
Personnel Characteristics and Comprehensiveness of Hospital on
Handwashing Compliance
Robert Komaria, Ermi Girsang, Ali Napiah
Faculty of Medical, Universitas Prima Indonesia, Indonesia
Keywords: Personnel Characteristics, Role of PIC, Comprehensiveness, Handwashing.
Abstract: The results of the 2018 prevention of infection control (PIC) committee regarding compliance with the
application of hand washing by doctors 53.3%, nurses 47.9% and other health workers 35.6% against a
minimum service standard of 85%. This condition is thought to be caused by individual characteristics and
hospital completeness (the role of PIC, and completeness of facilities and infrastructure). The purpose of this
study was to analyse the relationship between individual characteristics, the role of PIC and the completeness
of facilities and infrastructure to nurse compliance in the application of hand washing. This research was
conducted through a cross sectional survey approach with a population of 113 nurses with simple random
sampling technique. Data were collected through questionnaires and analysed with univariate, bivariate and
multivariate (using multiple logistic regression) methods. The results of the study of nurses less adherent to
washing their hands 64.6% and 35.4% obedient. Individual characteristics (knowledge p = 0.003 and attitude
p = 0.002), the role of PPI (p = 0.002), and completeness of facilities and infrastructure (p = 0.017) were
related to the compliance of nurses washing hands. It can be concluded that individual characteristics, the role
of PPI, and the completeness of facilities and infrastructure were an essential factors in improving compliance
with the implementation of hand hygiene.
1 INTRODUCTION
Healthcare Associated Infections (HAIs) are
infections in patients who have not been seen or are
not incubating when the patient first enters or occurs
during a patient being hospitalized for more than 48
hours, which does not appear at the time of hospital
admission or health care others (WHO, 2010).
The results of surveillance of infectious diseases
resulting from health services namely Healthcare
Associated Infections (HAI's) in US hospitals in 2013
reached 721,800 cases from 183 hospitals studied and
as many as 75,000 patients died while receiving
treatment at the hospital (CDC, 2014).
The Indonesian Infection Control Association
conducted a prevalence point survey of 11 hospitals
in Jakarta's Capital Region in 2010, showing the
HAI's incidence rate, namely surgical injury Infection
of 18.9%, infection that occurred in the urinary canal
of 15.1%, infection in primary blood flow of 26.4%,
pneumonia 24.5% and infections in other airways
15.1%, and other infections 32.1% (Perdalin, 2010).
Hospitals in the city of Medan, among others, Haji
Adam Malik Regional Hospital, have clean surgical
post-operative wound infections with a prevalence
rate of 5.6% (Nirbita, 2017). The high incidence of
HAI's indicates that transmission is still quite high
and is a threat to hospital services.
The lack of quantity and quality of hospital
infection control is closely related to compliance with
hand washing. According to the World Health
Organization (WHO) that compliance with hand
washing of health workers can control or control the
incidence of infection (WHO, 2014).
The level of compliance with hand washing in
developed countries such as the United States has not
been as expected, reaching 50%. The level of
compliance of nurses' hand hygiene did not differ
greatly at the Marmara University Hospital in
Istanbul reaching 43.2% (Karaaslan, et al, 2014).
Damanik Research (2012) and Pratama (2015) at
two hospital locations in Indonesia, Imanuel Hospital
Bandung and RSUD dr. Iskak, where the level of
compliance of nurses carrying out hand washing did
not reach half of the proportions of 48.3% and 36%.
The level of nurse compliance adheres to hand
hygiene is influenced by three factors: first, the
individual characteristic factors consist of
Komaria, R., Girsang, E. and Napiah, A.
Personnel Characteristics and Comprehensiveness of Hospital on Handwashing Compliance.
DOI: 10.5220/0010293202150220
In Proceedings of the International Conference on Health Informatics, Medical, Biological Engineering, and Pharmaceutical (HIMBEP 2020), pages 215-220
ISBN: 978-989-758-500-5
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
215

understanding, response, being busy due to heavy
workload. Second, organizational support factors
consist of standard operating procedures, rewards,
sanctions, training activities and adequate facilities /
infrastructure support, third, behavioral factors
consist of trust, confidence and other social support.
Another important thing is the role of the prevention
of infection control (PIC) committee in increasing
understanding to improve nurse compliance in the
application of hand washing for hand hygiene (Pittet,
2001; David, 2010; Turnip et al, 2020; Wijaya et al,
2019).
Karadag Research (2016); Jemal (2018); White
(2019); and Gon (2020) state knowledge, friend
suggestions, perceptions and beliefs, practices, and
consumables as determinants of hand hygiene.
Furthermore Shobowale research (2016); Kupfer
(2019): that the availability of facilities (easy access)
can improve hand washing hygiene.
Sands (2010), using the Behavior Centered
Design (BCD) theory related to behavioral change
interventions in improving hand washing compliance,
namely reporting hand hygiene, implementing hand
washing by peers, increasing interaction with patients
and other staff members, reducing stress, busyness,
and burdens cognitive related to the task.
Farhaoudi (2016) reviewed the WHO Multimodal
Hand Hygiene Improvement Strategy consisting of:
1) system changes to ensure access of health care
workers to hospital facilities with an approach to the
availability of alcohol-based hand washing facilities
in the service rooms, 2) training and continuing
education, 3) evaluation and feedback, 4) reminders
at work, and 5) providing safety climate through IPC
agencies. After intervention by carrying out and
providing a Strategy to Improve Hand Hygiene in the
service room, where the proportion of hand rubbing
behavior (18.1%) and hand washing (11.5%), there
was an increase in hand rubbing (18.1%) and hand
washing 11.5%) was much better among health
workers (p 0.001 <0.05). Zhao (2018) examines 5
aspects of the theory of Diffusion of Innovation
Theory (DIT): relative advantages, compatibility,
simplicity, testability, and observability significantly
influence hand washing practices.
A similar study by Boyce and Pittet (2011) states
that one of the obstacles in non-compliance with
washing hands is the difficulty of accessing a place to
wash hands or other tools used to wash hands. Ease
of accessing supplies of tools for washing hands,
sinks, soap or alcohol jell is very important to make
compliance according to standards. Other research
was conducted by Shobowale (2016); and Kupfer
(2019): stating the availability of hand washing
facilities or the ease of gaining access to hand
washing affects the cleanliness of hand washing.
Nurse hand washing compliance audit results at
the Royal Prima Hospital Medan in 2018 by the PIC
Committee with 53.3% doctor compliance, 47.9%
nurses and other health workers 35.6%.
Compliance is not in accordance with Minimum
Service Standards> 85%. Research is important
because hand hygiene is the duty and responsibility
of nurses and is cheap and easy to do to avoid
infection in hospitals, it only takes a strong desire and
willingness to implement. But in reality, this habit has
not gone according to expectations.
Previous studies generally used quantitative
research designs or types, mix methods, semi-
experiments with cross sectional accuracy. Theory
used by Behavior Centered Design (BCD) by Sands
(2010); Diffusion of Innovation Theory (DIT) by
Zhao (2018); Multimodal Hand Hygiene
Improvement Strategy by Farhaoudi, 2016) and other
behavioral theories. Statistical tests use correlation
and comparison (t-test) with intervention.
This research is a quantitative research. In this
study the focus is more on the determinants of hand
washing hygiene developed by Pittet. The study
results have contributed a lot to WHO and certainly
to different loci. This study uses a survey with a cross
sectional approach (data collection uses a
questionnaire and a checklist) which the observations
were simultaneously carried out. The variables were
measured after data collections. The data were
analyzed with univariate, bivariate and multivariate
(multiple logistic regression) methods to prove the
hypothesis.
2 METHOD
The study was conducted using inpatient nurses as
respondents in Royal Prima Hospital Medan as many
as 319 people and a sample of 113 nurse respondents
using a different hypothesis test proportion of one
sample. The sample technique uses simple random
sampling through lottery. Data collection by
distributing closed questionnaires and observations
for 30 days in March 2020.
The questionnaire using the Guttman scale
consists of knowledge totalling 10 with alternative
answers (true or false) grouped (good = 2 and not
good = 1), attitudes of 10 questions (agree and
disagree) categorized (positive = 2 and negative = 1),
roles PIC 15 statements (yes and no) are grouped
(support = 2 and less support = 1). Observation of the
completeness of facilities and infrastructure with a
HIMBEP 2020 - International Conference on Health Informatics, Medical, Biological Engineering, and Pharmaceutical
216
checklist of 7 items, alternative answers available and
absent, consisting of: sink, liquid soap, paper towels,
antibacterial liquid, free of inappropriate equipment,
bins, and posters are grouped (complete = 2 and
incomplete = 1). Observation of hand washing
hygiene 5 moments and 6 steps are grouped (obedient
= 2 and disobedient = 1). Before the data was
processed, the instrument validity and reliability tests
were performed.
The results of the validity test obtained the value
of the calculated r coefficient in the range 0.472-
0.913 is greater than r table, (0.361), it is assumed that
the data is normally distributed. Cronbach alpha value
count 0.929, 0.950, 0.950, 0.955, 0.902 and 0.854
greater than 0,700 (determination), it is assumed that
the questionnaire is said to be reliable.
After the data is collected, it is processed by
collecting, checking, coding, entering and processing.
Furthermore the data were analyzed through
univariate (descriptive), bivariate with chi square and
multivariate tests using multiple logistic regression
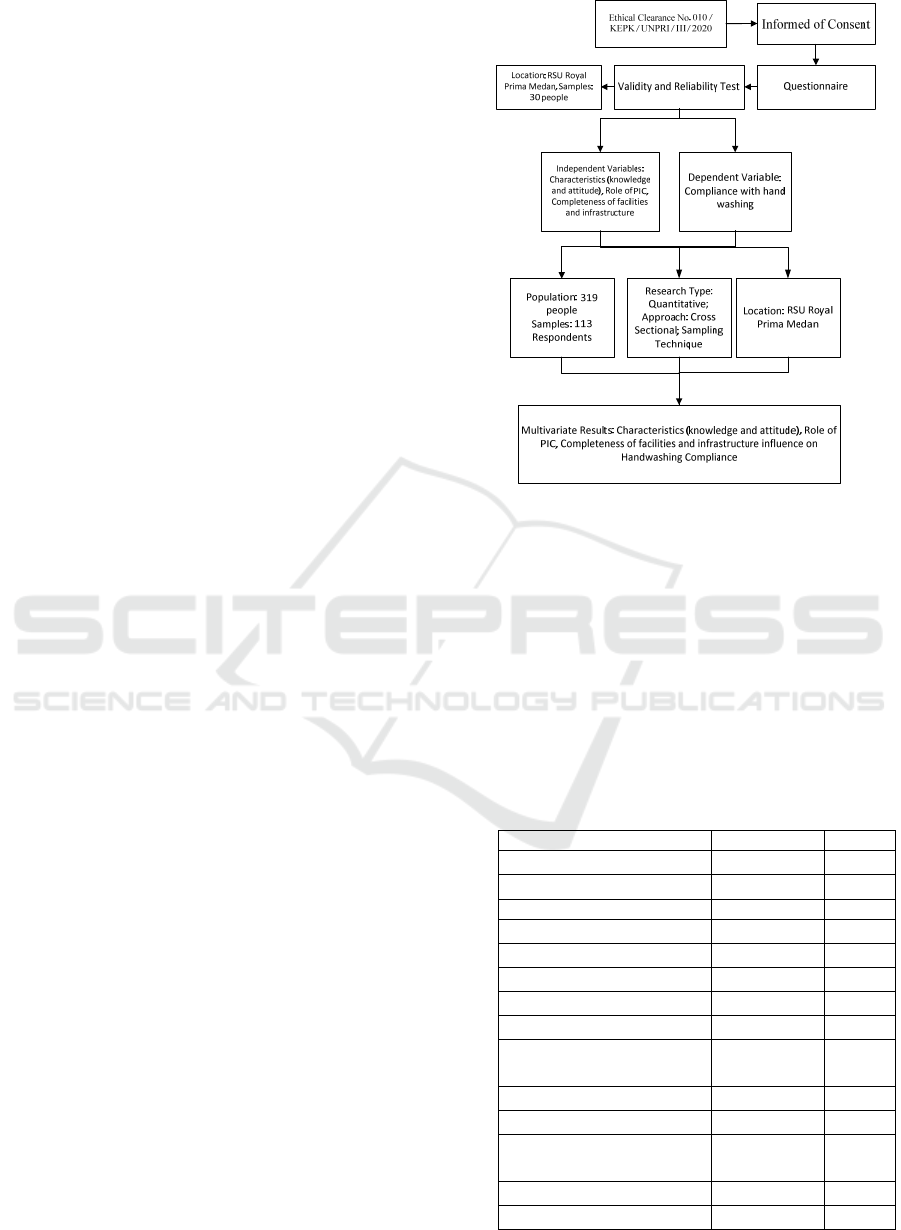
tests at the 5% level. The Research procedure is
shown in Figure 1.
3 RESULTS AND DISCUSSION
Analysis of the research questionnaire based on the
category is dummy (2 groups) with a mean or average
= 1.5, where the variable above the average is
knowledge (1.54), the role of PPI (1.58), while below
the average is the attitude variable about hand
washing hygiene (1.45%), completeness of facilities
and infrastructure (1.44) and compliance with the
application of hand washing (1.35%). Measurement
results of the research variable questionnaire. The
results of data analysis are described as follows.
3.1 Univariate Analysis
Respondents with good prioritization knowledge
(54%), being negative about washing hands (54.9%),
supporting PIC's role (58.4%), incomplete facilities
and infrastructure (55.8%) and poor compliance with
hand washing (64) , 6%).
Figure 1: Scheme of Research Procedure.
3.2 Bivariate Analysis
In Table 3, the results of the bivariate analysis explain
the variables of knowledge (0.006), attitude (0,000),
the role of PIC (0,000) and the completeness of
facilities & infrastructure (0.002) having a p value
less than 0.05. This means that the knowledge,
attitude, role of PIC and the completeness of facilities
& infrastructure are related to compliance with hand
washing.
Table 2: Distribution of Research Variables.
Knowled
g
e n %
N
ot
g
oo
d
52 46,0
Goo
d
61 54,0
Attitude
N
e
g
ative 62 54,9
Positive 51 45,1
Role of PIC
N
o
t
suppor
t
e
d
47 41,6
Suppor
t
e
d
66 58,4
Facilities &
infrastructure
n %
N
ot Complete 63 55,8
Complete 50 44,2
Compliance washing
hands
N
ot Obedien
t
73 64,6
Obedien
t
40 35,4
Personnel Characteristics and Comprehensiveness of Hospital on Handwashing Compliance
217
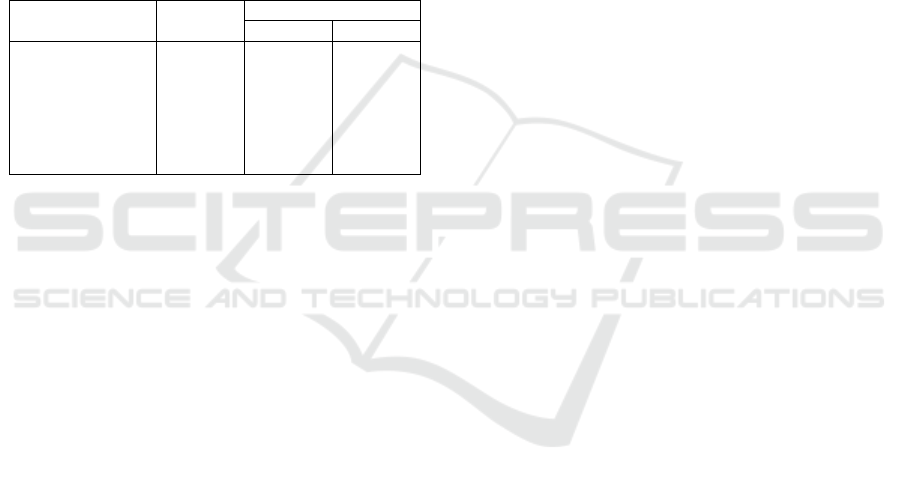
3.3 Multivariate Analysis
Table 3, Multivariate analysis results explain the
variables of knowledge (OR 5.149; p 0.003), attitude
(OR 5.176; p 0.002), the role of PIC (OR 6.156; p
0.002) and the completeness of facilities &
infrastructure (OR 3.293; p 0.017) p was smaller than
0.05. This means that the knowledge, attitude, role of
PIC and the completeness of facilities and
infrastructure have a positive effect on the
compliance of nurses' washing hands. Based on the
OR value, the PIC role variable was 6.156, which
means that the support role of the PIC tends to 6.156
times that nurses obey wash their hands rather than
the role of PIC less supportive.
Table 3: Bivariate and Multivariate Analysis Results.
Variables Bivariat
Multivariat
O
R
Si
g
Knowledge
0,006 5,149 0,003
Attitude
0,000 5,176 0,002
Role of PPI
0,000 6,156 0,002
Infrastructure
0,002 3,293 0,017
Based on the research results in the table 3, the
findings can be analysed as follows. The relationship
of knowledge to nurse compliance in the application
of hand washing. There was a link between
knowledge and compliance with the application of
hand washing. Based on the OR value of 5.149 which
means that the support role of PPI tends to 6.156
times nurses obediently wash their hands rather than
the role of PPI is less supportive.
In line with the results of Khairiah's research
(2012); Ananingsih and Rosa (2016) explained that
knowledge influences the level of compliance of
nurses in using personal protective equipment
including washing hands. The minimal moment of
hand washing is caused partly by the lack of
knowledge about the importance of hand washing and
hand washing techniques. Other similar studies by
Karadag (2016); Jemal (2018); White (2019); and
Gon (2020) state that knowledge influences the
hygiene of the hands of health workers. In the study
it can also be explained that nurses with good
knowledge are more obedient in washing their hands.
However, it is also possible for nurses who have good
knowledge but are not compliant to apply good hand
washing due to busyness or workload that is quite a
lot so that without deliberate neglect of washing
hands before and after touching patients.
3.4 Attitudes of Hand Washing
There was a relationship between attitudes towards
compliance with the application of hand washing.
Based on the OR value of 5.176 which means that a
positive attitude tends to 5.176 times the nurse
submissive to washing hands rather than the negative
attitude.
A similar study by Ernawati (2014) said nurses
before and after providing health services to patients,
nurses have not complied with hand washing in the
inpatient room. Karadag (2016) said that moderate
perceptions and beliefs in nurses and students can
improve hand hygiene to avoid infectious diseases.
To increase nurses ability to apply hand washing, the
head of the Inpatient Installation instructs each head
of the room to reprimand the nurse who is not
compliant to wash hands. In addition, learning models
need to be carried out through a 5-moment hand
washing campaign and 6 steps of hand hygiene
throughout the inpatient room held every 6 months.
3.5 Role of PPI on the Application of
Hand Washing
It was obtained a link between the role of PIC on
compliance with the application of hand washing.
Based on the OR value of 6.156 which means that the
role of PIC that supports tends to 5.176 times nurses
obediently wash their hands. From the role of PIC
was less supportive as a dominant factor because the
OR value was greater than other variables. According
to Boyce and Pittet (2011) that nurses in hospitals
have not complied with the precautions of HAI
influenced by the provision of
Educational activities or training has not been
continuous as a form of PIC's role.
The role of PIC in improving nurses' ability to
apply handwashing hygiene through training
activities. Farhaoudi's research (2016) explains that
ongoing training and education can affect nurses hand
hygiene compliance. In this study also explained that
nurses stated that the role of PIC was supportive so
that it could cause nurses to obediently wash their
hands. However, there were nurses who stated that
the role of the PIC committee was supportive, but
nurses did not obediently wash their hands. These was
because nurses have attended training so that
understanding and response to hand hygiene
appropriately with 6 stages. The need for a hospital
management to implement training for nurses who
have not yet attended training, especially a new
nurses.
HIMBEP 2020 - International Conference on Health Informatics, Medical, Biological Engineering, and Pharmaceutical
218

3.6 Facilities and Infrastructure
There was a correlation between the completeness of
facilities and infrastructure to the compliance of the
application of hand washing. Based on OR value of
3,293 which means that complete facilities and
infrastructure tend to be 3,293 times nurses
obediently wash their hands rather than incomplete
facilities and infrastructure. A similar study by Boyce
and Pittet (2011) states that one of the obstacles in
non-compliance with hand washing is the difficulty
of accessing a handwashing area or other supplies
used for washing hands. Ease of accessing supplies of
tools for washing hands, sinks, soap or alcohol jell is
very important to make optimal compliance
according to standards.
Other research was conducted by Shobowale
(2016); and Kupfer (2019): stating the availability of
hand washing facilities or the ease of gaining access
to hand washing affects the cleanliness of hand
washing.
The results of these observations can explain that
PIC's efforts to provide handwashing equipment such
as washbasins have not been optimal, so that the
completeness of hand washing facilities was
incomplete due to PPI supervision in monitoring
nurses who in charge of providing hand washing
facilities in the sink. This factor can prevent nurses
from doing hand washing of 5 moments and 6 stages
which recommended by the hospital.
The availability of complete facilities in the sink,
can’t guarantee the implementation of 5 moments
running well. Facts in the field, there were nurses who
have not washed their hands in accordance with the
SOP in the hospital. The need to monitor the
performance of nurses implementing hand washing
by placing Closed Circuit Television (CCTV) in each
inpatient room to assess and monitor the hand
washing program.
4 CONCLUSIONS
Statistically the individual characteristics (knowledge
p = 0.003 and attitude p = 0.002), the role of PPI (p =
0.002), and the completeness of facilities and
infrastructure (p = 0.017) correlate to the compliance
of handwashing nurses. It is recommended that
hospital management increase nurses' awareness
through socializing 5 moments with 6 stages and
completing facilities and infrastructure and applying
administrative sanctions or verbal reprimands to
health workers if 3 times are not compliant.
REFERENCES
Ananingsih P.D., & Rosa E.M. 2016. Kepatuhan 5 Momen
Hand Hygiene pada Petugas di Laboratorium Klinik
Cito. Yogya-karta. Jurnal Medicoeticolegal dan
Manajemen Rumah Sakit, 5 (1):16-24.
Boyce J.M., & Pittet D. 2011. Guideline for Hand Hygiene
in Health-Care Settings. Morb Mortal Wkly Rep.
Centers for Disease Control and Prevention (CDC), 2014.
HAI’s Data and Statistics. Diperoleh di:
https://www.cdc.gov/hai/surveillance/index.html.
David De Wandel, S.L. 2010. Behavioral Determinants of
Hand Hygiene Compliance in Intensive Care Units,
http://ajcc.aacnjour nals.org/content /19/ 3/230.
Ernawati. 2014. Penerapan Hand Hygiene Perawat di
Ruang Rawat Inap Rumah Sakit. Jurnal Kedok-teran
Brawijaya, 28(1): 2014.
Farhoudi F., Dashti A.S., Davani M.H., Ghalebi N., Sajadi
G., Taghizadeh R. Impact of WHO Hand Hygiene
Improvement Program Implementation: A Quasi-
Experimental Trial. BioMed Research International.
Volume 2016, Article ID 7026169, 7 pages.
http://dx.doi.org/10.1155/2016/7026169
Gon G., et al. (2020). Behavioural Determinants of Hand
Washing and Glove Recontamination before Aseptic
Procedures at Birth: A Time-and-Motion Study and
Survey in Zanzibar Labour Wards. International
Journal of Environmental Research and Public Health.
17, 1438; doi:10.3390/ijerph17041438.
Jemal S. 2018. Knowledge and Practices of Hand Washing
among Health Professionals in Dubti Referral Hospital,
Dubti, Afar, Northeast Ethiopia. Hindawi. Advances in
Preventive Medicine. Volume 2018, Article ID
5290797, 7 pages.
https://doi.org/10.1155/2018/5290797.
Karaaslan, et all. 2014. Compliance of Healthcare workers
with Hand Hygiene Practices in Neonatal and Pediatric
Intensive Care Units: Overt Observation. Interdis-
ciplinary Perspectives on Infec-tious Diseases.
Karadag M., Iseri O.P., Yildirim N., Etikan I. 2016.
Knowledge, Beliefs and Practices of Nurses and
Nursing Students for Hand Hygiene. Jundishapur J
Health Sci. 8(4):e36469.
Kupfer T.R., Wyles K.J., Watson F., Ragione R.M.L.,
Chambers M.A., Macdonald A.S. 2019. Determinants
of hand hygiene behaviour based on the Theory of
Interpersonal Behaviour. Journal of Infection
Prevention. 20(5):232–237.
Nirbita A., Rosa E.M., Listiowati E. 2017. Faktor Risiko
Kejadian Infeksi Daerah Operasi pada Bedah Digestif
di Rumah Sakit Swasta. Kes Mas: Jurnal Fakultas
Kesehatan Masyarakat. 11(2): 93~98.
Perdalin. 2010. Pedoman Managerial Pencegahan dan
Pengendalian. Infeksi di Rumah Sakit dan Fasilitas
Kesehatan Lainnya, Jakarta.
Pratama B.S., Mulyatim K., and Kasil R. 2015. Faktor
determinan kepatuhan pelak-sanaan hand hygiene pada
perawat IGD RSUD dr. Iskak Tulungagung. Jurnal
Kedokteran Brawijaya, 28(2).
Personnel Characteristics and Comprehensiveness of Hospital on Handwashing Compliance
219

Sands M., Aunger R. 2020. Determinants of hand hygiene
compliance among nurses in US hospitals: A formative
research study. PLoS ONE 15 (4): e0230573.
https://doi.org/10.1371/journal.pone.0230573
Shobowale E.O., Adegunle B., Onyedibe K., 2016. An
assessment of hand hygiene practices of healthcare
workers of a semi-urban teaching hospital using the five
moments of hand hygiene. Nigerian Medical Journal.
57(3): 49-54.
Turnip, A., Andrian, Turnip, M., Dharma, A., Paninsari, D.,
Nababan, T., Ginting, C.N., 2020. An application of
modified filter algorithm fetal electrocardiogram
signals with various subjects, International Journal of
Artificial Intelligence, vol. 18, no., 2020.
White S., Thorseth A.H., Dreibelbis R., Curtis V. 2020. The
determinants of handwashing behaviour in domestic
settings: An integrative systematic review.
International Journal of Hygiene and Environmental
Health. 227 (113512).
Wijaya, C., Andrian, M., Harahap, M., Turnip, A., 2019.
Abnormalities State Detection from P-Wave, QRS
Complex, and T-Wave in Noisy ECG, Journal of
Physics: Conference Series, Volume 1230, (2019)
012015. doi:10.1088/1742-6596/1230/1/012015.
World Health Organization (WHO). 2014. Hand Hygiene:
Why, How & When?. Diperoleh di:
http://webcache.google
usercontent.com/search?q=cache:axFelv
MWDPgJ:www.who.int/gpsc/5may/Hand_Hygiene_
Why_How_and_When_Brochure.pdf+&cd=12&hl=en
&ct=clnk&gl=id.
Zhao Q, Yang MM, Huang Y-Y, Chen W. 2018. How to
make hand hygiene interventions more attractive to
nurses: A discrete choice experiment. PLoS ONE
13(8): e0202014. https://doi.org/
10.1371/journal.pone.0202014.
HIMBEP 2020 - International Conference on Health Informatics, Medical, Biological Engineering, and Pharmaceutical
220
