
Creating Patient Decision Aid Tools
Andrea Corradini, Constantin Alexandru Gheoghiasa and Jesper Nordentoft
KEA Digital, Copenhagen School of Design and Technology, Lygten 37, 2400 Copenhagen NV, Denmark
Keywords: Patient Decision Aid Tools, Shared Decision Making, e-Health, Web Application.
Abstract: This paper reports on the creation of a web application that facilitates the development and implementation
of patient decision aid tools. We propose a software prototype model that allows medical personnel to easily
and rapidly create digital prototypes of patient decision aid tools independently on the medical condition. Our
application can be used as an online framework and is being tested by healthcare professionals.
1 INTRODUCTION
Several medical researchers and practitioners have
been advocating for enabling patients to have a more
active role in making decisions regarding the
treatments to choose to deal with their medical
condition. In order to achieve this, a shared decision
making process needs to be pursued and implemented
(Eason et al, 2012). Cross disciplinary studies have
shown several benefits for patients who are involved
in the decision process during their medical journey
(Lee & Emanuel, 2013). Those patients, once
empowered by providing them with a good
understanding of their condition, the diagnosis, the
possible set of treatments, and the pros and cons of
each of these treatments, can then make more
informed decisions about their treatment choice also
by factoring in personal wishes and life situation. One
of the main challenges in implementing this approach
is the appropriate creation of tools that can help
educating the patient, the healthcare professionals and
the other stakeholders involved in the patient’s
journey.
Patient decision aid tools (Ottawa Framework,
2019) have emerged as clinical frameworks or
guidelines in situations where there are alternative
courses of treatment. They are meant to educate the
patient and help him make a decision. Usually, these
tools are developed by researchers or healthcare
professionals in the form of small leaflets or paper
cards. In recent years, multimedia tools have been
emerging and a new development towards web-based
patient decision aid tools has also caught up
(Syrowatka et al., 2016). Developing patient aid tools
is not an easy process. It requires following a
standardized process that should include a carefully
planned development, available research-based
information, user testing, proper design, field testing
and evaluation (Coulter et al., 2013).
We created a prototype model of a web
application that makes it possible to create generic
decision aid tools. With the term generic, we refer to
a tool that is not tailored to a specific medical
condition but can instead be easily adapted to
accommodate to different conditions with only little
effort.
Our web application is intended to be a ready-to-
use software. It can be used as a sort of online content
management system for the generation of patient
decision aid tools that can be quickly prototyped and
generalized over medical conditions.
2 PATIENT DECISION AIDS
TOOLS
2.1 Related Work
The adoption of software programs by healthcare
professionals has seen an ascending trend in the last
decade. The joint work of software developers and
healthcare professionals has made it possible to create
tools that can help mediate the relation with the
patient, minimize the errors in the care process, help
doctors adhere to medical guidelines, streamline the
process and last but not least, help the patients to have
a better understanding of their illness, the treatment
options and their role in making a decision (Wright et
al., 2009).
Corradini, A., Gheoghiasa, C. and Nordentoft, J.
Creating Patient Decision Aid Tools.
DOI: 10.5220/0008951104070412
In Proceedings of the 13th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2020) - Volume 5: HEALTHINF, pages 407-412
ISBN: 978-989-758-398-8; ISSN: 2184-4305
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
407

Over the course of the last decade, medical
practitioners have documented better outcomes in
patients who have been actively involved in the
decision making (healio, 2016). The need to involve
patients in the medical decision process has been also
corroborated by scientific studies coming from the
area of medical sciences and socio-psychology (Lee
& Emanuel, 2013). The International Patient
Decision Aid Standards Collaboration has developed
quality criteria for the development of patients'
decision aid tools (Elwyn et al., 2016). The actual
development of such tools is then usually mainly
focused on specific illnesses, such as prostate cancer,
lung cancer, diabetes etc (AHRQ, 2019).
Like with most other areas, we have seen recently
a switch from the paper-based decision aid tools to
computer based ones. The benefits of digital decision
aid tools as compared to the paper based ones have
started to be investigated by both healthcare
professionals and researchers. The importance for
developing a computer-based decision aid tool was
supported by a review conducted by Syrowatka et al
(Syrowatka et al., 2016). The objective of this review
was to identify if computer-based decision aid tools
performed better than commonly used paper-based
decision aid tools. Furthermore, the same study made
a classification of the features that were integrated in
existing computerized decision aid tools. The purpose
of this classification was to identify whether specific
features performed better than others and to figure out
the degree of redundancy of incorporating certain
features in an effort to maximize the quality of the
decision making process. As with many other areas of
our lives, the online environment has the capability of
providing the user with a more interactive experience,
allows for a mix of multimedia components, which in
turns enables the user to have a better understanding
of the subject or theme that is being presented.
Furthermore, a digital decision aid tool can allow the
user to interact with it, thus making the information
presented and experience to be tailored to the specific
characteristics, needs and wants of the user.
As it has also been outlined in other research
studies (Hoffman et al., 2016), online platforms allow
for media rich components to be integrated, making it
possible for patients to benefit from a more
interactive experience that ultimately facilitates the
understanding of the information transmitted and
goes beyond the limitations of the paper-based
approaches. The media rich content can be presented
in terms of instructional videos, inserted in the
material send to the patient over the internet, or in
terms of dynamic graphs and images that can help the
patient better understand his individual case reported
to the average condition or how certain probabilities
related to the treatment would apply in his specific
case. Animations, icons and graphs can be used to
help bring the data from abstract to concrete. In
(Flynn et al., 2015), a computerized decision aid for
thrombolysis in acute stroke was developed. An
assessment on when it is the best time to
communicate to the patient certain medical related
information to ensure a proper reception and
understanding is also discussed.
One of the most prominent frameworks in the area
of decision aid tools development is Ottawa Decision
Support Framework (Ottawa Frameworks, 2019;
Ottawa Decision Aid, 2019). This framework is based
on identifying and resolving the decisional conflict
and is supported by extensive research from
psychology and sociology (Matlock and Spatz, 2014).
It consists of three major components: decisional
needs, decision quality, and decision support. The
potential impediments for adopting patient decision
aids on a large scale by clinicians is also discussed.
The main impediments identified were: poor
development, reluctance on the part of clinicians to
use them, prohibitive workflow, maligned incentives,
or inaccessibility at the time they are needed.
The web application we created facilitates the
development of patient decision aids tools and
incorporates several of the guidelines formulated in
the Ottawa Decision Support Framework. Our
applications is not a decision aid tool per se because
it does not target any specific illness. Our software
application focuses on the creation of web-based
decision aid tools for virtually any medical condition.
It provides a framework for the creation of a layout
where physicians and medical personnel can easily
enter research-based medical information and data to
educate patients and make it possible for them to
make choices when alternative treatments are
possible. With our application it is easy to quickly
prototype and standardize the creation of decision aid
tools. The data entered can be text, video clips, audio
clips, hypertext, and images.
2.2 Minimal Technical Requirements
While designing our application, and after an
empirical analysis of informal discussions with
medical personnel, we decided that it had to display a
set of minimum features. These are:
• web-based: the system must be accessible in a
web browser in order to avoid any additional
software installation
HEALTHINF 2020 - 13th International Conference on Health Informatics
408
• responsive: the user of the system will be able to
access the application from different screen-size
devices
• sharing and collaboration: this feature allows the
medical personnel to collaborate when creating
and defining the content of a given decision aid
tool for a specific condition
• published API for data communications: this
allows for a seamless integration of the
application with other systems used by the
medical organization
• print or export to PDF format: this caters for
patients that prefer a paper version of the tool;
digital features that are not available in paper
format (e.g. video clips) are to be replaced with
other supporting information and material (e.g. an
image of a QR code to scan with a cell phone and
play the video that could not be inserted in the
PDF).
2.3 User Roles
The system is designed with multiple user roles, each
role providing different levels of access and rights.
Specifically, we have the following roles and levels
of access:
• admin: it is the top-level user with access to the
entire technical related functions and user
administration functions; the typical person with
admin role is a developer or one person from the
medical institution
• designer: it is a specialist in creating patient
decision aid tool layouts; s/he designs and creates
new decision aid tools and usually has gone
through some training with the content
management system
• editor: it is person who provides the designer with
the research-based information when a certain
decision aid tool for a certain condition is being
created; s/he is a subject-matter expert but does
not need the technical expertise to create template
layouts
• user: it is the end user of the system, typically the
patient or a patient's relative, with no access to the
system back-end; s/he is only able to view, read,
provide personal input data entered via UI widgets
and print a decision aid tool after this was shared
with her/him in digital form by the medical
personnel.
Usually, the designer and editor are expected to
work in close collaboration when a new decision aid
tool is created. The designer turns the information
provided by the editor in graphical form and style
them according to a few predefined layouts.
3 PROTOTYPING GENERIC
PATIENT DECISION AID
TOOL
3.1 Overall System Architecture
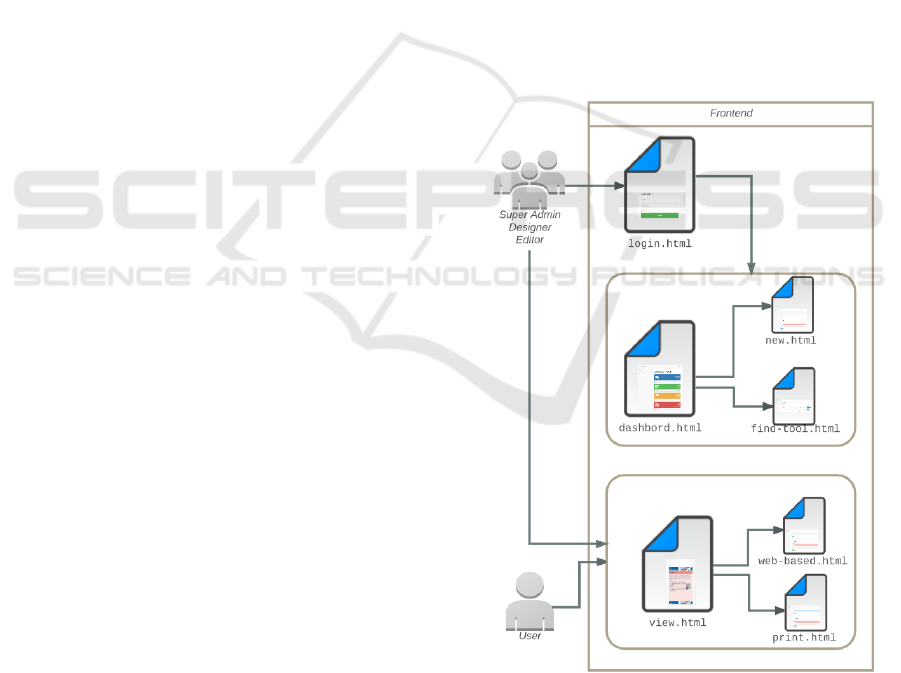
In this section, we present an overview of our system
architecture. We split the architecture into 3 main
components. Being a web application, we naturally
mapped our system onto a three-tier architecture
made up of a front-end, a middle tier, and a backend.
The front-end was created using standard web
technologies such as HTML 5, CSS 3, and a mix of
JavaScript and a set of JavaScript libraries. Figure 1
shows the different tasks allowed (indicated with file
names), the different user roles, and relations between
tasks and user roles.
Figure 1: Overall system architecture: front-end.
The system middle-tier is shown in Figure 2. We
created a model-view-controller architecture based on
PHP and hosted on a free cloud service. We
developed our own model-view-controller
Creating Patient Decision Aid Tools
409
architecture instead of using an existing framework.
Frameworks can prove very efficient in terms of
development time and security. Frameworks that are
used on a large scale have high security
implementations and the pre-built functions can
speed the process of development from hours to
minutes. However, frameworks have also limitations
(Manger et al., 2015). One of the major limitations is
that the developer is constrained to work within its
specifications and limits. In our context, we wanted
to be sure to be browser independent and to not
decrease our application performance due to large
overhead of additional framework code. Moreover, it
can prove difficult to introduce multiple frameworks
in the same project and due to the library limitations,
for the development of our application multiple
frameworks would have been required.
Frontend and middle-tier communicate with each
other through an RESTful API that, while
emphasizing the separation of concerns principle
among component, also acts as the system gateway to
data. With the API it is also possible to integrate our
architecture into other systems that the medical
institution might use.
Figure 2: Overall Architecture: Middle-Tier and Back-End.
Eventually, a MySQL database is used to persist
the data related to the information and meta-data
stored in each patient decision aid tool.
3.2 Creating a Decision Tool
In the section, we report on the process and steps
necessary to the creation of a patient decision aid tool.
The designer is the person in charge of going
though this process. Whenever a new decision aid
needs to be generated, basic information about it is
required for laying out a first simple structure of the
digital document (see Figure 3). This includes for
instance the title to assign to the decision aid tool, a
set of semantic tags, an image, and a variable number
of sections. The title is used on the cover page as well
as to identify the decision aid. The semantic tags are
keywords used to describe the decision aid tool being
build. These tags are used for search and
classification purposes when more aid tools are
available on the system backend. An image is
provided to ensure the visual identity of a decision aid
tool. While collecting system requirements, we were
made clear by the management of the hospital we
started this project on, that it was important to have a
uniquely identifiable message or text on whatever
decision aids implemented both on paper aids and
digital aids. At this stage, the image is typically the
logo of the institution. This is be placed as a footer on
each section/page of the decision aid tool being
created. An additional image can be uploaded to act
as background image throughout the pages of the
final product. Sections are the core components of a
decision aid tool, notably where the subject-matter
information is actually structured. This information
must be provided by subject-matter expert.
Figure 3: Initial steps in creating a new decision aid tool.
Each section has three main components: a title, a
color and the content of the section. At the moment,
we have a set of predefined sections including:
introduction, condition description, treatments, pros
and cons, user preferences, decision, conclusion, and
glossary. More sections can be created, and sections
can be deleted as well.
In the introduction section, text can be added to
introduce who is this tool targeted to or any other
information the expert believes should be conveyed
HEALTHINF 2020 - 13th International Conference on Health Informatics
410
at the very begin of the decision aid tool. The
condition description section provides an overview of
the medical condition. The section ‘treatment’
describes the available treatments along with the pros
and cons for each of them. The section ‘user
preferences’ is essentially supposed to be a short
questionnaire that the patient is asked to filled in.
The questionnaire can contain multi-choice
questions as well as open questions. Right after that
section, a typically one-page section follows where
the patient summarizes his/her decision, based on the
information process until that point. A possible
decision is not to decide any treatment at that point
but rather defer the choice, that is, delay the decision
to a later point in time or avoid the decision
altogether. A conclusion section is used to inform the
patient of the expected next steps. Eventually a
glossary section is used to list and describe all the
technical terms used in the decision aid tool. Sections
are color-coded i,e, are associated with different
colors to allow for a better navigation of the tool by
the intended final user.
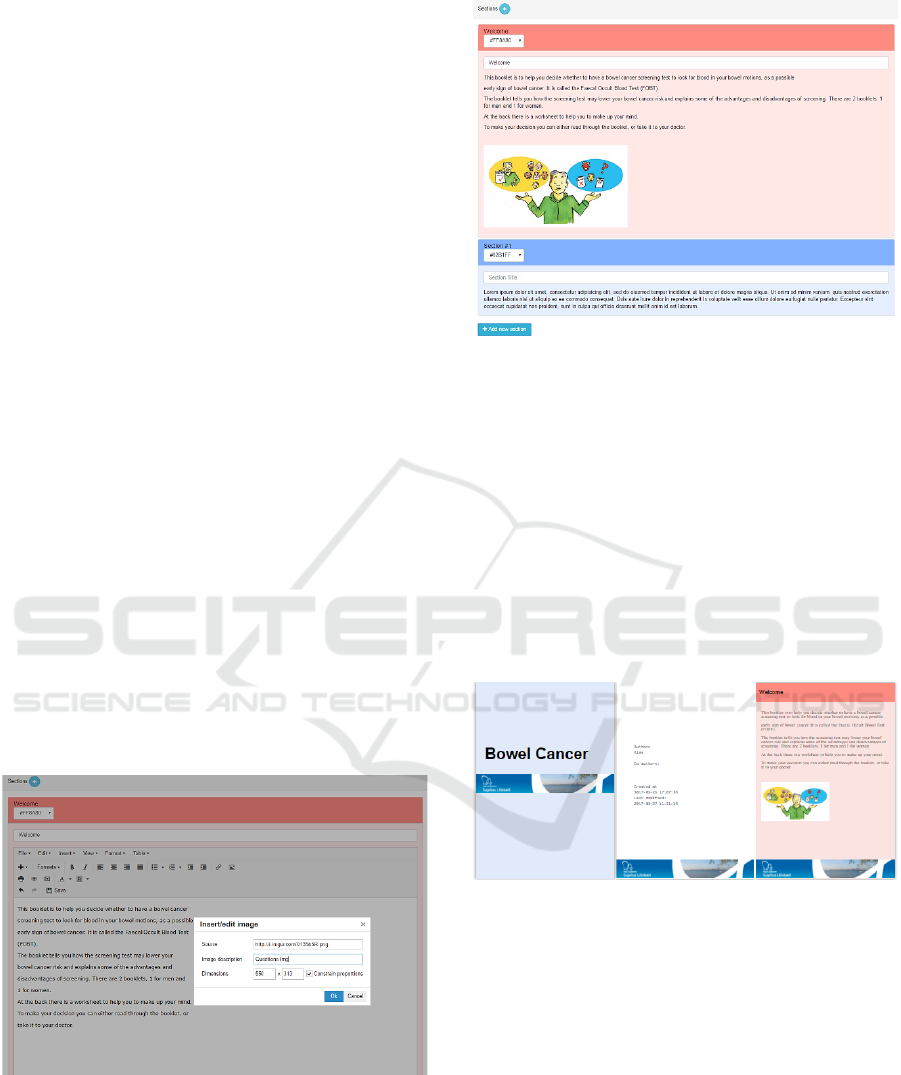
One of the most powerful functionalities of the
system is the way through which the content of a
section is created or edited. Once the designer presses
on the content of a section, an HTM editor is enabled.
The editor makes it possible for the user to enter and
edit the content of the section in any way s/he wants.
Figure 4 shows a screenshot of the editor in action,
more precisely in a case where the designer was
attempting at inserting an image into a section. Once
the designer finishes editing the content of a section,
s/he can save it and preview it.
Figure 4: Inserting an image in a section with text.
Figure 5 and Figure 6 show how a new decision
aid tool may look like in print mode (i.e. after
selecting the option to print the digital patient
decision aid tool) and the digital version after some
content has been added, respectively.
Figure 5: Patient decision aid tool as it looks in preview
mode after some data has been entered.
Another functionality of the tool is the
collaboration and sharing mechanism for the tools.
Here is the place where a designer can request access
to a tool if s/he does not have access to this tool yet.
Another functionality under development is the
automatic addition of terms into the glossary. The
rationale here is that, once the designer enter text into
a section, s/he can highlight a (sequence of) term(s)
and provide a description for it. By doing so, the term
will automatically be added in the glossary section
along with the description of its meaning.
Figure 6: The first three pages of a patient decision aid tool
formatted in print mode (preview).
4 CONCLUSION AND OUTLOOK
We developed a web-based application that helps
create generic patient decision aid tools. Our system
was developed based on requirements collected with
healthcare professional working at a Danish hospital.
At the moment, the system exists in its prototype
for it still requires further work and development even
after it has been released to the users for testing.
Primary usability testing with a few beta testers
resulted in positive feedback. The usability of the
Creating Patient Decision Aid Tools
411

system needs be thoroughly tested in the field, as the
purpose of this software is to become a tool that
professionals are willing to use and comfortable with.
The system usability also has to target a set of quality
criteria (Syrowatka et al., 2016; Elwyn et al., 2006)
Specifically, user testing needs to figure out if the tool
we have developed
• provides information in sufficient detail,
• presents data in an unbiased manner,
• includes methods to clarify values and
preferences,
• provides structured guidance for deliberation and
communication,
• presents information in a balanced manner,
• presents up-to-date research-based medical
evidence,
• discloses conflicts of interest,
• uses an appropriate plain language, and
• ensures that the decision is informed and value-
based
The API that we implemented allows for future
integrations of the software into the systems that the
healthcare professionals are already using on a daily
basis. The integration can be done based on both a
push or pull model.
As the next development step, we plan to integrate
the system with Merriam-Webster’s Medical
Dictionary (Merriam-Webster, 2019) and Google
Custom Search (Google, 2019). This integration will
allow the users to be able to access additional
resources in creating decision aid tools and the
patients will be able to find definitions of any terms
in a tool, if in doubt about the meaning.
REFERENCES
Eason, G., Elwyn, G., Frosch, D., Thomson, R., Joseph-
Williams, N., Lloyd, A., … Barry, M., 2012. "Shared
Decision Making: A Model for Clinical Practice",
Journal General Internal Medicine, 27(10):1361–1367.
Lee, E. O., & Emanuel, E. J., 2013. "Shared Decision
Making to Improve Care and Reduce Costs". New
England Journal of Medicine, 368(1):6–8.
Ottawa Hospital Research Institute, 2019. "Ottawa
Decision Support Framework", [Online] https://
decisionaid.ohri.ca/odsf.html (accessed on October
2019).
Syrowatka, A., Krömker, D., Meguerditchian, A. N., &
Tamblyn, R., 2016. "Features of Computer-Based
Decision Aids: Systematic Review, Thematic
Synthesis, and Meta-Analyses". Journal of Medical
Internet Research, 18(1):20.
Coulter, A., Stilwell, D., Kryworuchko, J., Mullen, P. D.,
Ng, C. J., & van der Weijden, T., 2013. "A systematic
development process for patient decision aids". BMC
Medical Informatics and Decision Making, 13(2):2.
Wright, A., Bates, D. W., Middleton, B., Hongsermeier, T.,
Kashyap, V., Thomas, S. M., & Sittig, D. F., 2009.
"Creating and sharing clinical decision support content
with Web 2.0: Issues and examples". Journal of
Biomedical Informatics, 42(2):334–346.
healio.com, "Shared decision making can lead to better,
individualized care,” Jan. 2016. [Online]. http://www
.healio.com/optometry/primary-care-optometry/news/
print/primary-care-optometry-news/%7B45e3e538-3b
8a-4847-b98f-ae5158a7950c %7D/shared-decision-ma
king-can-lead-to-better-individualized-care (accessed
on October 2019).
Elwyn, G., O’Connor, A., Stacey, D., Volk, R., Edwards,
A., Coulter, A., … Whelan, T., 2006. "Developing a
quality criteria framework for patient decision aids:
online international Delphi consensus process". BMJ,
333(7565):417.
AHRQ–Agency for Healthcare Research and Quality,
"Patient Decision Aids - Effective Health Care
Program". 2019. [Online] http://effectivehealthcare.
ahrq.gov/index.cfm/tools-and-resources/patient-
decision-aids/ (accessed on October 2019).
Hoffman, A. S. , Volk, R. J., Saarimaki, A., Stirling, C., Li,
L. C., Härter, M., Kamath, G. R., & Llewellyn-Thomas,
H., 2013. "Delivering patient decision aids on the
Internet: definitions, theories, current evidence, and
emerging research areas,” BMC Medical Informatics
and Decision Making, 13(2):13.
Flynn, D., Nesbitt, D. J., Ford, G. A., McMeekin, P.,
Rodgers, H., Price, C., Kray, C., & Thomson, R. G.,
2015. "Development of a computerised decision aid for
thrombolysis in acute stroke care". BMC Medical
Informatics and Decision Making, vol. 15, pp. 6.
Ottawa Hospital Research Institute, "Conceptual
Frameworks". [Online] https://decisionaid.ohri.ca/
models.html (accessed on October 2019).
Ottawa Hospital Research Institute, "Decision Aid Toolkit
- Patient Decision Aids". [Online]. https://decisionaid.
ohri.ca/resources.html (accessed on October 2018).
Matlock, D. D., & Spatz, E. S., 2014. "Design and Testing
of Tools for Shared Decision Making". 2014.
Circulation: Cardiovascular Quality and Outcomes,
7(3):487–492.
Manger, C., Trejderowski, T., & Paduch, J., 2010.
"Advantages and disadvantages of framework
programming with reference to Yii php framework,
gideon .net framework and other modern frameworks".
Studia Informatica, 31(4A):119–137.
dictionaryapi.com, "Merriam-Webster’s Medical
Dictionary with Audio" [Online]. https://www.
dictionaryapi.com/products/api-medical-dictionary.
htm (accessed on October 2019).
developers.google.com, "Google Custom Search". [Online]
https://developers.google.com/custom-search/
(accessed on October 2019).
HEALTHINF 2020 - 13th International Conference on Health Informatics
412
