
A Study of the Impact of the Organizational Purchasing Structure on
Supplier’s Performance in the Hospital Sector
Kaoutar Jenoui
Laboratory Smartilab, Moroccan School of Engineering Sciences (EMSI) Rabat, Morocco
Keywords: Purchasing, Hospital sector, performance, supplier, healthcare organization.
Abstract: The purchasing function plays a key role in the hospital sector. To achieve economies of scale in process costs,
one of the questions that arises as a healthcare organization is whether to centralize or decentralize purchasing
activities. Several managers of hospital systems mentioned the problem of choosing a better purchasing
structure. In most cases, the choice of the organizational purchasing structure directly involves an impact on
supplier’s performance. However, this impact has never been considered in this decision. Organizational
innovation is a major issue for the performance of hospitals, but the performance of suppliers also has a heavy
impact on the improvement of health infrastructure. Nowadays supplier’s performance is an essential element
for improving the quality process of hospital care. In this context, we propose to analyse whether considering
supplier’s performance could affect the decision regarding the organizational purchasing structure in the
hospital sector. We verify the influence of purchasing structures on both the objectives of the hospital
purchasing process, as well as on the performance of suppliers, through a study-test carried out in CHIS Rabat-
Morocco.
1 INTRODUCTION
In Morocco, the Ministry of Health has undertaken
several actions to make medical products available
and accessible to the population. It has a national list
according to the last revision, which was carried out
in 2011. The pharmaceutical products covered by this
list benefit from an annual budget allocated by the
Ministry of Health, to ensure their availability at the
level of public hospitals and health care facilities.
This budget increased by 67% between 2002 and
2012, reaching the sum of 1.6 billion dirham (
Cheng
E.W.L, 2001
). Despite the efforts made by the
ministry, access to medications and medical devices
in hospitals remains insufficient (Charles Collins
1994). The main factor that reduces the availability of
medical products is the inability to achieve good
supplier performance. Experiences have shown that it
is possible to improve access to these products by
making the best use of resources, and by streamlining
management processes (
Modi,2007). Indeed, the
choice of the purchasing structure could help to
develop the performance of the supplier's supply
chain. As it could also involve a variety of risks that
harm this performance. This change itself leaves an
indirect impact on the performance of the hospital's
supply chain. Choosing the right organizational
purchasing structure is essential for improving the
performance of the supplier's system. Therefore, our
study aims to highlight the improvement of the
organizational purchasing structure, and
simultaneously evolve the quality of services and
pharmaceutical products from suppliers. We propose
to organize this paper as follows. We will detail the
problematic in section 2. In Section 3, we will present
the two scenarios: centralized and decentralized
purchasing. In section 4, we will present the study-
test framing, followed by a discussion and analysis of
results. Finally, we will conclude with some
perspectives.
2 PROBLEM DESCRIPTION
From 1980 there have been six changes made to the
hospital purchasing system. Sometimes they are
based on the centralized structure, sometimes on the
decentralized structure, (see Table 1). After 2003, the
choice was to take the centralized structure as the
unique and stable choice. The application of each
structure has generated advantages and disadvantages
for hospitals. The budgets allocated to the purchasing
of pharmaceuticals products by the Ministry of Health
are of the order of 2 billion dirhams annually. This
budget has experienced a spectacular increase over
the past 12 years, as the budget for 2003 did not
exceed 300 million dirhams (
Juran, J.M. 1990).
Table 1: A brief history of the health care supply system
1917 Centralization Creation of the central
pharmacy in Casablanca
1980 Decentralization With many difficulties
encountered by the central
pharmacy, there was an
introduction of the direct
delivery system by
manufacturers to health
facilities.
1985-
1986
Centralization
The aggravation of problems
due to the small size of the
premises and the storage
spaces implies a return to
centralization. They installed
the new Berrechid unit for
the storage and distribution
of pharmaceuticals.
1994 Decentralization Creation of the supply
division under the general
secretariat of the Ministry of
Health.
1995 Centralization Implementation of the
Berrechid unit to centralize
medical products
purchases.
1997 Decentralization Decentralization of
purchasing
2001 Centralization Centralization of supply
(purchasing, storage,
distribution) by the
purchasing division.
2003 Decentralization Decentralization of
purchases in view of the
difficulties of regular
supplies.
In the face of all these changes and developments
in the organizational purchasing structure, Moroccan
hospitals continue to suffer from insufficient quality,
unavailability of pharmaceuticals products and rising
costs (
Deming, W.E. 1950). Storage and distribution
centers cost up to one billion Dirhams per year. In
addition, the storage and distribution of medical
products in Morocco costs the Ministry of Health
over 30 million Dirhams per year (
K. Jenoui,2017; A.
Abouabdellah, 2014). This shows huge costs due to the
poor performance of the supplier and the
inappropriate choice of organizational purchasing
structure. In this optic, we propose to study the impact
of the purchasing structure on the supplier’s
performance through a study-test to validate the main
causes of the variation in their performance and look
for possible solutions. We set two main objectives:
- Simulation of both scenarios with suppliers:
centralized structure, and decentralized structure,
with studying the impact of each of them on the
development of hospital objectives.
- Assessment of supplier performance in terms of
total cost and delivery date and analyse the impact of
implementing each purchasing structure on their
performance.
3 SCENARIOS MODELING:
CENTRALIZED AND
DECENTRALIZED
We will propose a model, which allows us to make a
comparison that relates to the differences between the
results of both scenarios. According to the suppliers
interviewed, we take stock of the costs, which are
presented in two types:
3.1 Variable or Operational Costs
Variable costs are costs constituted only by charges
that vary with the volume of activity of the company,
for example, the quantities produced and/or sold,
without necessarily being an exact proportionality
between the variation in charges and the variation in
the volume of products obtained.
3.2 Fixed Costs
Fixed costs correspond to the charges generated by
administration or sustainable investments. They are
not proportional to the quantities produced. To follow
sales price creation, variable costs are considered one
of the main issues for suppliers (
A. Marie, 2006; D.
Serrou, 2016
). Although the production cost is the
most important to indicate, it is often necessary to be
able to break down the cost structure into several
costs. In this study we have focused on the following
types:
The production cost, which consists of
making all direct expenses that were made to
produce a good, including the purchase and
consumption of materials, labor,
maintenance of equipment (
J. Dumoulin,
2004
).
The distribution cost, which includes all the
charges necessary for the distribution and
sale of the product. It includes expenses due
to the management of the stock of products,
transport to sale, but also additional
expenses directly linked to the distribution
of products (
P. Trouiller, 2013).
The preparation cost, which is the cost
associated to an order, includes all the
expenses necessary to prepare an order,
which depends of the number of parcels and
the number of units of parts, such as the costs
of handling, picking and packaging.
In our model, the notation used is shown in Table 2.
Table 2.
E: Central pharmacy
H: Number of hospitals, each represented by the
index i, where i ϵ {1, 4}
S: Number of suppliers, each is represented by the
index j, where j ϵ {1, 10}
Q
: Quantity of products ordered from each
supplier j
Dh
: The requirement date imposed for each
supplier j
TCc
: Total cost in centralization structure for
each supplier j.
TCd
: Total cost in decentralization structure
for each supplier j.
GC
: Gap time in centralization structure for
each supplier j.
GD
: Gap time in decentralization structure for
each supplier
j
.
Centralization Decentralizati
on
Unit price for
each product j
U
U
Distance
covered
Distance
between
supplier j and
central
pharmacy D
Distance
between
supplier j and
hospital i D
Preparation
cost per
product j
Cc
Cd
Delivery cost
per product j
Tc
Td
Labor cost for
distribution
per hour
Pc
Pd
Number of
parcels
delivered by
each supplier j
Nc
Nd
The delivery
date indicated
by each
supplier j
Dc
f
Dd
f
Number of
hours for
distribution
Distribution of
product j to the
central
pharmacy d
Number of
hours for the
distribution of
product j to the
hospital i d
The time
remaining to
the start of the
validity period
indicated by
each supplier j
for each
product i
Tc
Td
Total cost
TCc
Q
∗
U
Q
∗
Cc
Pc
∗
Tc
∗ D
+
d
∗ P
TCd
Q
∗
U
Q
∗
Cd
Pd
∗
Td ∗ D
+ d
* P
4 STUDY-TEST FRAMING
The CHIS Ibn Sina Rabat is one of the most important
hospital structures in Morocco. It brings together ten
specialized hospitals with a multi-site platform
created since 1954. The CHIS is implementing
significant resources to improve its daily efficiency.
In this context, our study aims to optimize logistics
activities. Currently, the hospital is leading a project
to regroup pharmacies, which must consider the
management of supplier performance. Consequently,
activities are carried out in redundancy in several
establishments and sometimes in several departments
within the same hospital. The strategy of pooling
resources was born because of several observations.
In most cases, the aim of the consolidation is to
reduce operating costs and increase the efficiency of
the system. It is in this optic that we are interested in
studying the impact of the organizational purchasing
structure on supplier performance. To implement the
test-study, we approached it by looking for 20
suppliers who would probably accept our test-study.
We contacted them by email, explaining the
objectives behind our study, and then we made
several phone calls with several potential participants
to discuss a short survey to assess needs. 80% of
suppliers indicated that they are not satisfied with the
organizational purchasing structure established by
healthcare organizations, and 45% of them are
interested in our test study, while 35% of suppliers do
not care about any change. 20% of suppliers show
interest in the hospital purchasing strategy, however,
only 45% of them are interested in participating in
this study, making a total of nine suppliers as
indicated in figure 1. The major challenge is to clearly
communicate the plan to each supplier, in a form that
they can understand and put into practice (Figure 2).
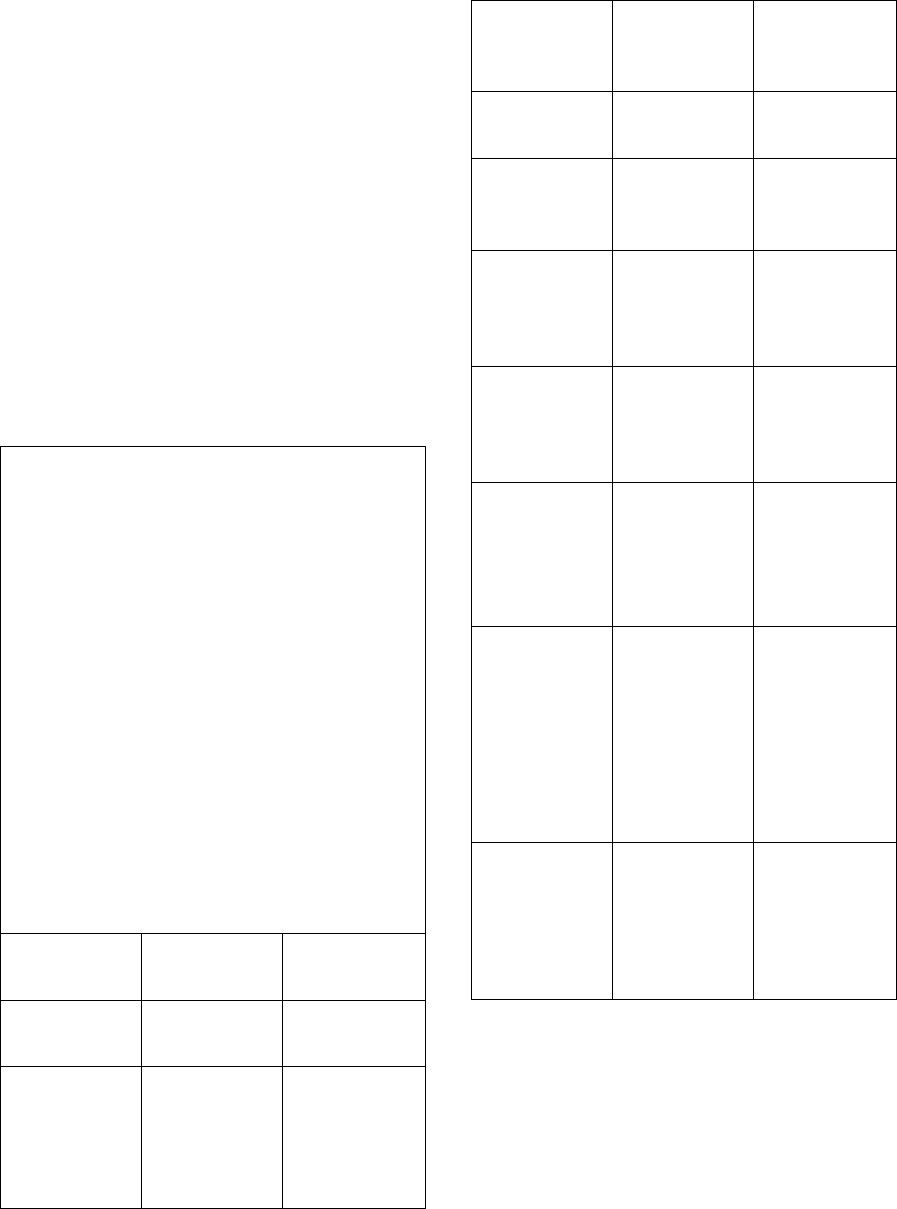
Figure 1 : Survey results
5 RESULTS ANALYSIS
Suppliers return responses to our study after three
months. Each of them prepared answers to our test,
using a team of experienced specialists in the medical
field.
Figure 2 : Input and Output flow
5.1 Unit Price and Distribution Costs
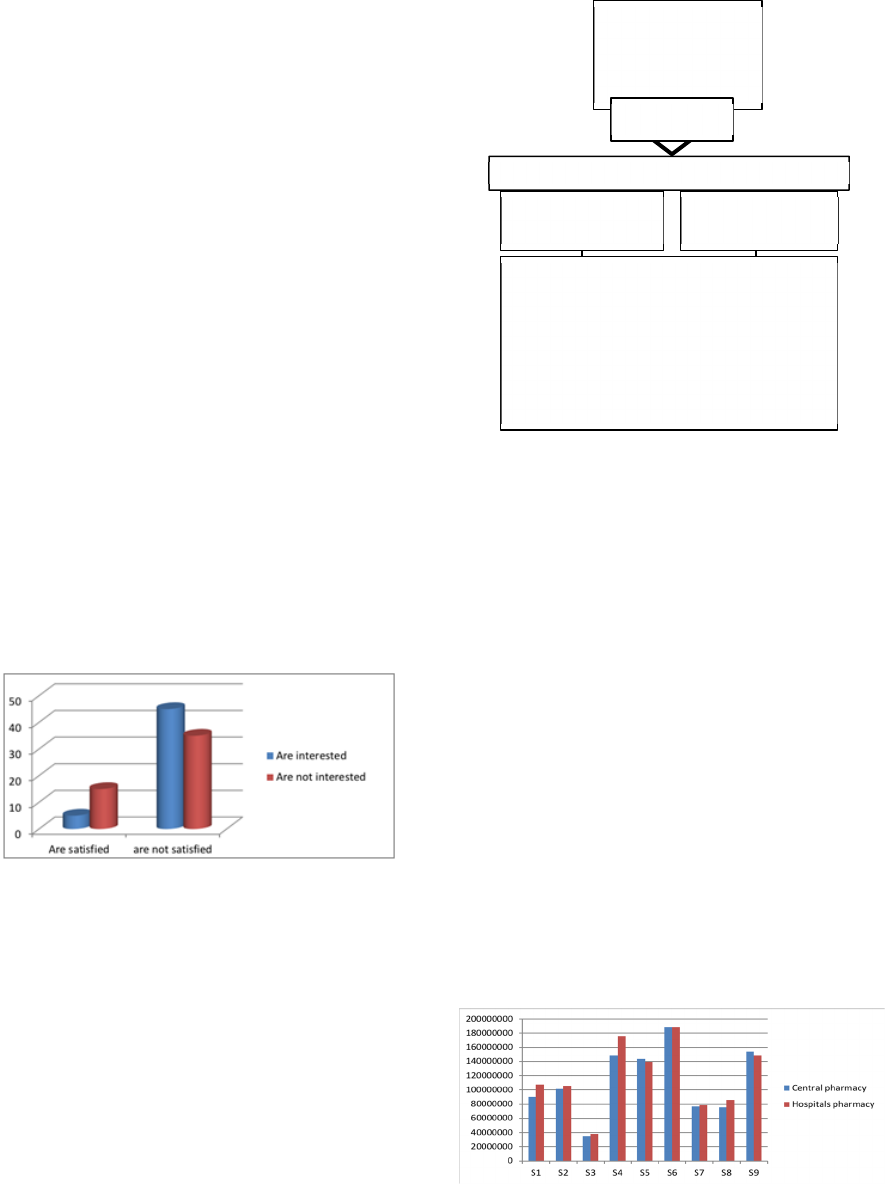
As shown in figure 3 and table 3, the unit price
increases in case of decentralization for most of
suppliers except suppliers 5 and 9. To understand this
behaviour, we show in figure 4 and 5, the details of
each supplier. As for supplier 9, he meets the delivery
time requirements for H3 and for the central
pharmacy; he delays delivery eight days for H1, H2
and H4. While supplier 9 has only 40% of the order
in the stock, either he will meet the delivery date for
Hospital 3 and delay delivery for others while
reducing the unit price, or he will deliver the central
pharmacy on time, while keeping the same initial
price and making urgent production. Following the
previous case, with only 50% of order in stock,
supplier 5 has two choices, either he delivers 30% to
H4 and 20% to H2 on time with the initial price, and
delays delivery for H1 and H4 while reducing the unit
price, or he choose to deliver the central pharmacy on
time with urgent production while keeping the initial
price.
Figure 3: Comparison of unit prices in both purchasing
structures
- Unit price
- Number of parcels
- Preparation cost
- Delivery cost
- Delivery time
- Time remaining for the
start of the validit
y
date
Out
p
ut flow
Input flow
- Quantity
requested
- Delivery date
9 suppliers
Decentralized
structure
Centralized
structure
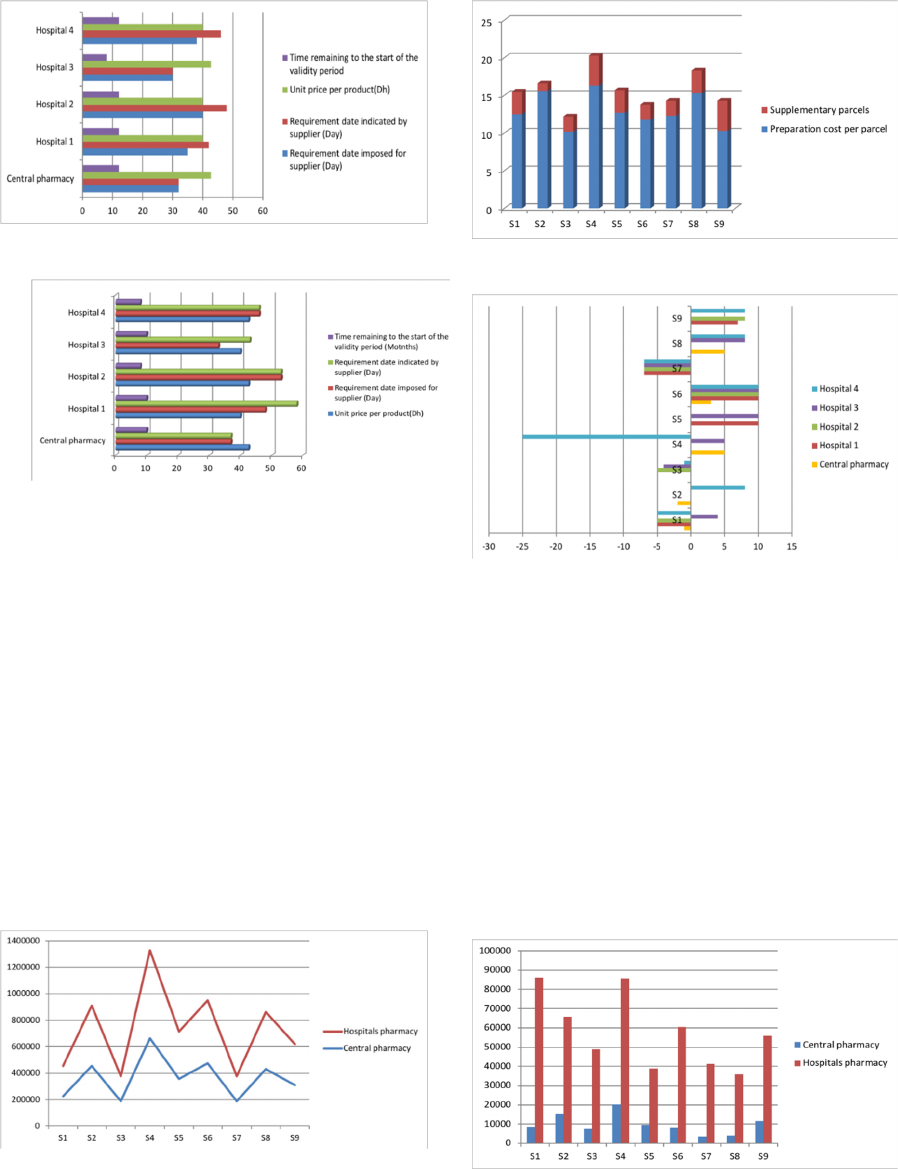
Figure 4: Results obtained for supplier 9
Figure 5: Results obtained for supplier 5
5.2 Preparation Costs
As shown in Figure 6 and table 4, preparation costs
are higher in the case of decentralization. The small
difference is justified by the number of optimized
parcels in the case of centralization. In addition, the
preparation cost per parcel, which differs from one
supplier to another.
Supplier 4 is distinguished by a maximum total
preparation cost, and a considerable cost difference
between both structures, which amounts to 0.07% of
the total cost. This difference is justified by the
additional number of parcels in the case of
decentralization (figure 7), and a high preparation
cost compared to other suppliers, which amounts to a
5.2% difference.
Figure 6: Comparison of preparation costs in both
purchasing structures
Figure 7: Additional parcels for each supplier
Figure 8: Delivery dates proposed by suppliers
5.3 Delivery Costs
As shown in Figure 9 and Table 5, the delivery costs
incurred by suppliers in case of decentralization are
much higher than in case of centralization. The
increasing number of delivery costs has been realized
due to the multiplication of possible routes to deliver
to several dispersed points. A large difference in the
delivery costs (up to 18%) is allocated to the delivery
of the order between both structures, which is
justified by the number of kilometers recorded by
each supplier traveling to each hospital, and the unit
cost delivery that differs from one supplier to another.
Figure 9: Comparison of delivery costs in both purchasing
structures
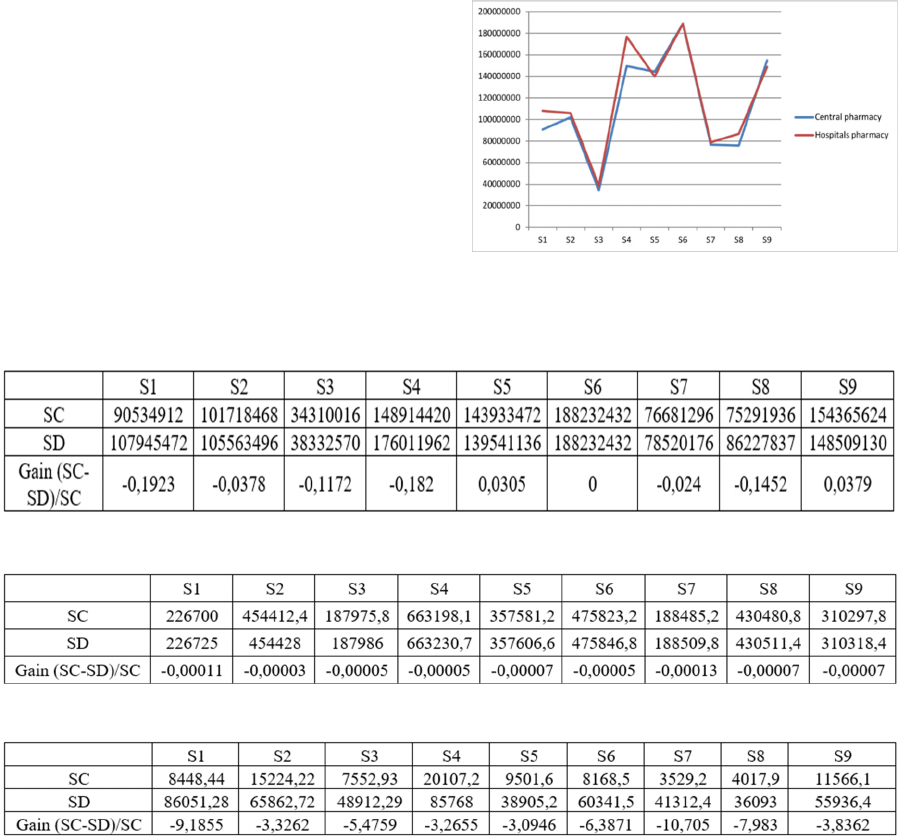
5.4 Change in Variable Costs
The results generated on the variable costs, for
different suppliers in both cases are indicated as
follows:
- The variable costs are strictly higher in the case of
decentralization:
In this case, the variable costs are higher for 55.6% of
suppliers, this being due to the increase of preparation
and delivery costs. The centralization system helps
suppliers to manage parcels in a better way by
enabling efficient optimization that can achieve
savings of up to 2.7% of the total cost. It is a small
gain, but still significant. In addition, most of
suppliers offer lower prices to purchasers in case of
centralized system, which is due to the large quantity,
which motivate suppliers to make urgent production,
to keep the market.
- The variable costs are higher or equal in the case
of centralization:
The time remaining to the start of the validity period
of medical products is imposed by hospitals to be at
least 18 months at the time of delivery. 22.2% of
suppliers respect this constraint for all orders, which
pushes them to increase prices. Variable product costs
are almost the same in both purchasing structures for
22% of suppliers.
Figure 10: Comparison of variable costs in both purchasing
structures
Table 3: Total order price generated in each structure
Table 4: Preparation costs in both structures
Table 5: Delivery costs values in both strategies
6 CONCLUSIONS
The hospital system must ensure an irreproachable
quality of service and optimize its supply chain.
Managers need to choose the most appropriate
organizational structure that helps pharmaceutical
suppliers improve their performance. Centralization
is a system in which decision-making and
administrative acts are organized around a single
center of power. In this study the centralized hospital
system gave better results, it is more efficient in terms
of variable costs, cost effectiveness and reduction of
expired medical products. However, this study does
not take into account the hidden costs generated by
suppliers, which will be taken into account in our next
study in which we will develop a decision-making
approach in the hospital sector for the choice of the
organizational purchasing structure.
REFERENCES
Cheng E.W.L, Li H. (2001) « Analytic hierarchy process:
An approach to determine measures for business
performance », Measuring Business Excellent, Vol 5,
N0 3, pp. 30-36
Charles Collins, Andrew Green. - Decentralization and
primary health care: some negative implications in
developing countries, 1994 - International Journal of
Health Services, Vol 24 (3), 459-475
Rapport de la commission « approvisionnement du secteur
public en médicaments et consommables médicaux»
Février 2008.
Modi, S.B. & Mabert, V.A. (2007). Supplier development:
Improving supplier performance through knowledge
transfer. Journal of operations management, 25, 42 -64
Juran, J.M. 1990. China’s Ancient History of Managing for
Quality, Quality Progress, July 1990, page 32
Deming, W.E. 1950. Elementary Principles of the
Statistical Control of Quality, JUSE
K. Jenoui, A. Abouabdellah, “Estimating supplier’s hidden
quality costs with Taguchi quality loss function and
Topsis method”. In 10th International Colloquium on
Logistics and Supply Chain Management, Rabat,
Morocco, 2017.
A. Abouabdellah, A. Cherkaoui, "Decision Support System
for Predicting the degree of a cancer patient's
empowerment". Journal of Theoretical and Applied
Information Technology, 60(3), 517-523, 2014.
A. Marie, C. Giuliani, A. Abouabdellah, A. Cherkaoui,
"The empowerment of patients factoring: Reporting to
a holonic approach". In 9th Conference on service
systems and service management, Troyes, France,
2006.
D. Serrou, A. Abouabdellah, “Logistics in the hospital:
Methodology for measuring performance”. ARPN
journal of engineering and applied sciences, 11(5), 250-
256, 2016.
P. Trouiller, Technical support for improving the
management and organization of hospital pharmacies,
2013.
