
Access Barriers of Infertility Services for Urban and Rural Patients
Binarwan Halim, Ermi Girsang*, Sri Lestari R. Nasution, Chrismis Novalinda Ginting
Faculty of Medicine, Universitas Prima Indonesia, Indonesia
Keywords: Access Barriers, infertility, urban, rural.
Abstract: The infertility problem is faced by 15-20% of couples of childbearing age that have an impact on couples
social and psychological problems, families and communities. Infertility services in Indonesia are not well
distributed and most are in urban areas. The infertility services in rural areas are normally difficult to access.
This study aims to detect differences in barriers to access the infertility services in urban and rural
communities who seek treatment at IVF Clinic. The study was conducted by quantitative methods using a
questionnaire. A total of 130 respondents were divided into two groups each 65 respondents for rural and
urban, respectively. The analyzed variables include knowledge, economic status, geography, social culture,
psychological, and religious. The data obtained were analyzed by chi-square and multivariate. It was found
three out of six significant variables (p = 0.014, p = 0.023 and p = 0.005) in multivariate analysis which are
the economic level, geographic location, and socio-cultural with an OR values of 2.606, 3.905, and 5.299,
respectively. The economic status in urban areas was higher than rural, geographical barriers in rural areas
were more than urban, and socio-cultural barriers with less support in rural compared to urban areas.
1 INTRODUCTION
Infertility is the failure of a partner to get pregnant at
least within 12 months of having sex regularly
without contraception. Infertility problems can have
a major impact on married couples who experience
them, in addition to causing medical problems,
infertility can also cause economic and psychological
problems (HIFERI, 2013). Normally, couples who
experience infertility will go through a long process,
where this process can be a physical and
psychological burden for infertility couples (Irianto,
2014). Fertility or fertility of a person can be
influenced by genetics, heredity, and age. The
infertility is classified into two types, namely primary
and secondary infertilities (Anwar, 2005).
The problem of infertility is not only a
gynecological problem, but it becomes a serious
health problem because these problems often affect
the quality of life, not only on the physical but also
have an impact on the psychological, social and
economic of the individuals and couples.
9,10,11
In the United States, health service gaps also
occur in infertility services. High medical costs,
barriers to access of services cause problems in
getting fertility services. The majority of patients
undergoing treatment with the Invitro Fertilization
(IVF) method in the United States pay for themselves
because they do not have health insurance that covers
IVF costs (Wu et al., 2014). Other factors that
contribute to barriers to access of the infertility
services are the level of education and knowledge,
race, ethnicity, religion, sexual orientation, gender
identity, marital status, and conscious or unconscious
discrimination (Peterson, 2005; Bennett et al. ., 2012;
Harzif et al., 2019; Thompson, 2006; Domar et al.,
2005).
Harris et al. (2017) and Chin et al. (2017) found
that geographical influence on access to infertility
services (Harris et al., 2017; Chin et al., 2017). Ho et
al. (2017) and Udgiri et al. (2019) found a socio-
cultural influence on access to infertility services (Ho
et al. 2017; Udgiri et al. 2019). Economic barriers in
the form of large income also affect access to
infertility services where financial support such as
health insurance is needed especially in rural
communities with lower economic status (Insogna et
al., 2018; Maxwell et al., 2017; Kaur et al., 2018 ;
Kunicki et al., 2018). Psychological conditions are
also reported to be one of the barriers to access
infertility services (Lakatos et al, 2017; Rooney et al,
2018; Omu et al, 2010; Turnip et al, 2020; Wijaya,
2019). Lakatos et al. (2017) and Rooney et al. (2018)
reported that symptoms of depression and anxiety in
Halim, B., Girsang, E., R. Nasution, S. and Ginting, C.
Access Barriers of Infertility Services for Urban and Rural Patients.
DOI: 10.5220/0010291901490157
In Proceedings of the International Conference on Health Informatics, Medical, Biological Engineering, and Pharmaceutical (HIMBEP 2020), pages 149-157
ISBN: 978-989-758-500-5
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
149

infertile women were more prominent than fertile
women (Lakatos et al., 2017; Rooney et al., 2018).
Various psychological responses appear in
couples who are facing infertility problems, including
low self-esteem, anger, sadness, jealousy towards
other couples who already have children, anxiety,
and, finally, depression (Wiweko et al. 2017).
Wiweko et al. (2017) found that the distribution of the
stress levels in infertile patients in the Yasmin IVF
Clinic in Indonesia accounts for 22% of the risk
factors for infertility, which are mainly associated
with the length of infertility. These symptoms are
physical symptoms and interfere with the couple’s
daily activities (Wiweko et al. 2017).
World Health Organization (WHO) and the
United Nations have made reproductive health a
global health care priority. Encouragement needs to
be given so that all stakeholders are moved to build
affordable, safe and effective infertility services
(Ethics Committee of the ASRM, 2015). Another
problem is that most regions in the world that have
high infertility rates find it difficult to access
infertility clinics that are rare and expensive, so that
most women become less concerned about their
future without children (Inhorn et al., 2014). Only
about 25% of infertile couples are able to access
infertility services both in developed and developing
countries (Sadeghi, 2015). The prevalence of
infertility according to the WHO is estimated at 8-
10%. Most infertile couples exist in developing
countries (Ombelet, 2011). The infertility rate in
Indonesia ranges from 12-15% or around 3 million
couples (Fauziah, 2012). The normal, young aged
couples have a 25% chance to conceive after 1 month
of unprotected intercourse; 70% of the couple’s
conceive by 6 months, and 90% of the couples have a
probability to conceive by 1 year (Anwar et al., 2016).
Indonesia has 34 fertility clinics that offer a
variety of treatment options, but the use of these
facilities is still very low. This is reflected in the
number of IVF cycles per year in Indonesia which is
still very low compared to other countries. The reason
is that fertility clinics tend to be centered in big cities,
especially in Java, and the distribution of patients and
the IVF cycle are not compatible with existing clinics
(Ombelet, 2011). Based on the 2017 IDHS, fertility
rates in North Sumatra declined from 3% in 2012 to
2.9% in 2017. In other words, infertility rates have
increased every year in North Sumatra (BKKBN,
2017). One of the fertility clinics in North Sumatra,
the Halim Fertility Center, has also seen an increase
in new patient visits each year where the average
number of new patient visits each year is 1300
patients. However, the use of existing infertility
clinics is still inadequate and referrals are still low.
The referral system from other health providers to
fertility service facilities is very influential (Klitzman,
2018).
Several attempts have been made to improve
access to infertility services in Indonesia. Bennett et
al. (2012) in his research found that there are four
keys that must be done to improve access to infertility
services in Indonesia, among others, improving
education and counseling, improving the referral
system, reducing medical costs and equitable fertility
service facilities. (Bennett et al., 2012). Harzif et al.
(2019) concluded that providing information about
infertility services to the community was proven to
increase patient acceptance of the treatment to be
provided (Harzif et al., 2019). The barriers to access
faced by infertility patients to reach the fertility clinic
can be different when viewed from the origin of the
patient, whether coming from urban or rural areas.
The barriers can be various factors such as
knowledge, geographical, socio-cultural, religious,
economic andpsychological barriers.
This study aims to determine various variations of
the obstacles faced by urban and rural communities,
so that with the results of this study, researchers can
map the strategy approach to help infertility patients
so they can get offspring. This study is different from
previous studies because the samples taken came
from patients visiting IVF clinics to find out more
clearly the characteristics and influential factors in
relation to their visits to IVF clinics so that solutions
can be found for more optimal infertility services.
2 METHOD
In this study, data collection was carried out using a
closed questionnaire in the form of multiple choices
with each question having a choice of 2-5 answers (a
total of 42 questions consisting of 5 questions of
respondents' identities and 37 questions including
knowledge of fertility, economic status, geography,
psychological, sociocultural and religious). We have
checked the existence of such a questionnaire before
designing new questionnaire but we did not find the
questionnaire and we designed our own questionnaire
about access barriers of infertility services.
The questionnaire consisted of six sections: First,
it included personal and demographic data (age,
marriage time, education levels, occupations). The
second section was concerning women’s knowledge
of infertility and its management. It consisted of 20
single and multiple response questions about the
definition, duration, etiology, and treatment of
HIMBEP 2020 - International Conference on Health Informatics, Medical, Biological Engineering, and Pharmaceutical
150
infertility. The next section was related to economic
status as a barrier to access, which consisted of 4
single questions about monthly income, knowledge
of how much infertility treatment cost, financial
ability, and hold health insurance to cover their
infertility treatment. The fourth section was related to
patient’s geographical barrier with 5 single questions
on accessibility to infertility care which consisted of
4 single questions about knowledge of availability of
fertility clinic in North Sumatera, the distance
between patients residence and fertility care,
availability of transportation to fertility care, and the
severity of the transportation field. Then, the fifth
section was about a patient’s psychological and
emotional barriers consist of 3 single questions about
fear of infertility treatment, an embarrassment of
being infertility couple, the embarrassment of
infertility treatment. Finally, the last section was
about socio-cultural factors which also consisted of 4
single questions about their beliefs and culture related
to infertility treatment, family endorsement for
infertility treatment, and gender of the medical
provider.
The questionnaire used first tested the validity
with Pearson product moment correlation coefficient,
called valid if the value is above 0.30. The valid
questions continue with the Cronbach’s alpha
reliability test. (reliable if the value is above 0.619).
The study was conducted at Halim Fertility Center
IVF Clinic at Stella Maris Hospital from August until
October 2019. The study population was patients
from IVF Clinic with an average visit of 1300 patients
/ year and with total sample was 130 patients.
Research samples that meet the inclusion criteria are
infertility >1 year, willing to participate as
respondents, able to communicate well, physically
and mentally. Exclusion criteria are if the
questionnaire answers are incomplete where there are
130 respondents who are divided into 2 groups
namely urban and rural. The sampling technique used
was consecutive sampling, where every new patient
who came during the study period was used as a
sample. We obtained the ethical clearance from the
hospital. Patients who are willing to become
respondents are asked to sign a willingness form to
participate in the study and are notified that the results
of the research will be published later. We perfomed
validity and reliability test to the questionnaire. The
validity test was conducted on 20 respondents at
Sarah General Hospital Medan and the research tool
in the form of researchers conducted interviews
directly with patients and read out the research
questions listed in the questionnaire. The independent
variables of this study were barriers of access to
infertility ( knowledge, economy, geographical,
psychological, social culture and religious) and
dependent variables were urban and rural patients.
Bivariate test analysis uses chi-square test for two-
parameter data and Kruskal Wallis for data of more
than two parameters, while multivariate data analysis
to determine correlations uses multiple logistic
regression tests. The results are presented in narrative
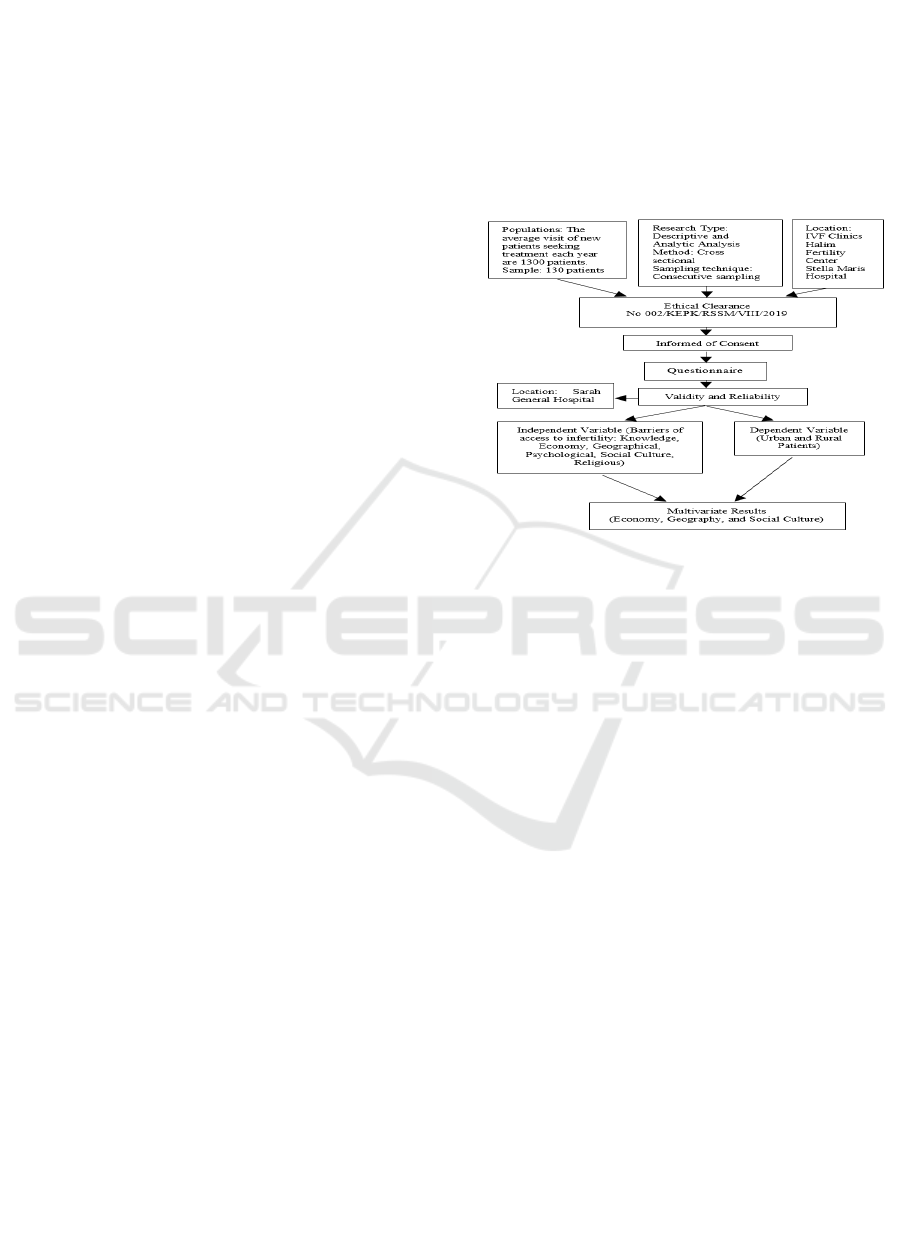
form in accordance with the related theory (figure 1).
Figure 1. Scheme of Research Process
3 RESULTS AND DISCUSSIONS
3.1 Validity and Reliability Tests
This study uses a questionnaire that has been tested
for validity using the Pearson product moment test.
Where if r count (rc)> r table (rt) (> 0.3) then the
question was declared valid. In Table 1, shows from
20 items of knowledge questions obtained 12 valid
items and 8 invalid. There were a number of
questions for Economic, geography, psychology,
social cultural, and religious variables (i.e., 5, 5, 3, 2,
and 2, respectively) which all of them were valid. The
detail validity tests results for each variable is shown
in Table 1, where K is Knowledge; E is Economy; G
is Geography; P is Psychology; S is Social Culture;
and R is Religious.
Access Barriers of Infertility Services for Urban and Rural Patients
151
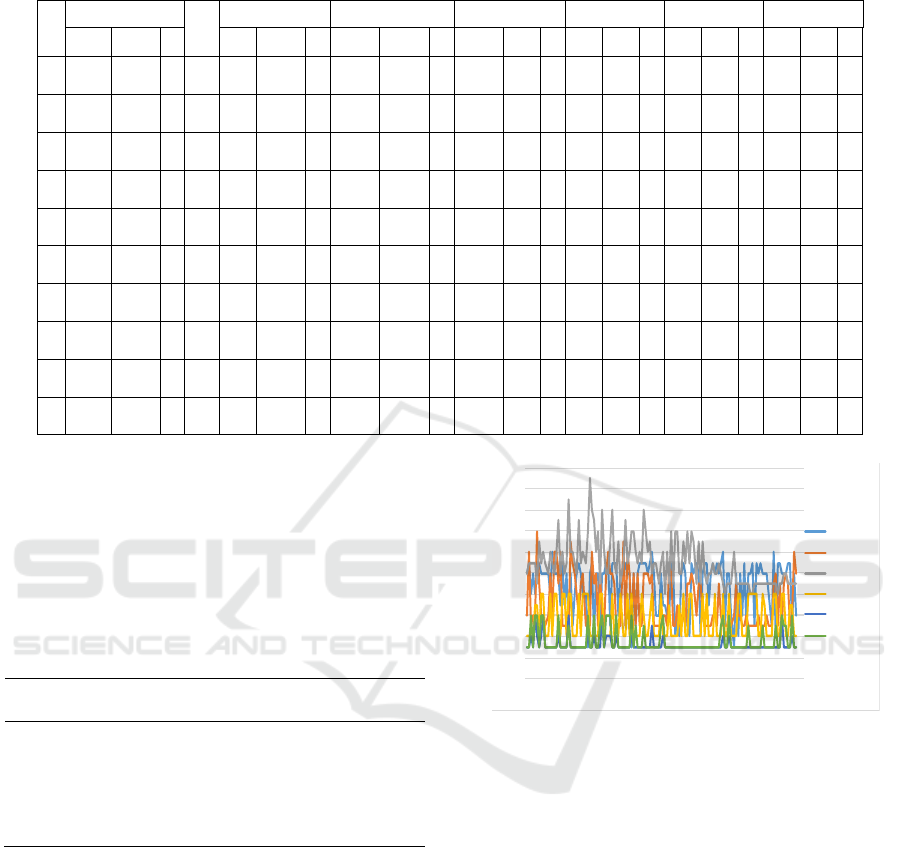
Table 1. Validity Test Result of Knowledge, Economics, Geography, Pyschology, Social Culture, and Religion.
N
o K No K E G P S R
rc rt v rc rt v rc rt v rc rt v rc rt v rc rt v rc rt v
1
0
.269 0.361 - 11
0
.61
5
0.361 + 0.641 0.361 + 0.724
0
.36
1
+
0
.81
5
0
.36
1
+
0
.33
1
0
.36
1
+
0
.64
9
0
.36
1
+
2
0
.374 0.361 + 12
0
.39
6
0.361 + 0.815 0.361 + 0.821
0
.36
1
+
0
.52
6
0
.36
1
+
0
.41
3
0
.36
1
+
0
.88
1
0
.36
1
+
3
0
.423 0.361 + 13
0
.37
7
0.361 + 0.375 0.361 + 0.815
0
.36
1
+
0
.45
8
0
.36
1
+
4
0
.268 0.361 - 14
0
.48
0
0.361 + 0.424 0.361 + 0.458
0
.36
1
+
5
0
.261 0.361 - 15
0
.28
4
0.361 - 0.815 0.361 + 0.424
0
.36
1
+
6
0
.154 0.361 - 16
0
.45
1
0.361 +
7
0
.144 0.361 - 17
0
.64
4
0.361 +
8
0
.384 0.361 + 18
0
.21
3
0.361 -
9
0
.375 0.361 + 19
0
.48
8
0.361 +
10
0
.424 0.361 + 20
0
.11
4
0.361 -
Table 2 is the reliability test results for each observed
variable. From Table 2 it can be seen that the results
of the reliability test on the questionnaire questions
regarding knowledge, economics, geography,
psychology, social culture and religious are reliable
because the Cronbach Alpha value >0.6.
Table 2. Reliability Test Results of Knowledge, Economics,
Geography, Psychology, Social Culture, and Religion.
Variables Cronbach`s
Alpha
Qty
Knowled
g
e 0.633 20
Economics 0.691 5
Geo
g
ra
p
h
y
0.687 5
Ps
y
cholo
gy
0.676 3
Social Culture 0.667 2
Reli
g
ious 0.654 2
Figure 2 shows the results of variable data from
130 respondents (urban: 1-65 and rural: 66-130). The
X-axis is the number of scores and the Y-axis is the
number of respondents. Light blue, orange, gray,
yellow, dark blue, and green colors are the variables
of knowledge, economic status, geography,
psychology, social culture, and religion with less,
low, there are obstacles, worries, less supportive, and
conflicting variables if scores ≤ 9, ≤6, ≤ 13, ≤4, ≤3,
and ≤3, respectively, and vice versa if the score is
greater.
Figure 2. Measurement results for 130 respondents for each
variable.
3.2 Bivariate Analysis
Table 3 shows the distribution of characteristics of
urban and rural respondents. Of the 130 respondents
in both the urban and rural groups, the majority of
respondents were <35 years old, namely 73.8% and
64.6%; for long time married, urban groups were
found 1-3 years as much as 35.4% and rural groups
were found >5 years as much as 50.8%. In terms of
education characteristics, the majority of urban and
rural groups have Bachelor /Magister/ Doctoral
degree educations, namely 81.5% and 76.9%, in
terms of employment, urban and rural groups have
housewives and other jobs as many as 47.7% and
63.1% Working conditions, the majority in the urban
and rural groups have leave of 83.1% and 75.4%.
0
2
4
6
8
10
12
14
16
18
20
1
7
13
19
25
31
37
43
49
55
61
67
73
79
85
91
97
103
109
115
121
127
133
Total
Score
Knowledge
Economics
Geography
Psychology
Social
Culture
Religious
HIMBEP 2020 - International Conference on Health Informatics, Medical, Biological Engineering, and Pharmaceutical
152

Table 3. Distribution of Characteristics of Urban and Rural
Respondents.
Characteristics
Urban Rural
n
(65)
%
(100)
n
(65)
%
(100)
Age (years)
< 35 48 73.8 42 64.6
> 35
17 26.2 23 35.4
Marriage time
< 1 5 7.7 6 9.2
1-3 23 35.4 17 26.2
4-5 15 23.1 9 13.8
> 5 22 33.8 33 50.8
Educations
Junio
r
&High School 12 18.5 15 23.1
Bachelor/Magister/
Doctoral Degree
53 81.5 50 76.9
Occupation
Private 28 43.1 14 21.5
Official Governmen
t
6 9.2 10 15.4
House wive&Others 31 47.7 41 63.1
Factors affecting access to infertility services in
this study are the level of knowledge, economic,
geographical, psychological / emotional, socio-
cultural, and religious levels (Table 4). Based on the
level of knowledge of respondents obtained the
results of statistical tests using the Chi Square test
there were no significant differences in the level of
knowledge of urban and rural groups (p = 0.453).
Based on the perspective level of the knowledge
about the fertility of the two groups does not have a
significant difference, on average have enough good
knowledge. This can be explained because the
samples taken were patients who come for treatment
at IVF clinics, which in general have already done a
lot of searching information and knowledge both
from the internet, social media, as well as by word of
mouth and the internet has been able to reach remote
areas, so rural communities also easily access
information and knowledge about fertility. This is
different with Harzif et al. (2019) found that
populations in urban and rural areas have
misperceptions about infertility, negative behavior
and inadequate knowledge. This might be due to
differences in the sample of patients taken and the
types of questions given in the questionnaire which
may have different weights (Harzif et al., 2019). The
study took samples from populations directly in
villages and cities and not those who came to the IVF
clinic.
The rural group had a lower economic level of
70.8% compared to the urban group of 49.2%.
Statistical test results at the economic level found
significant differences between urban and rural
groups (p=0.012). The level of income in the rural
group was significantly lower than in urban areas, it
is understandable that usually the rich live more in
cities. Of course, this economic ability influences
access to fertility treatment which is quite expensive.
In the rural group (92.3%) more expressed
geographical barriers compared to the urban group
(76.9%). From the statistical test results obtained a
significant difference in geographical factors between
urban and rural groups (p=0.015). When viewed from
geographical barriers, it clearly shows groups
especially those far from the center overcoming
fertility will experience difficulties. Fertility
treatment requires repeated visits and requires a
significant amount of time. This will also affect the
level of employment, economy and costs.
In psychological / emotional factors, both rural
and urban, groups that experienced more feelings of
worry than those who were not worried were rural as
much as 61.5% and urban as much as 60%. But from
the results of statistical tests there were no significant
differences at the psychological / emotional level
between urban and rural groups (p=0.857). Basically
a person has a feeling of shame or worry about
fertility conditions, especially when under pressure
from family, neighborhood or work environment. The
diagnosis of infertility can be a tremendous burden on
patients. The pain and suffering of infertility patients
is a major problem. Patients should be counseled and
supported when they undergo treatment (Lakatos et
al., 2017; Rooney et al., 2018). The burden of the
mind makes someone feel worried and maybe even
stressed in doing fertility treatments.
From the socio-cultural perspective, it was seen in
the rural and urban groups that more complained that
they experienced obstacles, namely 92.3% and
75.4%, respectively. Statistical test results on socio-
cultural factors found significant differences in socio-
culture between urban and rural groups (p = 0.009).
In rural groups more than urban areas, the level of
public trust in fertility services was still lacking, there
were still some worried that later offspring will not be
produced from their flesh and blood because they
were afraid of using other people's gamete cells.
Moreover, there was public trust in fertility services
was still lacking, there were still some worried that
later offspring will not be produced from their flesh
and blood because they were afraid of using other
people's gamete cells. Moreover, there was public
trust in raising infertility as karma due to errors made
by his family.
In the rural group about 83.1% who stated
contrary to religious while the urban group as much
as 70.8%. From the results of statistical tests, no
significant differences were found in groups facing
religious barriers between urban and rural groups
Access Barriers of Infertility Services for Urban and Rural Patients
153

(p=0.096). Basically the environment in Indonesia
both in cities and villages, the influence of religious
in family life is still large, many still consider children
a gift from God, if God still does not allow it, the
spouse still will not be able to have children. In
another study, there were religious barriers where the
IVF program was considered to be in conflict with the
religious and the values of the beliefs of the local
community (Thompson et al., 2006; Domar et al.,
2005).
Table 4. Proportions Distribution of Factors Affecting
Access to Infertility Services
Factors
Urban Rural p
n
%
n
%
Knowledge
Good 46 70.8 42 64.6
0.453
a
N
ot Good 19 29.2 23 35.4
Economics
Status
Low 32 49.2 46 70.8
0.012
a
High 33 50.8 19 29.2
Geographic
With barries 50 76.9 60 92.3
0.015
a
Without barriers 15 23.1 5 7.7
Psychological
Worry 39 60.0 40 61.5
0.857
a
N
o Worry 26 40.0 25 38.5
Socio-cultural
Less Supported 49 75.4 60 92.3
0.009
a
Supported 16 24.6 5 7.7
Religious
Contradicting 46 70.8 54 83.1
0.096
a
N
ot contradicting 19 29.2 11 16.9
a=Chi-Square
Table 5 shows the results of multivariate analysis
using multiple logistic regression tests. The variables
that qualify for testing (p<0.25) are economic,
geographic, socio-cultural, and religious. Based on
the results of statistical tests it is known that there are
three significantly different variables (p = 0.014; p =
0.023 and p = 0.005) in multivariate analysis, namely
the economic level with an OR value of 2.606 (95%
CI 1.210-5.611), geographic location an OR value of
3.905 ( 95% CI 1.203-12.677), and socio-cultural
with an OR value of 5.299 (95% CI 1.659-16.929),
while religious variables did not differ significantly
(p> 0.05). Thus it can be concluded that barriers in
economic level, geographical and socio-cultural
location differ in urban and rural patients in access to
infertility services at IVF Clinic.
Study by Deatsman et al. showed that
Ages
ranged from 18 to 67. One third (30.5%) were aware
fertility begins to decline at age 35, however this
varied among groups depending on prior history of
infertility or requiring fertility treatment. Nulliparous
women were more unaware of the health risks of
pregnancy over age 35 (1.4% vs 13.6%, P 0.02).
African Americans (AA) women were less likely to
think obesity (76% Caucasian vs 47.8% AA vs 66.7%
other, P < 0.05) and older age (88% Caucasian vs
60.9% AA vs 82.7% other, P 0.02) affected fertility
(Deatsman et al., 2016).
Table 5. Multivariate Analysis
Variables Coefisients p OR 95% CI
Selection 1
Economics 0.965 0.014 2.625 1.216-5.669
Geography 1.362 0.023 3.905 1.205-12.653
Socio-cultural 2.026 0.018 7.583 1.412-40.727
Religious -0.404 0.559 0.668 0.172-2.589
Constant -2.184 0.001 0.113
Selection 2
Economics 0.958 0.014 2.606 1.210-5.611
Geography 1.362 0.023 3.905 1.203-12.677
Socio-cultural 1.668 0.005 5.299 1.659-16.929
Constant -2.187 0.001
P =Probability; OR=Odd Rasio; CI=confidence interval.
Roupa et al examined 110 infertile women and
found that regarding marital status 94.4% (106) of the
participants were married and 3.6% (4) unmarried.
Regarding age, 64.5% were 20–29 years old, 20.0%
were 30-39 years old, 11,8% were 40-49 years old
and 3.7% were over 50 years old. As to occupation
status, 35% of the participants were employees in the
private sector, 27% were employees in the public
sector, 24% were self employees and 14% dealt with
the household. Regarding educational status, 3.6%
had finished primary school, 31.8% had finished high
school, 56.4% were University graduates and 8.2%
were graduates of another school (Roupa et al., 2009).
Socioeconomic status (SES) is an important social
determinant that can have profound impacts on
reproductive health. In the last decades, populations
of urban and rural regions have been subject to
categorization by various means of measuring SES. A
number of socioeconomic factors such as the
woman’s educational status, income per capita,
having a job, age at first marriage, life expectancy,
and infant mortality rates have been reported to be
associated with fertility rates by social scientists. In
recent years, the serum level of AMH has been
HIMBEP 2020 - International Conference on Health Informatics, Medical, Biological Engineering, and Pharmaceutical
154

considered a new marker of ovarian reserve. It is
influenced by age and exhibits a declining trend until
a woman reaches menopause. Both ovarian reserve
parameters, namely anti-Mullerian hormone level and
antral follicle count, exhibited a sig¬nificant
association with socioeconomic status (p=0.000 and
p=0.000, respectively). The association between
follicle stimulating hormone level and socioeconomic
status was also significant (p=0.000) (Barut et al.,
2016).
Reports also link fertility transition to
socioeconomic development. In 1993–94, 36% of the
population in India lived below the poverty line and
this rate dropped to 22% in 2005–2006, and this drop
was linked to the socioeconomic development. In
addition to a declining poverty rate, the fertility rate
declined from 3.5 to 2.9 among Indians in the same
time period (Barut et al., 2016).
Ali et al. in their study found that correct
knowledge of infertility was found to be limited
amongst the participants. Only 25% correctly
identified when infertility is pathological and only
46% knew about the fertile period in women’s cycle.
People are misinformed that use of intra-uterine
device (IUD) (53%) and oral contraceptive Pil
(OCPs) (61%) may cause infertility. Beliefs in evil
forces and supernatural powers as a cause of
infertility are still prevalent especially amongst
people with lower level of education. Seeking
alternative treatment for infertility remains a popular
option for 28% of the participant as a primary
preference and 75% as a secondary preference. IVF
remains an unfamiliar (78%) and an unacceptable
option (55%). Social stigma regarding infertility is
especially common across South Asia. For e.g. in
Andhra Pradesh, India 70% of women experiencing
infertility reported being punished with physical
violence for their failure. Women are verbally or
physically abused in their own homes, deprived of
their inheritance, sent back to their parents,
ostracized, looked down upon by society, or even
have their marriage dissolved or terminated if they are
unable to conceive (Ali et al., 2011).
Roudsari et al. in their study examined religion
impact women’s prespective of infertily. Religion and
spirituality are a fundamental part of culture and
influence how individuals experience and interpret
infertility counseling. Emerging categories included:
Appraising the meaning of infertility religiously,
applying religious coping strategies, and gaining a
faith-based strength. These were encompassed in the
core category of ‘relying on a higher being’.
Religious infertile women experienced infertility as
an enriching experience for spiritual growth. This
perspective helped them to acquire a feeling of self
confidence and strength to manage their emotions.
Hence, they relied more on their own religious coping
strategies and less on formal support resources like
counselling services. However, they expected
counsellors to be open to taking time to discuss their
spiritual concerns in counseling sessions. In addition
to focusing on clients’ psychosocial needs, infertility
counsellors should also consider religious and
spiritual issues. Establishing a sympathetic and
accepting relationship with infertile women will
allow them to discuss their religious perspectives,
which consequently may enhance their usage of
counselling services (Roudsari et al., 2011).
4 CONCLUSIONS
The results of the study of 65 respondents with 6 test
variables (ie, knowledge, economic status,
geography, social culture, psychological, and
religious) found that: (i) No significant differences
were found in the obstacles in the level of knowledge,
emotional / psychological level and religious between
the two urban and rural groups (p = 0.453; p = 0.857;
p = 0.096). (ii) Significant differences were found in
the barriers to economic, geographical and socio-
cultural status between urban and rural groups (p =
0.014; p = 0.023; p = 0.005). (iii) The most significant
correlations in rural access barriers compared to
urban areas are economic, geographical and socio-
cultural (OR 2.606; OR 3.905; OR 5.299).
From this study, we can map some strategies to
help infertility patients, for instance making
telemedicine to overcome geographical barriers,
improving the referral system and reducing medical
costs to overcome economic barrier.
REFERENCES
Ali, S., Sophie R., Imam AM., Khan FI., Ali SF., Shaikh A;
Farid-ul-Hasnain S., 2011. Knowledge, perceptions and
myths regarding infertility among selected adult
population in Pakistan: a cross-sectional study, BMC
Public Health; 11:760.
Anwar S., Anwar A., 2016. Infertility: A Review on
Causes, Treatment and Management, Women’s Health
Gynecol; 2(6): 1-5.
Anwar, R., 2005. Diagnostik Klinik Dan Penilaian
Infertilitas. In: Fertilitas Endokrinologi Reproduksi
Bagian Obstetri dan Ginekologi RSHS/FKUP
Bandung, Bandung Fakultas Kedokteran Universitas
Padjajaran.
Access Barriers of Infertility Services for Urban and Rural Patients
155

Barut, MU., Agacayak E., Bozkurt M., Aksu T., Gul T.,
2016. There is a positive correlation between
socioeconomic status and ovarian reserve in women of
reproductive age, Med Sci Monit; 22: 4386-4392
Bennett, LR., Wiweko, B., Hinting, A., et al., 2012.
Indonesian infertility patients’ health seeking behaviour
and patterns of access to biomedical infertility care: An
interviewer administered survey conducted in three
clinics, Reprod Health; 9: 1.
BKKBN., 2017. Survei Demografi dan Kesehatan
Indonesia (SDKI) 2017. Jakarta.
Chin, HB., Kramer, MR., Mertens, AC., Spencer, JB.,
Howards, PP., 2017. Differences in Women's Use of
Nedical Hepl for Becoming Pregnant by the level of
urbanization of county of residence in Georgia, J Rural
health ;33(1):41-49.
Deatsman S; Vasilopoulos T; Vlasak AR., 2016. Age and
Fertility: A Study on Patient Awareness, JBRA Assisted
Reproduction; 20(3): 99-106.
Domar, AD., Penzias, A., 2005. The stress and distress of
infertility: Does religion help women cope?., Sexuality,
Reproduction & Menopause;3(2):45-51.
Ethics Committee of the American Society for
Reproductive Medicine (ASRM)., 2015. Disparities in
access to effective treatment for infertility in the United
States: An Ethics Committee opinion, Fertil Steril; 104:
1104–1110.
Fauziah Y., 2012. Obstetri Patologi untuk Mahasiswa
Kebidanan dan Keperawatan, Nuha
Medika.Yogyakarta
Harris, JA., Menke, MN., Jessica, KH., Moniz, MH.,
Perumalswami, CR., 2017. Geographic access to
assisted reproductive technology health care in the
United Syayes: Population-based cross -sectional
study, Fertil Steril ;107(.4):1023-1027.
Harzif, AK., Santawi, VPA., ,Wijaya, S., 2019.
Discrepancy in perception of infertility and attitude
towards treatment options :Indonesian urban and rural
area, BMC Reproductive Health;16:126.
HIFERI., 2013. Konsensus Penanganan Infertilitas,
Himpunan Endokrinologi Reproduksi dan Fertilitas
Indonesia. Jakarta, edisi 1.
Ho, JR., Hoffman, JR., Aghajanova, L., Smith, JF.,
Cardenas, M., Herndon, CN., 2017. Demographic
analysis of a low resource, socioculturally diverse
urban community presenting for infertility care in a
United States public hospital, Contraception and
Reproductive Medicine ;2(17):1-9.
Inhorn, MC., Patrizio, P., 2014. Infertility around the globe:
New thinking on gender, reproductive technologies and
global movements in the 21st century, Hum Reprod
Update; 21: 411–426.
Insogna, IG., Ginsburg, ES., 2018. Infertility, Inequality,
and How Lack of Insurance Coverage Compromises
Reproductive Autonomy, AMA Journal of Ethics.;
20(12):E1152-1159.
Irianto, K., 2014. Panduan Lengkap Biologi Reproduksi
Manusia Untuk Paramedis dan Nonmedis, Alfabeta.
Bandung.
Kaur, M., Meena, KK., Meena, KL., Singh, K., et al., 2018.
Burden of infertility and its associated factors: A cross
sectional descriptive analysis of infertility cases
reported at a tertiary level hospital of Rajasthan,
International Multispecialty Journal of Health
;4(4):144-149.
Klitzman, R., 2018. Gatekeepers for infertility treatment?
Views of ART providers concerning referrals by non-
ART providers, Reproductive BioMedicine and Society
Online;5:17–30.
Kunicki, M., Lukaszuk, K., Liss, J., Jakiel, G.,
Skowronska., 2018. Demographic characteristics and
AMH levels in rural and urban women participating in
an IVF programme, Annals of Agricultural and
Environmental Medicine ;25(1):120-123.
Roudsari RL., Allan HT., 2011. Women’s Experiences and
Preferences in Relation to Infertility Counselling: A
Multifaith Dialogue, Int J Fertil Steril; 5(3): 158-167
Lakatos, E., Szigeti, JF., Ujma, PP., Sexty, R., Balog P.,
2017. Anxiety and depression among infertile women:
a cross-sectional survey from Hungary, BMC Womens
Health.;17(1):48.
Maxwell, E., Mathews, M., Mulay, S., 2017. The Impact
of Access Barriers on Fertility Treatment Decision
Making: A Qualitative Study From the Perspectives of
Patients and Service Providers, J Obstet Gynaecol Can
;1-8.
Ombelet, W., 2011. Global access to infertility care in
developing countries: a case of human rights, equity
and social justice, Facts, views Vis ObGyn; 3: 257–66.
Omu, FE., Omu, AE., 2010. Emotional reaction to
diagnosis of infertility in Kuwait and succesful client’s
perception of nurse’ role during treatment, BMC
Nurs.;18(9):5.
Peterson, MM., 2005. Assisted reproductive technologies
and equity of access issues, J Med Ethics ; 31: 280–285.
Rooney, KL., Domar, AD., 2018. The relationship between
stress and infertility, Dialogues Clin Neurosci; 20: 41–
47.
Roupa Z; Polikandrioti M; Sotiropoulou P; Faros E;
Koulouri A; Wozniak G; Gourni M., 2009. Cause of
Infertility in Women at Reproductive Age, Health
Science Journal; 3(2): 1-8.
Sadeghi, MR., 2015. Access to infertility services in middle
east, J Reprod Infertil; 16: 179.
Thompson, C., 2006. God is in the details: Comparative
perspectives on the intertwining of religion and assisted
reproductive technologies, Cult Med Psychiatry; 30:
557–561.
Turnip, A., Andrian, Turnip, M., Dharma, A., Paninsari, D.,
Nababan, T., Ginting, C.N., 2020. An application of
modified filter algorithm fetal electrocardiogram
signals with various subjects, International Journal of
Artificial Intelligence, vol. 18, no., 2020.
Udgiri, R., Patil, VV., 2019. Comparative Study to
Determine the Prevalence and Socio-Cultural Practices
of Infertility in Rural and Urban Field Practice Area of
Tertiary Care Hospital, Vijayapura, Karnataka, Indian
J Community Med ; 44(2):129–133.
HIMBEP 2020 - International Conference on Health Informatics, Medical, Biological Engineering, and Pharmaceutical
156

Wijaya ,C., Andrian, M., Harahap, M., Turnip, A., 2019.
Abnormalities State Detection from P-Wave, QRS
Complex, and T-Wave in Noisy ECG, Journal of
Physics: Conference Series, Volume 1230, (2019)
012015. doi:10.1088/1742-6596/1230/1/012015.
Distribution of stress level among infertility patients,
Middle East Fertility Society Journal; 22:145–148.
Wu, AK., Odisho, AY., Washington, SL., etal., 2014. Out-
of-pocket fertility patient expense: Data from a
multicenter prospective infertility cohort, J Urol;
191:427–432
Access Barriers of Infertility Services for Urban and Rural Patients
157
