).
HEALTHINF 2020 - 13th International Conference on Health Informatics
450
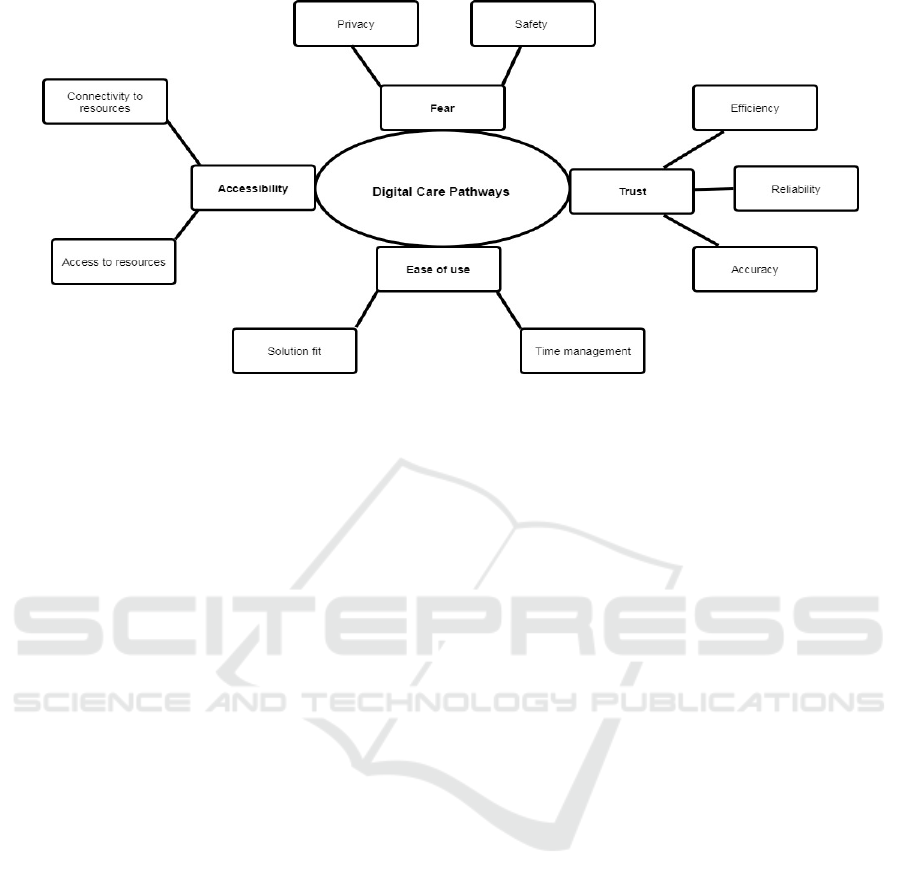
Figure 1: Patient Decision-Making Framework for Digital Care Pathways.
Patients described three sub-factors of trust that
they deemed to be an important of the decision-
making process - reliability, accuracy and efficiency.
Van Velsen et al. (2016) discussed trust in a
rehabilitation portal technology, which was mainly
determined by its reliability. They defined reliability
for the rehabilitation portal technology as: “That it
works properly; is not constantly offline. But also
scientifically reliable”. For patients, reliability is the
probability of the technology delivering results that
are consistent with their clinicians’ understanding.
Carbone et al. (2013) defined Accuracy for HIS as
“information generated to the extent to which test
results, diagnoses and treatments are error-free”.
For patients, the accuracy of digital care pathways
was one of the decision-making factors that should be
looked into before its adoption. One of the patients
mentioned: “my first thoughts to decide virtual clinics
would be its accuracy because else I don’t want to use
virtual technology that is giving error generated
results”.
Efficiency and quality have been discussed
regularly in the literature. The efficiency of
technology is one of the decision factors defined by
(Egea and González, 2011) for a clinician’s
acceptance to use and trust technology. They explain,
“a clinician who uses healthcare technology is
concerned by the quality and efficiency of the system
which impacts the patient’s care. Effectiveness of the
technology is that it can give a quick response or
reaction with minimal resources and/or time taken”.
Patients thought the efficiency of virtual clinics is
one of the decision factors that supported the hospital
in adopting it. One patient stated that: “How can
(hospital) decide to use virtual clinics if it was not
efficient enough while managing their time and
patients as well”.
4.2 Fear of Loss of Privacy and Safety
Fear of lack of regulations around privacy and safety
of patient’s data was another factor that was
mentioned by patients as one of the main decision-
making factors to adopt virtual clinics. Researchers
who have published on this topic, advocate for
regulations to protect privacy and ensure safety.
However, patients continue to have a fear of a data
breach. For example, Hsieh (2015) describes privacy
as the potential loss of confidential patient data in
Electronic Medical Record exchange systems as a
reason for low adoption by the hospitals. Patients
interviewed were concerned by the change of General
Data Protection Regulation (GDPR) regulations and
the impact it may have on their privacy of data. When
asked about the virtual clinics decision-making factor
that they think was considered, one patient mentioned
that: “my concerns around virtual clinics decision-
making will always be around privacy of my data and
the lack of awareness given to me around it … no one
briefed or talked about it”.
Similarly, patients considered that the safety of
their treatment as one of the Hospitals decision-
making factors to adopt virtual clinics. One of the
patients had concerns around the usage and safety of
virtual clinics stating that: “this is all government
doing to facilitate hospital, they have fewer resources,
and this is all to utilize that else why would you
implement something virtually when physical
consulting is safer and makes sense to the patient”.
A Patient’s Perspective on Decision-making for the Adoption of Digital Care Pathways
451

4.3 Ease of Use of Digital Care
Pathways
Ease of use of digital care pathways refers to how
patients see ease of use and comfort in using as
leading to the adoption of digital care pathways.
Almost every patient mentioned ease of use as a
leading decision-making factor in adopting virtual
clinics. Patients see virtual clinics as a means to
provide comfort in treatment, or as a means to ease
staff workload. Barry and Edgman-Levitan (2012)
advocate for this, stating that “patients need to be
involved in determining the management strategy
most consistent with their preferences and comfort”.
It was noticed that long waiting times could be
minimized from both the patients and the healthcare
professional’s perspective. One of the patients stated
that “I have small kids, going to the hospital with them
is tough. Through virtual clinics, I have specific time
with my clinician, and I don’t have to wait in long
queues”.
4.4 Accessibility to Healthcare
The fourth patient decision-making factor that our
framework captures is accessibility. Accessibility
covers the connectivity to the resources as well as
access to the resources. Access to resources describes
how patients think implementing virtual clinics has
helped to end long queues and wait time by utilizing
less staff and space in the hospital. One of the
concerns patients had with the implementation of
virtual clinics was the thought process behind the
connectivity to access virtual clinics. Patients living in
remote areas were concerned by their internet speed
and how these virtual clinics can be assessed.
Patients who had to travel a long way applauded
virtual clinics and how it solved their problem of
travelling. Also, it was noticed that long waiting times
could be minimized from both the patients and the
healthcare professional’s perspective. One of the
patients stated that
“As a virtual entity given that our
geographic area is quite big, I find it very difficult to
come to the hospital, it makes sense to introduce this
service and to do everything virtually”.
5 DISCUSSION AND
CONCLUSIONS
Globally, patient-centred care is talked about in
modern healthcare, yet challenges remain to regularly
engage patients in decision-making. This is echoed by
Barry and Edgman-Levitan (2012), who claim that
engaging clinicians and patients in decision-making
can help to achieve quality and trust: “Recognition of
shared decision making as the pinnacle of patient-
centred care is overdue”. To build a truly patient-
centred healthcare system, we need to involve patients
in decision-making, not only about their treatments,
but also about the decisions to adopt digital care
pathways.
We also studied the role which patients play in the
decision-making for the adoption of digital care
pathways. In the case study we conducted, one of the
decision factors from hospital perspective for the
adoption of virtual clinics was on patient-centred care
and making the experience better for patients, but we
found that patients themselves did not play any role in
the decision-making for the adoption of the virtual
clinic.
Although patients were happy with the care and
did not express an interest in participating in the
decision-making for the adoption of virtual clinics,
they did contest the decisions to adopt virtual clinics
as not being patient-centred. One patient stated “I see
virtual clinics as help to midwives, it has nothing to
do with patients. If I was on private insurance, would
they have adopted virtual clinics?”.
Generally, patients were satisfied with the care
hence less concerned with the involvement in the
decision-making process. One patient stated that “I
am happy with my care so yes it makes sense that my
involvement is minimal and having no experience in
decision-making, what would I suggest anyways”.
Another patient stated that “I am not an expert so
consulting me with decision-making is not a good
option, I am happy the way my treatment has gone and
for me, the care is the only factor that matters”.
There is some evidence that when patients have
made well-informed decisions, they also follow better
treatment routines (Joseph-Williams et al., 2010).
Patients are encouraged to think about the available
screening, treatment, or management options and the
likely benefits and harms of each so that they can
communicate their preferences. As stated by Stacey et
al. (2017) “when informed patients face discretionary
treatment, they make more conservative decisions,
often deferring or declining interventions”. These
effects seem to be strengthened when patients are
given decision coaching (a brief discussion with a
trained facilitator) to help them with the process of
discussion (Joseph-Williams et al., 2010).
We have identified that there is a gap, as different
theories such as TOE, HOT-fit or the medical-
individualistic perspective do not involve patients in
the decision-making for the adoption of digital care
HEALTHINF 2020 - 13th International Conference on Health Informatics
452

pathways. Therefore, we introduce the patient
decision-making framework for digital care pathways
which covers the patient’s perspective in the decision-
making process.
5.1 Future Work
Having established a foundation for the patient
decision-making framework for digital care
pathways, we will continue to build on this to
establish key processes and factors to further develop
the decision-making framework that includes both the
hospital staff and patient perspective of decision-
making factors for the adoption of digital care
pathways. The concept of a digital care pathway may
broaden the concept of how the medium of care for
the patients be enhanced.
We present the framework as a first step that
encapsulates research developments across patient-
centred care and recognise a need for empirical
research to validate patient decision-making. Our
subsequent focus will be on extending and modifying
existing techniques based on the identified patient
factors during our analysis. Furthermore, we will test
and refine it on a large scale with the healthcare sector.
One of the limitations of this study is the limited
number of patients interviewed. As this is a project in
progress, we are interviewing additional patients to
strengthen our findings.
ACKNOWLEDGEMENTS
This work was supported with the financial support of
the Science Foundation Ireland grant 13/RC/2094 and
co-funded under the European Regional Development
Fund through the Southern & Eastern Regional
Operational Programme to Lero - the Irish Software
Research Centre (www.lero.ie).
REFERENCES
Abbas, R. M., Carroll, N., Richardson, I. and Beecham, S.,
2017. The Need for Trustworthiness Models in
Healthcare Software Solutions. BIOSTEC 2017, Vol. 5,
pp. 451-456.
Abbas, R. M., Carroll, N., Richardson, I., "Protocol for a
Structured Literature Review of Decision-making Factors
for the Adoption of Health Information Systems 2019".
Available at: https://www.lero.ie/sites/default/files/TR_
2019_02.
Amoroso, E., Taylor, C., Watson, J. and Weiss, J., 1994,
November. A process-oriented methodology for
assessing and improving software trustworthiness. In
Proceedings of the 2nd ACM Conference on Computer
and communications security pp. 39-50.
Anderson, G., E. P. Steinberg, and H. Dawkins 1994. "Role
of the Hospital in the Acquisition of Technology."
Medical Innovation at the Crossroads 4: pp. 61-70.
Aron, R., S. Dutta, R. Janakiraman and P. A. Pathak 2011.
"The impact of automation of systems on medical
errors: evidence from field research." Information
systems research 22(3): pp. 429-446.
Baker, D., D. Bridges, R. Hunter, G. Johnson, J. Krupa, and
K. Sorenson 2002. "Guidebook to decision-making
methods." Department of Energy, USA.
Barry, M. J. and S. Edgman-Levitan 2012. "Shared Decision
Making — The Pinnacle of Patient-Centered Care."
New England Journal of Medicine 366(9): pp. 780-781.
Britten, N. 1995. "Qualitative research: qualitative interviews
in medical research." Bmj 311(6999): pp. 251-253.
Carbone, M., Christensen, A. S., Nielson, F., Nielson, H. R.,
Hildebrandt, T. and Sølvkjær, M., 2013, August. ICT-
powered Health Care Processes. In International
Symposium on Foundations of Health Informatics
Engineering and Systems pp. 59-68. Springer Berlin
Heidelberg.
Carroll, N., 2016. Key success factors for smart and connected
health software solutions. Computer, 49(11), pp. 22-28.
Carroll, N., Kennedy, C. and Richardson, I. 2016
‘Challenges towards a Connected Community
Healthcare Ecosystem (CCHE) for managing long-term
conditions’, Gerontechnology, 14(2), pp. 64–77.
Delbanco, T. and Gerteis, M. 2012 ‘A patient-centred view
of the clinician-patient relationship’. Available at:
https://www.uptodate.com/contents/a-patient-centered-
view-of-the-clinician-patient-relationship (Accessed:
10 December 2019).
Egea, J. M. O. and M. V. R. González 2011. "Explaining
physicians’ acceptance of EHCR systems: an extension
of TAM with trust and risk factors." Computers in
Human Behavior 27(1): pp. 319-332.
Elwyn, G., S. Laitner, A. Coulter, E. Walker, P. Watson and
R. Thomson 2010. "Implementing shared decision
making in the NHS." BMJ 341: pp. 5146.
Epstein, R. M., K. Fiscella, C. S. Lesser and K. C. Stange
(2010). "Why the nation needs a policy push on patient-
centered health care. "Health affairs 29(8): pp. 1489-1495.
Epstein, R. M. and R. L. Street 2011. The values and value
of patient-centered care, Annals Family Med.
Focke, A. and Stummer, C., 2003. Strategic technology
planning in hospital management. Or Spectrum, 25(2),
pp.161-182. doi: org/10.1007/s00291-002-0118-y
Gelijns, A. C. 1992. Technology and health care in an era of
limits, National Academies Press.
Gerteis M, Edgman-Levitan S, Daley J. Through the
patient’s eyes. San Francisco: Jossey-Bass, 1993.
Gravel, K., Légaré, F. and Graham, I. D. 2006 ‘Barriers and
facilitators to implementing shared decision-making in
clinical practice: A systematic review of health
professionals’ perceptions’, Implementation Science.
doi: 10.1186/1748-5908-1-16.
Guest, G., K. M. MacQueen and E. E. Namey 2011. Applied
thematic analysis, Sage Publications.
A Patient’s Perspective on Decision-making for the Adoption of Digital Care Pathways
453

Hsieh, P.-J. 2015. "Physicians’ acceptance of electronic
medical records exchange: An extension of the
decomposed TPB model with institutional trust and
perceived risk." International Journal of Medical
Informatics 84(1): pp. 1-14.
Ismail, N. I., N. H. Abdullah, and A. Shamsuddin, Adoption
of Hospital Information System (HIS) in Malaysian
Public Hospitals. Procedia - Social and Behavioral
Sciences, 2015. 172: pp. 336-343.
Izzatty Ismail, N., Abdullah, H. and Shamsuddin, A. 2015
‘Adoption of Hospital Information System (HIS) in
Malaysian Public Hospitals’, Procedia-Social and
Behavioral Sciences, 172, pp. 336–343.
Joosten, E. A., L. DeFuentes-Merillas, G. De Weert, T.
Sensky, C. Van Der Staak and C. A. de Jong 2008.
"Systematic review of the effects of shared decision-
making on patient satisfaction, treatment adherence and
health status." Psychotherapy and psychosomatics
77(4): pp. 219-226.
Joseph-Williams, N., R. Evans, A. Edwards, R. G. Newcombe,
P. Wright, R. Grol and G. Elwyn 2010. "Supporting
informed decision making online in 20 minutes: an
observational web-log study of a PSA test decision aid."
Journal of medical Internet research 12(2): e15.
Lennarson Greer, A. 1985 ‘Adoption of Medical Technology:
The Hospital’s Three Decision Systems’, Article in
International Journal of Technology Assessment in
Health Care. doi: 10.1017/S0266462300001562.
Légaré, F., S. Ratté, K. Gravel and I. D. Graham 2008.
"Barriers and facilitators to implementing shared
decision-making in clinical practice: update of a
systematic review of health professionals’ perceptions."
Patient education and counseling 73(3): pp. 526-535.
Leroy, G., H. Chen and T. C. Rindflesch 2014. "Smart and
Connected Health [Guest editors' introduction]." IEEE
Intelligent Systems 29(3): pp. 2-5.
Lippeveld, T., R. Sauerborn and C. Bodart 2000. Design and
implementation of health information systems, Citeseer.
Mulley, A. G. 2009. "Inconvenient truths about supplier
induced demand and unwarranted variation in medical
practice." Bmj 339: b4073.
Saldaña, J. 2015. The coding manual for qualitative
researchers, Sage.
Stacey, D., F. Légaré, K. Lewis, M. J. Barry, C. L. Bennett,
K. B. Eden, M. Holmes-Rovner, H. Llewellyn-Thomas,
A. Lyddiatt and R. Thomson 2017. "Decision aids for
people facing health treatment or screening decisions."
Cochrane database of systematic reviews (4).
Teplensky, J. D., M. V. Pauly, J. R. Kimberly, A. L. Hillman
and J. S. Schwartz 1995. "Hospital adoption of medical
technology: an empirical test of alternative models."
Health services research 30(3): pp. 437.
Tornatzky, L. G., M. Fleischer and A. K. Chakrabarti 1990.
Processes of technological innovation, Lexington books.
Van Velsen, L., S. Wildevuur, I. Flierman, B. Van
Schooten, M. Tabak and H. Hermens 2016. "Trust in
telemedicine portals for rehabilitation care: an
exploratory focus group study with patients and
healthcare professionals." BMC medical informatics
and decision making 16(1): pp. 11.
Yang, Z., A. Kankanhalli, B.-Y. Ng and J. T. Y. Lim 2013.
"Analyzing the enabling factors for the organizational
decision to adopt healthcare information systems."
Decision Support Systems 55(3): pp. 764-776.
Yusof, M. M., J. Kuljis, A. Papazafeiropoulou and L. K.
Stergioulas 2008. "An evaluation framework for Health
Information Systems: human, organization and
technology-fit factors (HOT-fit)." International journal
of medical informatics 77(6): pp. 386-398.
HEALTHINF 2020 - 13th International Conference on Health Informatics
454
