
An Efficient Algorithm for Kinematics Estimation with Application
to Dynamic Gait Stability using a Contact-less Skeleton Tracking
System
Michael Uelschen
1a
, Heinz-Josef Eikerling
1
, Sabrina Rbib
3
and Helge Riepenhof
2
1
Faculty of Engineering and Computer Science, University of Applied Sciences Osnabrück, 49076 Osnabrück, Germany
2
BG Klinikum Hamburg, Bergedorfer Str. 10, 21033 Hamburg, Germany
3
University of Lübeck, 23562 Lübeck, Germany
Keywords: Gait Analysis, Kinematics Estimation, Marker-less Skeleton Tracking, Orthopaedic Technical Support.
Abstract: This paper presents an optimized algorithm for estimating static and dynamic gait parameters. We use a
marker- and contact-less motion capture system that identifies 20 joints of a person walking along a corridor.
Based on the proposed gait cycle detection basic metrics as walking frequency, step/stride length, and support
phases are estimated automatically. Applying a rigid body model, we are capable to calculate static and
dynamic gait stability metrics. We conclude with initial results of a clinical study evaluating orthopaedic
technical support.
1 INTRODUCTION
The precise monitoring of regaining walking ability
after surgery treatment or the ability to compensate
disabilities caused by injuries is of importance as this
information can guide the rehabilitation process. In
current clinical practice, dynamic stability is usually
assessed using the Berg Balance Scale (Berg, Wood-
Dauphinee, Williams, & Maki, 1992) and gait speed
is usually assessed using the 10-meter walking test.
While these outcome measures have proven their
applicability in daily clinical practice, they have some
drawbacks for guiding the rehabilitation process or
tailoring remedial provisions. First of all, the scores
on the clinical scales do not show insight into the
mechanisms that contribute to a potential
improvement on the clinical scale. If for instance an
increased dynamic balance is found on the Berg
Balance Scale, it is not known whether this is the
result of recovery of the affected leg or an increased
use of the non-affected leg. The same applies for an
increased gait speed as measured on the 10-meter
walking test: it is unclear whether an increased gait
speed is the result of an increased step length and/or
an increased cadence (steps/min). Thus, a more
detailed movement analysis based on measurable
metrics would be of service.
a
https://orcid.org/0000-0002-0841-6954
Within research, dynamic stability has been
increasingly quantified relating the position of the
body’s center of mass (CoM) to the base of support
(BoS). The base of support is composed of the two
feet and the area between them. For elderly fallers it
has been shown that they exhibit a different
separation between the center of mass and base of
support during walking, when compared to elderly
non-fallers. This result suggests that the movement of
the center of mass in relation to the base of support
might enable the separation of fallers from non-
fallers, which would be of high clinical relevance.
Tracking the movement of the center of mass in
relation to the base of support, however, usually
requires a fully instrumented gait analysis which is
technically challenging, time-consuming and costly.
Hence, the use of instrumented gait analysis in daily
clinical practice is limited. Because of this, there is a
demand for a system that is capable of measuring foot
placement and center of mass plus is easy to use, fast
to set up, and affordable. By quantifying foot
placement, the system can also be used to detect
whether an increased walking velocity is the result of
an increased step length and/or an increased cadence.
For characterizing a patient’s gait according to the
above measures, the DynMetrics (Eikerling,
Uelschen, & Lutterbeck, 2016) system was extended
94
Uelschen, M., Eikerling, H., Rbib, S. and Riepenhof, H.
An Efficient Algorithm for Kinematics Estimation with Application to Dynamic Gait Stability using a Contact-less Skeleton Tracking System.
DOI: 10.5220/0008943100940101
In Proceedings of the 13th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2020) - Volume 1: BIODEVICES, pages 94-101
ISBN: 978-989-758-398-8
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
to devise the above measures. The marker-less
motion capturing system is capable of tracking foot
placement and the body’s center of mass by a network
of optical sensor nodes.
2 METHOD
2.1 Motion Capturing
The key algorithm was integrated into the contact-less
and marker-less gait recognition system DynMetrics
(Uelschen & Eikerling, 2015). The system permits to
capture and analyse the gait of a subject along a
walking corridor without any time-consuming pre-
paration of the person caused e.g. by attaching mar-
kers.
T
he system consists of a series of independent
sensor nodes that record the movements of a person
passing by. The constituent 3D data streams are fused
into a single continuous skeleton stream which is
based on a global coordinate system.
2.2 Algorithm Overview
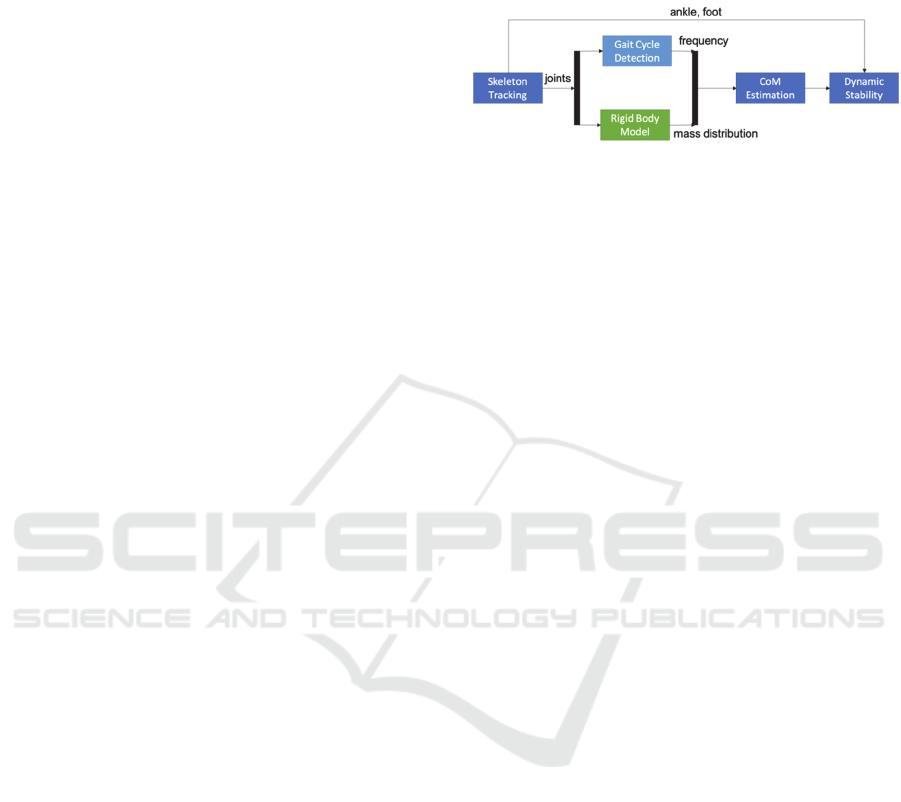
The block diagram shown in Figure 1 outlines the
proposed algorithm. The skeleton tracking system
outputs a skeleton stream of a moving subject. The
joints of each skeleton are used two-fold: (i) as input
to the gait cycle detection, and (ii) as basis for the
calculation of a rigid body model.
The control of postural stability or balance is an
essential function in human movements. It is defined
(Shumway-Cook & Woollacott, 2017) as a person’s
ability to keep the line of gravity passing through the
center of mass within the base of support area beneath
that person. In general movement tasks can be
classified into static (sitting or standing) and dynamic
(walking) stability.
In order to obtain these metrics, the center of mass
is estimated beforehand. Finally, using the ankle
positions the dynamic stability of gait is calculated.
The complete process is highly automated and
does not require any interaction by the operator of the
system (e.g. physical therapist). Therefore, we
achieve a high degree of reproducibility.
2.3 Contribution
The contributions of this paper are: (i) a rigid body
model that allows to derive CoM and that
approximates the gold standard, (ii) the estimation of
the gait frequency based on gait cycle detection using
linear regression, (iii) the computation of stability
metrics such as XCoM, and BoS based on the
inverted pendulum model, and (iv) initial results on a
clinical study evaluating orthopaedic footwear and
orthotics.
Figure 1: Pipeline algorithm.
3 GAIT CYCLE DETECTION
In this section we discuss the application of a peak-
finding algorithm in order to identify the gait cycles.
The estimated gait frequency (or alternatively
cadence) is an input parameter for the subsequent
stability assessment. The procedure uses the skeletal
data gained by tracking a patient's movements. First,
we explain the mathematical foundations.
3.1 Mathematical Preliminaries
The position in space is given as, where is the
temporal parameter,
,
,
(1)
We denote as anterior-posterior (main moving
direction), as horizontal, and as longitudinal axis.
For the metrics of gait stability, often only the
behavior in the horizontal plane is considered. That
implies
0.
The skeleton tracking system provides the
position of the skeleton as a stream of frames at
discrete points in time, which are given by
where
denotes the ordering of the frames in the sequence.
The skeleton tracking system estimates the
position of twenty joints in each frame: head,
shoulder center, spine, hip center, and in addition for
both body sides: shoulder, elbow, wrist, finger, hip,
knee, ankle, and toe. This raw data is the only input
to the algorithm that estimates the kinematics and
further gait metrics.
3.2 Gait Cycle
The recognition of individual steps is required to
estimate the dynamic gait metrics. We follow the
nomenclature given by (Perry & Burnfield, 2010).
The normal gait pattern is periodic, where a
period corresponds to a single stride. According to
An Efficient Algorithm for Kinematics Estimation with Application to Dynamic Gait Stability using a Contact-less Skeleton Tracking
System
95
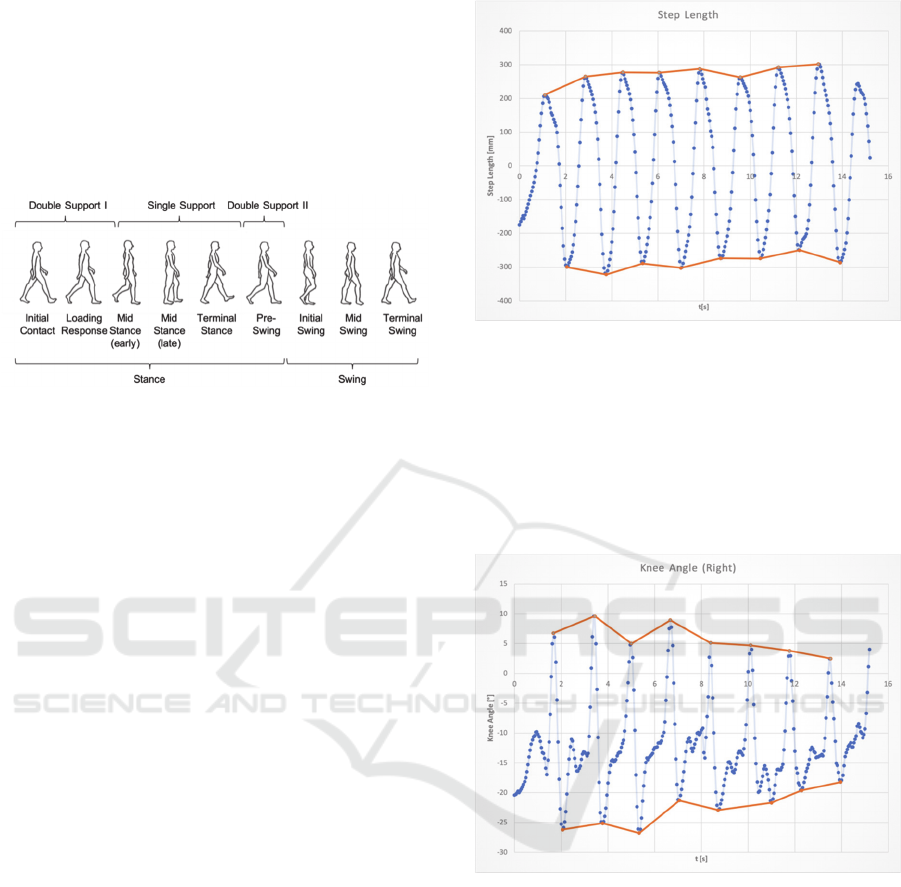
Figure 2, adapted from (Götz-Neumann, 2015), each
cycle can be divided into distinct phases.
The stance phase consists of five sub-phases
followed by the swing phase. It is composed of three
swing sub-phases before the gait cycle is completed.
The identification of the gait phases provides
important information for the clinical evaluation of a
patient's gait pattern.
Figure 2: Gait Cycle Breakdown.
Below we describe an optimized procedure which
automatically divides the movement into individual
gait cycles.
Each phase of a cycle is started or ended by a
defined event. Our algorithm identifies the following
gait events: minimum, maximum and zero distances
of the positions of the left and right ankle; maximum
flexion of the ipsilateral and contralateral knee; and
the vertical position of the lower limb (shank)
In order to find minimum or maximum values of a
function we need to identify the peaks in usually
noisy signal data. Under the assumption that has
a periodic shape the automatic multiscale-based peak
detection (AMPD) algorithm (Scholkmann, Boss, &
Wolf, 2012) provides a stable approach. A major
advantage of the algorithm is the absence of any
problem-specific parameter, so that a specific tuning of
the algorithm to the problem is not necessary. The
stability and reliability are proved by several
biomedical and non-biomedical applications.
In order to determine the individual gait phases, the
movement of the person is first divided into individual
steps. The distance between the left and right ankle is
used as the step length. A step is finished when the
distance becomes maximum or minimum.
Figure 3 shows the AMPD algorithm detecting
minimum and maximum distances of the left and right
ankle. Due to the calculation method the algorithm
may fail to find the initial or final peak.
Based on the detected gait cycles we can derive
basic temporal-spatial parameters (TSP) as step/stride
width and length, walking speed, and cadence given in
steps per minute. The latter parameter can then be used
to determine the gait frequency. These parameters are
used
for evaluation in the study described subsequently.
Figure 3: Peak detection using AMPD algorithm.
The transition from loading response to mid
stance is triggered when the knee angle of the
contralateral leg reaches its maximum value. The
AMPD algorithm detects the peak values (see Figure
4) reliably even if the curve shows a more complex
behaviour. The algorithm avoids to detect local
extreme values.
Figure 4: Detection of the flexion angle of the right knee.
4 GAIT STABILITY
The following section discusses how to derive the
center of mass and gives a sinusoidal approximation
based on the periodic walking pattern. This section
ends with advanced metrics in order to evaluate the
dynamic stability.
4.1 Rigid Body Model
In order to evaluate the stability of walking the center
of mass is a relevant parameter. To determine this
parameter, a body model is necessary, since the center
BIODEVICES 2020 - 13th International Conference on Biomedical Electronics and Devices
96
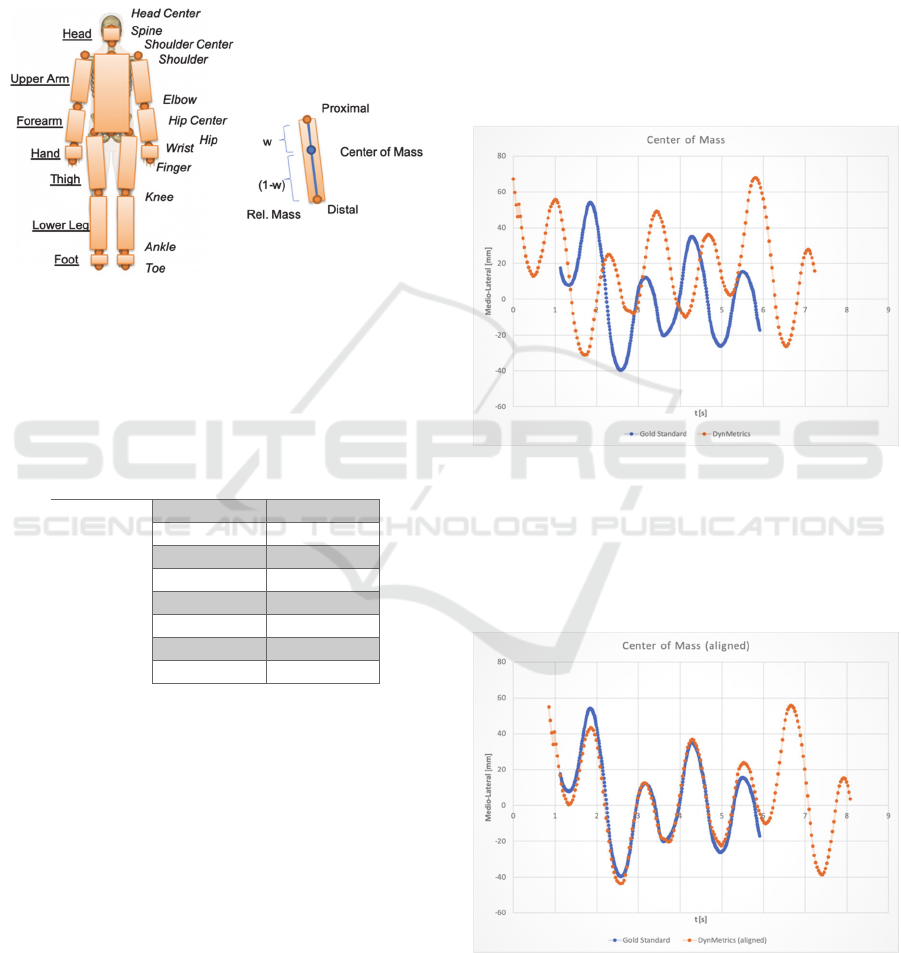
of mass is very difficult to obtain directly. We use a
segmented body model following the approach from
(Hanavan, 1964). Based on the skeleton the body
segments are defined.
Figure 5
shows on the left a 14-
segment body model, e.g. the forearm segment is
bound by the wrist and elbow joint. Each segment has
an individual center of mass and a percentage weight.
Figure 5: Segmented body model.
Finally, the overall center of mass is given by the
weighted mean of all single segments (Winter, 2009).
Table 1 summarizes the anthropometric data used for
the estimation of segments’ center of mass.
Table 1: Anthropometric data.
Segment Relative Mass w/(1-w)
Head 7.0
Trunk 43.0 0.60/0.40
Upper Arm 3.6 0.43/0.57
Forearm 2.2 0.43/0.57
Hand 0.7 0.30/0.70
Thigh 11.4 0.43/0.57
Lower Leg 5.3 0.43/0.57
Foot 1.8 0.43/0.57
The center of mass of each segment is defined by
its relative location with respect to the proximal ()
and distal (1) end point of the segment (see right
part of
Figure 5
). For example, the forearm segment
contributes 2.2% to the total mass. The segment is
spanned by the elbow (proximal) and wrist (distal)
joint of the skeleton. Its center of mass position is
given by
CoM,forearm
0.43∙
elbow
0.57
∙
wris
t
(2)
4.2 Gold Standard Comparison
The sketched rigid body model is compared to a
commercial marker-based motion capture system
(Vicon) that represents the gold standard. The
walking pattern of a person is recorded in parallel
using the DynMetrics and the Vicon system. The
center of mass of both systems is compared and
subsequently the deviation is analyzed. Vicon
(VICON, 2017) uses a similar segmented body model
as described, but the center of mass estimation is
based on different anthropometric data. Due to the
different local coordinate systems and the deviation
of the internal clocks the comparison of both time
series shows a shift in temporal and spatial direction
(see Figure 6). Also, the field of view and the frames
per second are varying.
Figure 6: CoM estimation compared to gold standard.
In order to avoid such effects both data sets are
aligned using an iterative closest-point algorithm.
Figure 7 shows the aligned time series. The result
indicates that DynMetrics estimates the body model
similar to the gold standard.
Figure 7: The aligned time series have similar shape.
An Efficient Algorithm for Kinematics Estimation with Application to Dynamic Gait Stability using a Contact-less Skeleton Tracking
System
97
4.3 CoM Sinusoidal Approximation
A relevant stability criterion is the medio-lateral
displacement of CoM. Due to the periodic walking
pattern we approximate CoM as a simple harmonic
motion within the horizontal plane, which is given as
CoM
∙sin
(3)
The amplitude (displacement) is denoted by
,
the angular frequency 2, and the phase angle
. During several functional tests of our skeleton
tracking system we observed that some subjects
slightly turned to the left or to the right while walking.
In order to get better approximation results we add
this drift perpendicular to the motion in anterior-
posterior direction. This results in the following
model
CoM
∙sin
(4)
In order to estimate the unknown parameter, we
use multiple linear regression method. Applying the
angle addition theorem
sinsincoscossin
(5)
we can rewrite equation (3) as
sin
sincos
cossin
(6)
From this we derive the motion equation
CoM
sin
cos
(7)
using
,
cos
,
sin
,
,
(8)
Based on skeleton frames and applying the
sketched body model
,
CoM,
with 0,…,
1 we get the following linear system of equations that
can be solved using the least squares method. The
vector representation is given by the following
equation:
CoM
∙
(9)
with
CoM
CoM,
CoM,
⋮
CoM,
(10)
1sin
cos
1sin
cos
⋮⋮ ⋮ ⋮⋮
1sin
cos
(11)
(12)
In order to find the solution equation (9) can be
rewritten to
∙
CoM
(13)
The motion in anterior-posterior direction of
CoM
is approximately linear. Since the subject
usually begins walking from double limb support
with velocity 0, we apply the linear regression
method to a polynomial of fourth degree. This gives
better approximation results as a simple linear motion
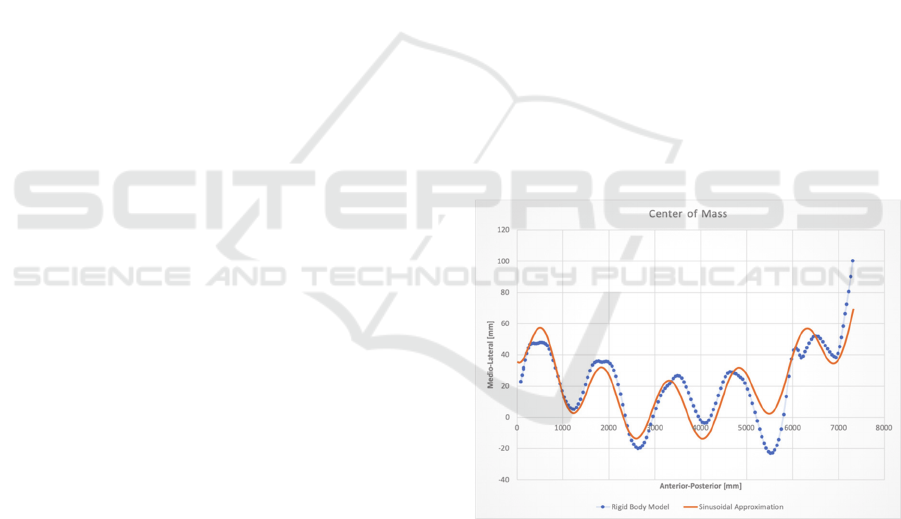
model. Figure 8 plots the behavior of center of mass
in two variants. The first curve is based on the
described body model. The second curve
approximates the periodic oscillations in medio-
lateral direction.
Figure 8: Center of mass exhibits sinusoidal behaviour.
4.4 Dynamic Stability
CoM is an established stability metric in static
situations. For the evaluation of the dynamic stability
of gait we follow the approach by (Hof, Gazendam,
& Sinke, 2005) that additionally considers the
velocity of CoM
CoM
that leads to extrapolated CoM
which is denoted as XCoM.
On the basis of the inverted pendulum model,
XCoM adds an additional displacement to the center
BIODEVICES 2020 - 13th International Conference on Biomedical Electronics and Devices
98

of mass position depending on the velocity of the
person divided by
/
, being the acceleration
of gravity and leg length. The parameter
is the
eigenfrequency of a non-inverted pendulum with
length .
The calculation of the dynamic gait stability
therefore results in
XCoM
CoM
CoM
(14)
XCoM
CoM
CoM
(15)
using velocity
CoM
CoM
,
CoM
.
We approximate using the gait frequency that
results from the cycle detection. The literature shows
different definitions of BoS, as for example in (Wu,
Brown, & Gordon, 2017) the lateral position of the
5th metatarsal bone is used.
Our approach is similar to (Hak, van Dieën, van
der Wurff, & Houdijk, 2014) using the position of the
lateral malleolus. For the calculation of the base of
support (BoS) and afterwards the margin of
stability (MoS)
we use the ankle position of the
left
left
and right foot
right
lef
t
leftsupport
right
rightsupport
lef
t
ri
g
h
t
/2 doublesupport
(16)
Finally, the margin of support is the difference
between the extrapolated CoM and BoS
XCoM
(17)
Figure 9: Dynamic gait stability.
The example in Figure 9 shows the dynamic
stability metrics XCoM and BoS.
In addition, the support phases are sketched below.
The BoS curve oscillates in medio-lateral direction
depending on the support phase.
5 ORTHOPAEDICS CASES
Figure 10: Walking corridor with four sensors on tripods.
5.1 Introduction
From an orthopaedics point of view, walking is a
complex process. The gait cycle - as pointed out in
section 3.2 - can be divided into different phases. This
division permits to distinguish in detail physiological
gait patterns from pathological forms and describe the
observable deviations in a differentiated way. In
addition, certain deficits in patients’ feet or lower
limbs can be at least partly compensated by
supporting orthopedic aids. In particular, the
provision of insoles or shows tailored to the patient
are common practical methods. The gait pattern of a
healthy subject shows some specific parameters and
all walking phases effect the main elements of
walking, walking speed, cadence and stride length.
Normally the gait patterns are periodic and fluent.
We have therefore extracted these elements from
the DynMetrics data using, both with and without
orthopedic additives (see (Götz-Neumann, 2015) for
reference values): (i) walking speed, (ii) cadence and
(iii) stride length. When people gain confidence while
walking, they usually increase walking speed,
cadence, and also stride length.
5.2 Method
Within
a
study
we
analysed
the
gait
of
53
impaired
subjects by means of the DynMetrics system. They
walked (see Figure 10) a distance of 8 m four times,
An Efficient Algorithm for Kinematics Estimation with Application to Dynamic Gait Stability using a Contact-less Skeleton Tracking
System
99
twice with orthopaedic technical support such as
custom-made insoles or adapted orthopaedic footwear
and twice without any aids. In addition to the analysis
of the gait, the subjects were asked assess the level of
achiness while walking by means of the Visual Analog
Scale (VAS) as shown in Figure 11.
The inclusion criterion of our investigation was
that an orthopaedic dressing assumed to be medically
indicated and that the orthopaedic compensation had
already been assessed as fitting by the attending
physician. Amputees were excluded from the study. In
the study design, it was also determined that the test
persons completed the four repetitions with and
without orthopaedic preparation in random order.
Figure 11: Visual Analog Scale (VAS).
5.3 Results
In subsequent discussion, the obtained results of two
test persons will be used as examples to point out the
change with respect to gait caused by using custom
made orthopaedic footwear. Subject 1 is 44 years old,
male. His dressing on the footwear includes a leg
length compensation of 1 cm and a shaft stiffener.
Subject 2 is 56 years old, male and his dressing
includes a heel elevation, shaft stiffening and rolling
aid, as well as diabetic soft tissue bedding.
Table 2: speed, cadence, stride length and VAS number of
subjects with and without orthopaedic additives.
Speed
[m/min]
Cadence
[1/min]
Stride
Length[m]
VAS
Number
Subject 1
With
additives
40.74 83.5 0.98 4
Without 34.16 84.2 0.81 5
Difference 6.58 -0.7 0.17 -1
Subject 2
With
additives
80.54 106.0 1.52 2
Without 72.80 112.4 1.30 3
Difference 7.74 -6.4 0.22 -1
Table 2 shows the arithmetic mean of the detailed
measures. Both cases are similar with respect to the
differences. There is increasing walking speed in both
cases while using orthopaedic additives. Subject 1
covers the distance by 6.58 meters per minute and
subject 2 by 7.74 meters per minute. The stride length
shows a similar pattern, both cases have an increased
stride length. With increasing walking speed and stride
length in both cases also the cadence decreases.
5.4 Discussion
As can be easily seen, painful walking influences the
walking speed. With increasing pain, the walking
speed decreases. The walking speed is mainly
influenced by the stride length and cadence. The
present study shows that the stride length increases
with decreasing pain and the cadence decreases. This
corresponds to the behavior of people with a physio-
logical, painless gait pattern. It is therefore not to be
assumed that the cadence is primarily increased by
orthopedic adjustments, but rather by the stride length,
which leads to a decrease in cadence at the same speed.
There is clearly a reverse correlation between cadence
and stride length. This means that as the cadence
increases while the stride length decreases and vice
versa in healthy and lower extremity disabled
population.
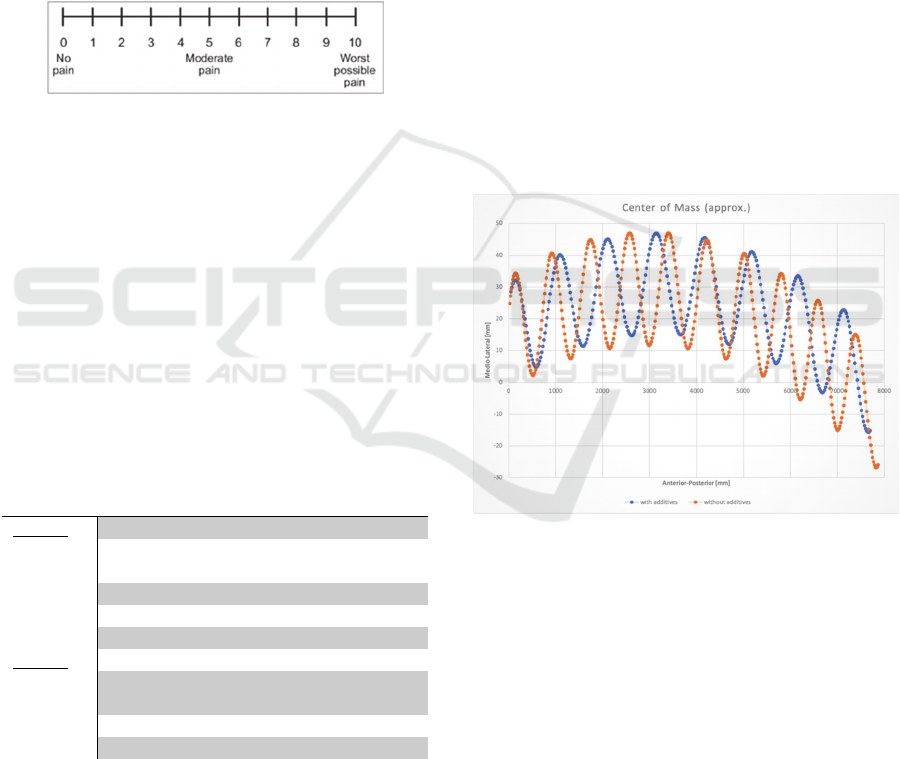
Figure 12: CoM depending on using orthopaedic additives.
Figure 12 shows the sway of subject 1. Due to
larger stride length when using orthopaedic footwear,
the oscillations are less dense. The medio-lateral
displacement without using orthopaedic footwear is
increased by 5 mm. From an orthopaedic point of view,
trunk control indicated by the CoM oscillations
essentially depends on the applicability of the deep
trunk muscles (Van Criekinge, et al., 2017). The
present investigations represented exclusively
volunteers who had completed or are in the final phase
of the rehabilitation process. At this point of therapy, a
significant improvement in trunk stability should
already have been achieved in any case, so that no
significant changes are to be expected in the area of
trunk control using orthopaedic aids.
BIODEVICES 2020 - 13th International Conference on Biomedical Electronics and Devices
100

6 CONCLUSIONS
In this paper we have presented a pipelined algorithm
that derives temporal-spatial and dynamic gait
parameters from skeletal data streams. Due to the
marker- and contact-less approach and the resulting
low effort the DynMetrics system which incorporates
the devised algorithms is able to be used in daily
clinical practice.
In order to give evidence for this we have used
system to track gait improvements for patients in need
of orthopaedic aids, i.e. according footwear and/or
insoles. Specifically tailoring such aids to the
individual patient is crucial to improve locomotion
and avoid pain. It could be shown that by featuring
the system the effect of using orthopedic additives
can be captured by objective, quantitative metrics
thus supporting the attending physician to direct the
prescription of compensating measures. In our basic
study we were able to nail down the differences in
essential gait parameters for patients with and without
those additives.
DynMetrics turned out to be suitable to capture
the according data in reasonable time without major
preparation effort. As expected, the additives can
have a positive influence on the walking speed, stride
length and cadence. Moreover, pain as measured by
VAS can be lessened by the use of these additives. In
addition to the use cases (orthopaedic and
neurological rehabilitation), the presented algorithm
can also be applied to other scenarios. Recently
(Henderson, Gordon, & Vijayakumar, 2017) show
that step width, medio-lateral displacement and BoS
are invariant to walking conditions and may provide
a robust metric in order to evaluate and compare
wearable robots or exoskeletons.
ACKNOWLEDGEMENTS
Partial support for the work was provided by Interreg-
Project MIND No. 151131-R4-1.
REFERENCES
Berg, K. O., Wood-Dauphinee, S. L., Williams, J. I., &
Maki, B. (1992). Measuring balance in the elderly:
validation of an instrument. Canadian journal of public
health, pp. 1073–1080. doi:ISSN 0003-9993
Eikerling, H.-J., Uelschen, M., & Lutterbeck, L. (2016).
Scalable Distributed Sensor Network for Contact-less
Gait Analysis - A Marker-less, Sensor-based System
for Steering Rehabilitation Measures. 9th International
Joint Conference on Biomedical Engineering Systems
and Technologies. Rome.
Götz-Neumann, K. (2015). Gehen verstehen (4. Auflage).
Stuttgart: Georg Thieme Verlag.
Hak, L., van Dieën, J., van der Wurff, P., & Houdijk, H.
(2014). Stepping asymmetry among individuals with
unilateral transtibial limb loss might be functional in
terms of gait stability. Physical Therapy, pp. 1480-
1488.
Hanavan, E. (1964). A mathematical model of the human
body. Air force aerospace medical research lab Wright-
Patterson AFB OH.
Henderson, G., Gordon, D., & Vijayakumar, S. (2017).
Identifying invariant gait metrics for exoskeleton
assistance. 2017 IEEE International Conference on
Robotics and Biomimetics (ROBIO). Macau.
Hof, A., Gazendam, M., & Sinke, W. (2005). The condition
for dynamic stability. Journal of Biomechanics, pp. 1-
8.
Perry, J., & Burnfield, J. (2010). Gait Analysis (2nd
edition). Thorofare: SLACK Incorporated.
Scholkmann, F., Boss, J., & Wolf, M. (2012). An Efficient
Algorithm for Automatic Peak Detection in Noisy
Periodic and Quasi-Periodic Signals. Algorithms, pp.
588-603.
Shumway-Cook, A., & Woollacott, M. (2017). Motor
Control: Translating Research Into Clinical Practice
(5th ed). Philadelphia: Wolters Kluwer.
Uelschen, M., & Eikerling, H.-J. (2015). A Mobile Sensor
System for Gait Analysis supporting the Assessment of
Rehabilitation Measures. Proceedings of the 6th ACM
Conference on Bioinformatics, Computational Biology
and Health Informatics (BCB '15) (pp. 96-105). New
York: ACM.
Van Criekinge, T., Saeys, W., Hallemans, A., Velghe, S.,
Viskens, P., Vereeck, L., . . . S., T. (2017, May). Trunk
biomechanics during hemiplegic gait after stroke: A
systematic review. Gait Posture, pp. 133-143.
doi:10.1016/j.gaitpost.2017.03.004
VICON. (2017). Plug-In Gait Reference System. Vicon
Motion Systems.
Winter, D. (2009). Biomechanics and Motor Control of
Human Movement (4th edition). Hoboken: Wiley.
Wu, M., Brown, G., & Gordon, K. (2017). Control of
locomotor stability in stabilizing and destabilizing
environments. Gait & Posture, pp. 191-196.
An Efficient Algorithm for Kinematics Estimation with Application to Dynamic Gait Stability using a Contact-less Skeleton Tracking
System
101
