
A Novel Blockchain based Platform to Support Chronic Care Model
Information Management
Luigi Lella and Sergio Piersantelli
Azienda Sanitaria Unica Regionale delle Marche, via Oberdan n.2, 60122 Ancona, Italy
Keywords: eHealth, eHealth Applications, Design and Development of Methodologies for Healthcare IT.
Abstract: Blockchain technology has been successfully used in many healthcare contexts, guaranteeing not only high
security and privacy levels in clinical data management, but also the continuous updating of patient clinical
pictures, to ensure the continuity of care and the reliability of data sources in statistical processing. These results
are related to the peculiar features of this technology such as the distributed ledger, the chaincode, the encryption
algorithms used to cypher information, the technological solutions used for block validation and the use of smart
contracts. This article aims to present a possible solution based on blockchain technology to the problem of
information management in the Chronic Care Model. The use of the blockchain makes it possible to create a
patient-centred system that not only allows patients, or authorized people, to exercise a constant control over
their health data, but it is also able to "contractualize" the agreements made in this regard together with the
collection of consent for the processing of health data. The blockchain also allows the preparation of validated
data sources for the subsequent statistical processing to update process and outcome indicators and the risk
prospects related to the care pathways activated for patients suffering from chronic pathologies.
1 INTRODUCTION
Patients involvement within the health information
system can lead to a marked improvement in individual
and social health outcomes (Kushniruk and Nøhr,
2016). These results are even more evident when
strategies are adopted to address the education of
patients in order to create a sort of partnership with
health professionals and other caregivers (Batalden et
al., 2016; Bodenheimer et al. 2002).
Designing an information system to support
healthcare activities can however be an extremely
complex activity, especially in the case of the treatment
of patients suffering from chronic pathologies that
require long and prolonged interactions with various
actors of the information system. These actors can be
not only professionals and caregivers, but also IoMT
devices that must constantly monitor vital parameters.
This is the case of the Chronic Care Model (CCM),
a model of health care for chronically ill patients
developed by Professor Wagner and his colleagues at
the McColl Institute for Healthcare Innovation, in
California (Wagner et al., 2001; Wagner et al., 1999).
The model proposes a series of changes at the level of
health systems useful in favouring the improvement of
the condition of chronic patients and suggests a
"proactive" approach between health personnel and the
patients themselves, with the latter becoming an
integral part of the care process (Coleman et al., 2009).
The CCM model is characterized by six
fundamental characteristics (Wagner et al.,1996).
Delivery System Design: the care activity is provided
with a clear subdivision of the tasks and
responsibilities between the various caregivers and
health professionals that take care of the patient,
making a clear distinction between planned assistance
(e.g.: follow up) and assistance in the acute phase
(acute care);
Self-management Support: that consists in assisting in
a collaborative way the patients and their families in
the acquisition of the necessary skills for the treated
disorders and diseases. The information system
intervenes in this phase by making available self-care
tools, references to community resources and tools for
assessing therapeutic compliance;
Decision Support: the presence of evidence based
decision support tools that can also be used by patients
to agree with their GPs the therapeutic or
pharmacological pathway to follow;
Clinical Information System: the information system
must mainly provide tools to support therapeutic
compliance, a system of indicators for the assessment
Lella, L. and Piersantelli, S.
A Novel Blockchain based Platform to Support Chronic Care Model Information Management.
DOI: 10.5220/0008869003030309
In Proceedings of the 13th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2020) - Volume 5: HEALTHINF, pages 303-309
ISBN: 978-989-758-398-8; ISSN: 2184-4305
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
303

of outcomes and care benefits and agendas for
assistance activities planning;
Community Resources: connection to territorial and
hospital resources for the training of the assisted and
for the reporting of care managers;
Health Care Organizations: connection to the
organizational structure, objectives and values of the
health system that takes care of the patient.
To date, within the CCM, adequate information
systems have not yet been defined that can support
patients in all their needs and actively involve them in
the care process. Indeed, it was noted that most of these
patients were marginalized if not even excluded from
any initiative of active involvement (Marmot et al.,
2012). These cases have led to a substantial worsening
of care outcomes and to an increase in care costs
compared to the average (Coulter et al., 2018) and to a
worsening of the quality of the assistance given to
disadvantaged patients (Mackert et al., 2016).
Difficulties have also been encountered in the
exchange of data in a secure and scalable manner
between the various system actors, in the support of
clinical communications especially in the cases of
patients living in remote areas, producing in this case
also a deterioration in efficacy and quality of care
services that should be supported by adequate
information systems (Zhang et al., 2018; Castaneda et
al., 2015; Berman and Fenaughty, 2005).
In general, the process of clinical information
retrieval is slow as health data, when not present in the
Electronic Health Record, must be recovered from
various sources, prepared in order to respect certain
schemas and sent to the recipient through appropriate
channels characterized by high levels of security and
reliability (Nourie, 2015). The process of clinical
information retrieval is also incomplete precisely
because of the extreme fragmentation of produced data
and the lack of those produced by the same patient, and
it is decontextualized because all the data are provider-
centred and not patient-centred. Furthermore health
information systems do not allow patients to know how
and by whom data is processed and do not allow to
govern access policies to them (Schoenberg, 2013).
The data are also not updated in real time (Ash et al.
2004).
In assisting patients suffering from chronicity, and
therefore also in CCM, remote patient monitoring
(RPM) is of fundamental importance, because it allows
to move some care services outside the traditional
clinical setting (typically at home care recipients). The
use of RPM can help to further reduce the cost of
assistance and improve the outcomes achieved. The
currently used tele-monitoring devices have now
become unobtrusive, user-friendly and equipped with
advanced features such as alerting and patient feedback
collection systems directly implemented at the device
level.
Currently no solutions have been defined that
allow secure management of the data in Internet of
Medical Things (IoMT) networks (Linn and Koo,
2017) and the sharing of data between authorized
devices in order to provide a complete information
framework to allow them to carry out automatic
operations safely through their actuators (Bolduc,
2017).
Finally, precisely because of the innumerable
sources of health data (most of which derive directly
from IoMT devices and the direct feedback of
patients), it is particularly difficult to bring them all
back into a single framework to generate a valuable
population level insight (Asokan and Asokan, 2015).
The blockchain technology (BC) can provide a
viable implementation solution that guarantees secure
access to health data, system scalability, privacy of
clinical data, and data collection to conduct evidence-
based studies of population medicine.
The aim of this article is to suggest a possible
solution for the implementation of a CCM support
information system which is based on the BC
technology. After a rapid examination of the main
characteristics of this technology (Section 2), the main
applications of the BC in medical and healthcare field
will be reviewed, with respect to the management and
sharing of clinical and remote control devices
information (Section 3). The architecture of CCM
support platform designed by ASUR will then be
illustrated together with a business case related to the
context of AV2 local health system of Marche Region
(Section 4).
2 BLOCKCHAIN TECHNOLOGY
MAIN FEATURES
A BC system can be considered as a distributed and
potentially incorruptible cryptographic database,
where it is possible to store sensitive and health data.
Technically it is essentially a peer-to-peer network
with an open and distributed ledger, whose updating is
based on appropriate consensus rules for the transfer of
blocks of information between entities that can be
people, organizations and devices.
BCs can be permissionless and permissioned. A
permissioned BC limits the number of actors who can
participate in the consensus validation process.
The data related to a new block contained in the
ledger spread through the peer-to-peer network as soon
HEALTHINF 2020 - 13th International Conference on Health Informatics
304

as it is possible to establish a communication between
each couple of authorized nodes. Each of the
authorized nodes, following the one that generated the
block, has the right to verify the validity of the block
and the correspondence with the network policies. If
the transaction is accepted, it is digitally signed and
stored in the distributed ledger. All rejected
transactions are entered into a temporary archive.
A register can be seen as an ordered sequence of
transactions divided into blocks. Each block can
represent a set of transactions (for example the transfer
of clinical data or information) and contains two
elements. The first is the header that includes a
timestamp and the hash code of the header of the
previous block. The second is the body that contains all
the transaction data properly encrypted.
The link that connects a header to the previous one
(starting from the first chronologically inserted that is
called “Genesis”) allows to set up the BC ensuring that
nobody can tamper the inserted data. The only way to
do this would be to control more than 51% of the nodes
before modifying the data in the distributed ledger.
This situation is attributable to the Byzantine Generals
Problem (BGP) (Melnyk et al., 2018). In these cases
the protocol to be used to manage the consent must be
Byzantine Fault Tolerant (BFT).
The distributed register can also contain smart
contracts (Szabo, 1997) that can help to regulate the
access to the data contained in the blocks and to
validate them. For example a smart contract can be
used to define privacy policies or to define appropriate
alerting rules linked to certain data-driven conditions.
3 RELATED WORK
With regard to the processing of personal and sensitive
data in the health field, there has always been a conflict
between data privacy (Pavlou, 2011) and data
accessibility that is the sharing of data between the
professionals who take charge of the patient (Culnan,
1984).
In contexts such as the CCM, professionals from
different fields and disciplines should be able to access
the contents of clinical records they need (Reti et al.,
2010). In the operative reality, interoperability between
information systems belonging to different healthcare
organizations or based on different technologies is
often not guaranteed (Detmer et al., 2008). This
problem is well known in the health field under the
name of care coordination (Klein et al., 2015).
In general, in the health sector there is a need to
implement secure and scalable systems capable of
ensuring access to data on a large scale, guaranteeing
trust and the compliance with the policies on sensitive
and personal data.
The first solutions for the management of health
data privacy and accessibility in the presence of multi-
professional teams or multiple health organizations
resort to multi-agent solutions (Isern and Moreno,
2016; Barrue et al., 2015; Wimmer, 2014). More
recently, solutions based on BC technology based on
the Electronic Health Record model have begun to be
considered. Some first implementations make use of
the distributed ledger of the BC, of a secure
management system of encryption keys and of a
characteristic system for blocks validation (Wood et
al., 2016), other solutions resort to the so-called
miners, or groups of nodes of the peer-to-network peer
that constitutes the BC, which are given the task of
validating new transactions (Azaria et al., 2016;
Ekblaw et al., 2016). Other more recent
implementations make use of BC cloud services to
ensure the secure and unalterable exchange of
information between multiple healthcare
organizations, in order to constantly update the
patient's clinical picture and to ensure continuity of
care (Xia et al., 2017). Such systems prove to be
particularly effective in contexts such as the treatment
of patients suffering from chronic disorders (e.g. HIV
and cancer). For chronic patients, permissioned BC-
based solutions have also been adopted, especially to
ensure privacy and data security (Dubovitskaya et al.,
2017). Also characteristic is the choice made by
(Benchoufi et al., 2017) to manage the patients'
informed consent through a CB to make it
unfalsifiable.
In general, however, for the management of
clinical data by multidisciplinary teams of
professionals, the tendency is currently to resort to the
Personal Health Record model where patients
themselves or their representatives are responsible for
managing the access policies to their data, monitoring
constantly their accesses and the uses made of them
(Chen et al. 2018; Yue et al., 2016; Ivan, 2016). This
choice is well suited to the CCM model, which
provides for a high level of involvement of the patient
who actively and consciously participates in the choice
of the therapeutic path.
With regard to remote monitoring systems using
IoMT devices, in recent times there has been the choice
of implementing solutions based on the BC (Griggs et
al.,2018; Wu et al., 2019).
For RPM through IoMT devices, it is generally not
recommended to use computationally heavy
algorithms such as Proof of Work (PoW) for block
validation and symmetric-type encryption algorithms
are used (Dorri et al. 2016, Dorri et al. 2017).
A Novel Blockchain based Platform to Support Chronic Care Model Information Management
305

Furthermore smart contracts for data processing are
implemented in order to identify critical situations and
to send alerts to the nodes associated with health
professionals (Griggs et al., 2018).
Overall, what emerges from the literature seems to
validate the choice of the BC for the safe and reliable
management not only of the communications between
professionals who take care of chronic diseases but
also of communications coming from or exchanging
IoMT devices (Dwivedi, 2019).
4 ASUR CCM MANAGEMENT
FRAMEWORK
A patient-centred CCM management framework
(CCMMF) will be implemented at the Area Vasta 2,
throughout the territory that revolves around the
community hospitals of Jesi, Loreto and Chiaravalle.
The CCMMF will interface with other systems
already used at regional level such as the regional
authentication system called FedCohesion, the Policy
Manager and the Regional Attribute Authority to give
the actors involved in the CCM the appropriate access
rights to the CCMMF platform. The regional reference
database for patients anagraphical data called ARCA
will be used together with the Electronic Health Record
called SIRTE and the regional catalogs containing the
updated data of the organizational structures.
The CCMMF will consist of a permissioned
blockchain (BC) based on the HyperLedger Fabric
(HLF) platform. The various nodes must first undergo
an authentication procedure before performing the
creation or validation of new blocks. The approval
(endorsement) of a set of transactions (sending
multiple clinical information) present in a new block
will follow a process characterized by various phases
(proposal, approval, ordering, validation and commit)
and will follow certain approval policies. In particular
these policies will identify which nodes must give the
endorsement for a given transaction class, while the
chaincode will guarantee that these policies have been
implemented.
Before committing, peers will execute the
chaincode to ensure that there are sufficient
endorsements and that they have been obtained from
the appropriate entities (those defined at the policy
level). In the end, a check will also be carried out on
the version of the registry before inserting the new
blocks to avoid attacks such as double spending
operations. Each transaction in a block contains its
read/write set or the set of cryptographic keys that have
been read or written at endorsement time.
The HLF framework introduces the channel
element. In HLF the channels are the first level of
segregation and information confinement. A ledger is
logically associated with a channel (a register itself
replicated as many times as there are peers associated
with that channel). Therefore peers that do not
participate in a channel do not have visibility on the
data written in it.
For a more accurate management of access within
a channel it is possible to define ACLs (Access Control
Lists). Access policies are written in blocks but on a
separate channel from the application data. Writing
within a channel the authorization logics there remains
an indelible auditable trace over time of all the
definitions made and all their modifications.
In this way it is possible to solve the problem of
managing access policies in a lightweight and scalable
manner, complying with the current provisions of the
GDPR (General Data Protection Regulation, 2016). By
accessing the channel dedicated to data access policies
produced by the peer-to-peer network, the patient, or a
person in charge thereof, can modify these policies at
any time, guaranteeing the traceability of accesses, the
data obscuration as well as the obscuration of
obscuration. In other words, not only unauthorized
nodes will not be able to access the contents of a file,
but they will also ignore their existence. It will also be
possible to recover all the health information produced
by the peer-to-peer network by going back along the
chaincodes associated with the various channels,
storing them in an exportable format and it will also be
possible to process all the information made available
by the client for statistical purposes.
The chaincode, at the time of accessing the data,
will perform a check on the authorization criteria
currently available and will apply them in response to
a request for a node. For the encryption of clinical data,
symmetric algorithms will be used to facilitate
transactions with and between IoMT device nodes.
In the CCMMF solution implemented by the
ASUR, smart contracts will also be used for the
purpose of processing data, and implementing alerting
systems in order to proactively alert caregivers and all
professionals who have taken care of the client of
important changes in the relative clinical picture.
The activities of the professionals operating within
the CCM will be managed through a workflow
management system (WMS). Thanks to this WMS
through an app that can be installed on the smartphone,
the assisted and its caregivers will have a complete
picture of the care path to follow and will receive alerts
on scheduled events (such as taking a drug, carrying
out an outpatient visit or of a therapeutic treatment) or
on critical events to be managed promptly by following
HEALTHINF 2020 - 13th International Conference on Health Informatics
306
the appropriate guidelines prepared by the
multidisciplinary team that took care of the client.
The CCMMF will initially be tested on care
pathways aimed at patients suffering from chronic
cardiovascular diseases and will provide real-time
monitoring of some vital parameters of the patient
(heart rate, blood pressure, ECG) using IoMT devices.
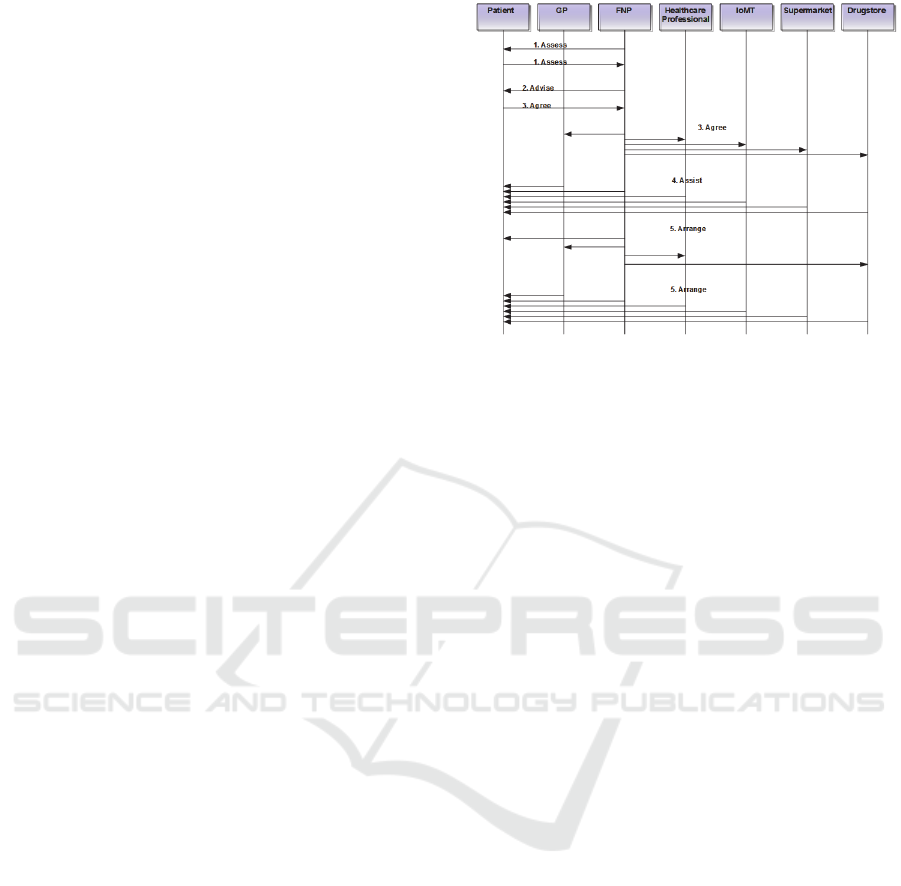
The figure shows a typical scenario relating to the
CCM. The main actors are the cardiac patient, the
general practitioner (GP), the family nurse
practictioner (FNP), the local professional (dietitian,
nutritionist, social worker, geriatrician, physiatrist,
wellness coach etc.), the drugstore (which can also
provide services in addition to the administration of
drugs, counselling services or registration of
parameters such as weight, body mass index, pressure
etc.), IoMT monitoring devices wearable by the
patients and any affiliated shops where patients can
purchase food monitoring the ingredients and
quantities purchased to check if the purchased product
is in line with the diet that patients must respect.
All these actors can create blocks or access blocks
belonging to their own channel, in compliance with the
access policies to the data established by the patient.
To ensure that the CCM is effectively applied, the
workflow of the entire care process must follow the so-
called ‘5As’ model (Glasgow et al., 2006). Following
the recruitment of the assisted by the GP, the path
followed by the CCM is started. The first phase
(1.assess) consists in the recovery, through
appropriate questionnaires, of the knowledge of the
patients about their chronicity, of their behavioural
habits and of their expectations of improvement. This
phase mainly involves the patient and the FNP who
administers the questionnaires. In the second phase (2.
advise) the FNP helps the client to understand what are
the possible therapeutic and pharmacological pathways
that can be followed. The ultimate aim is to allow the
patient to make an informed choice of the care pathway
registering it in the third phase (3.agree) within a
specific smart contract. This will allow the entire
assistance system to safeguard itself also from the legal
point of view. In the smart contract, the consent will
also be recorded in relation to the data processed in the
various channels activated, released in an informed
manner by the user.
In the fourth phase (4.assist) assistance is provided
following the pathway agreed with the patient. The
vital parameters of patient are also monitored in order
to
verify whether the chosen care pathway is giving
rise to objectively verifiable improvements. In this
patient-centred record patients can incorporate patient-
reported experience measures (PREM) and patient-re-
ported outcome measures (PROM) in addition to data
Figure 1: CCMMF communication diagram.
provided by wearable monitoring devices [16].
In the fifth phase (5.arrange) the FNP, in
agreement with the multidisciplinary team (GP,
dietician, nutritionist, social worker, geriatrician,
physiatrist, wellness coach etc.) who takes care of the
client, decides the modalities in which to conduct any
follow-up activities.
The main actors presented in the communication
diagram of Figure 1 will interface to an Enterprise
Service Bus which has the task of managing
communications between the healthcare IT platforms
used in the regional context and the main IT systems
that make up the backbone of the platform to be
realized.
The system components are shown in figure 2. The
circles represent the interfaces used by the system
actors. The professionals who take charge of the care
recipient have been divided into two groups consisting
of regional health personnel (who authenticate
themselves through the FedCohesion regional
authentication system) and non-healthcare personnel
operating in the regional territory (physiatrist, social
worker, dietician, nutritionist, wellness coach etc.) that
uses another strong authentication system included in
the interface.
The interfaces used by the main actors (with the
exception of the IoMT devices) have an adequate GUI
that guarantees adequate levels of usability /
accessibility considering the relative user categories.
The blockchain is implemented using the open
source framework HLF, which also allows the channel
mechanism to be implemented.
For the management of consent data, a special channel
must be used within the network that constitutes the
blockchain. A node must be created and managed
for each of the types of actors involved in the business
process of Figure 1.
A Novel Blockchain based Platform to Support Chronic Care Model Information Management
307
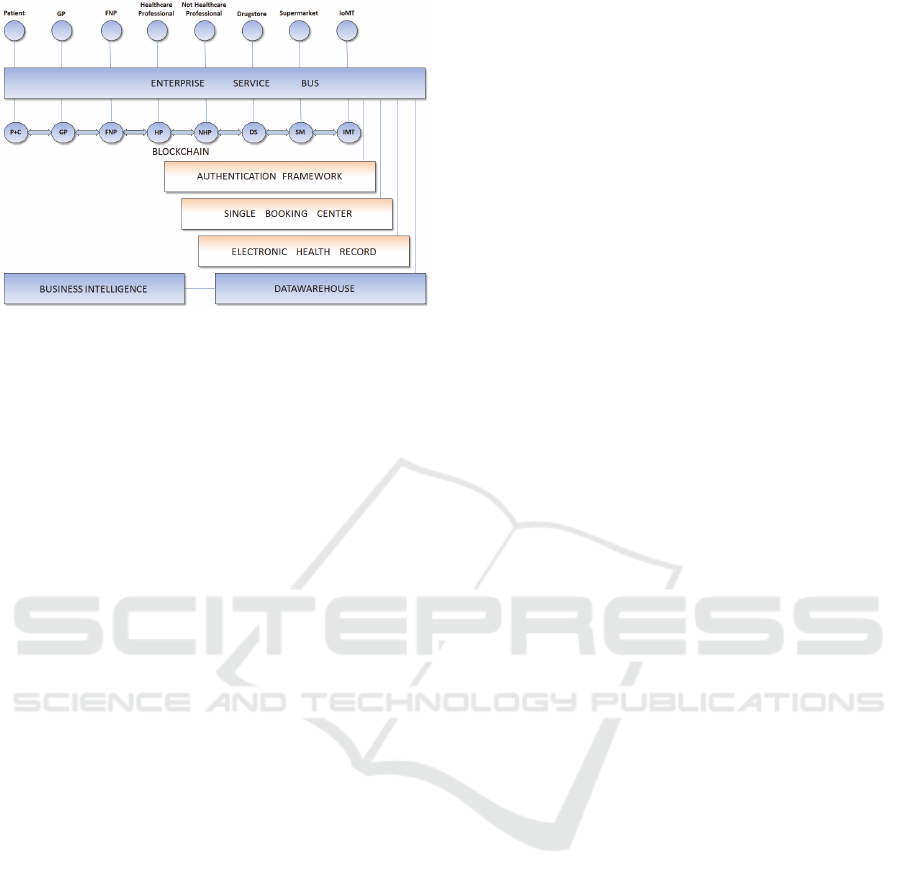
Figure 2: CCMMF architecture.
At the end of the route, all the sensitive and health
data produced must be recovered using the chaincode
associated with the route, in order to ensure its
completeness and validation.
5 CONCLUSIONS
After a brief summary of the BC technology features
and an examination of the main implementation
solutions relating to the IT support systems for care
activities aimed at patients suffering from diseases and
chronic disorders, a possible computerization solution
of the CCM based on BC technology was presented.
This platform will be used on an experimental level
for a year in a restricted territorial reality of the Marche
Region, and if it will present concrete and encouraging
levels of results it will soon be extended to the whole
regional territorial reality.
The outcome measures collected at the end of the
trial period will be used to evaluate the effectiveness of
the technological solution chosen to support the care
activities related to the CCM.
REFERENCES
Ash, J.S., Berg, M., Coiera, E.: Some unintended
consequences of information technology in health care:
the nature of patient care information system-related
errors, Journal of the American Medical Informatics
Association,, 11, (2), pp. 104-112 (2004).
Asokan GV, Asokan V.: Leveraging “big data” to enhance
the effectiveness of “one health” in an era of health
informatics. J Epidemiol Glob Health 2015
Dec;5(4):311-314 (2015).
Azaria, A., Ekblaw, A., Vieira, T., Lippman, A.: Medrec:
Using blockchain for medical data access and permission
management. In Open and Big Data (OBD), International
Conference on, pages 25–30. IEEE (2016).
Barrue, C., Cortes, A., Moreno, J., Cortes, U. Using
multiagent systems to mediate in an assistive social
network for elder population. In Artificial Intelligence
Research and Development: Proceedings of the 18th
International Conference of the Catalan Association for
Artificial Intelligence, volume 277, page 120. IOS Press.
(2015).
Batalden, M., Batalden, P., Margolis, P., Seid, M.,
Armstrong, G., Opipari-Arrigan, L., Hartung, H.:
Coproduction of healthcare service. BMJ Qual. Saf., 25,
509–517 (2016).
Benchoufi, M., Porcher, R., Ravaud, P.: Blockchain
protocols in clinical trials: Transparency and traceability
of consent. F1000Research 2017, 6, 66 (2017).
Berman, M., Fenaughty, A.: Technology and managed care:
Patient benefits of telemedicine in a rural health care
network. Health Econ., 14, 559–573 (2005).
Bodenheimer, T., Lorig K, Holman H, Grumbach K.: Patient
self-management of chronic disease in primary care.
JAMA: the journal of the American Medical Association.
,288:2469–2475 (2002).
Bolduc, M., The future of medical wearables, available
online: https://www.mpo-mag.com/issues/2017-06-
01/view_columns/the-future-of-medical-wearables 2017
, accessed on 13th Jun 2019 (2017)
Castaneda, C., Nalley, K., Mannion, C., Bhattacharyya, P.,
Blake, P., Pecora, A., Goy, A., Suh, K.S.: Clinical
decision support systems for improving diagnostic
accuracy and achieving precision medicine. J. Clin.
Bioinform., 5, 4 (2015).
Chen, Y., Ding, S., Xu, Z., Zheng, H., Yang, S.: Blockchain-
Based Medical Records Secure Storage and Medical
Service Framework. J. Med. Syst., 43, 5 (2018).
Coleman K., Austin B.T., Brach C., Wagner E.H.: Evidence
on the chronic care model in the new millennium, Health
Aff. 28 (1) (2009).
Coulter, A., Parsons, S., Askham, J.: World Health
Organization. Regional Office for Europe, European
Observatory on Health Systems and Policies. Where Are
the Patients in Decision-Making about Their Own care?.
available online: www.who.int/management/
general/decisionmaking/WhereArePatientsinDecisionM
aking.pdf, accessed on 10th September 2018 (2018).
Culnan, M. J.: The dimensions of accessibility to online
information: Implications for implementing office
information systems. ACM Transactions on Information
Systems (TOIS), 2(2):141–150 (1984).
Detmer, D., Bloomrosen, M., Raymond, B., Tang, P.:
Integrated Personal Health Records: Transformative
Tools for Consumer-Centred Care. BMC Medical
Informatics and Decision Making, 8(1) (2008).
Dorri, A., Kanhere, S.S., Jurdak, R.: Blockchain in internet
of things: Challenges and solutions., arXiv:1608.05187
(2016).
Dorri, A., Kanhere, S.S., Jurdak, R., Gauravaram, P.:
Blockchain for IoT security and privacy: The case study
of a smart home. In Proceedings of the IEEE
International Conference on Pervasive Computing and
HEALTHINF 2020 - 13th International Conference on Health Informatics
308

Communications Workshops (PerCom 2017), Kona, HI,
USA, 13–17, 618–623 (2017).
Dubovitskaya, A., Xu, Z., Ryu, S., Schumacher, M., Wang,
F.: Secure and trustable electronic medical records
sharing using blockchain. In AMIA Annual Symposium
Proceedings; American Medical Informatics
Association: Washington, DC, USA, 2017; Volume
2017, p. 650 (2017).
Dwivedi, A.D., Srivastava, G., Dhar, S., Singh, R.: A
Decentralized Privacy-Preserving Healthcare
Blockchain for IoT. Sensors,19, 326 (2019).
Ekblaw, A., Azaria, A., Halamka, J. D., Lippman, A.: A case
study for blockchain in healthcare:“medrec” prototype
for electronic health records and medical research data.
In: Proceedings of IEEE Open & Big Data Conference,
Vol. 13, p. 13 (2016).
General Data Protection Regulation, available online:
https://gdpr-info.eu/, accessed on 13th Jun 2019 (2016).
Glasgow R.E., Emont S., Miller D.C.: Assessing delivery of
the five ‘As’ for patient-centered counseling, Health
Promotion International, Volume 21, Issue 3, 245–255,
available online: https://doi.org/10.1093/
heapro/dal017, accessed on 13th Jun 2019 (2006)
Griggs, K.N., Ossipova, O., Kohlios, C.P., Baccarini, A.N.,
Howson, E.A., Hayajneh, T.: Healthcare Blockchain
System Using Smart Contracts for Secure Automated
Remote Patient Monitoring. J. Med. Syst., 42, 130
(2018).
Isern, D. and Moreno, A.: A systematic literature review of
agents applied in healthcare. Journal of medical systems,
40(2):43 (2016).
Ivan, D.: Moving toward a blockchain-based method for the
secure storage of patient records. In ONC/NIST Use of
Blockchain for Healthcare and Research Workshop;
ONC/NIST: Gaithersburg, MD, USA, (2016).
Klein, D. M., Fix, G. M., Hogan, T. P., Simon, S. R., Nazi,
K. M., Turvey, C. L.: Use of the Blue Button Online Tool
for Sharing Health Information: Qualitative Interviews
With Patients and Providers. Journal of Medical Internet
Research, 17(8):e199 (2015).
Kushniruk, A., Nøhr, C.: Participatory Design, User
Involvement and Health IT Evaluation. Stud. Health
Technol. Inform, 222, 139–151 (2016).
Linn, L.A., Koo, M.B.: Blockchain For Health Data and Its
Potential Use in Health IT and Health Care, available
online: https://www.healthit.gov/sites/ default/files/11-
74-ablockchainforhealthcare.pdf , accessed on 24th Nov
2017 (2017).
Mackert, M., Mabry-Flynn, A., Champlin, S., Donovan, E.E.,
Pounders, K.: Health Literacy and Health Information
Technology Adoption: The Potential for a New Digital
Divide. J. Med. Internet Res., 18, e264 (2016).
Marmot, M., Allen, J., Bell, R., Bloomer, E., Goldblatt, P.:
WHO European review of social determinants of health
and the health divide. Lancet, 380, 1011–1029 (2012).
Melnyk, D., Wang, Y., Wattenhofer, R.: Byzantine
preferential voting, arXiv:1803.02720 (2018).
Nourie, C.E. (Ed.). (2015, February). Your Medical Records,
available online:, from http://m.kidshealth.
org/en/teens/medical-records.html, accessed on March
01, 2018 (2015).
Pavlou, P. A.: State of the information privacy literature:
where are we now and where should we go? MIS
Quarterly, 35(4):977–988 (2011).
Reti, S. R., Feldman, H. J., Ross, S. E., Safran, C.: Improving
personal health records for patient-centered care. Journal
of the American Medical Informatics Association,
17(2):192–195 (2010).
Schoenberg, R.: Bridged patient/provider centred method
and system, in Editor (Ed.)^(Eds.): ‘Book Bridged
patient/provider centred method and system’ (Google
Patents, 2013, edn.) (2013).
Szabo, N.: Formalizing and Securing Relationships on Public
Networks. First Monday, [S.l.], sep. 1997. ISSN
13960466. available at: <https://firstmonday.
org/ojs/index.php/fm/ article/view/548/469>. Accessed
on Jun. 2019 (1997).
Wagner, E., Austin, B., Von Korff, M.: Organizing care for
patients with chronic illness. Millbank Q. (74):511-544
(1996).
Wagner, E.H., Davis C., Schaefer J., Von Korff M., Austin
B.: A Survey of Leading Chronic Disease Management
Programs:Are They Consistent with the Literature?
Managed Care Quarterly7(3): 56-66 (1999).
Wagner, E.H., Glasgow R., Davis C., Bonomi A., Provost L.,
McCulloch D., Carver P., Sixta C.: Quality Improvement
inChronic Illness Care: A Collaborative Approach,
Journal on QualityImprovement 27(2): 63-80 (2001).
Wimmer, H. A multi-agent system for healthcare data
privacy. In AMCIS (2014).
Wood, C., Winton, B., Carter, K., Benkert, S., Dodd, L., and
Bradley, J.: How blockchain technology can enhance
EHR operability. Available online:
https://www.hyperledger.org/wp-
content/uploads/2016/10/ARKInvest_and_GEM_
Blockchain_EHR_Final.pdf. Accessed on 13th Jun 2019
(2016).
Wu, L., Du, X., Wang, W., Lin, B.: An out-of-band
authentication scheme for internet of things using
blockchain technology, IEEE Access, vol.7, 58381-
58393 (2019).
Xia, Q.; Sifah, E.B.; Asamoah, K.O.; Gao, J.; Du, X.;
Guizani, M.: MeDShare: Trust-less medical data sharing
among cloud service providers via blockchain. IEEE
Access, 5, 14757–14767 (2017).
Yue, X., Wang, H., Jin, D., Li, M., Jiang, W.: Healthcare data
gateways: Found healthcare intelligence on Blockchain
with novel privacy risk control. J. Med. Syst., 40, 218
(2016).
Zhang, P., White, J., Schmidt, D.C., Lenz, G., Rosenbloom,
S.T.: Fhirchain: Applying blockchain to securely and
scalably share clinical data. Comput. Struct. Biotechnol.
J., 16, 267–278 (2018).
A Novel Blockchain based Platform to Support Chronic Care Model Information Management
309
