
Association of Epstein Barr Virus Infection to Prognosis Factors of
Invasive Breast Cancer in Semarang Kariadi General Hospital
Population
Wasisto Dwi Yudisaputro
1a
, Djoko Handojo
2 b
, Yan Wisnu Prajoko
2c
and Dik Puspasari
d
1
Surgical Oncology Trainee, Faculty of Medicine University of Diponegoro / RSUP Dr. Kariadi Semarang
2
Department of Oncology Surgery, Faculty of Medicine University of Diponegoro / RSUP Dr. Kariadi Semarang
3
Department of Pathology Anatomy, Faculty of Medicine University of Diponegoro / RSUP Dr. Kariadi
Keywords: Breast Cancer, Prognosis Factors of Breast Cancer, EBV Infection, Molecular Detection of EBV
Abstract: Breast cancer is the most common malignant disease in female. In addition to internal factors, external factors
such as viral infections are thought to have a role in the carcinogenesis process of breast cancer. In the case
of nasopharyngeal cancer, Epstein-Barr Virus (EBV) has been shown to be able to activate several signaling
pathways so that cancer cells become more aggressive and have a worse prognosis. This study aims to
determine the relationship of the detection status of EBV DNA with the prognosis factor of breast cancer. The
research design used in this study was analytic observational with a cross-sectional approach, with 71 paraffin
block samples from the Anatomical Pathology Laboratory of Kariadi General Hospital who obtained from
mastectomy or Breast Conserving Surgery. Samples was examined using PCR to detect EBV DNA in tumor
cells. age of breast cancer cases ranged from 23 to 78 years with median age of 52 years. From 71 samples,
there were 28 positive samples (39.4%) of EBV DNA and 43 samples (60.6%) were negative. Significant
results were obtained (p < 0.05) in the relationship between EBV infection and tumor size (p = 0.002), axillary
lymph node metastasis (p = 0.001), and lymphovascular invasion (p = 0.001). Our research could find a
significant statistical association in the status of axillary lymph nodes, lymphovascular invasion status and
tumor size in breast cancer samples infected by EBV and those not infected by EBV..
1 INTRODUCTION
Breast cancer is the most common malignant disease
in female (Bray et al.,2018). The incidence of breast
cancer in Indonesia in female is the highest (Manuaba
, Burmansyah, and Tjindarbumi, 2010; WHO, 2014)
. In addition to internal risk factors such as genetic
and sex hormones, external factors such as viral
infections also play a role in the process of
carcinogenesis (Alibek et al., 2013; Ahmed et
al.,2019). The relationship of the epstein-barr virus
(EBV) with breast cancer is based on several reasons,
such as the high incidence of male breast cancer,
which is reported in Mediterranean countries,
endemic areas for EBV, the occurrence of several
a
https://orcid.org/0000-0002-9791-1200
b
https://orcid.org/0000-0003-1694-2054
c
https://orcid.org/0000-0002-1126-4939
d
https://orcid.org/0000-0002-8043-564X
EBV-related lymphomas in the breast, and
morphological similarities between breast medullary
cancers and nasopharyngeal cancer (KNF) (Zekri et
al., 2012). EBV is a family of herpesviruses and has
two variations (type 1 and type 2) (Joshi and
Buehring, 2012;. Hjalgrim, Friborg, and Melbye,
2007). In the human body, EBV will settle in B
lymphocytes, and from B lymphocytes EBV will
produce several viral proteins (LMP, EBNA, and
EBER) that can affect cell growth signals from its
host (Chang, Moore, and Weiss, 2017; Kim, Kim,
Park, 2013; Kanda, 2018;He et al., 2003). Some
authors believe that EBV might play a role in the
oncogenesis of breast cancer not as a major etiology
but as a cofactor in the development of breast cancer
and can influence the aggressive nature of breast
116
Yudisaputro, W., Handojo, D., Prajoko, Y. and Puspasari, D.
Association of Epstein Barr Virus Infection to Prognosis Factors of Invasive Breast Cancer in Semarang Kariadi General Hospital Population.
DOI: 10.5220/0010488701160120
In Proceedings of the 1st Jenderal Soedirman International Medical Conference in conjunction with the 5th Annual Scientific Meeting (Temilnas) Consortium of Biomedical Science Indonesia
(JIMC 2020), pages 116-120
ISBN: 978-989-758-499-2
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

cancer (Louise et al.,1 995;Murray et al.,2003;
Arbach et al.,2006; Mazouni et al., 2011)
Treatment modalities for breast cancer include
surgery, chemotherapy, hormonal therapy,
immunotherapy, and external radiation (Panigoro and
Purwanto, 2012). The success of the therapy given
will be related to predictive factors and prognostic
factors (Ramli, 2015; Cianfrocca and Goldstein,
2004) Several established prognostic factors such as
hormone receptors, Her2 expression, tumor size,
axillary lymph node metastases and lymphovascular
invasion can affect the aggressive nature of breast
cancer so that it will affect the survival rate and
disease-free interval (Carter et al., 1989; Fisher et al.,
1988)
With the development of molecular biology, EBV
infection in breast cancer can be determined by using
PCR examination by detecting the presence of EBV
DNA in cancer cells22,23. The purpose of this study
is to find out whether there is a relationship between
the detection status of EBV DNA and the prognosis
factor for breast cancer. The results of this study not
only can find out the prevalence of EBV infection in
breast cancer cases in Kariadi Hospital, but also can
be the basis for further research on the role of EBV in
the carcinogenesis of breast cancer.
2 MATERIAL AND METHODS
2.1 Patients and Tissue
The research design used in this study was analytic
observational with a cross-sectional approach. This
study consisted of a Formalin-Fixed Paraffin-
Embedded (FFPE) of cancer biopsy from 71 cases of
invasive breast cancer stage I to III that had been
performed mastectomy or Breast Conserving
Surgery. The samples were taken from the pathology
anatomy laboratory of Kariadi Hospital from January
2019 to September 2019. Each paraffin tumor block
will be extracted DNA and then DNA amplification
by PCR was done in the pathology anatomy
laboratory of FKKMK UGM. The primers used were
(forward primers
5‘GGCCTCCAAGGAGTAAGAC-C3‘ and reverse
primers: 5‘CCCCTCTTCAAGGGGTC-TAC3') that
were circulating on the market24. The DNA positive
control for EBV comes from KNF where the virus
was detected and the negative control uses nuclease-
free distilled water instead of DNA.
Histopathological data provided axillary lymph node
metastasis, tumor size, receptor hormone status, Her2
overexpression status, degree of malignancy and
lymphovascular invasion and were obtained from
medical record data and anatomical pathology report
of Kariadi Hospital.
2.2 Statistical Analysis
Data is processed using the SPSS 20.0 for Windows.
The Chi square test was used for parametric test, and
Mann Whitney test for non-parametric test to
determine the relationship between the detection
status of EBV DNA with the degree of malignancy,
estrogen receptor status, progesterone receptor status,
Ki 67 status, lymphovascular invasion status, Her 2
status, and axilla lymph node metastasis. The value of
the significance is <0.05.
3 RESULTS
Study found that some relationship between EBV
DNA status and prognosis factors for breast cancer
among the patients (Table 1).
Association of Epstein Barr Virus Infection to Prognosis Factors of Invasive Breast Cancer in Semarang Kariadi General Hospital Population
117
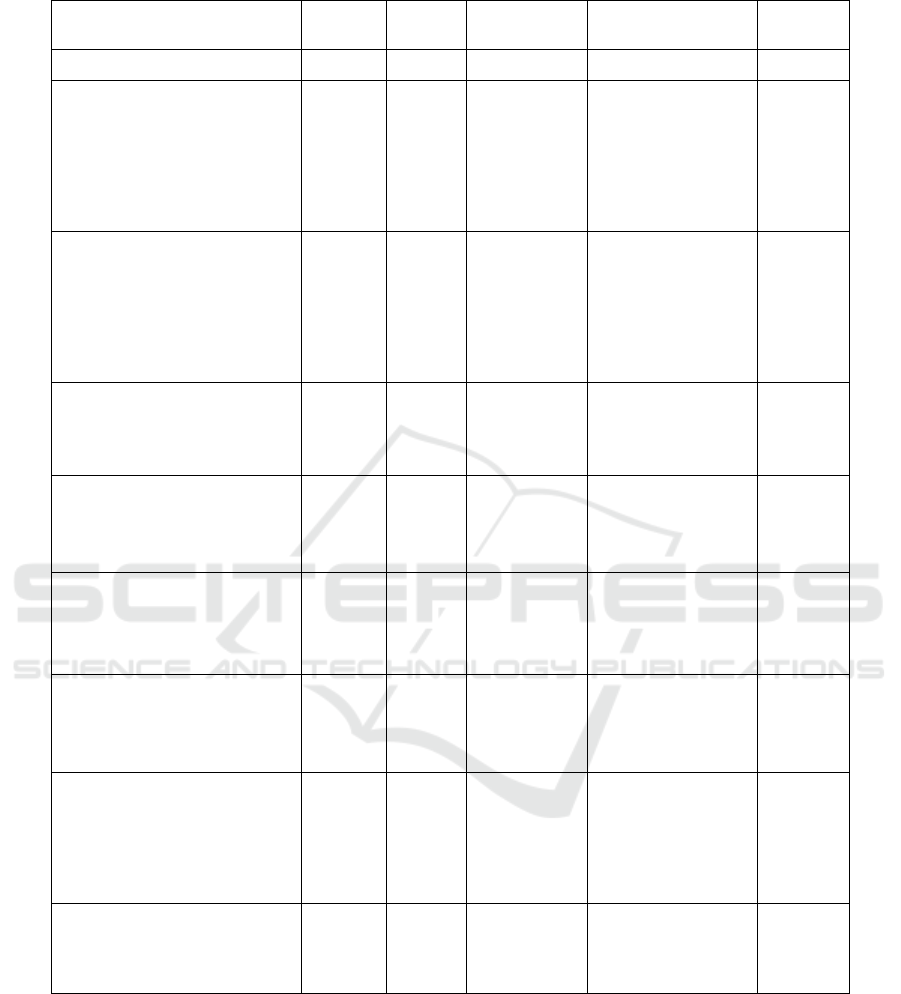
Table 1. Relationship between EBV DNA status and prognosis factors for breast cancer
Characteristics EBV (+) EBV (-) Mean ± SD Median (min – max) P Value
Age 49,97 ± 11,99 52 (23 – 78)
Tumor size
T1 0 0
T2 3 22 P = 0.002
T3 14 9
T4 11 12
Axillary lymph node metastasis
Negative 1 17
1 – 3 0 15 P = 0.001
4 – 10 18 8
>10 9 3
Estrogen Receptor
P = 0.605 Negative 10 18
Positive 18 25
Progesterone Receptor
P = 0.843
Negative 15 22
Positive 13 21
Her 2
P = 0,673
Negative 21 26
Positive 11 7
Ki 67
P = 0.750
< 20% 5 9
> 20% 23 24
Malignancy grade
P = 0.808
1 0 4
2 21 24
3 7 15
Lymphovascular invasion
P = 0.001
Negative 4 24
Positive 25 20
4 DISCUSSION
In this study the prevalence of breast cancer samples
which EBV Epstein Barr Virus (EBV) were detected
was 28 samples (39.4%). According to
epidemiological studies carried out by Huo Q et al. on
the basis of PCR examination, the prevalence of EBV
infection worldwide is 29.32% and prevalence at the
Asian level is 35.25% (Huo, Zhang, and Yang, 2012)
The prevalence of EBV DNA detection status in
this study has a higher rate than the prevalence
worldwide, or in Asia. The higher incidence can be
caused by demographic differences and the
characteristics of the research sample (Hjalgrim,
JIMC 2020 - 1’s t Jenderal Soedirman International Medical Conference (JIMC) in conjunction with the Annual Scientific Meeting
(Temilnas) Consortium of Biomedical Science Indonesia (KIBI )
118

Friborg, and Melbye, 2007)
This study proves the link between the EBV
infection and the incidence of breast cancer, but only
a small proportion of positive EBV cases develop into
breast cancer. This shows that only EBV alone is not
enough as an etiological factor in carcinogenesis, a
number of biological and environmental cofactors are
also needed for the occurrence of breast cancer
(Alshammari, 2017).
The results of our study have significant statistical
association of EBV infection with tumor size. This
result is in accordance with some studies
conductedpreviously. Arbach in his research found
that EBV infection in breast cancer cells can increase
the ability of these tumor cell mutations such as
invasion, angiogenesis, and metastasis. As in the case
of nasopharyngeal cancer, the LMP-1 oncoprotein
produced by EBV induces cyclooxygenase 2 (COX-
2) which then induces vascular endhotelial growth
factor that plays a role in the process of angiogenesis
through NF-κB signaling (Arbach et al., 2015).
LMP-1 is directly related to oncogenesis, because
it is able to activate several cellular signaling
pathways such as Nuclear Factor-κB, c-Jun NH2-
terminal kinase (JNK), p38 kinase,
phosphatidylinositol 3-kinase (PI3K), and several
other possible pathways. thereby resulting in
continuous proliferation and inhibits apoptosis (Sun
et al.,2015)
One of the oncoproteins found in Epstein-Barr
virus is EBNA-1. The oncogenic role of EBNA-1
protein has been reported by some previous
researchers. EBNA-1 can reduce p53 levels by
triggering ubiquitin specific protease USP7 so that
p53 becomes unstable. In the end the breast gland
epithelium is infected with EBV so that the cells
become proliferated continuously and anti-apoptotic
(Frappier, 2012)
The results of our study have significant statistical
association of EBV infection with The metastatic
status of axillary lymph nodes and lymphovascular
invasion status. These findings come in agreement
with studies conducted by Fessahaye et al., 2017. Our
study shows that tumor cells contained in the EBV
gene have the potential for metastases to occur, which
suggest aggressive tumor behaviour, and making
them a poor prognostic factor. Arbach et al. who
showed that EBV infection of breast tumor enhances
its mutagenic properties, such as invasion,
angiogenesis, and metastasis.
5 CONCLUSION
The conclusion of this study is, there are significant
statistical association in the status of axillary lymph
nodes, lymphovascular invasion status and tumor size
in breast cancer samples infected by EBV and those
not infected by EBV.
REFERENCES
Ahmed ES, Elnour LS, Siddig EE and Hassan R. Molecular
detection of Epstein-Barr virus in breast cancer among
Sudanese female population: a case-control study
[version 1; peer review: 2 not approved].
F1000Research 2019, 8:1355
(https://doi.org/10.12688/f1000 research.19422.)
Alshammari F A, Association between HPV , CMV , EBV
and HS Viruses and Breast Cancer in Saudi Arabia, J.
Cancer Prev. Curr. Res., 2017, vol. 7, no. 3, pp. 1–7
Arbach H, Viglasky V, Lefeu F, Guinebretière JM, Ramirez
V, Bride N, Boualaga N, Bauchet T, Peyrat JP, Mathieu
MC, Mourah S, Podgorniak MP, Seignerin JM, Takada
K, Joab I. Epstein-Barr virus (EBV) genome and
expression in breast cancer tissue: effect of EBV
infection of breast cancer cells on resistance to
paclitaxel (Taxol). J Virol. 2006 Jan;80(2):845-53. doi:
10.1128/JVI.80.2.845-853.2006. PMID: 16378986;
PMCID: PMC1346837.
Alibek K, Kakpenova A, Mussabekova A, Sypabekova M,
Karatayeva N. Role of viruses in the development of
breast cancer. Infect Agent Cancer. 2013;8:32.
Published 2013 Sep 2. doi:10.1186/1750-9378-8-32
Bray, F., Ferlay, J., Soerjomataram, I., Siegel, R.L., Torre,
L.A. and Jemal, A. (2018), Global cancer statistics
2018: GLOBOCAN estimates of incidence and
mortality worldwide for 36 cancers in 185 countries.
CA: A Cancer Journal for Clinicians, 68: 394-424.
https://doi.org/10.3322/caac.21492.
Carter CL, Allen C, Henson DE. Relation of tumor size,
lymph node status, and survival in 24,740 breast cancer
cases. Cancer. 1989 Jan 1;63(1):181-7. doi:
10.1002/1097-0142(19890101)63:1<181::aid-
cncr2820630129>3.0.co;2-h. PMID: 2910416
Chang Y, Moore PS, Weiss RA. Human oncogenic viruses:
nature and discovery. Philos Trans R Soc Lond B Biol
Sci. 2017;372(1732):20160264.
doi:10.1098/rstb.2016.0264
Cianfrocca M, Goldstein LJ. Prognostic and predictive
factors in early-stage breast cancer. Oncologist.
2004;9(6):606-16. doi: 10.1634/theoncologist.9-6-606.
PMID: 15561805.
Fessahaye G, Elhassan AM, Elamin EM, Adam AM,
Anghesom Ghebremedhin A, Ibrahim ME. Association
of Epstein - Barr virus and breast cancer in Eritrea.
Infect Agents Cancer 12, 62 (2017).
https://doi.org/10.1186/s13027-017-0173-2
Association of Epstein Barr Virus Infection to Prognosis Factors of Invasive Breast Cancer in Semarang Kariadi General Hospital Population
119

Fisher B, Redmond C, Fisher ER, Caplan R. Relative worth
of estrogen or progesterone receptor and pathologic
characteristics of differentiation as indicators of
prognosis in node negative breast cancer patients:
findings from National Surgical Adjuvant Breast and
Bowel Project Protocol B-06. J Clin Oncol. 1988
Jul;6(7):1076-87. doi: 10.1200/JCO.1988.6.7.1076.
PMID: 2856862
Frappier L. Contributions of Epstein-Barr nuclear antigen 1
(EBNA1) to cell immortalization and survival. Viruses.
2012 Sep;4(9):1537-47. doi: 10.3390/v4091537. Epub
2012 Sep 13. PMID: 23170171; PMCID:
PMC3499818.
He B, Raab-Traub N, Casali P, Cerutti A. EBV-encoded
latent membrane protein 1 cooperates with
BAFF/BLyS and APRIL to induce T cell-independent
Ig heavy chain class switching. J Immunol. 2003 Nov
15;171(10):5215-24. doi:
10.4049/jimmunol.171.10.5215. PMID: 14607922;
PMCID: PMC4625407.
Hjalgrim H, Friborg J, Melbye M. The epidemiology of
EBV and its association with malignant disease. In:
Arvin A, Campadelli-Fiume G, Mocarski E, et al.,
editors. Human Herpesviruses: Biology, Therapy, and
Immunoprophylaxis. Cambridge: Cambridge
University Press; 2007. Chapter 53. Available from:
https://www.ncbi.nlm.nih.gov/books/NBK47424/
Huo Q, Zhang N, Yang Q. Epstein-Barr virus infection and
sporadic breast cancer risk: a meta-analysis. PLoS One.
2012;7(2):e31656. doi: 10.1371/journal.pone.0031656.
Epub 2012 Feb 21. PMID: 22363698; PMCID:
PMC3283657.
Joshi D, Buehring GC. Are viruses associated with human
breast cancer? Scrutinizing the molecular evidence.
Breast Cancer Res Treat. 2012 Aug;135(1):1-15. doi:
10.1007/s10549-011-1921-4. Epub 2012 Jan 25.
PMID: 22274134
Kanda T. EBV-Encoded Latent Genes. Adv Exp Med Biol.
2018;1045:377-394. doi: 10.1007/978-981-10-7230-
7_17. PMID: 29896676.
Kim JH, Kim WS, Park C. Epstein-Barr virus latent
membrane protein 1 increases genomic instability
through Egr-1-mediated up-regulation of activation-
induced cytidine deaminase in B-cell lymphoma. Leuk
Lymphoma. 2013 Sep;54(9):2035-40. doi:
10.3109/10428194.2013.769218. Epub 2013 Feb 28.
PMID: 23363221.
Louise G. Labrecque, Diana M. Barnes, Ian S. Fentiman
and Beverly E. Griffin, Epstein-Barr Virus in Epithelial
Cell Tumors: A Breast Cancer Study, Cancer Res
January 1 1995 (55) (1) 39-45;
Manuaba T, Burmansyah, Tjindarbumi D, Panduan
Penatalaksanaan Kanker Solid, 2010th ed. Denpasar:
Sagung Seto, 2010.
Mazouni C, Fina F, Romain S, Ouafik L, Bonnier P,
Brandone JM, Martin PM. Epstein-Barr virus as a
marker of biological aggressiveness in breast cancer. Br
J Cancer. 2011 Jan 18;104(2):332-7. doi:
10.1038/sj.bjc.6606048. Epub 2010 Dec 21. PMID:
21179039; PMCID: PMC3031896.
Murray PG, Lissauer D, Junying J, Davies G, Moore S, Bell
A, Timms J, Rowlands D, McConkey C, Reynolds GM,
Ghataura S, England D, Caroll R, Young LS. Reactivity
with A monoclonal antibody to Epstein-Barr virus
(EBV) nuclear antigen 1 defines a subset of aggressive
breast cancers in the absence of the EBV genome.
Cancer Res. 2003 May 1;63(9):2338-43. PMID:
12727860..
Panigoro S, Purwanto H, Panduan Penatalaksanaan
Kanker payudara. Jakarta: Kementerian Kesehatan,
2012
Ramli,M , Update Breast Cancer Management, Vol 38
(2015): Supplement 1 Pp 28-53
Sun L, Zhao Y, Shi H, Ma C, Wei L. LMP-1 induces
survivin expression to inhibit cell apoptosis through the
NF-κB and PI3K/Akt signaling pathways in nasal
NK/T-cell lymphoma. Oncol Rep. 2015
May;33(5):2253-60. doi: 10.3892/or.2015.3847. Epub
2015 Mar 10. PMID: 25760809.2
WHO, Indonesia 2014 Cancer Incidence,pp. 22–23, 2014.
https://www.who.int/cancer/country-
profiles/idn_en.pdf
Zekri A R., Bahnassy AA, Mohamed W S, El-Kassem F A,
El-Khalidi S J, Hafez M M, Hassan Z K, Epstein-Barr
virus and breast cancer: Epidemiological and Molecular
study on Egyptian and Iraqi women, Journal of the
Egyptian National Cancer Institute, Volume 24, Issue
3,2012,Pages 123-131,
.
.
.
JIMC 2020 - 1’s t Jenderal Soedirman International Medical Conference (JIMC) in conjunction with the Annual Scientific Meeting
(Temilnas) Consortium of Biomedical Science Indonesia (KIBI )
120
