
Alternative Approaches for Supporting Lattice-based Access Control
(LBAC) in the Fast Healthcare Interoperability Resources (FHIR)
Standard
Steven Demurjian
1
, Thomas Agresta
2
, Eugene Sanzi
1
and John DeStefano
3
1
Department of Computer Science & Engineering, University of Connecticut, 371 Fairfield Way, Storrs,
Connecticut, U.S.A.
2
Department of Family Medicine, University of Connecticut Health Center, 263 Farmington Avenue, Farmington,
Connecticut, U.S.A.
3
SMC Partners, LLC, 10 Columbus Boulevard,, Hartford, Connecticut, U.S.A.
Keywords: Healthcare, Multi-level Security, Lattice based Access Control, FHIR, Sensitivity Level.
Abstract: A major challenge in the healthcare industry is the selective availability, at a fine-grained level of detail, of a
patient’s data to the various clinicians, nurses, specialists, home health aides, family members, etc. where the
decision of who can see which information at which times is controlled by a patient. The information includes:
contact and demographics, current conditions, medications, test results, past medical history, history of
substance abuse and treatment, mental health information, sexual health information, records relating to
domestic violence, reproductive health records, and genetic information. To control sensitivity, multi-level
security (MLS) using lattice-based access control (LBAC) can be used to extend the traditional linear
sensitivity levels of mandatory access control with the ability to define a complex lattice of sensitivity
categorizations suitable for the wide variety of the aforementioned information types. This paper applies and
extends our prior work on multi-level security for healthcare using LBAC by exploring alternative approaches
to integrate this approach into the Fast Healthcare Interoperability Resources (FHIR) standard at the
specification level of the standard.
1 INTRODUCTION
One of the major challenges in the healthcare industry
is to ensure that a patient’s healthcare information is
securely accessible to a wide range of stakeholders
(e.g., physicians, clinicians, medical specialists,
nurses, non-medical staff, home health care
providers, pharmacists, patients, family members,
etc.) to administer patient care in a variety of settings
such as physician offices, hospitals, rehab facilities,
emergency rooms, home based care settings, etc. The
challenge from a data security perspective is to
provide fine-grained access control to a patient’s
healthcare information that is able to precisely define
which portions of the information should be available
to which stakeholders at what time. Granular sharing
of medical, health, and fitness data is becoming an
increasingly important aspect of patient care,
considering new government initiatives which aim to
broaden the sharing of a person’s health data beyond
traditional boundaries.
In this situation, the information that needs to be
controlled has many different levels of permissions
due to its sensitivity and confidentiality: controlled by
the various types and granularity of information to
which patients want to control access (Caine &
Hanania, 2013); providing fine grained access
control to allow a patient to define: who may
view/modify what (Sujansky, et al., 2010); and,
providing a way for patients to provide their data to
an emergency physician in time critical situations
(Peleg, et al., 2008). Of particular relevance, the work
of (Caine & Hanania, 2013) identified 11 medical
information items that are partitioned into 5 protected
items such as: contact information and demographics,
information relevant to current conditions,
medications (prescribed and over-the-counter), test
results (blood pressure, blood tests, imaging tests,
etc.), and past medical history; and, 6 sensitive items
such as: history of substance abuse and treatment,
Demurjian, S., Agresta, T., Sanzi, E. and DeStefano, J.
Alternative Approaches for Supporting Lattice-based Access Control (LBAC) in the Fast Healthcare Interoperability Resources (FHIR) Standard.
DOI: 10.5220/0010150800930104
In Proceedings of the 16th International Conference on Web Information Systems and Technologies (WEBIST 2020), pages 93-104
ISBN: 978-989-758-478-7
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
93

mental health information, sexual health information,
records relating to domestic violence, reproductive
health records, and genetic information.
Given the variety and scope of a patient’s
healthcare information, one security approach that
may address the granularity issue for fine-grained
control is multi-level security (MLS), which has its
origins in the lattice-based access control model
(LBAC) (Denning, 1976) and the mandatory access
control model (MAC) (Bell & LaPadula, 1976). Both
models rely on sensitivity levels (e.g., unclassified U,
confidential C, secret S, top secret TS, etc.) that are
assigned to objects (termed classifications) and users
(termed clearances). Access to objects depends on a
comparison of a user’s clearance against an object’s
classification based on the type of operation (read,
write, etc.). MAC utilizes a strict linear order while
LBAC utilizes a lattice.
In fact, our recent work (Demurjian et al., 2017)
explored the use of multi-level security for healthcare
using an LBAC approach to define five sensitivity
levels from least secure to most secure, further
subdivided by different categories to replace the four
traditional ones (TS, S, C, U):
Level 0: Basic Demographic Data such as
city, state, general health condition, fitness
data.
Level 1: Medical History Data such as patient
name, address, day/month of birth, weight,
height, next of kin, history, immunization,
and a separate mental health history.
Level 2: Summary Clinical Data such as R
x
and
OTCs, allergies, diagnoses, treatment plan,
and, for mental health, separate diagnoses,
and treatment plan.
Level 3: Detailed Clinical Data such as
imaging studies, laboratory tests, mental
health encounters (excluding psychotherapy
notes), and clinical data (e.g., heart rate,
blood oxygen level, blood pressure, etc.).
Level 4: Sensitive Clinical Data used by
medical specialists on genetics, substance
abuse, mental health psychotherapy notes,
reproductive health, and domestic violence.
Different categories of information at the same
sensitivity level can be authorized to users based on
required Level/Category combinations.
The main focus of this paper is to apply our prior
work (Demurjian et al., 2017) on multi-level security
for healthcare that we developed and explore
alternative approaches to integrate this approach into
Fast Healthcare Interoperability Resources (FHIR)
(HL7 International, 2020). FHIR provides structures
for sharing EHR data between healthcare providers.
Data is accessed through resources utilizing a
location URL as part of a REST API in conjunction
with a logical ID. This allows data that resources
describe to sync between separate FHIR systems. We
focus on the FHIR base resources (e.g., patients,
practitioners, and family relationships; organizations,
services, appointments, and encounters) and clinical
resources which are for a patient’s health history.
Note that these alternative approaches are described
at the specification level of the FHIR resources and
not from an implementation perspective.
The main objective of this paper is to explore the
utilization of our prior work (Demurjian et al., 2017)
on multi-level security for healthcare to incorporate
the lattice and our security approach into the
resources of FHIR. Section 2 provides background on
healthcare, multi-level security, and FHIR. Section 3
reviews our prior work in LBAC in the health care
domain. Section 4 applies our prior LBAC work to
FHIR by discussing the way that Level/Categories
can be assigned at the schema level to a resource and
its components. This includes exploring two
approaches that utilize various FHIR capabilities and
features and reviewing our LBAC implementation
strategy. Finally, Section 5 concludes our paper
.
2 BACKGROUND
This section provides background material on
concepts used in the rest of this paper. Section 2.1
reviews the different kinds of healthcare information
and systems. Section 2.2 briefly summarizes the
history of MLS as realized by the MAC and LBAC
access control models. Section 2.3 briefly reviews the
FHIR specification. Section 2.4 briefly discusses
multi-level security in healthcare.
2.1 Healthcare Information & Systems
Caine and Hanania (Caine & Hanania, 2013)
organized the recipients and information in the
context of patients managing and sharing their
medical data into 11 data items: contact information
and demographics, information relevant to current
conditions, medications, test results, past medical
history, history of substance abuse and treatment,
mental health information, sexual health information,
records relating to domestic violence, reproductive
health records, and genetic information. These data
categories have parallels to what we have loosely
characterized as medical/health/fitness data in this
paper. However, there are three categories of data
that we believe are missing from this list: fitness data
WEBIST 2020 - 16th International Conference on Web Information Systems and Technologies
94

collected by patients utilizing fitness devices and
mobile apps; medical data collected by patients using
their own medical devices and mobile apps; and,
medical data collected by patients at the direction of
their physician (e.g., Holter Cardiac Monitor) that
may record data or feed data to the physician via a
phone link, the web, or a mobile app. Thus, we
propose adding Patient-Supplied Fitness, Patient-
Supplied Medical, and Patient/Physician Directed
Medical data to this list.
This challenge of patients sharing information is
further complicated by the fact that a patient’s
healthcare information is stored in multiple locations
in a variety of health information technology (HIT)
that includes: electronic health records (EHRs),
practice management systems (PMS), e-prescribing
systems, personal health records (PHRs), etc. The
majority of these systems must adhere to various laws
such as the Health Insurance Portability and
Accountability Act (HIPAA) (HIPAA, 2017) for the
security, availability, transmission, and release of a
patient's medical information. The sharing of
information among multiple HITs is being facilitated
in part by the Fast Healthcare Interoperability
Resources (FHIR) (HL7 International, 2020)
standard, a health information exchange (HIE)
standard created by HL7 to promote secure sharing of
healthcare data among multiple HIT systems.
2.2 Multi-level Security and LBAC
LBAC (Denning, 1976) and MAC (Bell & LaPadula,
1976) share the approach of security sensitivity levels
that are assigned to subjects (clearance) and objects
(classification) with the permissions for the subject to
read and/or write an object based on the relationship
between clearance and classifications. MAC typically
is modelled using four sensitivity levels which are
hierarchically ordered from most to least secure: top
secret (TS) < secret (S) < classified (C) < unclassified
(U). LBAC generalizes this approach by ordering the
sensitivity levels in a lattice that determines the
relative ranking of each sensitivity level vs. the
others. Security policies in LBAC and MAC are
defined by a security administrator to control
information flow in computer systems where users
are prohibited from changing their security attributes.
In LBAC and MAC, access to objects (e.g., segments
of an XML document, tables in a database, etc.) by
subjects (e.g., users, processes in a system, etc.) is
granted based on the security definitions on the
targeted object (exhibited via tags) and the credentials
granted to the user.
From a definition and management perspective, a
security administrator would set the clearance level of
users following the predefined sensitivity levels (e.g.,
TS, S, C, and U) to establish the levels for both
subjects and objects. These levels are then augmented
on a user-by-user basis by assigning the ability to read
and/or to write an object. Once this has all been
established for an application, definition of
permissions and levels (e.g., the elements of a
patient’s health record) can be used to maintain
confidentiality by preventing an unauthorized
provider to access sensitive information (e.g., not all
medical providers are able to access mental health
history) and to prohibit a patient from changing their
own record. The use of multi-level security in the
traditional military context is directly analogous to its
application in healthcare. The major difference is that
the “sensitivity” of information in the traditional
military context relates to the risk to national security
of improper disclosure, while the “sensitivity” level
of patients’ medical information relates to the privacy
risk associated with release to unauthorized users.
In LBAC, the work of Denning (Denning, 1976)
on lattice-based access control defines a set of
security classes SC (analogous to security
classifications) that is then organized into a
universally bounded lattice that defines a partial order
across the set SC. Such a representation expands the
traditional DoD version of MLS so that a set of
security classification levels can be defined in a
complex lattice to represent a richer set of
relationships among various types of information
from a sensitivity perspective that are more conducive
to the complex and rich sensitivity of healthcare data.
The work of Landwehr (Landwehr, 1981) is a
comprehensive review of the formal models for
computer security circa 1981 and discusses both MLS
and lattice-based access control.
The lattice approach expands MLS by defining a
finite set of elements (security levels) that are
augmented with a partial ordering in order to define,
for each pair of elements, a least upper bound and a
greatest lower bound. The “compartment sets” can be
partially ordered with one another via subset
relationships, so that given two sets, one compartment
set is greater than or equal to another compartment
set. As a result, security classifications in MLS can
include not only a sensitivity level (top secret, secret,
confidential, etc.) but also a compartment set.
2.3 FHIR
FHIR enables the retrieval of healthcare data by
providing a common API to locate and exchange
Alternative Approaches for Supporting Lattice-based Access Control (LBAC) in the Fast Healthcare Interoperability Resources (FHIR)
Standard
95

healthcare records. FHIR’s data exchange structure is
built on the concept of resources, which provide a
meaningful set of healthcare related data concepts.
FHIR provides over 145 different resources for:
patients, observations, medications, patient consent,
etc. Requests for a specific resource are available
through a REST API that supports instance level
interactions such as: read, vread (version read),
update, patch (update a portion of a resource), delete,
and history interactions. FHIR resources are
organized in categories: foundation resources, base
resources, clinical resources, financial resources,
and specialized resources. We highlight only a subset
relevant for the paper. The base resources describe:
patients, practitioners, and family relationships;
organizations, services, appointments, and
encounters. The clinical resources are for a patient’s
health history, including: diagnostic data,
medications, care provision, and request/response
communication. HAPI FHIR (HAPI FHIR, 2020) is a
Java implementation of the FHIR specification. HAPI
FHIR provides resource models for all resources
defined in the current FHIR r4 specification.
Interactions with FHIR resources are defined by the
FHIR standard's REST API.
2.4 MLS in Healthcare
Despite the long history of MLS (since 1976) and its
wide usage in governmental and commercial settings,
there has been limited attention paid to the usage of
MLS for health care. A recent review of access
control models deployed by EHRs (Fernández-
Alemán, Señor, Lozoya, & Toval, 2013) found that
out of 35 articles, 27 specifically utilized RBAC. Our
own attempts to identify MAC examples in health
care found only three references. (Alhaqbani & Fidge,
2008; Gajanayake, Iannella, & Sahama, 2014;
Hafner, Memon, & Alam, 2007). In terms of the use
of MLS and MAC for security and privacy in health
care, a post in the Healthcare Exchange Standards
Blog (Moehrke, 2010) discussed the usage of the
traditional military classification scheme in a health
care setting. This work points to the definition of
confidentiality labels in HL7 standards that are part
of the vocabulary for FHIR HL7 (FHIR
Confidentiality, 2020). Specifically, in the HL7 FHIR
standard, the confidentiality labels are: U –
unrestricted, L – low, M – moderate, N – normal, R –
restricted, and V – very restricted. Note that the usage
of confidentiality levels in this standard denotes the
type of data to protect and the conditions under which
to protect that data; they are not the same as
sensitivity levels in MAC/MLS.
3 LBAC CLASSIFICATION FOR
HEALTHCARE
This section presents our work (Demurjian et al.,
2017) on an appropriate set of sensitivity labels for
the healthcare domain that can be utilized for both
classifications and clearances. As part of the process,
we demonstrate that the rich semantics of
health/medical/fitness data along with the varied
requirements of stakeholders, necessitates that we
move beyond a traditional linear-based MLS scheme
to one that is lattice-based. In the rest of this section,
a three-part approach is presented. First, we explain
and review lattice-based access control in detail
through a discussion of three key efforts (Denning,
1976; Landwehr, 1981; Sandhu, 1993). In the
process, we transition to an MLS schema that has
sensitivity levels, within each of which there may be
multiple different categories of data that are related to
one another in a lattice-based context. Second, we
propose a set of security levels and categories for
healthcare data to achieve a fine-grained security of
medical/health/fitness data per the items from Table
1 of Caine and Hanania (Caine & Hanania, 2013)
reviewed in Section 1. Once defined, these levels are
then organized into a lattice whose structure is
impacted by the way that medical stakeholders utilize
different categories of data within each level. The
sensitivity level lattice that is proposed is one
example of the way healthcare data could be
classified, but is not the only possible way to
characterize such data. The third part of this section
illustrates several alternative characterizations, which
we term Sensitivity Profiles. Each Sensitivity Profile
includes sensitivity labels that categorize
medical/health/fitness data in different ways that are
consistent with how information is utilized by
different stakeholders/HIT systems in different
contexts, easily understood by stakeholders, and
clearly connote the confidentiality of the different
types of healthcare information. Our premise is that it
is highly unlikely that one single, universal set of
sensitivity labels could be defined that would be
suitable for all of the possible use cases in healthcare;
as a result, we present alternate Sensitivity Profiles
and discuss the situation under which each would be
relevant in terms of the involved stakeholders and/or
HIT systems/health information exchange (HIE).
WEBIST 2020 - 16th International Conference on Web Information Systems and Technologies
96
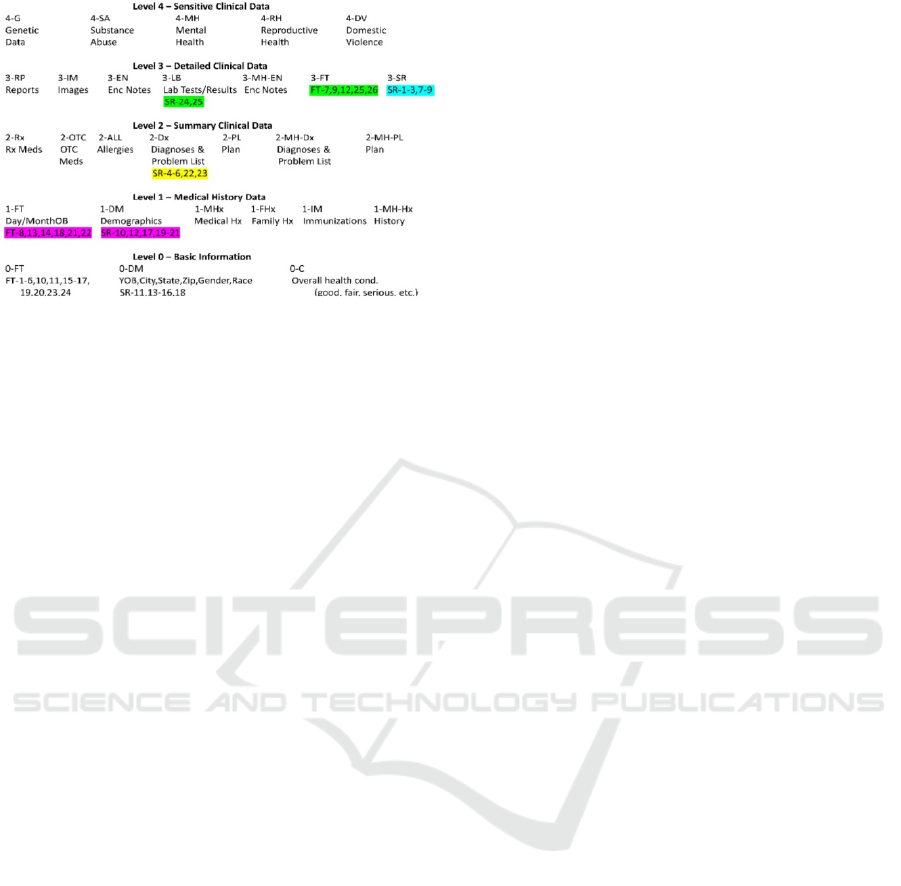
Figure 1: Sample Healthcare Sensitivity Levels.
The objective of this section is to propose and
discuss a set of sensitivity levels for labelling fine-
grained security of medical/health/fitness data per the
items in Table 1 of Caine and Hanania (Caine &
Hanania, 2013). The lattice to be presented in this
section is intended for use by healthcare organizations
(e.g., hospitals, clinics, medical specialist offices,
etc.) to securely share healthcare data via HIE with an
agreed upon set of security levels that are represented
by a lattice. To begin, Figure 1 defines a set of five
different sensitivity Levels (0 to 4) for healthcare, and
within each level there are different categories of data
that will be given to different users based on their
need. The five levels replace the four traditional ones
(TS, S, C, U) and are defined as:
Level 0: Basic Information contains data that is
freely available to anyone: basic
demographics such as city and state of
residence and surveillance data from (11,13-
16,18) (0-DM); general health condition (0-
C); and information related to tracking
fitness data (1-6,10,11,15-17,19,20,23,24)
(0-FT) such as date, time, type, and duration
of activity, etc.
Level 1: Medical History Data contains data
that has some restrictions: detailed
demographic data such as the patient name,
address, day/month of birth, weight, height,
next of kin, medical record ID of the patient,
surveillance data (10,12,17,19-21) (1-DM);
more sensitive patient-collected fitness data
(8,13,14,18,21,22); history of the patient and
his/her family, immunizations (1-MHx, 1-
FHx, 1-IM respectively); and mental health
history (1-MH-Hx).
Level 2: Summary Clinical Data including
prescription (2-Rx) and over-the-counter
medications (2-OTC), allergies (2-ALL),
medical diagnoses and problem list that
includes the provider name and ID and
surveillance data (4-6,22,23) (2-Dx), plan
for treatment or other related instructions (2-
PL), and, for mental health, separate
diagnoses (2-MH-Dx), and treatment plan
(2-MH-PL).
Level 3: Detailed Clinical Data contains
reports from imaging studies (CT Scans,
MRIs, X-Rays, etc.) (3-RP), the images
from the studies (3-IM), detailed
information on each medical visit (encounter
notes, 3-EN), laboratory tests ordered, dates,
and results including surveillance data from
(24,25) (3-LB), information about mental
health encounters (excluding psychotherapy
notes) (3-MH-EN), surveillance data (1-3,7-
9) (3-SR), and clinical data (e.g., heart rate,
blood oxygen level, blood pressure, etc.)
from fitness devices (7,9,12,25,26) (3-FT).
Level 4: Detailed Clinical Data contains
reports from imaging studies (CT Scans,
MRIs, X-Rays, etc.) (3-RP), the images
from the studies (3-IM), detailed
information on each medical visit (encounter
notes, 3-EN), laboratory tests ordered, dates,
and results including surveillance data from
(24,25) (3-LB), information about mental
health encounters (excluding psychotherapy
notes) (3-MH-EN), surveillance data (1-3,7-
9) (3-SR), and clinical data (e.g., heart rate,
blood oxygen level, blood pressure, etc.)
from fitness device (7,9,12,25,26) (3-FT).
Level 5: Sensitive Clinical Data contains
sensitive information used by specialists
including data on genetics (4-G), substance
abuse (4-SA), mental health psychotherapy
notes (4-MH), reproductive health (4-RH),
and domestic violence (4-DV).
Level 0 is the least secure, while Level 4 is the
most secure. Each of the levels have different
categories of information, that while at the same
sensitivity level as one another, have the ability to be
authorized to different users based on the
combination of Level/Category. This Level/Category
combination corresponds to the security
level/compartment as defined in Landwehr
(Landwehr, 1981). This was also shown in the
example of Figure 5, where S-LW represents the
combination of the S-L Level/Category and the S-W
category, combining the two categories of data (L and
W) within one level (S). In Figure 1, examples of
Level 2 categories are: prescription (2-Rx) and over-
Alternative Approaches for Supporting Lattice-based Access Control (LBAC) in the Fast Healthcare Interoperability Resources (FHIR)
Standard
97
the-counter medications (2-OTC), allergies (2-ALL)
and diagnoses/problems (2-Dx). In general terms,
Level 0 is public data available to anyone without
control, Level 1 is for use by administrative staff,
Level 2 is for use by clinical staff (RNs, PAs, etc.),
Level 3 is for use by medical providers, and Level 4
for is for use by specific medical specialists. A patient
would have access to all of the levels.
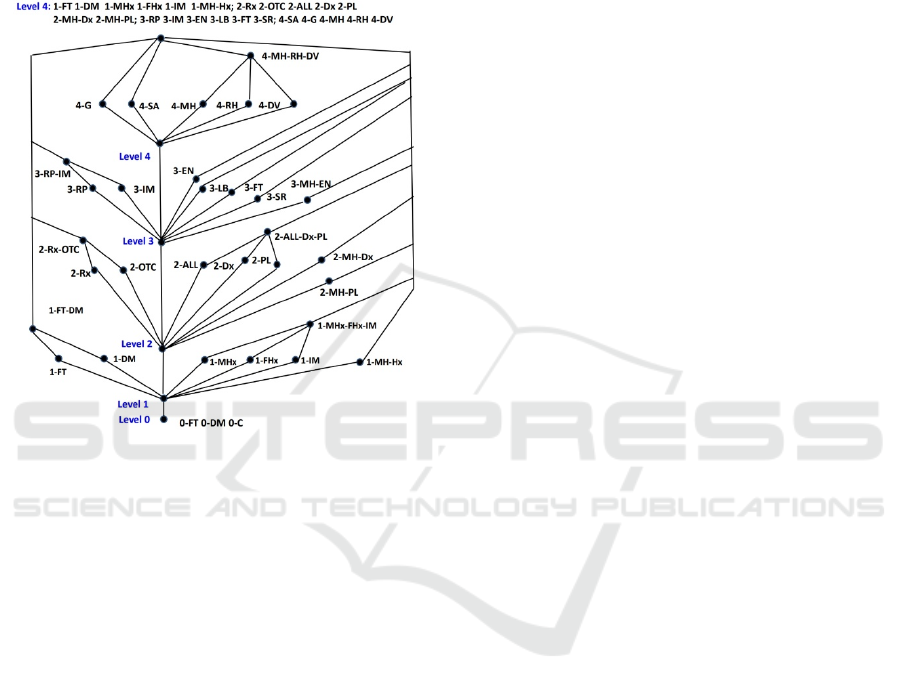
Figure 2: Corresponding Lattice based on Figure 1.
Figure 2 shows one possible lattice utilizing the
sensitivity levels and categories as given in Figure 1,
which is based on the work of Smith (Smith, 1990)
which defines a product lattice that combines ordered
security levels (i.e., TS, S, C, U) with eight different
categories of data (A, K, L, Q, W, X, Y, Z); note that
a category in this case is akin to a compartment as
described by Landwehr (Landwehr, 1981) and this
similar to our approach of sensitivity levels with
categories. In Figure 2, there are different
combinations of categories at each level that represent
the likely usage of that medical data by a particular
stakeholder. Starting from the bottom up in the figure,
notice that on the lower right-hand side for Level 1,
medical and family histories and immunizations are
grouped as: 1-MHx-FHx-IM. On the lower left hand
side, patient supplied fitness data and demographic
categories are grouped as: 1-FT-DM. For Level 2,
prescription and over-the-counter medications are put
together into the group 2-Rx-OTC with medical
plans, diagnoses, and allergies in a separate group 2-
ALL-Dx-PL. Some medical providers might have
access to medications (2-Rx-OTC) while others
might need access to both and would be assigned 2-
Rx-OTC and 2-ALL-Dx-PL. For Level 3, there is a
linking of imaging and the associated reports into the
group 3-RP-IM while information on encounter notes
and laboratory tests/results can be separately assigned
to a medical provider.
Access to summary mental health encounter
information (3-MH-EN) can also be separately
assigned. Finally, at Level 4, categories for mental
health psychotherapy notes, reproductive health, and
domestic violence are grouped into 4-MH-RH-DV
since a medical provider treating one of those
categories likely needs to know about the information
in the other two, but may not require access to genetic
or substance abuse data. Genetic (4-G) and substance
abuse (4-SA) categories can be separately assigned.
Note that in some cases, there may be a medical
provider that needs all five of the categories in Level
4. The top level collects all categories into one logical
unit. Two or more healthcare organizations (e.g.,
hospital A, hospital B, clinic C) that wish to securely
share information on patients could agree to use the
same set of sensitivity levels/categories (Figure 1)
and corresponding lattice (Figure 2). This is
analogous to DoD and federal organizations that
agree to (TS, S, C, U) in that setting. One final note is
that a recent article (Gajanayake, Iannella, & Sahama,
2014) on privacy for Electronic Health Records has
utilized the mandatory access control approach to
define an object sensitivity tree with allowed and
prohibited sensitivity labels where a user would
receive an aggregation of multiple allowed and
prohibited levels. While their approach is related to
our work it differs in that they are limited to a linear
ordering of MAC (not the lattice of LBAC) and didn’t
demonstrate as comprehensive a treatment of medical
data as given in Figure 1.
Given the lattice as presented in Figures 1 and 2,
the various Level/Category combinations can be
assigned to different users/stakeholders based on
individual needs. For example, all information in
level 0 is essentially public and freely available.
Administrative users such as office staff would have
access to level 0 as well as all of level 1 that includes
1-FT, 1-DM, 1-MHx, 1-FHx, 1-IM. Stakeholders that
are clinical staff (RN, LPN, etc.) for a given patient
would have access to levels 0 and 1, as well as 2-Rx,
2-OTC, 2-ALL, 2-Dx, and 2-PL. Stakeholders that
are part of the medical provider team (MDs) for a
given patient, would have access to levels 0, 1, and 2,
as well as 3-RP, 3-IM, 3-EN, 3-LB, 3-FT, and 3-SR.
Lastly, a specialist medical provider would have one
or more of: 4-SA, 4-G, 4-MH, 4-RH, and 4-DV. In
the last category, it may be necessary to protect
specific information by specialist, for example:
Protect mental health information: Eliminate 4-MH;
WEBIST 2020 - 16th International Conference on Web Information Systems and Technologies
98

Protect HIV information: Eliminate 4-RH; Protect
Genetic information: Eliminate 4-G; and, Protect
Substance Abuse information: Eliminate 4-SA.
In addition, the different mental health
information categories that exist from Level 1
through Level 4 provide the ability to tailor access to
sensitive mental health information for different
stakeholders. A psychiatrist would have access to: 1-
MH-Hx, 2-MH-Dx, 2-MH-PL, 3-MH-EN, and 4-
MH. This subdivision allows some of the mental
health information on lower levels to be available to
stakeholders that need access to lower level mental
health such as 1-MH-Hx and 2-MH-Dx but would not
be allowed access to other levels. The scenarios to be
presented in Section 5 include more detailed
examples of stakeholders and their necessary
permissions in regards to Level/Category
combinations of the Figure 2 lattice.
4 ALTERNATIVE APPROACHES
FOR LBAC AND FHIR
This section explores alternative approaches for
incorporating LBAC with Level/Category in Section
3 into FHIR. These approaches are at the level of the
specification with specific examples of FHIR
resources. Section 4.1 discusses the way that the
Level/Category can be assigned at the schema level
to a resource’s attributes, resources, and references to
other resources. The next two sections explore two
different approaches for including LBAC with
Level/Category, namely, FHIR Security Levels in
Section 4.2 and FHIR Extensions in Section 4.3.
Section 4.4 explores the various implementation
strategies that can be utilized in order to realize
LBAC within the FHIR framework. Note that all of
the information in Figures 3, 4 and 7, as well as other
FHIR examples are from publicly available freely
citable web pages of (FHIR resources, 2020).
4.1 LBAC & Resources Concepts
In this section, we explore the way that the different
FHIR resources can be labelled and classified using
the sensitivity levels in the categories in Figure 1. To
assist us in the process, Figure 3 contains the 145
currently defined FHIR resources. There are a
number of resources that are particularly relevant to
demonstrate five different sensitivity levels in Figure
1 and the way to position each of those resources in
one primary sensitivity level. FHIR Resources of
interest to us are:
Figure 3: Alphabetical List of Resources.
• Related to individuals: Person who is patient or
medical stakeholder; Patient who receives
medical services; Practitioner who is a physician,
visiting nurse, home health aide, etc.; and,
Organization that administers or provides
medical care.
• Related to a patient’s health record: Medication
tracks medications that a patient is taking or has
taken; AllergyIntolerance keeps tracks of any
allergies;
FamilyMemberHistory for personal
and family medical history; and, Immunizations
which tracks vaccines.
• Summary data: MedicationRequest to record a
prescription for a patient; Condition for the
different diagnosis for a patient; Observation that
keeps track of actual results of vital signs,
different types of tests, social history, etc.; and,
CarePlan to track the different plans among
medical stakeholders to manage care.
• Detailed clinical data on a patient: ImagingStudy
for the actual test results of an imaging study;
and, DiagnosticReport that contains information
on a patient's laboratory or other medical tests.
The remainder of this section explores the relevant
sensitivity level for a subset of the FHIR resources
shown in the previous bulleted list, and in the way that
the sensitivity of the resource itself, in terms of the
actual data stored for the resource, is interpreted.
To begin, we start with the first basic resource that
underlies all healthcare applications that are
developed using FHIR, the Person resource as given
in Figure 4 in the XML format. Note that in addition
to XML, a resource can also have a json and Turtle
format. The information in the Person resource has
basic name and demographic information, including
attributes for: identifier, name, gender, telcom,
birthdate, and active. The address attribute represents
Alternative Approaches for Supporting Lattice-based Access Control (LBAC) in the Fast Healthcare Interoperability Resources (FHIR)
Standard
99
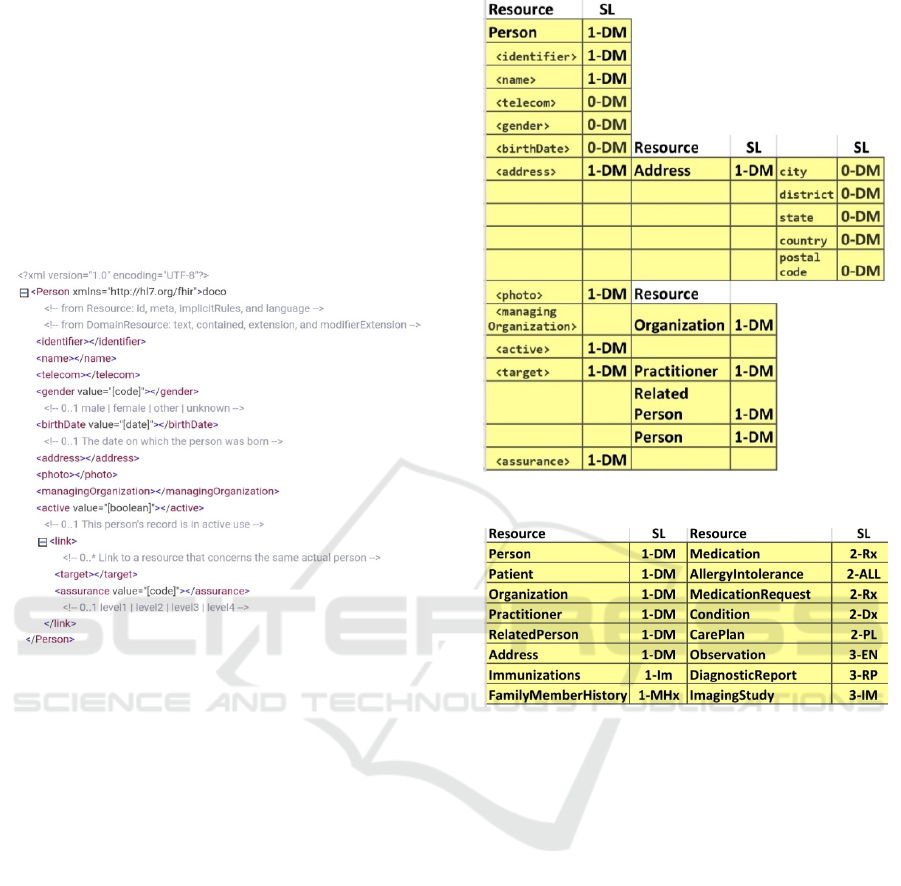
the inclusion of another resource, Address. The
managingOrganization attribute is a reference to 0 or
1 instances of an Organization resource and the
attribute target is a reference to one or more
Practitioner, RelatedPerson, or Person resource
instances who are involved with the Person. The type
of information that is included in the Person resource
is represented as sensitivity levels 1-DM and 0-DM
in Figure 2, representing the demographics from
levels 1 and 0 respectively. This means that a person
resource is primarily demographics information.
Figure 4: Person Resources in XML Format.
From a sensitivity Level and Category perspective,
we assign a level of 1-DM for the entire Person
resource, shown in Figure 5. This is a resource level
assignment of sensitivity coupled with the
demographics category. The 1-DM is utilized since
there is some information in the Person resource that
cannot be released to the general public. Within the
resource itself, each of the individual attributes can
have the same or lower sensitivity levels. Within the
Person resource, the embedded address resource's
attributes for city, district (county), state, country, and
postal code, would be tagged at sensitivity level 0-
DM, since this is public information that could be
utilized for statistical analysis of state and country
wide healthcare data. The sensitivity of the
managingOrganization attribute will be governed by
the sensitivity of the Organization resource, also 1-
DM, to allow information about an organization to be
protected. For the other Person attributes: date of
birth and gender are 0-DM, with all remaining
attributes defaulting to level 1-DM, which includes
references via the target attribute to the involved
Practitioner, RelatedPerson, or Person resource.
Figure 6 summarizes the sensitivity levels.
Figure 5: Sensitivity Levels (SL) for Person.
Figure 6: Sensitivity Levels (SL) of Select FHIR Resources.
4.2 Approach A: FHIR Security Labels
Approach A leverages the capabilities of the (FHIR
Security Labels, 2020) in an attempt to represent the
levels and categories of our LBAC approach using
the coding capabilities available in FHIR. One of the
capabilities of the FHIR security levels is the ability
to define confidentiality levels U – unrestricted, L –
low, M – moderate, N – normal, R – restricted, and V
– very restricted as discussed in Section 2.4 (FHIR
Confidentiality, 2020). Consider the example from
(FHIR Security Labels, 2020) on a patient resource
with a tag added with a confidentiality level of R.
While this could support the Level of our LBAC
approach, and we could map our five Levels it would
not be sufficient to support the Categories.
<Patient xmlns="http://hl7.org/fhir">
<meta>
<security>
<system
value="http://terminology.hl7.org/Code
System/v3-Confidentiality"/>
WEBIST 2020 - 16th International Conference on Web Information Systems and Technologies
100
<code value="R"/>
<display value="Restricted"/>
</security>
</meta>
... [snip] ...
</Patient>
One of the other capabilities that has the potential
to be leveraged as part of the standard is the HL7
Healthcare Privacy and Security Classification
System (HL7 HCS, 2020). The FHIR version of has
five different security labels: confidentiality
classification, sensitivity category, compartment
category, integrity category, and handling caveat; we
will focus on the first two that have been excerpted
from (FHIR Security Labels, 2020):
• “Confidentiality Classification: Security label
metadata classifying an IT resource (clinical fact,
data, information object, service, or system
capability) according to its level of sensitivity,
which is based on an analysis of applicable
privacy policies and the risk of financial,
reputational, or other harm to an individual or
entity that could result if made available or
disclosed to unauthorized individuals, entities, or
processes. Example Uses: Unrestricted, Normal,
Very restricted.”
• “Sensitivity Category: Security label metadata
that "segments" an IT resource by categorizing
the value, importance, and vulnerability of an IT
resource perceived as undesirable to share.
Example Uses: STDs, Psychiatric care, Celebrity
status.”
For confidential classification, the security label
has a cardinality of 0 or 1 which means it may or may
not be present; so a resource may have a classification
or may not. These are the confidentiality levels U, N,
R, etc. For the sensitivity category, the label has a
cardinality of 0 or multiple, may not be present, or
one or more. This gives the impression that the
sensitivity category potentially could be applied to
not only the resource but to different parts of the
resource, namely the attributes. This makes sense as
shown in our examples in Section 4.1, a given
resource might have different Level/Category
combinations at the attribute level.
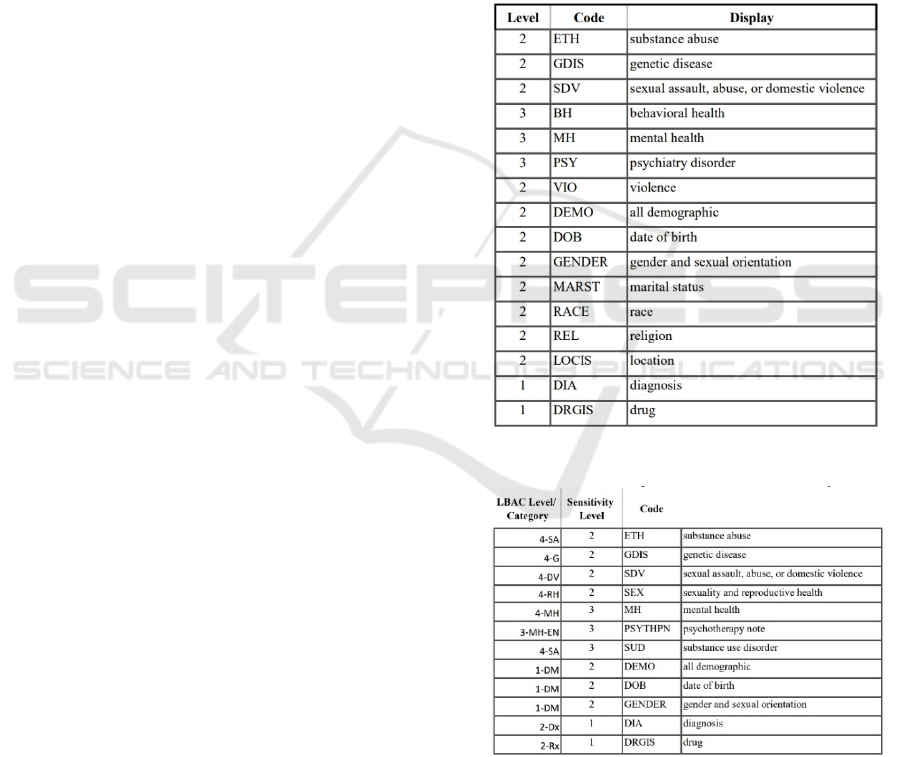
From a sensitivity Level and Category
perspective, we assign a level of 1-DM for the entire
Person resource, shown in Figure 5. The information
sensitivity labels have been excerpted from (FHIR
Information Sensitivity, 2020) and are shown in
Table 1. Notice that there are 4 sensitivity levels that
range from least sensitive 1 to most sensitive 4.
Notice that many of these information sensitivities
have parallels to our categories in Figure 1. So, it
would be possible to map the codes in Table 1 to the
categories in Figure 1. The issue is whether this
mapping will allow us to establish different codes for
each resource or even the attributes of each resource.
If it only works on the resource level this would not
be sufficient to support LBAC. To illustrate the
potential correlation between our LBAC and the
information sensitivity levels, Table 2 contains a
mapping between Figure 1 and a subset of Table 1.
Note that there was no obvious way to map all of our
Level/Categories in Figure 1 to all of the different
information sensitivity levels in Table 1; it not
feasible to realize FHIR Security Labels.
Table 1: Information Sensitivity Levels.
Table 2: Correlating LBAC with Information Sensitivity.
4.3 Approach B: FHIR Extensions
Approach B to integrating LBAC into FHIR utilizes
the extensions capability (FHIR Extensions, 2020)
which allows a resource to be modified with
additional features that then must be published with a
Alternative Approaches for Supporting Lattice-based Access Control (LBAC) in the Fast Healthcare Interoperability Resources (FHIR)
Standard
101

formal definition call and the structure definition to
be shared within the FHIR community. This allows
the extensions to be used by app developers and their
applications. In this section, we provide an extension
for supporting LBAC as presented in Section 3 in
Figure 7. The extension is meant to represent Level
and categories as given in Figure 1 such as 1-DM, 2-
Rx, 2-MH-Dx, etc. These strings of characters are
decomposed to be stored in the extension of the
resource. The top portion of Figure 7 is the structure
definition of the LBAC extension. You can see there
are two attributes in the extension: an integer level
with the value of 0 to 4 which represents the levels as
shown in Figure 1; and, a character string that can be
multiple characters and corresponds to the category
such as DM, Rx, etc.
<!-- LBAC FHIR Extension-->
<extension xmlns="http://hl7.org/fhir"
url="http://hl7.org/fhir/StructureDefinition/lbac" >
<extension url="level">
<valueInteger value=integer>
<!--value ranges from 0 to 4 -->
</extension>
<extension url="category">
<valueString=”[string]”/>
<!-- 1..* multiple characters -->
</extension>
</extension>
<!-- Person instance with extension-->and I
<?xml version="1.0" encoding="UTF-8"?>
<Person xmlns="http://hl7.org/fhir">
<extension xmlns="http://hl7.org/fhir"
url="http://hl7.org/fhir/StructureDefinition/lbac" >
<extension url="level">
<valueInteger value=1>
<!—Level 1 portion of 1-DM -->
</extension>
<extension url="category">
<valueString=”DM”/>
<!— Category DM portion of 1-DM -->
</extension>
</extension>
<id value="example"/>
<text>
<status value="generated"/>
<div xmlns="http://www.w3.org/1999/xhtml">
<table>
<tbody>
<tr>
<td> Name</td>
<td> Peter James <b> Chalmers</b>
<!—other data for person-->
</Person>
Figure 7: LBAC Extension and Person Instance.
The bottom portion of Figure 7 contains the
extension as applied to the Person resource instance,
which has the sensitivity level of 1-DM as was shown
in Figure 5. The extension goes at the top of the
resource instance, and a portion of the person instance
has been shown with the rest omitted. This LBAC
FHIR extension would have to be integrated into all
of the resources that you wish to control using LBAC
in your healthcare application. Of course, when this
is included in all of the different instances for your
application, the remaining issue is the required
implementation infrastructure that is necessary to
enforce LBAC for any given application, which is the
subject of Section 4.4.
4.4 LBAC Implementation Strategy
In this section, we report on the implementation
strategy for Approach B FHIR Extensions in Section
4.3 in two related areas:
1. An LBAC database component that is intended
to store the complete lattice for a given
application and specific user permissions to
access the resources.
2. An LBAC access control server that will be the
piece of software that interacts with HAPI FHIR
(HAPI, 2020), an open-source Java-based library
of the FHIR standard.
We review each of these components.
The LBAC database component will be the
repository that stores:
• The complete set of levels in all categories as
shown in Figure 1. This will require recoding all
of the different Level/Category combinations
such as 1-DM, 2-Rx, 3-MH-Dx, etc. into a
computer compatible form. For instance, the five
different levels from 0 to 4 can be given the
unique identifiers L0 to L4. Also, all of the
different strings that represent the categories can
be put into a table that maps each string to unique
category ID, e.g., table entry such as <C1, DM>,
<C2, Rx>, and <C3, MH-Dx>, etc. Finally, there
will be a separate mapping table with entries such
as [S1, L1, C1], [S2, L2, C2], and [S3, L3, C3],
where each of these combinations has been given
a unique identifier for sensitivity S, of which we
assume that there are n of them.
• The complete lattice as given in Figure 2 which
has the relationships among all of the
Level/Category combination sensitivity levels
from Figure 1. The application-specific lattice in
Figure 2 contains pairwise comparisons among
the S1, S2, ..., Sn sensitivities.
WEBIST 2020 - 16th International Conference on Web Information Systems and Technologies
102
• All of the complete permissions to the specific
Level/Categories from the lattice of Figure 2 that
have been authorized to the different users. As
previously stated this would include: Office Staff
1-FT, 1-DM, 1-MHx, 1-FHx, 1-IM; RN, levels
0 and 1, as well as 2-Rx, 2-OTC, 2-ALL, 2-Dx,
and 2-PL; MDs) levels 0, 1, and 2, as well as 3-
RP, 3-IM, 3-EN, 3-LB, 3-FT, and 3-SR; and,
psychiatrist 1-MH-Hx, 2-MH-Dx, 2-MH-PL, 3-
MH-EN, and 4-MH.
The LBAC access control server leverages the
capabilities of HAPI FHIR (HAPI, 2020) with a
HAPI-FHIR server that can be used in front of an
HIT. The HAPI-FHIR server architecture has two
main functionalities. First, a HAPI RestfulServer is a
Servlet that a developer utilizes to: create instances of
user-defined resource provider and, specify the
Servlet path. Second, a Resource Provider is a class
that represents one FHIR resource (e.g., Patient) that
has a number of empty annotated methods for CRUD
verbs that a developer needs to implement. These
empty annotated methods are utilized to parse HTTP
requests and convert the transferred data to/from
FHIR format/Back-end System format.
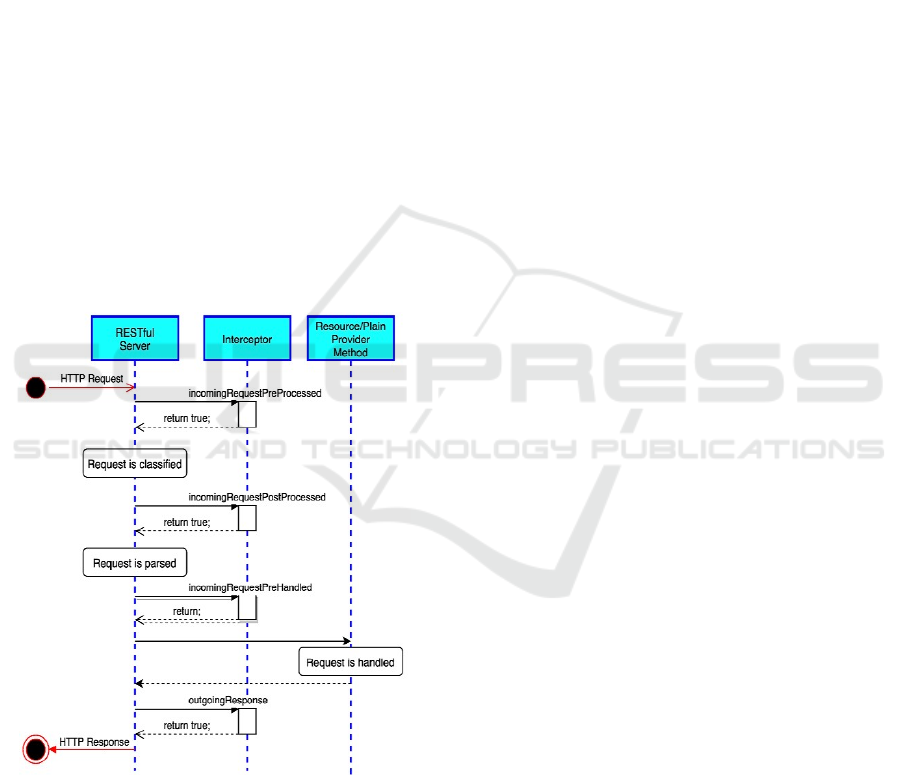
Figure 8: HAPI Interceptor Methods.
The HAPI-FHIR library provides a key capability
for supporting LBAC, specifically, a general HAPI
server interceptor in Figure 8 (HAPI Interceptor,
2016) which is a programmatic approach that allows
a developer to examine each incoming HTTP request
to add useful features to the HAPI RestfulServer such
as authentication, authorization, auditing, logging,
etc. The general HAPI interceptor, the
InterceptorAdapter class, defines a number of
methods that enable a developer to interact with the
incoming HTTP requests at different points of the
request lifetime. As Figure 8 shows, these methods
are: incomingRequestPreProcessed that is invoked
before performing any action to the request;
incomingRequestPostProcessed that is invoked after
determining the request type which classifies the
request; incomingRequestPreHandled which is
invoked before sending the request to the Resource
provider; and, outgoingResponse which is invoked
after the request is handled by the appropriate
Resource provider. Each of these methods must
returns either true, to continue processing the request,
or false, to abort and reject the request. Moreover, a
developer may extend the InterceptorAdapter class
and implement the needed methods and register the
extended class in the HAPI RestfulServer.
All of the capabilities of the interceptor can be
utilized to do the required LBAC permission checks
whenever a user is attempting to access a resource
that has been extended using our Levels and
Categories as discussed in Section 4.3. Specifically,
whenever there is an attempt to access a resource by
a health care application, the intercept capability
performs a LBAC security check to determine if the
user has the correct authorization to a subset of the
lattice to access the requested instance of the
resource. Recall the example from Section 3, an MD
for a given patient would have access to levels 0, 1,
and 2, as well as 3-RP, 3-IM, 3-EN, 3-LB, 3-FT, and
3-SR. That individual would have access to the
resources through LBAC authorization to those
Level/Categories. If the user attempted to access a
resource at the domestic violence 4-DV, they would
be denied. The interceptors can be utilized to ensure
that only those resources that have been authorized by
the lattice permissions can be returned to the user.
Note that we have utilized interceptors in our prior
research and have significant experience in their
usage (Rivera Sánchez, et al. 2019).
5 CONCLUSIONS
The paper has applied our prior work on multi-level
security using lattice-based access control (LBAC)
for healthcare (Demurjian et al., 2017) to the Fast
Healthcare Interoperability Resource (FHIR)
standard. Specifically, this paper: explored the
integration of our ideas into the resources of FHIR;
presented and discussed two different approaches,
FHIR Security Labels and FHIR Extensions, as
Alternative Approaches for Supporting Lattice-based Access Control (LBAC) in the Fast Healthcare Interoperability Resources (FHIR)
Standard
103

potential solutions for LBAC in FHIR; and, discussed
an LBAC Implementation Strategy that could be
actually utilized to realize a feasible solution. In
support of this work: Section 2 reviewed background
on healthcare, multi-level security, and FHIR;
Section 3 reviewed our prior LBAC approach for
healthcare; and, Section 4 discussed assigning
Level/Categories to a resource, explored the two
aforementioned approaches, and discussed our
current implementation strategy. The alternative
approaches presented in section 4 were described at
the specification level of the FHIR resources and not
from an implementation perspective.
REFERENCES
Alhaqbani B, Fidge C. Access Control Requirements for
Processing Electronic Health Records, Business
Process Management Workshops, AHM ter Hofstede,
B Benatallah, and H-Y Paik, (eds.), Springer, LNCS,
4928, 2008;371-382.
Bell, D. E., & La Padula, L. J. (1976). Secure Computer
Systems: Unified Exposition and Multics
Interpretation. Bedford, Mass.: MITRE Corp.
Caine K, Hanania R. Patients want granular privacy control
over health information in electronic medical records. J
Am Med Inform Assoc 2013;20(1):7-15.
Denning DE. A Lattice Model of Secure Information Flow,
Communications of the ACM 1976;19(5):236-243.
Department of Defense. Department of Defense Trusted
Computer System Evaluation Criteria 15 August
1983;23. Available at: http://csrc.nist.gov/
publications/history/dod85.pdf
Fernández-Alemán JL, Señor IC, Lozoya PÁO, and Tonal
A. Security and privacy in electronic health records: A
systematic literature review. J Biomed. Inform
2013;46(3):541–562.
Ferraiolo et al. (2001). Proposed NIST standard for role-
based access control. ACM Transactions on
Information and System Security (TISSEC), 4(3), 224–
274.
FHIR Confidentiality (2020). HL7 v3 Value Set
Confidentiality Classification. https://www.hl7.org/
fhir/v3/ConfidentialityClassification/vs.html
FHIR Information Sensitivity (2020). HL7 v3 Value Set
Information Sensitivity Policy. https://www.hl7.org/
fhir/v3/InformationSensitivityPolicy/vs.html
FHIR Resources (2020). https://www.hl7.org/fhir/
resourcelist.html
FHIR Security Labels (2020). Retrieved July 15, 2020.
https://www.hl7.org/fhir/security-labels.html
Gajanayake R., Iannella R., and Sahama T. (2014). Privacy
Oriented Access Control for Electronic Health Records,
Special Issue on e-Health Informatics and Security,
Electronic Journal for Health Informatics, 8(2),e15.
HAPI FHIR (2020). HAPI FHIR - The Open Source FHIR
API for Java. https://hapifhir.io/
HAPI interceptor (2016). University Health Network.
HAPI Server Interceptors. http://hapifhir.io/
doc_rest_server_interceptor.html
HIPAA (2017). Health Information Portability and
Accountability Act. http://www.hhs.gov/ocr/hipaa
HL7 HCS (2020). Healthcare Privacy and Security
Classification System. Retrieved July 15, 2020.
http://www.hl7.org/implement/standards/product_brief
.cfm?product_id=345
HL7 International. (2020). Index - FHIR v4.0.1.
http://hl7.org/fhir/
Landwehr CE, Formal Models for Computer Security,
ACM Computing Surveys 1981;13(3):247-278.
Moehrke J. Data Classification - a key vector enabling rich
Security and Privacy Controls, Healthcare Exchange
Standards Blog, August 10, 2010. Available at:
https://healthcaresecprivacy.blogspot.com/2010/08/dat
a-classification-key-vector-through.html
Peleg, M, et al. Situation-Based Access Control: privacy
management via modeling of patient data access
scenarios. J Biomed Inform 2008;41(6):1028-40.
Rivera Sánchez, Y.K., Demurjian, S., and Baihan, M.
(2019). A service-based RBAC & MAC approach
incorporated into the FHIR standard. Digital
Communications and Networks, 5(4):214-225,
Elsevier.
Ryutov et al. (2005). Adaptive Trust Negotiation and
Access Control. SACMAT '05 Proceedings of the tenth
ACM symposium on Access control models and
technologies (pp. 139-146).
Sandhu R. Lattice Based Access Control Model, IEEE
Computer 1993;26(11):9-19.
Smith, G. (1990). The Modeling and Representations of
Security Semantics for Database Applications.
Doctoral Dissertation, George Mason UUniversit
Sujansky WV, et al. A method to implement fine-grained
access control for personal health records through
standard relational database queries. J Biomed Inform
2010;43(5 Suppl):S46-50.
The Office of the National Coordinator for Health
Information Technology. (2018, September 19).
Meaningful Consent Overview | HealthIT.gov.
https://www.healthit.gov/topic/meaningful-consent-
overview
The Office of the National Coordinator for Health
Information Technology. (2019). Patient Consent for
Electronic Health Information Exchange |
HealthIT.gov. Retrieved January 24, 2020,
U.S. Department of Veterans Affairs - Office of Public and
Intergovernmental Affairs. (2019). VA achieves critical
milestone in its Electronic Health Record
Modernization Program. Retrieved January 4, 2020, t
Yasnoff, W. A. (2015). A Feasible and Sustainable
Approach to Health Information Infrastructure Via
Mobile Devices. http://mediasite.uchc.edu/media
site41/Play/b409b6fea70b4ec5b3fc34355340ac521
WEBIST 2020 - 16th International Conference on Web Information Systems and Technologies
104
