
Doctor's Leadership Style and Nurse Performance in Inpatient Room
Sudiarto, Ermi Girsang*, Ali Napiah Nasution
Faculty of Medicine, Prima Indonesia University
Keywords: Doctor's leadership style, executive nurse performance.
Abstract: The relationship between doctors and nurses in providing health care to patients is a more binding
partnership where there should be harmonization of tasks, roles and responsibilities and an open system. To
manage the implementation of health services, especially nursing, of course it takes a doctor's leadership
factor which in its application can have an impact on nurses' performance. The fact that in the application of
nursing care the role of doctors as clinical leaders is less assertive which has an impact on the performance
of nurses that is not yet optimal. This study analyzes the influence of the doctor's leadership style on nurses'
performance in the inpatient room. This type of quantitative research is analytic descriptive approach. The
number of samples were 38 nurses. Data collection is carried out through questionnaires and documentation
studies. The questionnaires were conducted in face-to-face with the participants in order to maintain the
validity of the research. Data were analyzed bivariately using chi square test and multivariate using multiple
logistic regression tests. The results of the study show that democratic leadership style, participatory,
authoritarian and Laissez-faire leadership style significantly influence the performance of the nurses. The
independent leadership style variable is the most dominant influencing the performance of the implementing
nurse. The results of this study are expected to be useful information and suggestions for hospital
management by involving the larger functions of doctors in governance and management. It is hoped that
the improvement of doctors' leadership abilities will have a direct impact on improving the performance of
nurses.
1 INTRODUCTION
Health and care professionals not only require
clinical experts but also have competence in
leadership and management skills that enable them
to be more actively involved in the planning,
delivery and transformation of services for patients.
To make a change that actually takes place in
achieving its goals, leadership is needed. There are
many examples of bad practice and system failure in
health care due to lack of leadership at the
individual, group and organizational level (Salim,
2016).
Greater doctor participation at the level of
strategic decision making has the potential to benefit
various hospitals. Greater doctor involvement is
beneficial for the decision-making process in the
hospital and has important implications for policy
and practice (Sarto and Veronesi, 2016).
The competence of doctors as leaders in health
services in hospitals, often referred to as clinical
leaders. For health care workers, especially doctors,
the leadership factor is needed in carrying out daily
tasks. The main task of the doctor is to lead the
health care technical team and in every medical
treatment certainly involves many parties ranging
from nurses, nutrition installations, medical records,
the availability of facilities and infrastructure and
doctors. Clinical leadership is a driver of efforts to
develop a vision of clinical services in hospitals. The
creation of a world-class clinical vision and
achievement strategy is a practical example of
clinical leadership in hospitals. But being a clinician
may not necessarily have clinical leadership
abilities. Given the large variety of professions in
hospitals and the complexity of hospital organization
management, this situation will prevent clinicians
from developing leadership abilities. The situation
will become even more difficult due to autonomy in
each profession, a hierarchy of competencies, and a
high workload (Trisnantoro et al., 2011).
In the case of health workers, of course the
highest number of personalities and the most
frequently dealing with patients served are nurses.
Data from the Ministry of Health showed the largest
number of nurses in 2016 among other health
Sudiarto, ., Girsang, E. and Nasution, A.
Doctor’s Leadership Style and Nurse Performance in Inpatient Room.
DOI: 10.5220/0010293302210228
In Proceedings of the International Conference on Health Informatics, Medical, Biological Engineering, and Pharmaceutical (HIMBEP 2020), pages 221-228
ISBN: 978-989-758-500-5
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
221

professions, 345,276 people or 30.19% of the total
recapitulation of health professionals in Indonesia,
namely 1,143,494 people. To manage the
implementation of health services, especially
nursing, of course it takes leadership factors from
doctors who in their application can have an impact
on nurse performance. Therefore, this research is
conducted on nurses because they are closely related
to doctors and patients and they also provide
services according to the doctors’ suggestions and
nursing intakes. The good performance of nurses is a
bridge in answering quality assurance of health
services provided to both sick and healthy patients,
health service facilities including hospitals (Ministry
of Health, 2018; Turnip, 2020; Wijaya, 2019).
The relationship between doctors and nurses in
providing health care to patients is a more binding
partnership where there should be harmonization of
tasks, roles and responsibilities and an open system.
According to the AMA, if collaboration between
doctors and nurses goes as determined it will have a
direct impact on patients, because many positive
aspects can be generated. In fact, in practice there
are various obstacles to collaboration between
doctors and nurses so that collaboration is difficult
to be created, among others, the dominance of
power, differences in the level of knowledge /
education, communication and perspective
(Rahaminta and Sulisno, 2012).
The main key in improving the quality of health
services is nurses who have high performance.
However, it is not uncommon to find complaints
related to the quality of health services which
originates from the performance of nurses. Even
criticism of nurses' performance in providing
services is often complained of and has often been
published in the mass media. It was reported that
there were nurses in the hospital saying harshly to
patients when serving health checks, nurses were not
responsive in providing services, and nurses were
less friendly to patients (Nurjannah, 2016).
Criticism or complaints regarding nurses'
performance can be minimized by taking into
account the factors that can influence them.
According to Ilyas, the factors that influence works
behavior and performance are individual,
organizational, and psychological variables. The
individual variables consist of abilities, skills,
background and demographics. The organizational
variables consist of resources, leadership, rewards,
structure and job design. The psychological
variables consist of perception, attitude, personality,
learning and motivation (Ilyas, 2016). One factor
related to the performance of organizational
variables is leadership. In this study limited to
clinical leadership of doctors (clinical leadership).
National Health Service (NHS) highlights the
importance of effective leadership in the system
especially the need to involve more doctors in the
leadership. Health and care professionals not only
require clinical experts but also have competence in
terms of leadership and management skills that
enable them to be more actively involved in
planning, delivering and transforming services for
patients and to make a change that actually happens,
requires leadership . There are many examples of
bad practice and system failure in health care due to
lack of leadership at the individual, group and
organizational level (NHS Leadership Academy,
2012).
Including leadership and management aspects in
the health service system on a team, department,
hospital or government scale in the health sector is
not an option, but an obligation for all clinicians.
This leadership is manifested through various types
of leadership styles. Leadership style is a way of
working and behaving leaders in guiding their
subordinates to do something (Kartono, 2014).
Given global trends, such as an aging population
and rapid adoption of new technologies, the way in
which health care is delivered has changed
substantially in the past 10 years, which in turn
brings the need for new ways to lead the health care
team. For this reason, a leadership style that is
focused on creating positive relationships is
associated with higher patient satisfaction, and
reducing patient mortality, medication errors, use of
controls and hospital-acquired infections.
Several factors that can affect one's leadership
style include many aspects, such as psychological,
sociological, cultural, political, historical,
geographical, technical, and economic aspects.
Based these factors it is very possible if the
leadership style in one country will also be different
from other countries, such as in two different
countries: leaders from different regions will also
give a difference in the leadership style. This
becomes a characteristic that grows and develops
closely related to a person's background and how the
values are instilled when he grows and grows older,
until finally becoming a leader (Laurent and
Djastuti, 2013).
Studies of the leadership style and its influence
on the work results or performance of its members
have been widely carried out. Tewal's research
found that there was a positive and significant
influence between organizational culture, leadership,
and motivation on nurse performance.
HIMBEP 2020 - International Conference on Health Informatics, Medical, Biological Engineering, and Pharmaceutical
222

Simultaneously that organizational culture,
leadership, and motivation significantly influence
nurse performance (Tewal, Mandey and Rattu,
2017). The difference with others, this research is
only focuses on leadership style.
Haan in his research found that there was a
relationship between leadership style (authoritarian,
democratic, participatory, liberal) and the work
motivation of nurses (de Haan, P.L.M., BitjuniH.J.
Kundre, 2019). The difference with this study is that
the dependent variable Haan examines nurses' work
motivation while this study examines the
performance variables of nurses implementing
inpatient rooms. Moura in his research found that
nursing leadership has a positive and significant
impact on job satisfaction (Moura et al., 2017). The
difference with this research is that the dependent
variable Moura examines nurse job satisfaction.
Duwayri explained that to achieve the highest level
of staff satisfaction nurse managers need to use
several leadership styles, which are relational
focused on transformational and transactional styles
(Duwayri, 2019). Research conducted by Artiningsih
found that the leadership style and motivation of the
head of the room had no significant effect on nurse
performance while discipline had a significant and
dominant effect on nurse performance (Artianingsih,
2016). Suratno's research found that leadership
strategies are very important to enhance the role of
nurses where leaders can form an effective work
environment for nurses and improve the quality of
service to patients. Health institutions must create a
healthy work environment that benefits nurses and
patients, monitors well-being and promotes healthy
behaviors to nurses (Suratno, Ariyanti and Kadar,
2018).
Goh's research found that nurse leaders in this
study tended to rate themselves higher than others.
The results imply the need to include self-awareness
elements in nursing leadership development
programs (Goh, Ang and Della, 2018). The
difference with this research is that the independent
variable besides Goh leadership style also examines
the organizational commitment variable. Overall
research focusing on leadership style and quality of
nurse performance (based on several previous
studies, these two factors are the most dominant in
improving the quality of service in a hospital) which
is still rarely done before.
2 METHODOLOGY
The study was conducted in the inpatient room at
Royal Prima Hospital Medan in August-December
2019. The hospital has implemented a modern
service system in the form of an integrated
computerized information system. The population
was 319 nurses implementing inpatient wards with a
sample of 76 respondents by random sampling
technique. Data collection was done by distributing
questionnaires containing 8 items each statement
about the leadership style of doctors (democratic,
participatory, authoritarian, and Laissez-faire) with
alternative answers Yes given a score of 3,
Sometimes given a score of 2, Not given a score of 1
and 20 statement items about the performance of the
implementing nurse with alternative answers Yes
given a score of 3, Rarely given a score of 2, Not
given a score of 1.
Validity and reliability tests were carried out on
30 nurses implementing at the same hospital as the
study location. The validity test results obtained
Rcount coefficient values in the range 0.393-0.749>
Rtable = 0.361, it was assumed that the data was
normally distributed. The reliability test results
obtained Cronbach's Alpha count values in the range
0.834-0.892> 0.7; assumed a reliable questionnaire.
Questionnaires were distributed in the second and
third week of December.
Data processing through the Editing stage: to
check the suitability of the data with expectations
and check the completeness and uniformity of the
data. Coding: to simplify the analysis and also to
speed up data entry. Processing: done after all
variables are coded. Data that has been given a code
is then entered first in the master table. Cleaning:
this process aims to ensure that the data that has
been entered is really clean from errors. Data were
bivariately analyzed using the chi square statistical
test and multivariate with multiple logistic
regression tests. The research process scheme is
given as in Figure1.
Doctor’s Leadership Style and Nurse Performance in Inpatient Room
223
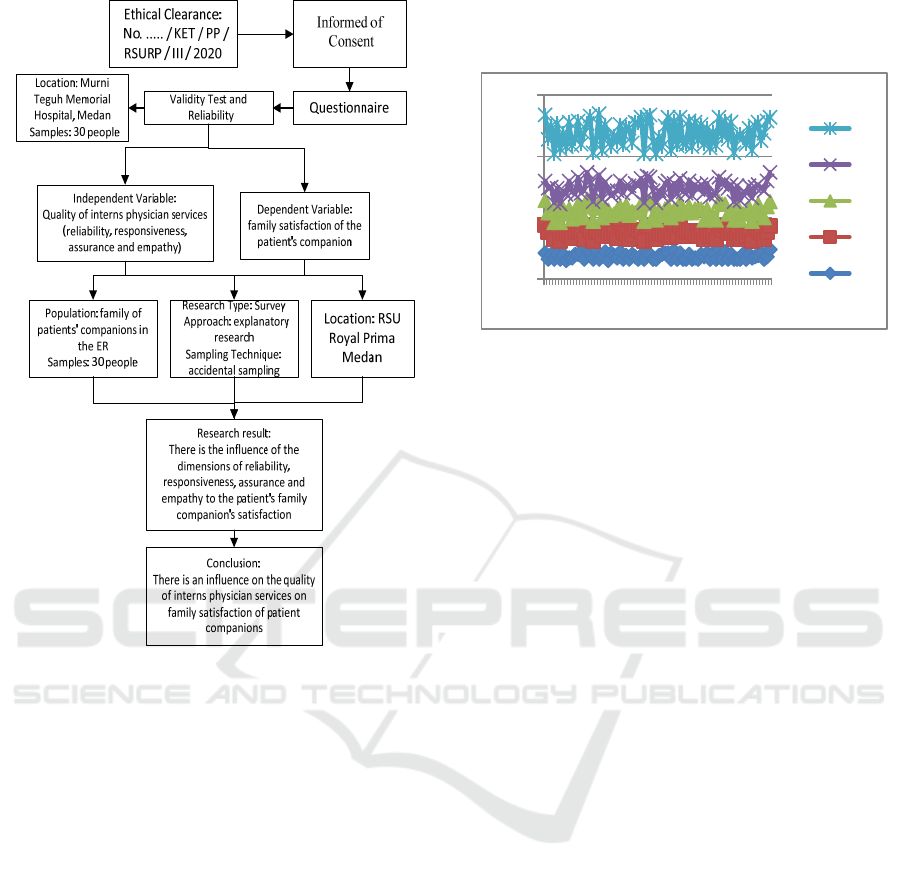
Figure 1. Scheme of Leadership Style and Nurse
Performance Research
3 RESULTS AND DISCUSSION
Analysis of the research questionnaire based on
dummy categories (2 groups) with a mean or
average = 1.50; where all the variables above the
average are democratic (1.62); participatory (1.67);
authoritarian (1.55); free of action (1.54) and nurse
performance (1.57). The results of the measurement
of the research variable from the questionnaire as in
Figure 1 and Table 1. Figure 1 indicate the form and
data distribution value of each evaluated variables.
The measured data distribution for independent and
dependent variables can be seen in Figure 2.
In
Figure 2, D is Democratic, P is Participatory, A is
Authoritarian, F is Laissez-faire / Free action, and N is
Nurse Performance.
Based on the assessment of the implementing
nurses, there are still doctors who do not apply a
democratic leadership style (38.2%). This is evident
from the answers of implementing nurses that some
doctors in determining action plans to patients do
not always ask for ideas from implementing nurses
and do not respect the nature of implementing nurses
in carrying out health service tasks.
Figure 1: The measured data from questionnaire of 76
respondents.
The results of multiple logistic regression tests
on the doctor's democratic leadership style obtained
value of the regression coefficient = 1.714; p =
0.008 with the value Exp (B) = 5.553. This means
that the respondents considered that the democratic
leadership style applied by doctors was good, had a
5.553 times greater chance of carrying out tasks with
good categories compared to respondents who rated
the leadership style as not good.
A study conducted by Tewal found that there
was a significant positive effect between
organizational culture, leadership, and motivation on
nurse performance. Simultaneously that
organizational culture, leadership, and motivation
significantly influence nurse performance (Tewal,
Mandey and Rattu, 2017).
Human resource management in a hospital
requires the right leadership style so that it can form
a synergy between superiors and subordinates (in
this study between doctors and implementing
nurses). With the application of appropriate
leadership styles, it is expected that a harmonious
communication relationship between doctors and
nurses implementing in improving the performance
of health services to patients will be better.
Doctors who apply the majority participatory
style tend to carry out tasks in either category and
not vice versa. Chi square statistical test results
obtained p value (0.001) < (0.05) means that there
is a relationship between the participative leadership
style of the doctor and the task of the implementing
nurse.
The results of multiple logistic regression tests
on the physician participatory leadership style
obtained the value of the regression coefficient =
1.804; p = 0.008 with the value Exp (B) = 6.073.
0
50
100
150
1 8 152229364350576471
N
F
O
P
D
HIMBEP 2020 - International Conference on Health Informatics, Medical, Biological Engineering, and Pharmaceutical
224
This means that respondents who rated the
participatory leadership style that doctors applied
were good, 6.073 times more likely to carry out
tasks in a good category compared to respondents
who rated the participative leadership style that
doctors applied was not good.
Nurses who state that doctors apply the majority
authoritarian style carry out tasks in either category
and those who declare doctors do not apply the
majority authoritarian style carry out tasks in the less
good category. Chi square statistical test results
obtained p value (0.002) < (0.05) means that there
is a relationship between the authoritarian leadership
style of the doctor and the performance of the
implementing nurse.
The results of multiple logistic regression tests
on the doctor's authoritarian leadership style
obtained the value of the regression coefficient =
1.937; p = 0.004 with the value of Exp (B) = 6.936
This means that respondents who rated the
authoritarian leadership style applied by doctors
were good, had a 6.936 times greater chance of
carrying out tasks in a good category compared to
respondents who assessed the authoritarian
leadership style applied by doctors was not good.
Nurses who state that doctors apply the laissez-
faire, the majority carry out tasks by category and
who state the doctor does not apply the freestyle act,
the majority carry out tasks with unfavorable
categories. Chi square statistical test results obtained
the value of p (0,000) < (0.05) means there is a
relationship between the free leadership style of
doctors' actions with the performance of the
implementing nurses.
The results of the multiple logistic regression test
on the doctor's free leadership style obtained a
regression coefficient of 1.804; p = 0.008 with the
value of Exp (B) = 6.073. This means that
respondents who judge doctors to adopt a free
leadership style of action as well, have a 6.073 times
greater chance of carrying out tasks in a good
category compared to respondents who judge the
leadership-free style of action that doctors apply is
not good.
From the results of the multivariate test in Table
2 it can be concluded that the leadership style of
Authoritarian is the dominant variable influencing
the performance of nurses implementing inpatient
rooms. This is evidenced from the coefficient value
of the Laissez-faire leadership style (1.804) higher
than the democratic leadership style (1.714), from
the participative leadership style (1.350) More
clearly as in Tables 2 and 3.
Table 1: Chi square test results (Bivariate Analysis).
Leadership
Nurse Performance
p-
value
Good
Not Good
n % n %
Democratic
Applied 35 74,5 12 25,5 0,000
Not 8 27,6 21 72,4
Participatory
Applied 36 70,6 15 29,5 0,001
Not 7 28,0 18 72,0
Authoritarian
Applied 31 73,8 11 26,2 0,002
Not 12 35,3 22 64,7
Laissez-faire
Applied 32 78,0 9 22,0 0,001
Not 11 31,4 24 68,6
Table 2: Results of multiple logistic regression tests
(Multivariate Analysis).
Variables B Wald
d
f
Sig.
Exp
(B)
Democratic 1,714 7,024 1 0,008 5,553
Laissez-faire
1,804 6,988
1
0,008 6,073
Participatory
1,350 4,290
1
0,038 3,857
Authoritarian
1,937 8,401
1
0,004 6,936
Constant -3,196
17,205
1
0,000 0,041
In Trisnantoro's research, it is explained the
influence of various models or styles of doctor
leadership on the performance of implementing
nurses. Hospital core business is clinical services.
Patients and their families come to the hospital to get
clinical services from the health workers who work
in it. Health workers who work in hospitals consist
of various professions and each profession has a
diverse hierarchy of competencies. The large
number of variations is a barrier for the
implementation of services oriented to patient safety
and satisfaction, if there is no leadership that unites
the vision of service from these various professions.
For this reason, leadership is needed to build a spirit
of togetherness through shared vision and shared
values in the service mechanism in hospitals
(Trisnantoro et al., 2011). Much researched
assumptions indicate that greater physician
involvement in governance and management roles
Doctor’s Leadership Style and Nurse Performance in Inpatient Room
225

will have broader benefits for the efficiency and
effectiveness of health care organizations.
The results showed that there was an influence of
the doctor's democratic leadership style on the
performance of nurses implementing inpatients. The
statement of implementing nurses in general is that
doctors adopt a democratic leadership style (61.8%).
This is evident from the statement of implementing
nurses, among others, that doctors value the ability
of each implementing nurse in providing health
services; the doctor gives an explanation of the
implementation of nursing actions to the
implementing nurse openly; if there is a planning of
a new method for administering an action, the doctor
provides the widest possible information; and
doctors help implementing nurses in solving
problems related to the implementation of health
services.
Based on the results of multiple logistic
regression tests, the value of p 0.008 <0.05 means
that there is an influence of the democratic
leadership style of the doctor on the performance of
the executing nurse. In other words the more
democratic leadership styles are applied by doctors,
the task of implementing nurses also increases. But
there are still nurse nurses with poor performance,
this can be caused by a less supportive work
environment such as conditions when the patient is
busy, the nurse's workload is high, and the number
of nurses is still less compared to the number of
patients who must be served.
The results showed that there was an influence of
the physician participatory leadership style on the
performance of nurses implementing inpatient
rooms. This is based on the statement of the
implementing nurse who in general doctors apply a
participative leadership style (67.1%). This is
evident from the statement of the implementing
nurse which among others is that if there is a
planning of a new method in the delivery of health
services or actions, the doctor proposes to the
implementing nurse; the doctor gives direction to the
implementation of the duties of the implementing
nurse clearly; doctors appreciate the ability of
implementing nurses in carrying out health service
tasks; and doctors consider the results of the analysis
of the problem of implementing nurses related to
problems in the implementation of health services.
Based on the results of multiple logistic
regression tests, the value of p 0.008 <0.05 means
that there is an influence of the participative
leadership style of the doctor on the task of the
nurses implementing the inpatient room. In other
words the more applied the participatory leadership
style by doctors, the task of implementing nurses
also increased. But there are still nurses with poorly
performing tasks, this can be caused by a less
supportive work environment such as conditions
when the patient is crowded, the workload of nurses
is high, and the number of nurse nurses is still
insufficient compared to the number of patients who
must be served.
Based on the assessment of the executive nurse
that there were doctors who did not apply the
participative leadership style (32.9%) it was proven
that the nurse's response was that in determining the
action plan to the patient, the doctor did not always
ask for advice from the implementing nurse and
likewise in determining the purpose of the action on
the patient, the doctor makes his own decision
before proposing to the implementing nurse.
The results showed that there was an influence of
the doctor's authoritarian leadership style on the
performance of nurses implementing inpatients. The
statement of the implementing nurse generally states
that the doctor applies an authoritarian leadership
style (71.7%). This is evident from the statement of
implementing nurses, among others, that doctors
provide information only limited to the importance
of the task to the implementing nurse; the doctor
uses full authority in assigning duties to the
implementing nurse; and doctors crack down on
implementing nurses who violate the provisions of
the actions they provide. Based on the results of
multiple logistic regression tests the p value of 0.038
<0.05 means that there is an influence of the
authoritarian leadership style of the doctor on the
task of the implementing nurse in the inpatient room.
In other words the more authoritarian leadership
styles applied by doctors, the task of implementing
nurses also increases.
Ilyas states that theoretically there are three
groups of variables that affect performance, one of
which is an organizational variable with subvariable
leadership (Ilyas, 2016). In this case, what is meant
is the leadership of the doctor as the decision maker
as well as the person in charge of health measures
given to patients who in practice collaborate with
nurses. The American Medical Association
interprets collaboration between doctors and nurses,
the process by which doctors and nurses plan and
practice together as colleagues, working
interdependently within the boundaries of their
practice by sharing values and mutual recognition
and respect for everyone who contributes to caring
for individuals. , family and community (Rahaminta
and Sulisno, 2012).
HIMBEP 2020 - International Conference on Health Informatics, Medical, Biological Engineering, and Pharmaceutical
226

The results showed that there was an influence of
the doctor's Laissez-faire leadership style on the
performance of nurses implementing inpatients. This
is based on the statement of the implementing nurse
that in general doctors do not adopt a leadership
style that is free of action (53.9%). Evidenced by the
statement of the executing nurse, the majority said
no to the statement that in determining the action
plan to the patient, the doctor handed over to the
implementing nurse; doctors control the
implementation of actions to patients by nurses at a
minimum; and doctors rarely coordinate
implementing nurses in carrying out their duties.
Based on the results of multiple logistic regression
tests, the value of p 0.004 <0.05 means that there is
an influence of the Laissez-faire leadership style on
the performance of implementing nurses. In other
words the more authoritarian leadership styles
applied by doctors, it tends to affect the task of
implementing nurses. Based on the results of the
multiple logistic regression tests the four democratic
leadership style variables have an exponent value of
5.553; participatory leadership style has a coefficient
value of 3.857; authoritarian leadership style has a
coefficient value of 6.936; and the Laissez-faire
leadership style has a coefficient value of 6.073.
Of the four independent variable exponent
values, it is seen that the authoritarian variable has a
higher value, in other words the Laissez-faire
variable is the most dominant influencing the
performance of the implementing nurse.This
because doctors generally serve many patients so
that. So there is a tendency for doctors not to
coordinate or in other words tend to give freedom to
other implementing nurses to take actions and
decisions individually related to the provision of
health services in the inpatient room.
Management of human resources in a hospital
requires the right leadership style so that it can form
a synergy between superiors and subordinates in this
study are doctors and nurses implementing. With the
application of the right leadership style, it is
expected that there is a harmonious communication
relationship between doctors and nurses
implementing in improving the performance of
nursing care services to patients.
Some of the results of previous studies that are in
line with this study are Moura who found that
nursing leadership has a positive and significant
impact on job satisfaction (Moura et al., 2017).
Artiningsih's research found that the leadership style
of the head of the room was influential but not
significant to the performance of nurses in Brigjend
H. Hasan Basry Kandangan Hospital (Artianingsih,
2016). Research Naseem et al. find the
transformational style of the leader to achieve a
statistically optimal nurse presentation statistically
significant effect on the level of job satisfaction of
nurses (Naseem et al., 2018).
Sfantou et al.'s study found that leadership style
plays an integral role in increasing quality measures
in health care and nursing (Sfantou et al., 2017). Al-
Yami's research found a significant relationship
between nurses' organizational commitment in
relation to transformational leaders, showing staff
becoming more committed to the hospital when a
manager displays transformational leadership
characteristics (Al-Yami, Galdas and Watson, 2018).
Research by Fatimah et al. Found that there was a
significant leadership effect on nurse job satisfaction
(Fatimah, Wahyuni and Widjasena, 2016). The
results of the study are contrary to the results of this
study, namely Ibrahim et al. Which found that no
statistically significant relationship was found
between leadership style and nurse performance
(Ibrahim, Sanaa Abd El-Azim., El Sayed, Rasha
Ibrahim., Attala, Magdy Mamdouh & Elmezin,
2016).
The provision of nursing services is a complex
activity and involves various individuals. In order to
achieve the nursing goals, activities required to
apply leadership skills. Therefore, leadership arises
as a synergistic result of various skills ranging from
administrative (planning, organizing, controlling,
controlling), technical skills (management,
marketing, and procedural technical), and
interpersonal skills (Subanegara, 2005).
4 CONCLUSIONS
Modeling results show that the regression coefficient
value (r = 1.714: p = 0.008); participatory (r = 1.804:
p = 0.008); authoritative (r = 1.350: p = 0.038); and
laissez-faire (r = 1.937: p = 0.004) on performance.
The conclusion of this study is that the doctor's
leadership style has a significant effect on the nurse's
performance and the laissez-faire style is the
dominant factor. Doctors should avoid applying the
Laissez-faire leadership style because this variable
has the most dominant influence on the nurse's
performance. Implementing nurses should strive to
improve the duties of nursing care as best as
possible.
Doctor’s Leadership Style and Nurse Performance in Inpatient Room
227

REFERENCES
Al-Yami, M., Galdas, P. and Watson, R. (2018)
‘Leadership style and organisational commitment
among nursing staff in Saudi Arabia’, Journal of
Nursing Management, 26(5), pp. 531–539. doi:
10.1111/jonm.12578.
Artianingsih, D. W. (2016) ‘Pengaruh Gaya
Kepemimpinan Kepala Ruangan, Motivasi dan
Disiplin Terhadap Kinerja Perawat Di Rumah Sakit
Umum Daerah (RSUD) Brigjend H. Hasan Basry
Kandangan Kalimantan Selatan’, Dinamika Ekonomi:
Jurnal Ekonomi dan Bisnis, 9(1), pp. 87–104.
de Haan, P.L.M., BitjuniH.J.Kundre, R. (2019) ‘Gaya
Kepemimpinan Dengan Motivasi Kerja Perawat Di
Rumah Sakit Jiwa’, Jurnal Keperawatan, 7(2), pp. 1–7.
Duwayri, T. S. (2019) ‘Leadership Styles of Nurse
Managers/Leaders and Staff Nurses Job Satisfaction
and Outcome Pattern in Workforce: A Systematic
Review’, 8(2), pp. 1–24. doi: 10.9790/1959-
0802080124.
Fatimah, R., Wahyuni, I. and Widjasena, B. (2016)
‘Pengaruh Kepemimpinan Dan Motivasi Kerja
Terhadap Kepuasan Kerja Perawat Rawat Jalan
Rumah Sakit Islam Harapan Anda Tegal’, Jurnal
Kesehatan Masyarakat (e-Journal), 4(3), pp. 614–622.
Goh, A. M. J., Ang, S. Y. and Della, P. R. (2018)
‘Leadership style of nurse managers as perceived by
registered nurses: A cross-sectional survey’,
Proceedings of Singapore Healthcare, 27(3), pp. 205–
210. doi: 10.1177/2010105817751742.
Ibrahim, Sanaa Abd El-Azim., El Sayed, Rasha Ibrahim.,
Attala, Magdy Mamdouh & Elmezin, N. K. (2016)
‘Relationship between Head Nurses’ leadership styles
and Staff Nurses’ job performance’, Journal of
Nursing and Science (IOSR-JHNS), 5(1), pp. 66–74.
doi: 10.9790/1959-05146674.
Ilyas, Y. (2016) Kinerja: Teori, Penilaian dan Penelitian.
Jakarta: Pusat Kajian Ekonomi Kesehatan FKM
Universitas Indonesia.
Kartono, K. (2014) Pemimpin dan Kepemimpinan.
Jakarta: PT. Raja Grafindo Persada.
Kementerian Kesehatan (2018) Profil Kesehatan Indonesia
2017. Jakarta.
Laurent, M. and Djastuti, I. (2013) ‘Resep Kepemimpinan
Sang Dokter Bandeng (Fenomenologi Gaya
Kepemimpinan dr. Daniel Nugroho S. di Bandeng
Juwana Grup)’, Jurnal Studi Manajemen &
Organisasi, 10(1), pp. 60–74. doi:
10.14710/jsmo.v10i1.5577.
Moura, A. A. de et al. (2017) ‘Liderança e satisfação no
trabalho da enfermagem: revisão integrativa’, Acta
Paulista de Enfermagem, 30(4), pp. 442–450. doi:
10.1590/1982-0194201700055.
Naseem, S. et al. (2018) ‘Relationship between Leadership
Styles of Nurse Managers and Staff Nurses Job
Satisfaction in Public Hospital of Punjab, Pakistan’,
International Journal of Social Sciences and
Management, 5(3), pp. 201–208. doi:
10.3126/ijssm.v5i3.20611.
NHS Leadership Academy (2012) Clinical Leadership
Competency Framework: Self assessment tool. United
Kingdom: NHS Leadership Academy.
Nurjannah (2016) Pengaruh Gaya Kepemimpinan Kepala
Ruangan terhadap Kinerja Perawat Pelaksana di
Ruang Rawat Inap Rumah Sakit Umum Daerah
(RSUD) Tgk Chik Ditiro Sigli. Universitas Sumatera
Utara.
Rahaminta, B. and Sulisno, M. (2012) ‘Pengalaman
Perawat Berkolaborasi Dengan Dokter Di Ruang
ICU’, Journal of Nursing, 1(1), pp. 74–80.
Salim, N. A. (2016) Instrumen Penilaian Kompetensi
Clinical Leadership, Mutu Pelayanan Kesehatan.
Sarto, F. and Veronesi, G. (2016) ‘Clinical leadership and
hospital performance: Assessing the evidence base’,
BMC Health Services Research. BMC Health Services
Research, 16(2). doi: 10.1186/s12913-016-1395-5.
Sfantou, D. et al. (2017) ‘Importance of Leadership Style
towards Quality of Care Measures in Healthcare
Settings: A Systematic Review’, Healthcare, 5(4), p.
73. doi: 10.3390/healthcare5040073.
Subanegara, H. P. (2005) Diamond Head Drill &
Kepemimpinan dalam Manajemen Rumah Sakit.
Yogyakarta: Andi Publisher.
Suratno, K., Ariyanti, S. and Kadar, I. (2018) ‘The
Relationship between Transformational Leadership
and Quality of Nursing Work Life in Hospital’,
International Journal of Caring Sciences, 11(3), pp.
1416–1422. Available at:
www.internationaljournalofcaringsciences.org.
Tewal, F. S., Mandey, S. L. and Rattu, A. J. M. (2017)
‘Analisis Pengaruh Budaya Organisasi,
Kepemimpinan, Dan Motivasi Terhadap Kinerja
Perawat Rumah Sakit Umum Daerah Maria Walanda
Maramis Minahasa Utara’, Jurnal EMBA: Jurnal Riset
Ekonomi, Manajemen, Bisnis dan Akuntansi, 5(3), pp.
3744–3753.
Trisnantoro, L. et al. (2011) Clinical Leadership.
Universitas Gadjah Mada. doi: 10.1016/B978-0-7020-
4344-4.00003-1.
Turnip, A., Andrian, Turnip, M., Dharma, A., Paninsari,
D., Nababan, T., Ginting, C.N., 2020. An application
of modified filter algorithm fetal electrocardiogram
signals with various subjects, International Journal of
Artificial Intelligence, vol. 18, no., 2020.
Wijaya ,C., Andrian, M., Harahap, M., Turnip, A., 2019.
Abnormalities State Detection from P-Wave, QRS
Complex, and T-Wave in Noisy ECG, Journal of
Physics: Conference Series, Volume 1230, (2019)
012015. doi:10.1088/1742-6596/1230/1/012015.
HIMBEP 2020 - International Conference on Health Informatics, Medical, Biological Engineering, and Pharmaceutical
228
