
Comparison of Tear Interleukin-6 level, Conjunctival Inflammation,
and Tear Film Function in Daily Conventional Hydrogel and
Extended Silicone Hydrogel Contact Lens Wear
Tri Rahayu
1a
, Adisti
1b
, Weni Puspitasari
2c
and Umar Mardianto
1d
1
Department of Ophthalmology, Faculty of Medicine, Universitas Indonesia, Jakarta, Indonesia
2
Recidency Training Program Student of Department of Ophthalmology, Faculry of Medicine, Universitas Indinesia,
Jakarta, Indonesia
Keywords: Soft Contact Lense, Interleukin-6, Ocular Inflammation, Non Invasive-Tear Break Up Time, Tear Meniscus,
Optical coherence tomography
Abstract: Background: Contact lenses were increasing use worldwide. Silicone hydrogel material was proposed to be
safe for overnight Soft Contact Lens wear. This study aim to evaluate IL-6 levels, conjuctival inflammation,
tear function and tear menisci parameters after overnight wear of silicone hydrogel Soft Contact Lens and
compare with daily wear of hydrogel SCL. A randomized controlled trial carried out in myopia subjects,
treated using daily hydrogel (Nefilcon-A) SCL in one eye, and overnight silicone hydrogel (Lotrafilcon-B)
SCL in the fellow eye for 14 days. The slit lamp examination, NIBUT, Schirmer test, tear menisci measured
with OCT, and tear sampling for IL-6 were performed before and after SCL wear. One hundred and for eyes
from 52 subjects were included. The tear IL-6 significantly increases 6.37 pg/mL in Lotrafilcon-B and 4.46
pg/mL in Nefilcon-A. There were no significant conjunctival hyperemia changes in both groups (p=1.000)
nor significant correlation of tear IL-6 levels and conjunctival hyperemia (p = 0.234). The NIBUT of both
groups were decrease significantly (p=0.000). The Schirmer I were not significant changes after SCL wear.
The tear meniscus height were not significantly decrease in both groups. The tear meniscus area were
decrease significantly 1,181.5 μm2 in the the Lotrafilcon-B group and 1,795.0 μm2 in the Nelfilcon-A group.
The tear meniscus volume were decrease 0.08 μL in the the Lotrafilcon-B 0.05 μL in the Nelfilcon-A
group.The correlation between NIBUT, Schirmer I test and tear menisci parameter was not significant. Two
weeks of daily hydrogel and weekly silicone hydrogel SCL wear comparably increases tear IL-6, did not
increase conjunctival hyperemia, decreases NIBUT, tear menisci, without significant alterations in Schirmer.
1 INTRODUCTION
Prevalence of contact lens (CL) wear is increasing
with many reason.1–3 Increasing prevalence of
myopia4,5 lead to the increase of contact lens wear.
International contact lens prescribing in 2019 data4
shows that the mean age at fitting was in early 30s
(32.8 ± 14.9 years) and even younger in Asian
markets. Soft contact lens (SCL) was prescribed for
87%. Conventional hydrogel SCLs were prescribe for
21% daily wear CL patients compare to 57% of
silicon hydrogel for daily wear CL patients. Only 7%
a
https://orcid.org/0000-0000-0000-0000
b
https://orcid.org/0000-0000-0000-0000
c
https://orcid.org/0000-0000-0000-0000
d
https://orcid.org/0000-0000-0000-0000
extended wear SCLs were prescribed by the
practitioners.5 However, due to patient's need to have
good visual acuity over the time, then emerges
demand on overnight or extended wear (EW) SCL.
Contact lens wear can lead to complications
including corneal hypoxia, inflammation, contact
lens related discomfort and dryness.1,6 Conjunctival
hyperemia was one of its inflamation signs. It was
resulted by increase vascular permeability that were
often ascociated with tear Interlukin (IL)-6.7,8 Tear
IL-6 level in soft contact lens wearer have been
evaluated in some studies.8–12
Rahayu, T., Adisti, ., Puspitasari, W. and Mardianto, U.
Comparison of Tear Interleukin-6 level, Conjunctival Inflammation, and Tear Film Function in Daily Conventional Hydrogel and Extended Silicone Hydrogel Contact Lens Wear.
DOI: 10.5220/0010489401550163
In Proceedings of the 1st Jenderal Soedirman International Medical Conference in conjunction with the 5th Annual Scientific Meeting (Temilnas) Consortium of Biomedical Science Indonesia
(JIMC 2020), pages 155-163
ISBN: 978-989-758-499-2
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
155

Silicone hydrogel material was developed to
increase CL oxygen permeability. It is important to
prevent cornea hypoxia due to overnight CL wear
however, the addition of hydrophobic silicone
components lower the SCL wettability and cause
discomfort. Surface treatment makes SCL surface
becomes more hydrophilic, more comfortable to
wear, decrease dry eyes risk.6 On the other hand,
contact lenses made from conventional hydrogel
material need to have a high water content to increase
its oxygen permeability. High water content is related
to SCL dehydration and protein deposit that can cause
decrease of pre- and post-lens tear layer.13–15 Such
condition can cause low wettability and make tear
easier be evaporated.
SCL wearing duration could also affect tear layer
function. Fahmy et al16 reported that Daily Wear
(DW) SCL is more comfortable than weekly/monthly
wear with the same SCL. Similar result was found in
SiHy SCL with increased comfort in DW rather than
Extended Wear (EW).17
Evaluating tear film functions could be performed
with measuring Non-Invasive Break Up Time
(NIBUT), Schirmer, and tear volume.18,19 Tear
meniscus could be assess non invasively with Optical
Coherence Tomography (OCT). It was reported OCT
have a great precision to measure tear meniscus.
As far as our knowledge, there is no prior study
that evaluate the inflamation rate of SCL users with
an appropriate manner of SCLs wearing schedule
based on it’s material oxygen permeability. The aim
of this study to compare the effect of weekly wear of
silicon hydrogel SCL and daily wear conventional
hydrogel SCL on tear IL-6 level, conjunctival
inflammation, tear film functions, and the correlation
among that parameters.
2 MATERIAS AND METHODS
The subjects were recruited with inclusion criteria of
low to moderate myopia (-0.50 to -6.00 Diopters) and
astigmatism less than 1 diopters, subjects with 6/6
BCVA on both eyes, aged ≥18-35 years, had a good
general condition and were able to undergo a follow-
up procedure. The subjects with abnormal corneal
topography, have a disease or history of allergic or
atopic disease, NIBUT less than 10 seconds, work in
exposure to chemicals, smoke, hazardous gases, and
welding / flame sparks were excluded. Subjects who
did not come for follow up according to the schedule
determined by the researcher, resigned while the
research was in progress, experiencing severe
inflammation or infection in the eye, or did not use
SCL according to the instructions given by the
researcher consider to be drop out from the study.
Ethical clearance was obtained from the Ethics
Committee of the Faculty of Medicine Universitas
Indonesia (N0: KET-
135/UN2.F1/ETIK/PPM.00.02/2019).
Conjunctival inflammation with the was assessed
based on slit lamp camera photos by 2
ophthalmologist. The assessment was carried out
using the Efron Grading System.20 If there is a
difference of opinion between the two assessors, the
value taken is the highest grading number. Tear
samples were taken before and 14 days after SCL
wear. The tear IL-6 was examined at Biochemistry
Laboratory Faculty of Medicine, Universitas
Indonesia using the Human Interleukin-6 Elisa Kit
Coma Biotech® Quote JC5607 Product No.
K0331194 from Indonesian Genetics Science LLC.
The NIBUT was measured with Tearscope-plus®
(Keeler, Windsor, UK), determined by the time
(second) of Tearscope mirres on the cornea break
after blink. Schirmer I test was performed using
Schirmer test strips. Tear meniscus examination was
measured 3 times, 20-60 minutes, 7 days, and 14 days
after using SCL by measuring tear meniscus hight
(TMH) and tear meniscus area (TMA) using anterior
OCT of Cirrus™-HD OCT 5000, Carl Zeiss,
Germany. Manual measurement with ImageJ
software was used to measure TMV. Assessments
were done 3 times, 20-60 minutes, 7 days, and 14
days after using SCL. All the examiner were blinded
to the type of the SCL worn by the subjects.
3 RESULTS
There were 52 subjects (104 eyes) included to this
study, 10 subjects are male and 42 are female. The
mean age of subjects is 22.12±1.79 years.
JIMC 2020 - 1’s t Jenderal Soedirman International Medical Conference (JIMC) in conjunction with the Annual Scientific Meeting
(Temilnas) Consortium of Biomedical Science Indonesia (KIBI )
156
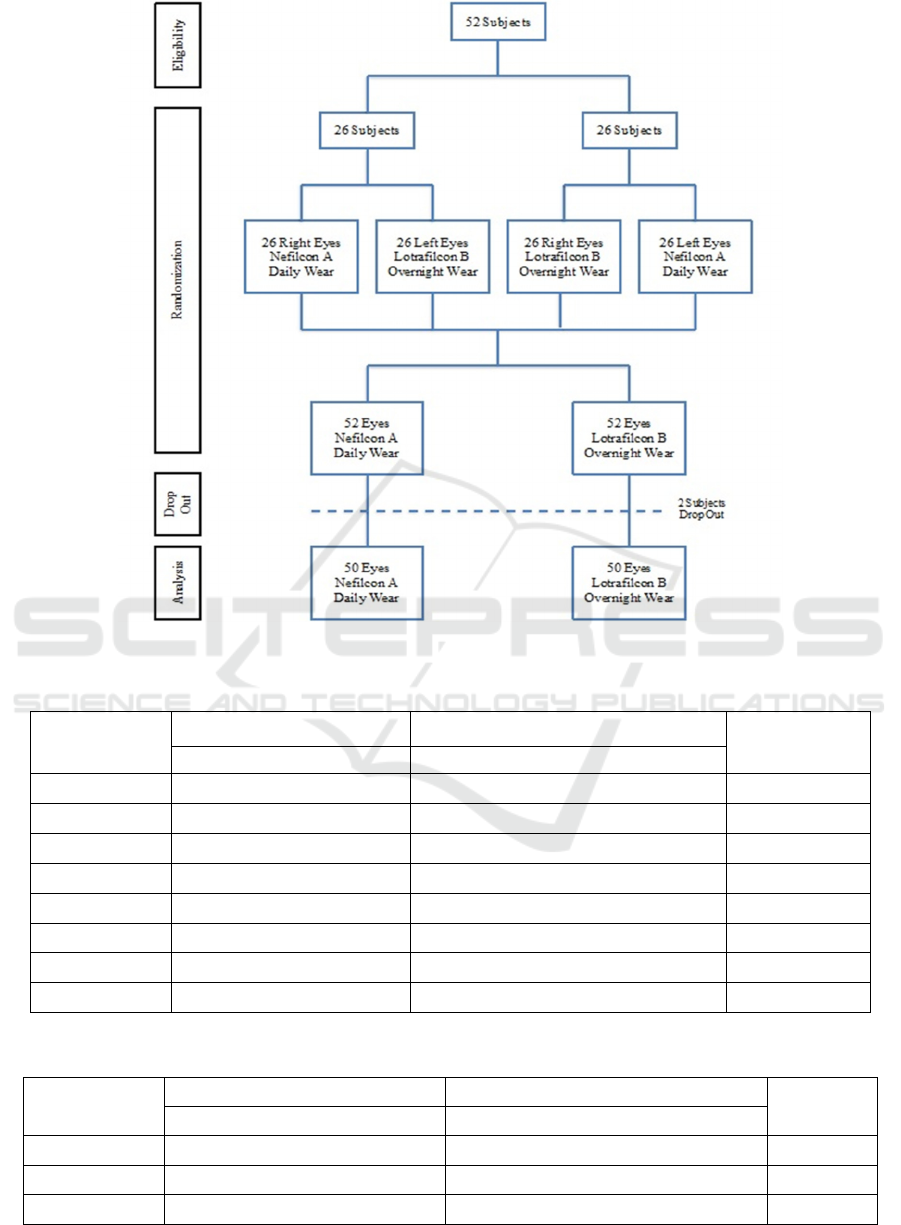
Figure 1. Scheme of Recruitment
Table 1. Clinical Characteristics data of Subjects in Two Groups
Parameter
Nefilcon A Lotrafilcon B
P value
Mean / Med (SD / Range) Mean / Med (SD / Range)
UCVA 0,40 (0,02 - 0,86) 0,50 (0,03 - 0,86) 0,386*
Spher (D) -1,25 (-6,00 - -0,50) -1,00 (-6,00 - -0,50) 0,169*
Cyl (D) -0,25(-1,25 - 0,00) -0,25 (-1,25 - 0,00) 0,399*
SCL (D) -1,25 (-6,00 - -0,50) -1,00 (-6,00 - -0,50) 0,059*
K1 (D) 42,93 (± 1,27) 42,92 (± 1,23) 0,697
K2 (D) 44,03 (± 1,23) 44,08 (± 1,22) 0,364
IL-6 pre (pg/ml) 1,24 (0,04 - 160,10) 0,95 (0,04 - 171,02) 0,695*
NIBUT 14,70 (± 3,72) 16,76 (± 5,05) 0,001
Table 2. The IL-6 Tear Level Before and After SCL wear between Groups
Parameter
Nefilcon A Lotrafilcon B
P value*
Median (Range) pg/ml Median (Range) pg/ml
IL-6 pre 1,24 (0,04 - 160,10) 0,95 (0,04 - 171,02) 0,695
IL-6 post 5,97 (0,07 - 698,95) 12,66 (0,11 - 1118,59) 0,101
IL-6 increase 4,46 (0,01 – 685,40) 6,37 (0,05 – 1115,8) 0,117
Comparison of Tear Interleukin-6 level, Conjunctival Inflammation, and Tear Film Function in Daily Conventional Hydrogel and Extended
Silicone Hydrogel Contact Lens Wear
157
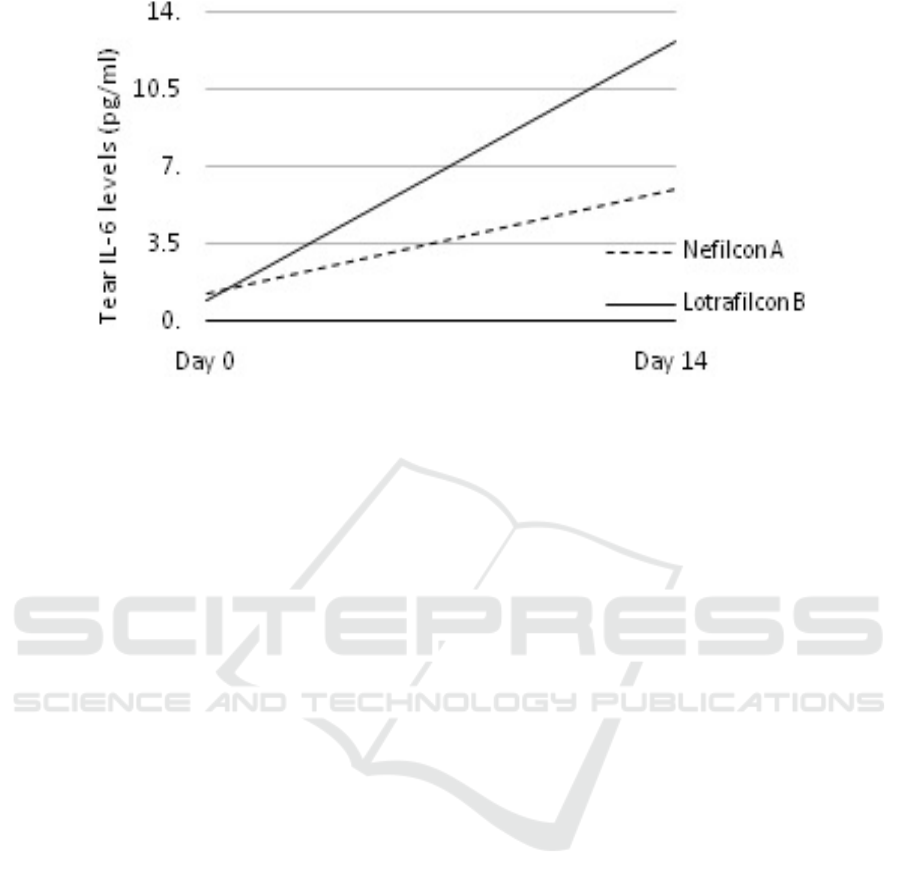
Figure 2. Comparison between IL-6 levels before and 14 days after daily use Neflicon A and weekly use of Lotrafilcon B
Lotrafilcon B were used in 21 eyes and 31 left eyes
while Nefilcon A were used in 31 right eyes and 21
left eyes. Two subjects were dropped out due to non-
compliance of SCL wear and lost to follow-up. Data
analysis was carried out in 100 eyes of 50 subjects, 50
eyes with Nefilcon A daily wear and 50 eyes with
Lotrafilcon B overnight wear (figure 2).
There is no significant difference in UCVA,
spherical and cylindical power correction,
keratometric value, and IL-6 tear levels between
groups before using SCL. The NIBUT value of
subjects in Lotrafilcon group was significantly higher
compare to those in Nefilcon group. However the
difference is not clinically significant, since the mean
NIBUT value of both group are in normal range.
(tabel 1).
There is a significant increase of tear IL-6
level after 14 days SCL wear in both groups
(p=0.000). However, there were no significant
differences in the delta IL-6 tear levels between
groups as seen in Table 2. The increasing tear IL-6
levels in weekly Lotrafilcon B SCL wearer seems
higher compare to those in daily Nefilcon A SCL
wearer. However, the difference is not statistically
signifinat. Figure 2.
There is no significant differences in
conjunctival inflammation, determined with Efron’s
Grading System, betwen two groups of SCL wearer
before and after 14 days using SCL as well
(p=0.000).The difference of conjunctival
inflammation changes was also not statistically
significant between two groups of SCL wearer (figure
3). Table 3 and 4 shows that the correlation between
tear IL-6 and conjunctival inflammation was not
significant. There was significant decrease the mean
of NIBUT in both groups after 14 days SCL wear.
The mean of NIBUT value changes were 3.4 seconds
in Nefilcon A daily SCL wear and 4.6 seconds in
Lotrafilcon B weekly SCL wear. The NIBUT
decrease after 14 days Lotrafilcon weekly SCL wear
was significantly greater rather than that in Nefilcon
daily SCL wear (p=0.008, Wilcoxon rank test). There
were no significant difference of Schirmer I change
before and after SCL wear between groups, that were
0.41 mm (-6.0 – 7.0 mm) in Nefilcon A group and
0.69 mm (-10 – 10 mm) in Lotrafilcon B group (p=
0.401, Wilcoxon rank test).
JIMC 2020 - 1’s t Jenderal Soedirman International Medical Conference (JIMC) in conjunction with the Annual Scientific Meeting
(Temilnas) Consortium of Biomedical Science Indonesia (KIBI )
158
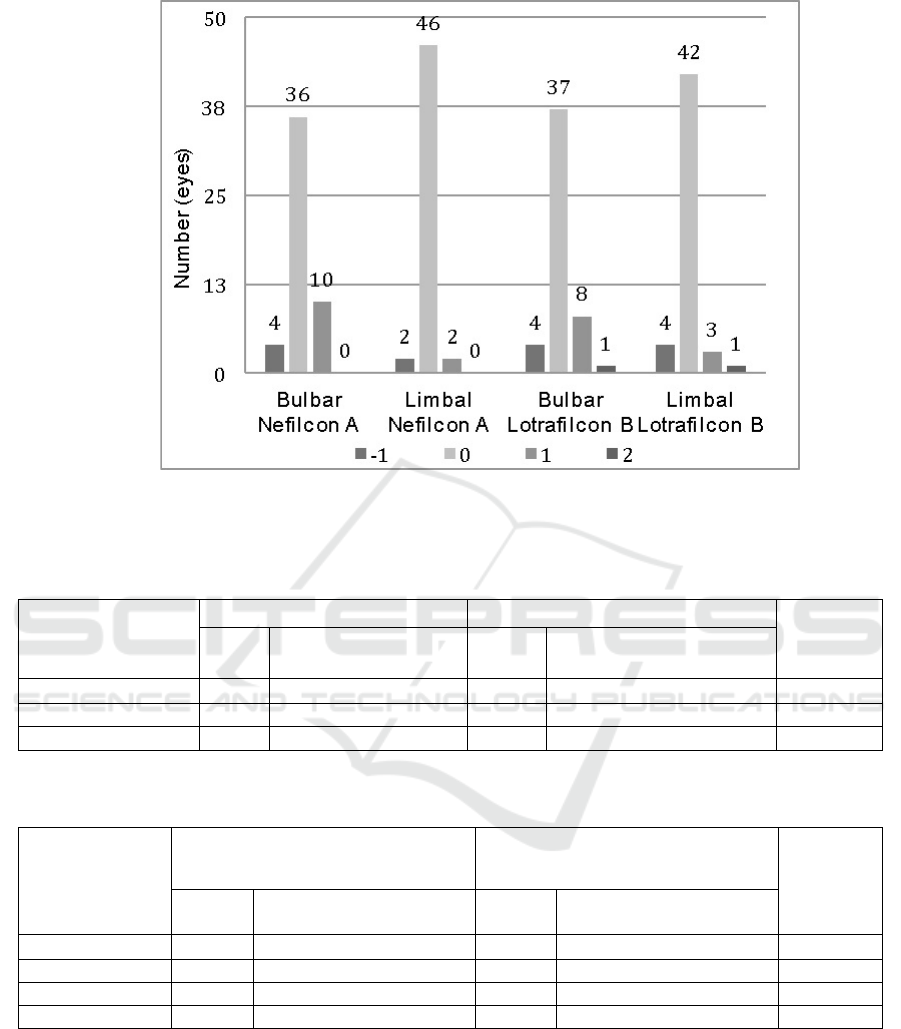
Degrees changes -1:One degree down, 0:No changes, 1:Increases by 1 degree, 2:increase by 2 degrees
Figure 3. Changes in the degree of conjunctival inflammation before and after daily use of Nefilcon A LKL and weekly use
of Lotrafilcon B
Table 3. Correlation between conjunctival bulbar inflammation and changes in IL-6 levels
Conjunctival
inflammation
(Efron’s Grade)
Nefilcon A Lotrafilcon B
P value*
n
Tear IL-6 Median
(Range)
n
Tear IL-6 Median
(Range)
(1) 9 0,38 (0,02 - 685,40) 10 4,61 (0,06 - 230,30) 0,243
(2) 40 4,60 (0,01 - 120,46) 36 5,61 (0,05 - 1115,80) 0,905
(3)** 1 8,48 (8,48 - 8,48) 4 15,7 (2,45 - 29,77) ----
*Mann Whitney rank. ** Not tested
Table 4. Correlation between conjunctival limbal inflammation and changes in IL-6 levels
Conjunctival
inflammation
(Efron’s Grade)
Nefilcon A Lotrafilcon B
P value*
n
Tear IL-6
Median (Ran
g
e)
n
Tear IL-6
Median (Ran
g
e)
(0) 1 0,13( 0,13 - 0,13) 0 ------ ----
(1) 46 4,46 (0,01 - 685,40) 47 7,03 (0,05 - 1115,8) 0,424
(2) ** 3 26,5 (0,05 - 120,46) 2 1,35 (0,83 - 1,87) ----
(3) ** 0 ------ 1 29,8 (29,8 - 29,8) ----
Comparison of Tear Interleukin-6 level, Conjunctival Inflammation, and Tear Film Function in Daily Conventional Hydrogel and Extended
Silicone Hydrogel Contact Lens Wear
159
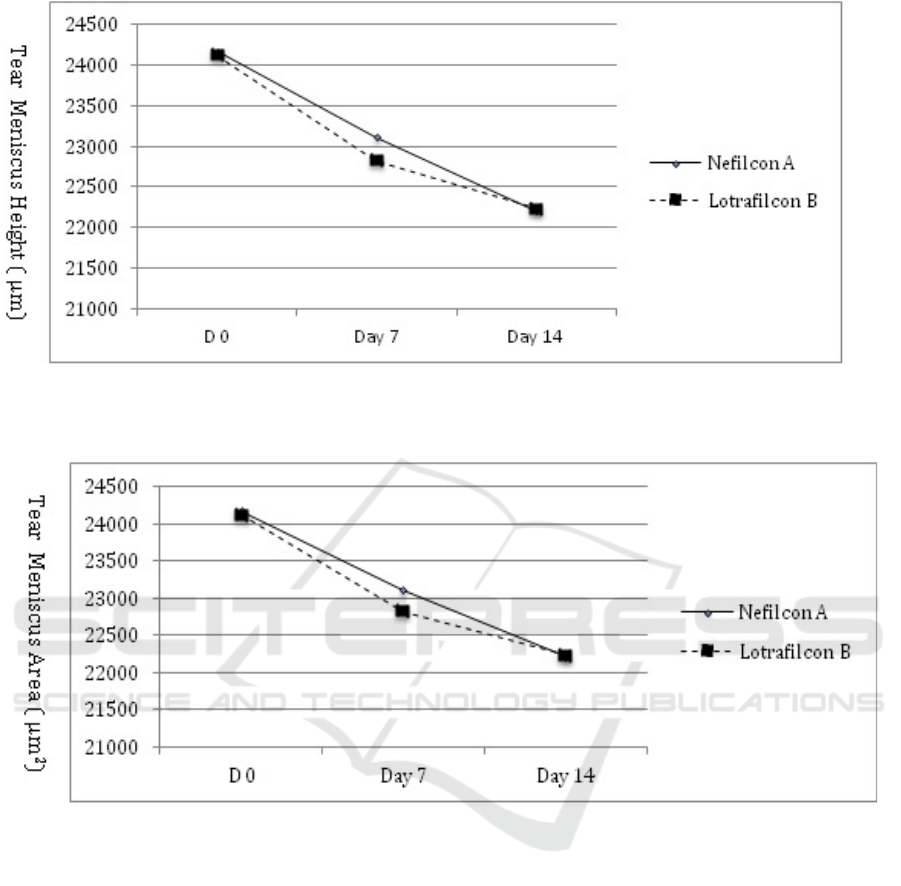
Nelfilcon A; Anova p=0.236
Lotrafilcon B; Anova p=0.476
Figure 3. Tear Meniscus Height mean value at day 0, day 7, and day 14 evaluation
Nelfilcon A: Anova p=0.001 0 vs 7 : p=0.085 7 vs 14: p=0.116 0 vs 14: p=0.000
Lotrafilcon B: Anova p=0.003 0 vs 7 : p=0.058 7 vs 14: p=0.548 0 vs 14: p=0.003
Figure 4. Tear Meniscus Area mean value changes from initial to day 14 evaluation
JIMC 2020 - 1’s t Jenderal Soedirman International Medical Conference (JIMC) in conjunction with the Annual Scientific Meeting
(Temilnas) Consortium of Biomedical Science Indonesia (KIBI )
160
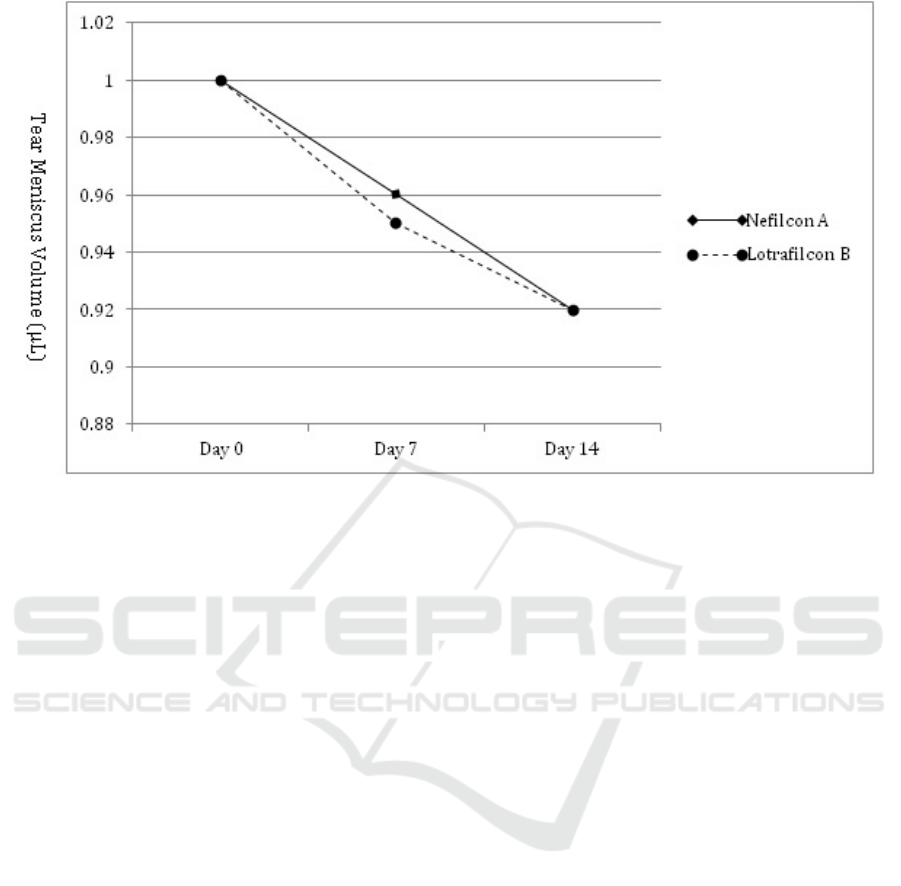
Nelfilcon A: Anova p=0,002 0 vs 7 : p=0,116 0 vs 14: p=0,001 7 vs 14: p=0,216
Lotrafilcon B: Anova p=0,005 0 vs 7 : p=0,073 0 vs 14: p=0,004 7 vs 14: p=0,56
Figure 5. TMV mean value changes from initial evaluation to day 14 evaluation
There are no significant TMH decrease in both
Nelfilcon A group (p=0.236, Anova test) and
Lotrafilcon B group (p=0.476, Anova test)(figure3).
There is also no significant diference TMH decrease
between group (p=0.556, Wilcoxon rank test).
There were significant decreases in mean of TMA
value after day 14 days of SCL wear, which are
1.795,0 μm2 in Nelfilcon A group and 1,181.5 μm2
in Lotrafilcon B group (figure 4). The decreases of
TMA between group have no significant difference
(p= 0.898, Wilcoxon rank test).
Changes in TMV mean value on both groups were
also found insignificantly different (p>0.05).
Changes in TMV mean value for Nelfilcon A and
Lotrafilcon B groups after 14 days are -0.08 μL and -
0.05 μL. These results were statistically insignificant
(p= 0.342). Figure 5 showed significant decrease of
TMV after 14 days wearing SCL, while the decrease
after 7 days wearing SCL was found insignificant.
Spearman correlation test was carried out in this
study. It is found that neither in group Nelfilcon A or
Lotrafilcon B was found significant correlation
between NIBUT or Schirmer 1, both initial and final
evaluation results, and TMH, TMA, and TMV both
initial and final evaluation results (r < ±0,3).
4 DISCUSSION
The level of IL-6 in tears increased significantly after
14 days SCL in both groups (p=0,000). However, the
difference in the increase of that was not significant
between groups (p=0.117). It could be proposed that
14 days of silicon hydrogel weekly overnight SCL
wear have equally effect in tear IL-6 levels increase
with daily conventional hydrogel SCL wear. Poyraz
et al9 found that increasing IL-6 values in
conventional hydrogel SCL users and silicone
hydrogel SCL wearer did not have significant
differences. In Poyraz’s study both SCL types were
used daily.
The conjuctival hyperemia of the subjects in this
study were not significantly changed before and after
14 days SCL wear, both in Nefilcon A group
(p=1.000) and Lotrafilcon B group (p=1.000). Fonn
et al21 reported that subjects using conventional
hydrogel SCL shows significantly higher increase
conjunctival injection compare to that who use silicon
hydrogel SCL. The effects difference of SCL wear in
Fonn’s study was probably caused by both type of
SCL with different Oxygen permeability were use for
overnight wear. Brennan et al22 found that
conventional hydrogel weekly SCL wearer showed a
significant higher level of conjunctival inflammation
compare to silicon hydrogel SCL wearer. Covey et
al23 reported the level of inflammation in high Dk
Comparison of Tear Interleukin-6 level, Conjunctival Inflammation, and Tear Film Function in Daily Conventional Hydrogel and Extended
Silicone Hydrogel Contact Lens Wear
161

silicone hydrogel SCL wearer were the same as in
normal not wearing SCL eyes, it was grade 2 (mild),
similar with our study. This suggests that 14 days of
properly SCL wear did not triger a significant
conjunctival inflammation yet.
There is no significant correlation between
elevated tear IL-6 levels with conjunctival
inflammation found in this study. Significant increase
in tear IL-6 after 14 day SCL wear was not followed
by an increase in conjunctival vascular injection.
Same findings were reported by Enrique de
Salamanca et al24 and Kalsow et al25, who suggest
that an increase in cytokines on the ocular surface
often occurs before the appearance of clinical
symptoms. Dogru et al8 reported that 2 weeks daily
use of silicone hydrogels SCL has a close relationship
with increased IL-6 in tears wich is not accompanied
by significant changes in the surface damage of the
conjunctiva or cornea, as well as changes in
keratoconjunctival cell morphology.
Soft Contact Lens wear could induce CLIDE,
because it increases evaporation, disturbs tear film
stability6,14 and alters tear production. Conventional
hydrogel SCL may cause CLIDE due to its high water
content, protein deposit, low wettability, and friction
between SCL and ocular surface.6,18,26 Meanwhile,
silicone hydrogel SCL that is more hydrophobic, have
lower wettability, and its extended wearing could
increase the risk of CLIDE.
The subjects of both groups experience
significant decrease of NIBUT after 2 weeks using
both SCL. This finding is similar to previous
studies.8,27,28 Weekly overnight Lotrafilcon B wear
dcreases NIBUT significantly greater compare to
daily Nefilcon A SCL wear (p=0.008). SCL wear
could intervere physiological quality of tear film due
to evaporation.8,14
We found no significant changes in Schirmer I
results after 14 days SCL wear in both group.
Iskeleli29 also found no decrease in Schirmer I
evaluation after 3 months of Lotrafilcon A and
Lotrafilcon B SCL wear. Other study by Dogru et al8
found no significant decrease after 2 weeks using
daily wear silicon hydrogel SCL.
There was no significant decrease of TMH after 2
weeks using both type of SCL. There was also no
significant difference of TMH decrease between the
two groups. This findings was similar with
Santodomingo-Rubido et al11 that found no
significant TMH difference between 4 groups of
Silicon Hydrogel wear for 1, 3, 6, 12, and 18 months.
Tear Meniscus Area was not significanty decrease
after 2 weeks using SCL, with no significant
difference between groups. Wang et al30 found no
significant decrease in TMA after 20 minutes using
two SCL types. Wang et al used 20 adapted subjects
using Balafilcon A on one eye and Galyfilcon A on
the other eye.
Our study found that both daily wear conventional
hydrogel and weekly silicone hydrogel SCLs waer
significantly decreases TMV after 2 weeks with no
significant difference between group. This is
accordance to study by Wang30 that found no
significance difference in TMV decrease in adapted
subjects after 20 minutes and 4 hours using SCL.
We found no correlation between NIBUT and
Schirmer I examination, both groups. Wang et al also
found no correlation between NIBUT and tear
volume which was assessed with fluorometry.31 It is
proposed that NIBUT shows tear film stability, not
tear quantity.
The correlation between Schirmer I and tear
menisci parameters has been studied both in normal
and dry eyes populations. Raj A et al32 evaluated tear
menisci in normal population using Fourier Domain
OCT and showed no correlation between Schirmer 1
and TMH. This result may be affected by Schirmer 1
method that used direct contact to eye so it affected
secretion reflex and tear base. Meanwhile, evaluation
with OCT used non-invasive method to measure tear
menisci at one time.
5 CONCLUSIONS
Tear IL-6 level increased significantly after 14 days
daily conventional and weekly silicone hydrogel SCL
wear. The increased tear IL-6 level occur before the
increase conjunctival hyperemia. The NIBUT,
Schirmer I, and tear menisci parameters have each
functions that can be replaced by one another. After 2
weeks of using daily wear Nefilcon A and weekly
Lotrafilcon B SCLs decereases the NIBUT and Tear
Meniscus Volume. It is suggested to evaluate tear
stability in long term SCL wearer.
REFERENCES
Lim CHL, Stapleton F, Mehta JS. Review of contact lens–
related complications. Eye Contact Lens.
2018;44(October):S1–10.
Moreddu R, Vigolo D, Yetisen AK. Contact Lens
Technology: From Fundamentals to Applications. Adv
Healthc Mater. 2019;8(15):1–24.
Nichols JJ, Willcox MDP, Bron AJ, Belmonte C, Ciolino
JB, Craig JP, et al. The TFOS International Workshop
on Contact Lens Discomfort: Executive summary.
Investig Ophthalmol Vis Sci. 2013;54(11).
Holden BA, Fricke TR, Wilson DA, Jong M, Naidoo KS,
Sankaridurg P, et al. Global Prevalence of Myopia and
High Myopia and Temporal Trends from 2000 through
JIMC 2020 - 1’s t Jenderal Soedirman International Medical Conference (JIMC) in conjunction with the Annual Scientific Meeting
(Temilnas) Consortium of Biomedical Science Indonesia (KIBI )
162

2050. Ophthalmology [Internet]. 2016;123(5):1036–42.
Available from:
http://dx.doi.org/10.1016/j.ophtha.2016.01.006
Morgan P, Woods CA, Tranoudis IG, Efron N, Jones L, B.
NLM, et al. International Contact Lens Prescribing in
2019. Contact Lens Spectr. 2020;
Kojima T. Contact lens-associated dry eye disease: Recent
advances worldwide and in Japan. Investig Ophthalmol
Vis Sci. 2018;59(14 Special Issue):DES102–8.
Cheung SW, Cho P, Chan B, Choy C, Ng V. A comparative
study of biweekly disposable contact lenses: Silicone
hydrogel versus hydrogel. Clin Exp Optom.
2007;90(2):124–31.
Dogru M, Ward SK, Wakamatsu T, Ibrahim O, Schnider C,
Kojima T, et al. The effects of 2 week senofilcon-A
silicone hydrogel contact lens daily wear on tear
functions and ocular surface health status. Contact Lens
Anterior Eye. 2011;34(2):77–82.
Poyraz C, Irkec M, Mocan MC. Elevated tear interleukin-6
and interleukin-8 levels associated with silicone
hydrogel and conventional hydrogel contact lens wear.
Eye Contact Lens. 2012;38(3):146–9.
Schultz CL, Kunert KS. Interleukin-6 levels in tears of
contact lens wearers. J Interf Cytokine Res.
2000;20(3):309–10.
Santodomingo-Rubido J, Wolffsohn JS, Gilmartin B.
Changes in ocular physiology, tear film characteristics,
and symptomatology with 18 months silicone hydrogel
contact lens wear. Optom Vis Sci. 2006;83(2):73–81.
Hibi M, Murakami M, Saito M, Hirano T, Taga T,
Kishimoto T. Molecular cloning and expression of an
IL-6 signal transducer, gp130. Cell. 1990;63(6):1149–
57.
Vidal-Rohr M, Wolffsohn JS, Davies LN, Cerviño A.
Effect of contact lens surface properties on comfort,
tear stability and ocular physiology. Contact Lens
Anterior Eye. 2018;41(1):117–21.
Craig JP, Willcox MDP, Argüeso P, Maissa C, Stahl U,
Tomlinson A, et al. The TFOS International Workshop
on Contact Lens Discomfort: Report of the contact lens
interactions with the tear film subcommittee. Investig
Ophthalmol Vis Sci. 2013;54(11).
Fonn D. Targeting contact lens induced dryness and
discomfort: What properties will make lenses more
comfortable. Optom Vis Sci. 2007;84(4):279–85.
Fahmy M, Long B, Giles T, Wang CH. Comfort-enhanced
daily disposable contact lens reduces symptoms among
weekly/monthly wear patients. Eye Contact Lens.
2010;36(4):215–9.
Stapleton F, Tan J. Impact of contact lens material, design,
and fitting on discomfort. Eye Contact Lens.
2017;43(1):32–9.
Bron AJ, Abelson MB, Ousler G, Pearce E, Tomlinson A,
Yokoi N, et al. Methodologies to diagnose and monitor
dry eye disease: Report of the diagnostic methodology
subcommittee of the international Dry Eye Workshop
(2007). Ocul Surf. 2007;5(2):108–52.
Downie LE, Craig JP. Tear film evaluation and
management in soft contact lens wear: a systematic
approach. Clin Exp Optom. 2017;100(5):438–58.
Efron N. Grading scales for contact lens complications.
Ophthalmic Physiol Opt. 1998;18(2):182–6.
Fonn D, MacDonald KE, Richter D, Pritchard N. The
ocular response to extended wear of a high Dk silicone
hydrogel contact lens. Clin Exp Optom.
2002;85(3):176–82.
Brennan NA, Coles MLC, Comstock TL, Levy B. A 1-year
prospective clinical trial of balafilcon A (PureVision)
silicone-hydrogel contact lenses used on a 30-day
continuous wear schedule. Ophthalmology.
2002;109(6):1172–7.
Covey M, Sweeney DF, Terry R, Sankaridurg PR, Holden
BA. Hypoxic effects on the anterior eye of high-Dk soft
contact lens wearers are negligible. Optom Vis Sci.
2001;78(2):95–9.
Enríquez-de-Salamanca A, Castellanos E, Stern ME,
Fernández I, Carreño E, García-Vázquez C, et al. Tear
cytokine and chemokine analysis and clinical
correlations in evaporative-type dry eye disease. Mol
Vis. 2010;16(February):862–73.
Kalsow CM, Reindel WT, Merchea MM, Bateman KM,
Barr JT. Tear cytokine response to multipurpose
solutions for contact lenses. Clin Ophthalmol.
2013;7:1291–302.
Efron N. Contact Lens Complications: Third Edition.
Contact Lens Complications: Third Edition. 2012.
Eghosasere I, E IJ, Joy O. Effect of Soft Contact Lens
Materials on Tear Film Stability and Central Corneal
Radius of Curvature: A Comparative Study of
Polymacon and Lotrafilcon B. Sierra Leone Journal of
Biomedical Research 2011;3(3):144–50.
Walther H, Subbaraman LN, Jones L. Novel in vitro
method to determine pre-lens tear break-up time of
hydrogel and silicone hydrogel contact lenses. Contact
Lens Anterior Eye [Internet]. 2019;42(2):178–84.
Available from:
https://doi.org/10.1016/j.clae.2018.11.002
Iskeleli G, Karakoc Y, Ozkok A, Arici C, Ozcan O, Ipcioglu
O. Comparison of the effects of first and second
generation silicone hydrogel contact lens wear on tear
film osmolarity. Int J Ophthalmol. 2013;6(5):666–70.
Wang J, Cox I, Reindel WT. Upper and lower tear menisci
on contact lenses. Investig Ophthalmol Vis Sci.
2009;50(3):1106–11.
Wang J, Palakuru JR, Aquavella J V. Correlations Among
Upper and Lower Tear Menisci, Noninvasive Tear
Break-up Time, and the Schirmer Test. Am J
Ophthalmol. 2008;145(5).
Raj A, Dhasmana R, Nagpal RC. Anterior segment optical
coherence tomography for tear meniscus evaluation and
its correlation with other tear variables healthy
individuals. J Clin Diagnostic Res. 2016; 10(5):NC01–
4..
Comparison of Tear Interleukin-6 level, Conjunctival Inflammation, and Tear Film Function in Daily Conventional Hydrogel and Extended
Silicone Hydrogel Contact Lens Wear
163
