
The Effectiveness of Tele Mental Health
Shelly Iskandar
1
, Steven Saputro
2
, Syifa Nabilah
2
, Tania
2
, Tiara Syafitri Putri
2
, Vimal Chander
2
,
Mutiara Utami
1
1
Department of Psychiatry, Faculty of Medicine, Universitas Padjadjaran/Hasan Sadikin General Hospital, Bandung
2
Faculty of Medicine, Universitas Padjadjaran, Bandung
Keywords: tele mental health, telepsychiatry, telemedicine, effectiveness.
Abstract: Background: The emergence of 2019 novel coronavirus (2019-nCoV) in Wuhan, China in December 2019
has caused coronavirus disease (COVID-19) and created a confusing situation. COVID-19 is considered
responsible for an increase in psychological problems including anxiety, depression, and even mass hysteria.
However, along with these conditions, orders to minimize direct contact and time spent in public were
implemented to prevent the spread COVI-19, so many psychiatrists turned face-to-face care to tele mental
health. This paper will provide the effectiveness of tele mental health compared with face-to-face care in
regards to psychiatric services in a setting of quarantine or isolation. A manual search was conducted to select
articles published between 2005 and 2020 using the PubMed database. We included full-text articles
published in English that reported the effectiveness of telepsychiatry in a setting of quarantine or isolation.
Among 557 articles, only 5 studies met all criteria and were included in the review. These articles reported
the effectiveness of tele mental health for those who are in a setting of quarantine or isolation. Tele mental
health helps those who need psychiatric services, but are not able to have a face-to-face consultation. This
review shows equivalent overall effects between tele mental health or face-to-face care in psychiatric services.
While the results are equivalent, few studies were obtained. Thus, more research is needed to establish
equivalence.
1 INTRODUCTION
The emergence of 2019 novel Coronavirus (2019-
nCoV) in Wuhan and the pandemic COVID-19
announcement from the World Health Organization
(WHO) in March 2020, has changed the world rapidly
and evoking multiple responses. (Coronavirus
disease, 2019; Chen JA,et al.2020; Moring JC, et
al.2020) It has infected more than 100 nations around
the world and had been declared as public health
emergency.(Health UDo,2019) As part of spreading
mitigation, the Centers for Disease Control and
Prevention (CDC) recommend limiting outdoor
movement and practicing social distancing.(Mark
É,et al.2020) This restriction may provoke stress and
in the end worsen mental health condition over time.
(Whaibeh E,et al 2020) This can be seen from the
elevating of anxiety, depression, mass hysteria,
posttraumatic stress disorder (PTSD) and negative
societal behaviors rates.(Ćosić K,et al.2020; Duan L
and Zhu G,2020)
There are the hindrance in mental health
treatment, and the consequences are lost work
productivity, unemployment, homelessness, marital
and parenting problems, domestic violence, drug and
alcohol abuse, suicides and others.(Ćosić K,et
al.2020; Tanielian TL,et al.2008) The increasing
demand for mental health services become a potential
risk of creating a global public mental health crisis.(
Ćosić K,et al.2020)
A survey conducted by Centers for Disease
Control and Prevention (CDC) shown that in June
2020, 40% of Americans reported struggling with
mental health or substance abuse problems.( Mark
É.,et al 2020) Quarantine, isolation, trauma
experienced by frontline workers, victims and their
family also create a challenges for healthcare
providers, including mental health provider.(
Whaibeh E,et al 2020)
Despite the adverse repercussions that have
occurred, mental health services must still be done.6
To meet the needs, many mental health center had to
adopt new strategies to ensure continuity of
treatment.(Moring JC,et al.2020) Tele mental Health
has a potential in addressing the psychological
problems of this condition. (Whaibeh E,et al 2020)
296
Iskandar, S., Saputro, S., Nabilah, S., Tania, ., Putri, T., Chander, V. and Utami, M.
The Effectiveness of Tele Mental Health.
DOI: 10.5220/0010370502960300
In Proceedings of the International Conference on Health Informatics, Medical, Biological Engineering, and Pharmaceutical (HIMBEP 2020), pages 296-300
ISBN: 978-989-758-500-5
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
Tele mental health is promising approach to reducing
the treatment gap for isolated patients to access
mental health provider.(Hubley S,2020) Tele mental
health may be an ideal solution to reduce the risk of
clinicians or patients being infected while still
providing the treatment.6 Tele mental health is the
provison of mental and behavioral health care at
distance, including psychiatric evaluations, therapy
(individual, group, family), psychoeducation and
medication management.(Whaibeh E,2020) The
objective of the current review was to provide an
overview of scientific publication on the
effectiveness of tele mental health compared to face
to face intervention for those who are in a setting of
quarantine or isolation.
2 METHODS
2.1 Search Strategy
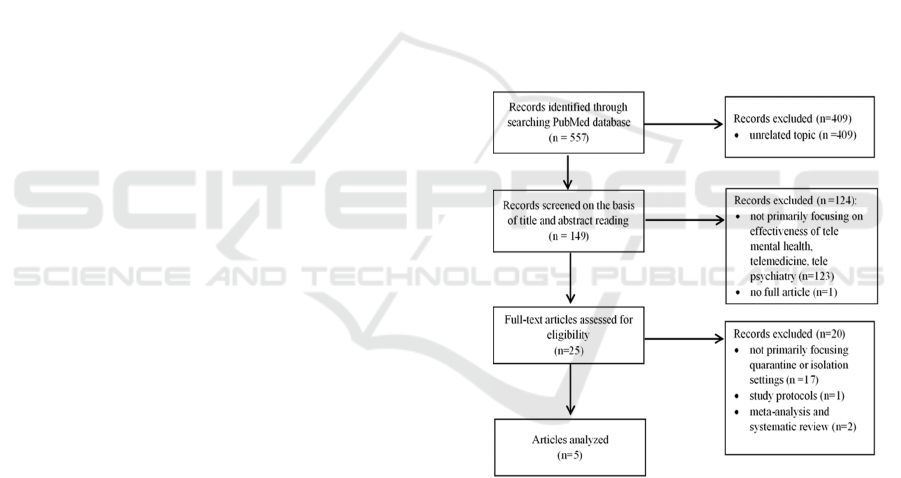
A multi-step literature search was performed. First,
systematic searches were conducted in the PubMed,
which publised between 2005 and 2020. The search
was done using the following combinations of key
terms: tele mental health effectiveness OR psychiatric
telemedicine effectiveness OR telepsychiatry
effectiveness. We searched the reference lists of
retrieved articles. Then, abstracts identified by this
process were then screened and full-text articles were
inspected against the inclusion and exclusion criteria.
Studies were eligible for inclusion when the
following criteria were fulfilled.
1. Full-text articles published in English
2. Full-text articles reporting the effectiveness of tele
mental health.
The exclusion criteria were:
1. Reviews, meta-analyses, study protocols,
abstracts and any other non-original data;
2. Lacking a clear primary focus on the effectiveness
of tele mental health in quarantine/isolation
setting.
The level of evidence of each study was
determined using the Oxford Centre for Evidence-
Based Medicine 2011 definition.(Group
OLoEW,2011)
3 RESULTS
We reviewed 5 studies that met our inclusion and
exclusion criteria. For brevity and conciseness, as
extracted from the 5 reviewed articles as follows:
Namkee G. Choi et al (2014): Objectives is to report
both depression and disability outcomes of telehealth
problem-solving therapy (tele- psychotherapy via
Skype video call) for low-income homebound older
adults over 6 months post intervention. Tele mental
Health Domain: Tele psychotherapy via Skype video
call and phone call. N Sample: 158 participants (56 in
tele-PST, 63 in in-person PST, and 39 in care call).
Study Design: (i) Randomized control trial. Outcome
Evaluation: Hamilton Rating Scale for Depression
(HAMD), (ii) WHO Disability Assessment Schedule
(WHODAS). Conclusion: Both tele psychotherapy
and in-person psychotherapy were efficacious
treatments for low-income homebound older adults;
however the effects of tele- psychotherapy on both
depression and disability outcomes were sustained
significantly longer than those of in-person
psychotherapy. Limitations of Study: The sample was
small and limited to those who were willing to be
randomized to tele-psychotherapy and to those
without cognitive deficits and other mental health
conditions. Level of Evidence is 2.
Namkee G. Choi et al (2014): Objectives is To
evaluate clinical effectiveness of a brief, aging
service–integrated, videoconferenced behavioral
activation (tele-BA) treatment delivered by lay
counselors compared with videoconferenced
problem-solving therapy (tele-PST) delivered by
licensed clinicians and attention control (AC;
telephone support calls). Tele mental Health Domain:
Videoconferencing for tele-BA and tele-PST
Telephone for attention control (AC). N Sample: 277
participants. Study Design: Randomized Clinical
Trial. Outcome Evaluation: Hamilton Rating Scale
for Depression (HAMD). Conclusion: Compared
The Effectiveness of Tele Mental Health
297

with participants in the AC group, participants in the
tele-BA and tele-PST groups had significantly higher
response and remission rates and medium to large
effect sizes. Limitations of Study: (i) All participants
resided in a single, large metropolitan area, which
may limit generalizability of the findings to non-
metropolitan areas. (ii) The lack of a longer (ie,
beyond 9 months) follow-up period. Level of
Evidence is 2.
Michelle Lampman et al (2019): Objectives is to
to examine if self-reported access to primary care is
associated with actual patient wait times and use of
telephone visits, and to assess whether this
relationship differs by rural residence. Tele mental
Health Domain: Telephone visits. N Sample: 160,447
Veterans. Study Design: Cross sectional. Outcome
Evaluation: Telephone visits Conclusion: As actual
wait time for routine appointments increases,
Veterans served by clinics with a higher percent of
rural Veterans perceive telephone visits more
positively. Limitations of Study: Not stated by
authors. Level of Evidence is 3.
Amanda K. Gilmore et al. (2019): Objectives is to
test the usability of a mobile health intervention
targeting alcohol and drug misuse, suicide
prevention, posttraumatic stress symptoms, coping
skills, and referral to formal assistance for individuals
who have experienced sexual assault. Tele mental
Health Domain By application (SC-Safe) Interviews
were conducted through teleconferencing. N Sample:
13 participants. Study Design: Qualitative study.
Outcome Evaluation: (i) Sexual Experiences Survey.
(ii) The Patient Health Questionnaire (iii).
Posttraumatic stress disorders Checklist (PCL5) (iv)
Alcohol Use Disorders Identification Test (AUDIT-
C). (v) SC-Safe questionaire about application.
Conclusion: The participants indicated that SC-Safe
would be a helpful resource for individuals who
experience sexual assault due to the pervasive barriers
that these individuals face to accessing care.
Limitations of Study: (i) The current study included a
small sample of individuals to assess initial usability
of SC-Safe (ii) Future work is needed to understand
the post-SAMFE healthcare needs of men, sexual and
gender minorities, and different racial/ethnic groups..
Level of Evidence is 3.
Choi et al (2020): Objectives is to evaluate the
acceptance and preliminary efficacy of in-home
telehealth delivery of problem-solving therapy (tele-
PST) among depressed low-income homebound older
adults in a pilot randomized control trial designed to
test its feasibility and preliminary efficacy. Tele
mental Health Domain: Videoconferencing for tele-
PST Telephone. N Sample: 121 participants. Study
Design: Randomized control trial. Outcome
Evaluation: (i) Hamilton Rating Scale for Depression
(HAMD). (ii)Treatment Evaluation Inventory (TEI)
Conclusion: Almost all participants had extremely
positive attitudes toward tele-PST at the 12-week
followup. Tele-PST also appears to be an efficacious
treatment modality for depressed homebound older
adults and to have significant potential to facilitate
their access to treatment. Limitations of Study: (i) The
study period was rather short (24 weeks), so not able
to examine the relationship between long-term
treatment outcome and the treatment modality, as
well as cost analysis of tele-PST delivery versus in-
person PST delivery. (ii)The sample was limited to
older adults without cognitive and sensory deficits.
Tele-PST for older adults with cognitive and sensory
deficits, especially auditory and visual, may not be
feasible as such deficits can impair the ability to
interact with a therapist over a videoconference
connection. Level of Evidence is 2.
4 DISCUSSION
The COVID-19 has been a global health issue since
the number of cases increases throughout out many
countries. Patients with COVID-19 should be isolated
or quarantined. This condition allows the patients
having psychological problems. Since the patients are
limited to meet people, a technological revolution in
mental health care is approaching. The use of
technology to reach populations whom to be
quarantined allows the doctor and the patient are able
to communicate without face to face.
This systematic review evaluates the effectiveness
of of tele mental health compared with face-to-face
care in regards to psychiatric services in a setting of
quarantine or isolation. This review suggests that
using tele mental health care and face-to-face care
had equivalent overall effects. Almost all of the
associated technologies can be effectively used to
treat and evaluate mental disorders without
compromising the quality of service. This review
presents its discussion under the following headings
and subheadings.
4.1 Modalities
In conducting tele mental health, there are some
technologies that can be used such as:
Videoconferencing and telephone
Videoconferencing omits presence physically
and some physical cues could not be assessed,
but overall the examiner was still able to
HIMBEP 2020 - International Conference on Health Informatics, Medical, Biological Engineering, and Pharmaceutical
298

observe the expressions of the client.
Telephone omits visual cues, but examiner was
still able to assed their expression by voices.
(Mohr D,et al.2011)
Application
Applucation in the study had some limitation in
interaction, but strengthened by interview by
videoconferencing.( Whaibeh E,et al.2020)
4.2 Isolation or Quarantine Settings
There are some situations before that resembles the
condition caused by COVID-19 like:
Homebound older
Social isolation is a state in which the
individual lacks a sense of belonging socially,
lacks engagement with others, has a minimal
number of social contacts and they are deficient
in fulfilling and quality
relationships.(Nicholson Jr NR,2009)
Sexual assault
There are several systemic (e.g., access to
services), logistical (e.g., financial constraints),
and attitudinal (e.g.,stigma, confidentiality
concerns) barriers to accessing healthcare
services immediately after sexual
assault.(Gilmore AK,2019)
Rurality
Rural residents have identified several barriers
to accessing care including distance, access to
transportation, and availability of services.
(Douthit N, 2015.) COVID‐19‐related social
isolation may be enforced by government
restrictions and/or due to an individual's fears
of infection. (Kato TA,2020) Both condition
almost similar.
4.3 Effectiveness
The advantages of tele mental health care include
improved access, reduced costs, flexibility, and
interactive sessions between clients and clinicians.(
Farrell SP,et al.2009; Tillfors M,et al.2008) Most
important things about tele mental health care are
skills to use technologies (both clinicins and clients),
good quality of equipments (both sofware and
hardware), good quality of internet services, and
evaluation of services.(Christensen H,and Hickie IB
2010) Another concerns are about marginalizing
clients with physical and cognitive disabilities who
are unable to use the equipment properly, making in-
person services as the only feasible choice.(Ybarra
ML,and Eaton WW 2005).
5 DISCUSSION
Our finding suggests that there were no significant
differences between participants receiving
telemedicine or face-to-face psychiatric services.
Tele mental health can effectively reduce psychiatric
symptoms, reduce cost. Therefore, it can be used as
an adaptable solution for COVID-19 pandemic
situation. Mental health providers providing this
service is advised to benefit from feedback collected
from clinicians and clients. Considering the potentials
of tele mental health care, further research is required
to optimize its current applications and to explore its
future promises.
REFERENCES
Chen JA, Chung W-J, Young SK, Tuttle MC, Collins MB,
Darghouth SL, et al. COVID-19 and telepsychiatry:
Early outpatient experiences and implications for the
future. General Hospital Psychiatry. 2020;66:89-95.
Choi NG, Marti CN, Bruce ML, Hegel MT, Wilson NL,
Kunik ME. Six‐month postintervention depression and
disability outcomes of in‐home telehealth problem‐
solving therapy for depressed, low‐income homebound
older adults. Depression and anxiety. 2014;31(8):653-
61.
Choi NG, Marti CN, Wilson NL, Chen GJ, Sirrianni L,
Hegel MT, et al. Effect of Telehealth Treatment by Lay
Counselors vs by Clinicians on Depressive Symptoms
Among Older Adults Who Are Homebound: A
Randomized Clinical Trial. JAMA Network Open.
2020;3(8):e2015648-e.
Christensen H, Hickie IB. Using e‐health applications to
deliver new mental health services. Medical Journal of
Australia. 2010;192:S53-S6.
Choi NG, Hegel MT, Marti CN, Marinucci ML, Sirrianni
L, Bruce ML. Telehealth problem-solving therapy for
depressed low-income homebound older adults. The
American Journal of Geriatric Psychiatry.
2014;22(3):263-71.
Coronavirus disease 2019 (COVID-19) Situation Report.
World Health Organization; 2020 (diunduh March 25,
2020). Tersedia dari:
https://www.who.int/docs/default-
source/coronaviruse/situation-reports/202AQ00324-
sitrep-64-covid-19.pdf?sfvrsn=703b2c40_2.
Ćosić K, Popović S, Šarlija M, Kesedžić I. Impact of human
disasters and Covid-19 pandemic on mental health:
Potential of digital psychiatry. Psychiatria Danubina.
2020;32(1):25-31.
Douthit N, Kiv S, Dwolatzky T, Biswas S. Exposing some
important barriers to health care access in the rural
USA. Public health. 2015;129(6):611-20.
The Effectiveness of Tele Mental Health
299

Duan L, Zhu G. Psychological interventions for people
affected by the COVID-19 epidemic. The Lancet
Psychiatry. 2020;7(4):300-2.
Farrell SP, Mahone IH, Zerull LM, Guerlain S, Akan D,
Hauenstein E, et al. Electronic screening for mental
health in rural primary care: implementation. Issues in
mental health nursing. 2009;30(3):165-73.
Gilmore AK, Davidson TM, Leone RM, Wray LB, Oesterle
DW, Hahn CK, et al. Usability testing of a mobile
health intervention to address acute care needs after
sexual assault. International journal of environmental
research and public health. 2019;16(17):3088.
Group OLoEW. " The Oxford 2011 Levels of Evidence."
Oxford Centre for Evidence-Based Medicine.
http://www cebm net/index aspx? o= 5653. 2011.
Health UDo, Services H. Secretary Azar declares public
health emergency for United States for 2019 novel
coronavirus. 2020 Jan 31. 2020.
Hubley S, Lynch SB, Schneck C, Thomas M, Shore J.
Review of key telepsychiatry outcomes. World Journal
of Psychiatry. 2016;6(2):269.
Kato TA, Sartorius N, Shinfuku N. Forced social isolation
due to COVID‐19 and consequent mental health
problems: Lessons from hikikomori. Psychiatry and
clinical neurosciences. 2020.
Lampman M, Stockdale S, Kaboli PJ, Jaske E, Wood GB,
Clinton WL, et al. The effects of telephone visits and
rurality on veterans perceptions of access to primary
care. The Journal of the American Board of Family
Medicine. 2019;32(5):749-51.
Mark É. Czeisler; Rashon I. Lane MEP, MD; Joshua F.
Wiley, PhD; Aleta Christensen, MPH; Rashid Njai,
PhD; Matthew D. Weaver, PhD; Rebecca Robbins,
PhD; Elise R. Facer-Childs, PhD; Laura K. Barger,
PhD; Charles A. Czeisler, MD, PhD; Mark E. Howard,
MBBS, PhD; Shantha M.W. Rajaratnam, PhD. Mental
Health, Substance Use, and Suicidal Ideation During
the COVID-19 Pandemic. United States: CDC; 2020.
Mohr D, Cuijpers P, Lehman K. Supportive accountability:
a model for providing human support to enhance
adherence to eHealth interventions. Journal of medical
Internet research. 2011;13(1):e30.
Moring JC, Dondanville KA, Fina BA, Hassija C, Chard K,
Monson C, et al. Cognitive Processing Therapy for
Posttraumatic Stress Disorder via Telehealth: Practical
Considerations During the COVID‐19 Pandemic.
Journal of Traumatic Stress. 2020.
Nicholson Jr NR. Social isolation in older adults: an
evolutionary concept analysis. Journal of advanced
nursing. 2009;65(6):1342-52.
Tanielian TL, Tanielian T, Jaycox L. Invisible wounds of
war: Psychological and cognitive injuries, their
consequences, and services to assist recovery.Rand
Corporation; 2008.
Tillfors M, Carlbring P, Furmark T, Lewenhaupt S, Spak
M, Eriksson A, et al. Treating university students with
social phobia and public speaking fears: Internet
delivered self‐help with or without live group exposure
sessions. Depression and Anxiety. 2008;25(8):708-17.
Whaibeh E, Mahmoud H, Naal H. Tele mental Health in the
Context of a Pandemic: the COVID-19 Experience.
Current Treatment Options in Psychiatry. 2020:1-5.
Ybarra ML, Eaton WW. Internet-based mental health
interventions. Mental health services research.
2005;7(2):75-87.
HIMBEP 2020 - International Conference on Health Informatics, Medical, Biological Engineering, and Pharmaceutical
300
