
Description of Methicillin-resistant Staphylococcus aureus Infection at
Arifin Achmad General Hospital, Riau Province from 2015-2019
Dewi Anggraini
1,2
a
, Dewi Santosaningsih
3
b
, Kuntaman
4
c
, Muhammad Ihsan
5
d
and Syifa Farhani Ridha
6
e
1
Department of Microbiology, Faculty of Medicine, Universitas Riau, Pekanbaru, Indonesia
2
Doctoral Program, Faculty of Medicine, Universitas Airlangga, Surabaya, Indonesia
3
Department of Clinical Microbiology,
Faculty of Medicine, Universitas Brawijaya/Dr. Saiful Anwar Hospital, Indonesia
4
Department of Clinical Microbiology,
Faculty of Medicine, Universitas Airlangga/Dr.Soetomo Hospital, Indonesia
5
Department of Surgery,
Faculty of Medicine, Universitas Riau, Pekanbaru, Indonesia
6
Medical Education Program, Faculty of Medicine, Universitas Riau, Pekanbaru, Indonesia
Keywords: MRSA, Hospital, Staphylococcus aureus
Abstract: Methicillin-Resistant Staphylococcus aureus (MRSA) is one of the most important pathogen causing hospital-
associated infections worldwide. This study aimed to determine the prevalence of MRSA infections at Arifin
Achmad General Hospital, Riau Province, Indonesia. This study was a retrospective study using MRSA
infected patients' medical record data in Arifin Achmad General Hospital during 2015-2019. There were 600
isolates of Staphylococcus aureus enrolled in this study. Of this, the prevalence of MRSA ranged between
23.8% and 42.7%. The highest prevalence of MRSA infections was found in the surgical ward (44.8%). The
MRSA isolates were mostly found among pus specimens (66.5%) and obtained from patients with skin, and
soft tissue infections.. vancomycin, tigecycline, and linezolid were highly susceptible to the MRSA isolates.
The MRSA infections were frequently found among male patients (51.2%), 46-55 years old (27.9%), length
of stay 7-13 days (26.7%), onset more than two days (54.7%), no history of surgery (51.2%), and not referred
patients (81.4%). In conclusion, the prevalence of MRSA at Arifin Achmad General Hospital was relatively
high. A further hospital surveillance system should be set up to monitor this.
1 INTRODUCTION
Staphylococcus aureus (S. aureus) is a skin flora in
humans. However, it is an important pathogen,
particularly among susceptible hosts (Erikawati et al.,
2016). These bacteria are the most common cause of
pyogenic infections of the skin and soft tissues
(Kliegman et al., 2016). Methicillin-resistant
Staphylococcus aureus (MRSA) is a specific strain of
S. aureus with resistance to almost all β-lactam
antibiotics such as penicillin, methicillin, and
cephalosporin (Gayatri et al., 2015). MRSA is
resistant to β-lactam due to a change of penicillin-
binding protein (PBP2) to PBP2a, which has a low
a
https://orcid.org/0000-0001-7507-2445
b
https://orcid.org/0000-0002-0156-6976
c
https://orcid.org/0000-0003-4897-8879
d
https://orcid.org/0000-0003-2883-3541
e
https://orcid.org/0000-0003-3196-3865
affinity for β-lactam (Conly, 2018). The emergence
of MRSA has become a significant problem because
of the limited antibiotic therapy of MRSA infections.
Since MRSA was first discovered in the 1960s
(Wong et al., 2018), the prevalence of MRSA
infections has increased (Negara, 2016).
Little is
known regarding the epidemiology of MRSA
infections in Indonesia, especially in Riau. MRSA
infection features must be investigated continuously
because of changes in the prevalence and patterns of
antibiotic resistance. This study aimed to determine
the epidemiology of MRSA infections at Arifin
Achmad General Hospital, Riau Province, during
2015-2019.
184
Anggraini, D., Santosaningsih, D., Kuntaman, ., Ihsan, M. and Ridha, S.
Description of Methicillin-resistant Staphylococcus aureus Infection at Arifin Achmad General Hospital, Riau Province from 2015-2019.
DOI: 10.5220/0010489801840189
In Proceedings of the 1st Jenderal Soedirman International Medical Conference in conjunction with the 5th Annual Scientific Meeting (Temilnas) Consortium of Biomedical Science Indonesia
(JIMC 2020), pages 184-189
ISBN: 978-989-758-499-2
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
2 MATERIALS AND METHODS
A retrospective study was conducted at Arifin
Achmad General Hospital, Riau Province, Indonesia,
during April-June 2020. The MRSA isolates were
obtained by clinically indicated culture in the
Microbiology Laboratory of Arifin Achmad General
Hospital from 2015-2019. The Vitek 2 system carried
out confirmation of identification and antibiotic
susceptibility test. Antibiotics tested included
clindamycin, erythromycin, tigecycline, vancomycin,
linezolid, amoxicillin, amoxicillin/clavulanic acid,
piperacillin/tazobactam, ampicillin/sulbactam,
cefazolin, ceftriaxone, ceftazidime, cefepime,
cefoxitin, ertapenem, meropenem, gentamicin,
ciprofloxacin, trimethoprim/sulfamethoxazole, and
rifampicin.
The patient's clinical data were collected from the
medical record data and analyzed using the SPSS
statistical software version 23.
3 RESULTS
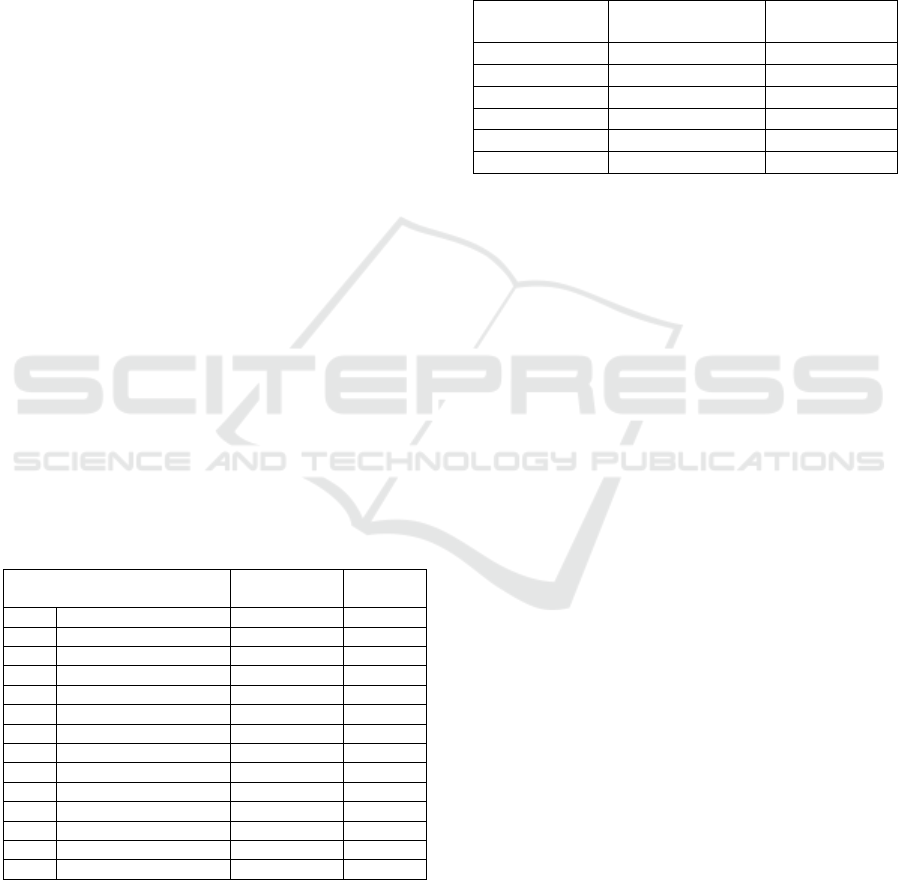
3.1 Prevalence of MRSA Infections
Overall, 600 samples of S. aureus were collected, 197
of MRSA (32.8%). The highest MRSA prevalence
was found in 2019 (42.7%), while the lowest was
2016 (23.8%). The highest prevalence was in the
surgical ward (43.8%).
Table 1: MRSA prevalence at Arifin Achmad General
Hospital, Riau Province 2015-2019.
Variable
MRSA
(n=197)
S. aureus
(n=600)
Period 2015 16 (30,2%) 53
2016 24 (23,8%) 101
2017 45 (32,8%) 137
2018 48 (30,2%) 159
2019 64 (42,7%) 150
Total 197 (32,8%) 600
Ward Intensive Care Uni
t
21 (30,0%) 70
Neonatal Care Uni
t
2 (11,1%) 18
Surgical Ward 57 (43,8%) 130
Medical Ward 62 (32,3%) 192
Mix Ward 18 (24,3%) 74
Fetomaternal Ward 3 (30,0%) 10
Outpatient clinic 31 (33,3%) 93
Emergency Uni
t
3 (23,1%) 13
3.2 Distribution of MRSA based on
Source of Specimen
MRSA was mostly found in pus and sputum (66.6%
and 19.3%, respectively). Only three MRSA isolates
were found in tissue and urine each (1.5%).
Table 2: Distribution of MRSA isolates based on the type
of specimens at Arifin Achmad General Hospital, Riau
Province 2015-2019.
Specimen Frequency
(N=197)
Percentage (%)
Pus 131 66,5
Tissue 3 1,5
Bloo
d
13 6,6
Sputum 38 19,3
Urine 3 1,5
Othe
r
9 4,6
3.3 Diagnosis and Characteristics
based on MRSA Patients
Based on 197 culture results identified as MRSA,
there were 86 medical records that could be accessed
in this study. MRSA cases were mostly found in
patients with skin and soft tissue disorders (59%),
followed by lung disorders (16%). The frequency of
MRSA was higher in men (51.2%) than in women
(48.8%). MRSA was mostly found in patients with
46-55 years (27.9%), and the least was 12-16 years
old (1.2%). MRSA infections were common in
patients with a treatment duration of 7-13 days
(26.7%) with an onset of more than 2 days (54.7%).
MRSA patients mostly did not have a history of
surgery (51.2%) and were not transferred from other
healthcare facilities (81.4%).
3.4 Antimicrobial Sensitivity Pattern
The antibiotics that have the highest sensitivity were
tigecycline, vancomycin, and linezolid (100%). All
isolates were resistant to amoxicillin,
amoxicillin/clavulanic acid, piperacillin/tazobactam,
ampicillin/sulbactam, cefazolin, ceftriaxone,
ceftazidime, cefepime, cefoxitin, ertapenem, and
meropenem.
Description of Methicillin-resistant Staphylococcus aureus Infection at Arifin Achmad General Hospital, Riau Province from 2015-2019
185
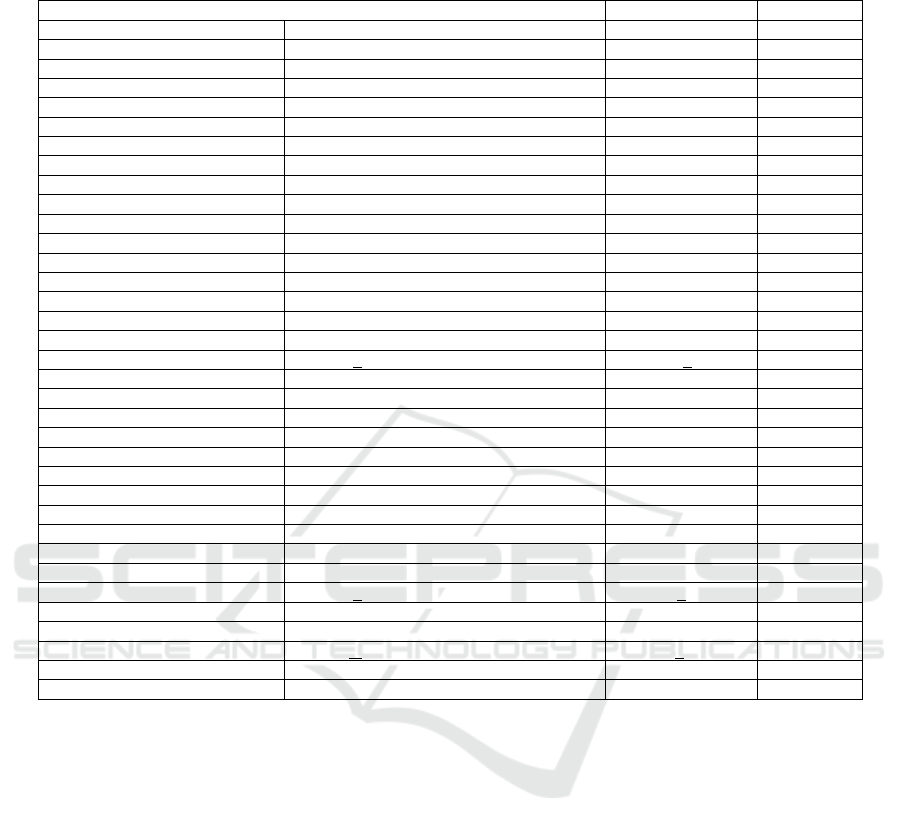
Table 3: Diagnosis and Characteristics of MRSA patients at Arifin Achmad General Hospital, Riau province in the period
2015-2019.
Varia
b
le Frequency (N= 86) Percentage (%)
Diagnosis Skin and Sof
t
-Tissue 51 59,3
Heart and bloodstream 3 3,5
Lungs 14 16,3
Bone and join
t
11 12,8
Nervous system 3 3,5
Other 4 4,7
Gende
r
Male 44 51,2
Female 42 48,8
Age 0
–
5 8 9,3
6
–
11 3 3,5
12
–
16 1 1,2
17
–
25 8 9,3
26
–
35 9 10,5
36
–
45 17 19,8
46
–
55 24 27,9
56
–
65 12 14
> 65 4 4,7
Mean + SD 39,7 + 19
Length of Stay <1 day 17 19,8
1
–
6 days 15 17,4
7
–
13 days 23 26,7
14 -20 days 7 8,1
21
–
27 days 8 9,3
28
–
34 days 5 5,8
35
–
41 days 1 1,2
42
–
48 days 2 2,3
49
–
55 days 2 2,3
56
–
62 days 1 1,2
>62 days 5 5,8
Mean + SD 17,7 + 26,7
Onse
t
0
–
2 days 39 45,3
>2 days 47 54,7
Mean+ SD 7,8 + 14,9
History of Surgery 42 48,8
Transferred from another hospital 16 18,6
4 DISCUSSION
The mean prevalence of MRSA at Arifin Achmad
General Hospital from 2015-2019 was 32.8%.
Research conducted at Dr. Saiful General Hospital
Anwar obtained an MRSA prevalence of 38.2%
(Erikawati et al., 2016). The study conducted at 427
centers in 45 countries found an MRSA prevalence
of 40.3% (Diekema et al., 2019). Arifin Achmad
General Hospital has made efforts to reduce MRSA
infections, including handwashing education,
isolating patients, using personal protective
equipment, disinfection of equipment and rooms, and
using antibiotics according to culture results. The
variation in prevalence found at Arifin Achmad
General Hospital is probably due to the absence of
screening in the patient, so it is difficult to identify
whether the infection source came from the Arifin
Achmad General Hospital or from outside the
hospital.
The highest MRSA prevalence in this study was
found in the surgical ward (44.8%). A study
conducted at the Port-of-Spain General Hospital
showed that MRSA's prevalence in the surgical ward
was 39.4% (Ramdass et al., 2018). Research
conducted at Dr. Soetomo Hospital, Surabaya, in
2018 found that the highest prevalence of MRSA
carriers was found in surgical wards (Kuntaman et
al., 2016). MRSA contamination in surgical wards is
more significant than in medical wards (Nkuwi et al.,
2018), which results in a greater risk of infection.
MRSA infections are common in skin and soft
tissue disorders. S. aureus is a typical skin floral that
can cause a skin infection when the skin barrier is
damaged, which can produce pus (Erikawati et al.,
2016).
This also causes pus to be the most common
specimens of isolated MRSA, as the results of
JIMC 2020 - 1’s t Jenderal Soedirman International Medical Conference (JIMC) in conjunction with the Annual Scientific Meeting
(Temilnas) Consortium of Biomedical Science Indonesia (KIBI )
186

Figure 1: MRSA antimicrobial sensitivity patterns in the Arifin Achmad General Hospital, Riau province in the period of
2015-2019.
previous studies (Erikawati et al., 2016; Garoy et al.,
2019).
This study found that MRSA infections at Arifin
Achmad General Hospital were more common in
men. This study's results are the same as in previous
studies (Garoy et al., 2019; Nuryah et al., 2019; Sit et
al., 2017). Gender is not associated with MRSA
infection (Garoy et al., 2019),
but men are more
susceptible due to less adherence to hygiene behavior
than women (Humphrey et al., 2015).
The 46-55 year age group is the most common
group infected by MRSA. This result is because this
age group is at a productive age, where they do much
physical activity. There is a greater risk of injury,
making it easier for bacteria to enter the body (Nuryah
et al., 2019).
Most patients are hospitalized from 7-13 days.
Patients with a treatment duration of 7-13 days had a
2.7 times greater risk of becoming infected with
MRSA than those with 1-6 days of stay, and this risk
will increase along with the increasing length of stay
(Loke et al., 2015).
Most MRSA infections were found with the onset
of more than 2 days. This result is consistent with
Diekema's research in 2019 in which MRSA
infections were more common in nosocomial isolates
(Diekema et al., 2019).
In this study, it was found that more patients with
MRSA infection at Arifin Achmad General Hospital
were found without a history of surgery. Previous
studies have found MRSA is common in patients with
a history of surgery (Abidin et al., 2020; Alrabiah et
al., 2016) and concluded that a history of surgery is a
risk factor for MRSA infection (Graffunder and
Venezia, 2002).
MRSA infection occurring soon after
surgery is usually rare. MRSA infection after surgery
can usually be surgical site infection (SSI) or
bacteremia. Emergency surgery, contaminated
surgery, decreased immunity, and the presence of
comorbid in a patient can increase the risk of MRSA
infection (Gurusamy et al., 2013).
In this study, MRSA infections at Arifin Achmad
General Hospital were less common in referral
patients. An increase in MRSA infections in one
hospital can accelerate the transmission among
hospitals. In other words, it increases infection in
other hospitals, depending on the relationship among
the hospitals (Lee et al., 2011).
The antibiotics with the best sensitivity for MRSA
at Arifin Achmad General Hospital are tigecycline,
vancomycin, and linezolid. These antibiotics are an
option in empiric therapy for MRSA (VanEperen and
Segreti, 2016).
0,00,00,00,00,0000000
58
30,2
100
74,6
62,2
64,3
100
100
31,3
71,6
0,0
20,0
40,0
60,0
80,0
100,0
120,0
Amoxicillin
Amoxicillin/ClavulanicAcid
Ampicillin/Sulbactam
Piperacillin/Tazobactam
Cefazolin
Ceftriaxone
Ceftazidime
Cefepime
Cefoxitin
Ertapenem
Meropenem
Gentamicin
Ciprofloxacin
Tigecycline
Trimethoprim/Sulfamethoxazole
Clindamycin
Erythromycin
Vancomycin
Linezolid
Levofloxacin
Rifampicin
Description of Methicillin-resistant Staphylococcus aureus Infection at Arifin Achmad General Hospital, Riau Province from 2015-2019
187

5 CONCLUSION
The prevalence of MRSA at Arifin Achmad General
Hospital from 2015-2019 was quite high and varied
due to the difficulty of detecting the source of
infection. The highest prevalence of MRSA was
found in the surgical ward, with the most specimen
source was pus. MRSA infection was mostly found in
male patients aged 46-55 years, with an onset of more
than 2 days, have no history of surgery, and were not
referred from other hospitals. The antibiotics with the
best sensitivity for MRSA at Arifin Achmad General
Hospital are tigecycline, vancomycin, and linezolid,
which are recommendations for MRSA empirical
therapy.
6 ETHICAL STATEMENT
Ethical approval was obtained from the Ethics Unit
for Medical and Health Research Ethics, Faculty of
Medicine, University of Riau Number:
B/021/UN.19.5.1.1.8/UEPKK/2020.
REFERENCES
Abidin, N.Z.B.Z., Voon, L.C., Yu, W.Z., Zakaria, M.,
Lim, M. and Rosli, N.K., 2020. MRSA Infection in
General Surgical Wards in a Malaysian Tertiary
Hospital: A Retrospective Study. Ann Clin Surg. 2020;
1 (2), 1008.
Alrabiah, K., Al Alola, S., Al Banyan, E., Al Shaalan, M.
and Al Johani, S., 2016. Characteristics and risk factors
of hospital acquired–methicillin-resistant
Staphylococcus aureus (HA-MRSA) infection of
pediatric patients in a tertiary care hospital in Riyadh,
Saudi Arabia. International journal of pediatrics and
adolescent medicine, 3(2), pp.71-77.
Conly, J.M. 2018. Methicillin-Resistant Staphylococcus
Aureus (MRSA). In: Conn's Current Therapy. Elsevier;
pp. 579–585.
Diekema, D.J., Pfaller, M.A., Shortridge, D., Zervos, M.
and Jones, R.N., 2019, March. Twenty-year trends in
antimicrobial susceptibilities among Staphylococcus
aureus from the SENTRY antimicrobial surveillance
program. In Open forum infectious diseases (Vol. 6,
No. Supplement_1, pp. S47-S53). US: Oxford
University Press.
Erikawati, D., Santosaningsih, D. and Santoso, S., 2016.
Tingginya prevalensi MRSA pada isolat klinik periode
2010-2014 di RSUD Dr. Saiful Anwar Malang,
Indonesia. Jurnal Kedokteran Brawijaya, 29(2),
pp.149-156.
Garoy, E.Y., Gebreab, Y.B., Achila, O.O., Tekeste, D.G.,
Kesete, R., Ghirmay, R., Kiflay, R. and Tesfu, T., 2019.
Methicillin-resistant Staphylococcus aureus (MRSA):
prevalence and antimicrobial sensitivity pattern among
patients—a multicenter study in Asmara, Eritrea.
Canadian Journal of Infectious Diseases and Medical
Microbiology, 2019.
Gayatri, A.A.Y., Utama, S., Somia, A.S.A. and Merati,
T.P., 2015. MRSA infection in patients hospitalized at
Sanglah hospital: a case series. Acta Medica
Indonesiana, 47(1).
Graffunder, E.M. and Venezia, R.A., 2002. Risk factors
associated with nosocomial methicillin-resistant
Staphylococcus aureus (MRSA) infection including
previous use of antimicrobials. Journal of
Antimicrobial chemotherapy, 49(6), pp.999-1005.
Gurusamy, K.S., Koti, R., Toon, C.D., Wilson, P. and
Davidson, B.R., 2013. Antibiotic therapy for the
treatment of methicillin-resistant Staphylococcus
aureus (MRSA) infections in surgical wounds.
Cochrane Database of Systematic Reviews, (8).
Humphreys, H., Fitzpatick, F. and Harvey, B.J., 2015.
Gender differences in rates of carriage and bloodstream
infection caused by methicillin-resistant
Staphylococcus aureus: are they real, do they matter
and why?. Clinical Infectious Diseases, 61(11),
pp.1708-1714.
Kliegman, R.M., Behrman, R.E., Jenson, H.B. and Stanton,
B.M., 2016. Nelson textbook of pediatrics. Edition 20.
Elsevier Health Sciences, pp.1429-1435
Kuntaman, K., Hadi, U., Setiawan, F., Koendori, E.B.,
Rusli, M., Santosaningsih, D., Severin, J. and
Verbrugh, H.A., 2016. Prevalence of methicillin
resistant Staphylococcus aureus from nose and throat of
patients on admission to medical wards of DR Soetomo
Hospital, Surabaya, Indonesia. Southeast Asian Journal
of Tropical Medicine and Public Health, 47(1), p.66.
Lee, B.Y., McGlone, S.M., Wong, K.F., Yilmaz, S.L.,
Avery, T.R., Song, Y., Christie, R., Eubank, S., Brown,
S.T., Epstein, J.M. and Parker, J.I., 2011. Modeling the
spread of methicillin-resistant Staphylococcus aureus
(MRSA) outbreaks throughout the hospitals in Orange
County, California. Infection control and hospital
epidemiology, 32(6), p.562.
Loke, H.Y., Kyaw, W.M., Chen, M.I.C., Lim, J.W., Ang,
B. and Chow, A., 2019. Length of stay and odds of
MRSA acquisition: a dose–response relationship?.
Epidemiology & Infection, 147.
Negara, K.S., 2016. Analisis implementasi kebijakan
penggunaan antibiotika rasional untuk mencegah
resistensi antibiotika di RSUP Sanglah Denpasar: studi
kasus infeksi methicillin resistant staphylococcus
aureus. Jurnal Administrasi Rumah Sakit Indonesia,
1(1).
Nkuwi, E.J., Kabanangi, F., Rugarabamu, S. and Majigo,
M., 2018. Methicillin-resistant Staphylococcus aureus
contamination and distribution in patient's care
environment at Muhimbili National Hospital, Dar es
Salaam-Tanzania. BMC research notes, 11(1), p.484.
Nuryah, A., Yuniarti, N. and Puspitasari, I., 2019.
Prevalensi dan Evaluasi Kesesuaian Penggunaan
Antibiotik pada Pasien dengan Infeksi Methicillin
JIMC 2020 - 1’s t Jenderal Soedirman International Medical Conference (JIMC) in conjunction with the Annual Scientific Meeting
(Temilnas) Consortium of Biomedical Science Indonesia (KIBI )
188

Resistant Staphylococcus Aureus di RSUP Dr. Soeradji
Tirtonegoro Klaten. Majalah Farmaseutik, 15(2),
pp.123-129.
Ramdass, M., Balliram, S., AC, B.N., Mohammed, B.,
Singh, R., Maharaj, J. and Boodram, A., 2018.
Prevalence of methicillin-resistant Staphylococcus
aureus in the surgical wards of the port-of-Spain
general hospital, Trinidad and Tobago. West Indian
Med J, 67(1), pp.57-59.
Sit, P.S., Teh, C.S.J., Idris, N., Sam, I.C., Omar, S.F.S.,
Sulaiman, H., Thong, K.L., Kamarulzaman, A. and
Ponnampalavanar, S., 2017. Prevalence of methicillin-
resistant Staphylococcus aureus (MRSA) infection and
the molecular characteristics of MRSA bacteraemia
over a two-year period in a tertiary teaching hospital in
Malaysia. BMC infectious diseases, 17(1), p.274.
VanEperen, A.S. and Segreti, J., 2016. Empirical therapy
in methicillin-resistant Staphylococcus aureus
infections: an up-to-date approach. Journal of
Infection and Chemotherapy, 22(6), pp.351-359.
Wong, J.W., Ip, M., Tang, A., Wei, V.W., Wong, S.Y.,
Riley, S., Read, J.M. and Kwok, K.O., 2018.
Prevalence and risk factors of community-associated
methicillin-resistant Staphylococcus aureus carriage in
Asia-Pacific region from 2000 to 2016: a systematic
review and meta-analysis. Clinical Epidemiology, 10,
p.1489.
Description of Methicillin-resistant Staphylococcus aureus Infection at Arifin Achmad General Hospital, Riau Province from 2015-2019
189
