
Screening and Evaluation Platform for Depression and Suicidality in
Primary Healthcare
Fernando Cassola
1
, Alexandre Costa
1
, Ricardo Henriques
1
, Artur Rocha
1
, Marlene Sousa
2
,
Pedro Gomes
2
, Tiago Ferreira
2
, Carla Cunha
2
and João Salgado
2
1
INESC TEC - INESC Technology and Science, Porto, Portugal
2
ISMAI - Instituto Universitário da Maia, Maia, Portugal
Keywords: Web-based Platform, Decision Support, Screening, Healthcare, Depression, Suicide.
Abstract: This work presents a screening and evaluation platform for depression and suicidality that has been tested in
the scope of primary healthcare. The main objective is to improve the efficiency and effectiveness of screening
processes. A web-based, decision support platform was provided for qualified healthcare professionals. The
platform provides several assessment tools for patient evaluation and monitoring of their treatment, along
with follow up appointment management. A preliminary evaluation process was carried out to understand the
health professional’s satisfaction. This revealed there was general satisfaction with its integrated functions
and all the provided methods of assessment. In conclusion, the project sustains the goal of improving the
treatment outcomes for clinical depression by refining the screening methods and consequently increase the
screening effectiveness and efficiency.
1 INTRODUCTION
Available data indicates that the time period elapsed
between the first depressive episodes and the
respective diagnose by a clinician is about 4 years
(Almeida et al., 2013). Additional references
(Farvolden, McBride, Bagby, & Ravitz, 2003)
suggest that general practitioners fail to diagnose up
to half of the cases of major depressive disorder or
anxiety. On the other hand, depression is associated
with suicide, medical illness and increased risk of
accidental death (Fawcett, 1993).
Screening tools may help physicians and other
health professionals in primary health care to timely
recognize and adequately follow depressive disorder
and suicidality cases. The Stop Depression project
aims at aiding healthcare professionals in this task, in
order to provide a better response to the previously
identified weaknesses.
The StopDepression (“Stopdepression.pt,” 2017)
project (EEA GRANT 91SM3), supported by the
EEA Grants Iceland, Liechtenstein and Norway, is a
mental health project deployed in a primary care
setting (ACeS – Agrupamento de Centros de Saúde
do Porto Ocidental - Portugal). The main goal is to
improve the effectiveness of the means used for
detecting depression and managing the risk of
suicide. It’s an initiative inspired by the stepped care
model (Williams & Martinez, 2008) which has
specific objectives: detecting depression in early
stages, assessing suicide risk and improving the
patient’s treatment progress - based on web
technologies - always considering the severity and
symptomatology of each case.
To achieve these goals, a set of training sessions,
complemented by computer-based tools were
delivered to professionals. These have been applied
to face-to-face appointments to systematically
diagnose and thoroughly follow up the treatment of
depression. This paper describes the main software
pieces in the Stop Depression platform and how they
orchestrate in a computer aided diagnosis and
decision support solution.
2 RELATED WORK
In the last decades, several health organizations (e.g.,
United States Preventive Services Task Force
[USPSTF], 2002, 2016; World Health Organization
210
Cassola, F., Costa, A., Henriques, R., Rocha, A., Sousa, M., Gomes, P., Ferreira, T., Cunha, C. and Salgado, J.
Screening and Evaluation Platform for Depression and Suicidality in Primary Healthcare.
DOI: 10.5220/0006369002100215
In Proceedings of the 3rd International Conference on Information and Communication Technologies for Ageing Well and e-Health (ICT4AWE 2017), pages 210-215
ISBN: 978-989-758-251-6
Copyright © 2017 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
(World Health Organization, 2012); National
Institute for Health and Clinical Excellence [NICE],
2009), have been drawing attention to the importance
of improving detection and management of mental-
health problems such as depression.
One way to do this is by performing a systematic
screening and assessment of mental-health problems
in order to promote their adequate treatment (Siu et
al., 2016).
In this context, web-based screening platforms are
being developed and increasingly used for a variety
of mental-health problems (including depression and
suicidal risk) in various healthcare settings and
populations across the world (Farvolden et al., 2003;
Fothergill et al., 2013; Oromendia, Bonillo, &
Molinuevo, 2015).
For instance, the Web-Based Depression and
Anxiety Test (Farvolden et al., 2003) is a web-based
self-report screening instrument that has been used in
a rehabilitation centre in Toronto to effectively screen
for major depressive disorder and a number of
common anxiety disorders. Through this platform,
the healthcare professional has access to a report that
summarizes the person’s responses to several
questions elaborated according to the DSM-IV
criteria for these disorders (American Psychiatric
Association, 2000), which contributes to the
healthcare professional’s decision about the
diagnostic and treatment of the patients (Farvolden et
al., 2003).
Likewise, the Internet-based Behavioural Health
Screen (BHS) is a screening instrument that has been
developed by Diamond and colleagues (2010) to help
detect mental health problems and suicidal risk in
adolescents and young adults in a North-American
primary care. This tool facilitates healthcare
professionals the administration of several
questionnaires, as well as its interpretation and
integration (Diamond et al., 2010).
Also, the Integrating Mental and Physical
Healthcare: Training and Research (Matcham et al.,
2017) is a screening tool that has been used across two
London National Health Service (NHS) Trusts to help
detect depression, anxiety and the severity of nicotine
dependence in patients with chronic conditions. This
web-based platform helps not only the detection, but
also the management of these mental-health disorders
(Matcham et al., 2017).
A common trait among these platforms is that they
help healthcare professionals to perform screening
and diagnosis by integrating validated paper-based
psychometric measures (e.g., PHQ-9; Kroenke,
Spitzer, & Williams, 2001) that maintain good
psychometric properties when adapted to web-based
versions (van Ballegooijen, Riper, Cuijpers, van
Oppen, & Smit, 2016).
However, to our knowledge, although these
platforms are extremely useful tools, the majority
fails to provide healthcare professionals with case
management support information which is essential
for an effective approach to mental health care
(O’Connor, Whitlock, Gaynes, & Beil, 2009).
In order to pursue this goal, we analysed
requirements in the scope of the national context and
proceeded to the development of a case management
platform, which complements the ones previously
developed (Rocha et al., 2012; Warmerdam et al.,
2012) to support low intensity Internet-based
interventions.
The Stop Depression’s key contributions are: 1)
Integrating the screening and assessment of the
severity of depression and suicidal risk; and 2)
Providing healthcare professionals with suggestions
and guidelines for specific interventions based on the
assessment outcome, according to evidence-based
guidelines preconized by NICE (2010).
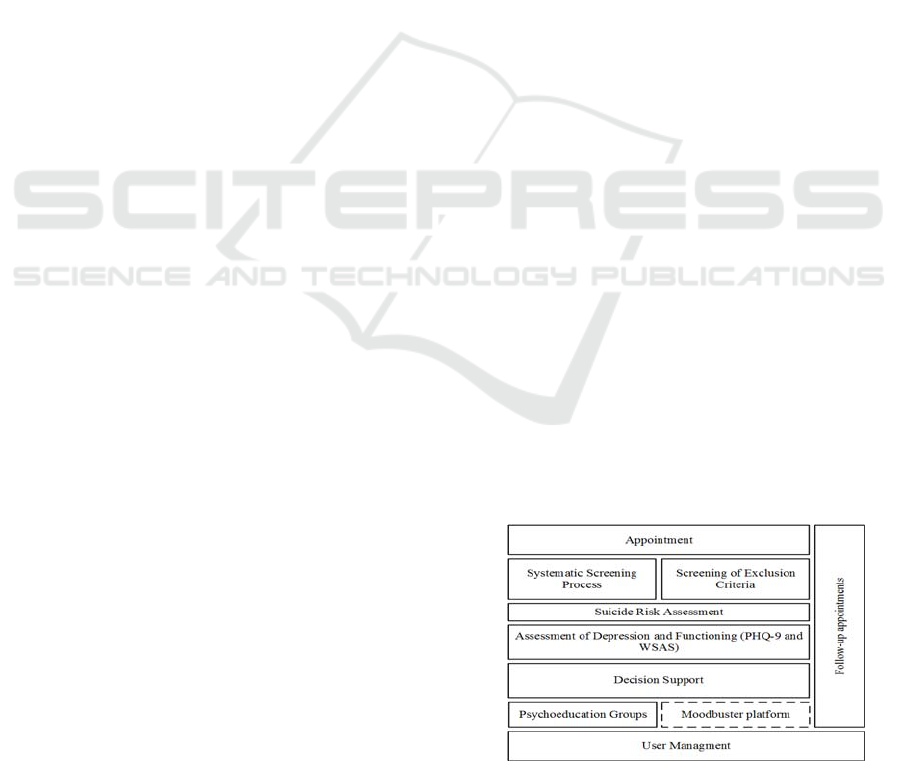
3 DESCRIPTION OF THE
PLATFORM COMPONENTS
The depression and suicidality evaluation platform
records the systematic screening, evaluation and
follow-up of patient’s depressive symptoms. This
takes place during their appointments in the primary
healthcare services. It includes a computer aided
diagnosis and decision support module that leverages
on the input from the remaining modules and its
progress over time to suggest an appropriate course
of action, based on a stepped care model. Figure 1
depicts the logical organization of the software
modules that were developed to achieve these goals.
The following subsections present a brief description
of modules implemented in the context of this project.
Figure 1: Stop Depression platform components.
Screening and Evaluation Platform for Depression and Suicidality in Primary Healthcare
211

3.1 User Management
Stop Depression is a pilot implementation project,
therefore this platform is not yet integrated with
SClínico (“spms.min-saude.pt,” 2017), the software
used by most of the primary healthcare institutions in
Portugal.
In order to deal with this challenge, the platform
includes functionalities to manage multiple user
profiles that are able to interact with different
functionalities. These users include medical doctors
and nurses which are able to screen and evaluate
patients; and psychologists that deliver interventions
to patients assigned to them.
From the technical point of view, an independent
structure was created to hold the subsect of health
records related with the patient mental health. Aside
from dealing with the necessary security issues by
means of authentication and access control over a
secure transport layer, particular attention was paid to
privacy, therefore no information that can directly or
indirectly identify the patient is ever stored.
3.2 Systematic Screening Process
Prior or during an appointment three straight
questions are prompted. Answers to these questions
are used to determine if a more thorough evaluation
should follow. The goal is to quickly detect the
presence of depression and eventual suicidal ideation.
3.3 Screening of Exclusion Criteria
This step narrows a particular disorder or ailments
that prevents the participation of the patient in this
study, such as heavily affected neurocognitive
functions that compromise interpretation abilities,
speech, social interactions and cognition. Psychotic
disorders, including schizophrenia, also fall out of the
spectrum of the study.
3.4 Suicide Risk Assessment
The goal of this process is to weight the factors that
impact the patient’s suicide risk (Jacobs et al., 2003).
The platform is able to draw an inference process to
suggest a treatment course that may address the
patient’s condition. It considers the patient’s
immediate safety as an active measure for critical
cases and suggests urgent procedures if needed.
3.5 Assessment of Depression and
Functioning (PHQ-9 and WSAS)
The Patient Health Questionnaire (PHQ-9)
assessment module is used to make a swift but
thorough assessment of the severity of depression and
has been validated for use in primary care services
(Cameron, Crawford, Lawton, & Reid, 2008). The
final score is computed by summing the value of
every answer and indicates the degree of depression.
This questionnaire can also be used to monitor the
patient’s progress recurrently, in order to evaluate
their progress.
Alongside PHQ-9, the patient fills in a
questionnaire aimed at measuring the impairment of
functioning. The Work and Social Adjustment Scale
(WSAS) helps to determine conditions or disorders
that may affect or deteriorate an individual’s abilities
to execute or participate in certain standard day-to-
day tasks (Mundt, Marks, Shear, & Greist, 2002). It
is also used as supplement with PHQ-9 to evaluate the
progress of the patient’s treatment.
3.6 Decision Support
Having completed the interview process, the platform
will show to the interviewer the calculated risk within
the suicide risk scale, which can be used as an aid for
suicide risk assessment. In addition, and depending
on the asserted risk, recommendations and
instructions on how to proceed according to different
degrees of severity are also suggested.
The platform evaluates the severity of depression
based on a weighted analysis of the PHQ-9 and
WSAS. It infers the degree of depression the patient
might have, along with a recommendation on how the
healthcare professional should proceed.
Any outcome presented in this section can’t be
seen as a prognostic, but rather a result of a computer
aided diagnostic tool, that can help the decision of a
qualified healthcare professional. Several important
dimensions not currently taken into account by the
decision support module need to be considered when
assessing depression degrees and suicide risks, such
as, the patient’s current physical state, medical health
history and other psychosocial grades (Williams &
Martinez, 2008).
From the technical perspective it represents a
classification problem. Health professionals have
defined screening rules to rate the patient into disjoint
groups. Said rules form the nodes of a decision-tree
classifier (Silberschatz, Korth, & Sudarshan, 2011).
ICT4AWE 2017 - 3rd International Conference on Information and Communication Technologies for Ageing Well and e-Health
212
3.7 Follow-up Appointments
Healthcare professionals register appointments
periodically, as a treatment monitoring process. This
include the reassessment of the PHQ-9 and WSAS
questionnaires, along with a re-evaluation of the risk
of suicide when necessary. The goal of this module is
to help determining the effectiveness of a treatment
and how well a patient is adapting to it.
3.8 Psychoeducation Groups
Psychoeducation groups are a form of psychotherapy
based on a shared therapeutic experience, which
involves the presence of a therapist, the patient and
other individuals working through similar ailments.
Therefore, group therapy considers the interaction
between group members as a vehicle of change
(Whitfield, 2010), which might play an important role
on the patient’s treatment progress.
The platform allows psychoeducation group
administrators to manage and schedule different
sessions, through the use of a calendar-like interface,
enabling them to choose which schedule best fits the
patient’s need.
3.9 Moodbuster Platform
When a patient is assigned to a computer based
treatment, the system will generate credentials that
allows the user to login on the moodbuster platform.
The moodbuster is an innovative digital solution for
the treatment of depression that is being used in a
follow-up study in a blended care setting. This an
Internet-based depression treatment that “is
considered a promising clinical and cost-effective
alternative to current routine depression treatment
strategies such as face-to-face psychotherapy”
(Kleiboer et al., 2016).
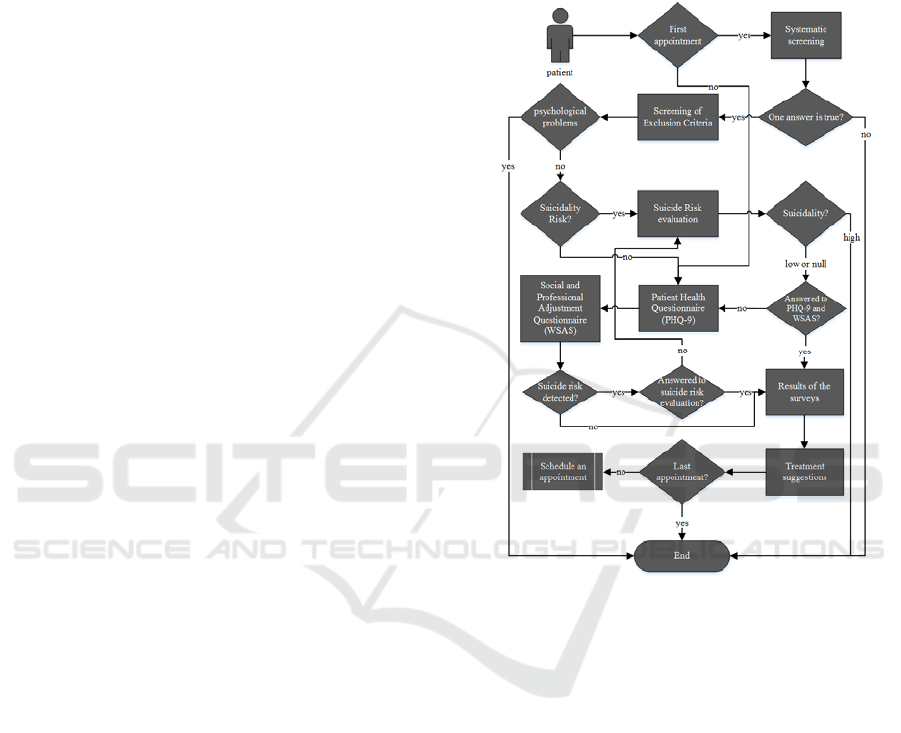
4 PLATFORM WORKFLOW
In the following section we expose the platform’s
workflow, and how appointments progress during an
interview with the patient. Figure 2 shows a
synthesised flowchart of this process.
When a patient attends a medical appointment in
the primary care, a healthcare professional checks for
previous records in the screening and evaluation
platform. If any is present, the professional is required
to repeat the PHQ-9 and WSAS questionnaires
(which may themselves trigger other instruments). On
the other hand, in the case of a first appointment, the
following steps of the screening and evaluation
workflow will happen.
The process begins with the systematic screening,
which may lead to the conclusion that no symptoms
of depression or suicide risk are present, then
resuming to the standard medical appointment.
Figure 2 - Platform Workflow.
If the systematic screening yields a possible
positive result for depression and suicide risk, the
platform will guide the professional through a list of
exclusion criteria. For instance: bipolar disorder,
borderline personality disorder, obsessive-
compulsive disorder, etc., including the suicide risk.
When the professional recognizes that the patient
presents one or more of these exclusion criteria, the
professional will step the patient out of the study,
while recording these results before resuming the
medical appointment.
When excluded due to risk of suicide, the platform
will point out the next steps based on the severity of
that assessment.
If the patient does not meet any exclusion criteria,
the results of PHQ-9 and WSAS instruments are used
to determine the severity of depression and the next
steps of its treatment. These steps also include the
schedule of follow-up appointments to assess the
progress of the patient’s mental health status.
Screening and Evaluation Platform for Depression and Suicidality in Primary Healthcare
213
In either case, the PHQ-9 includes a question to
acknowledge the risk of suicide. If detected, the
suicide risk is then reassessed in all subsequent
appointments.
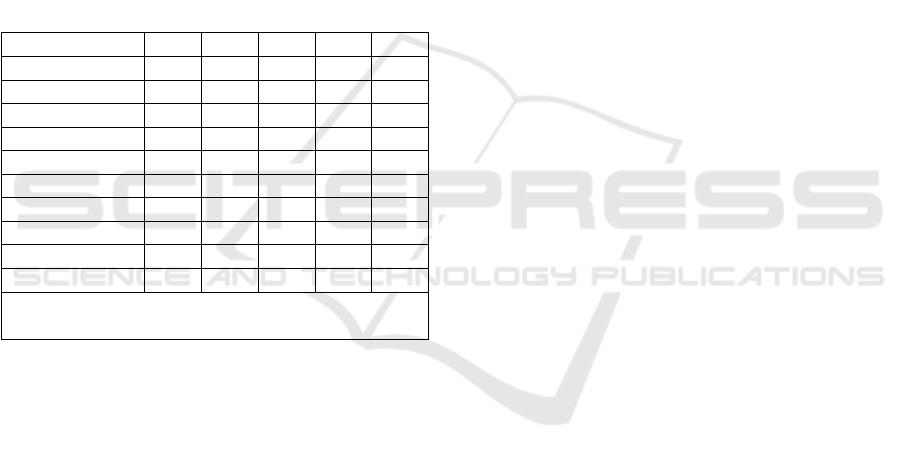
5 PRELIMINARY RESULTS
As a method for analysing user’s satisfaction, a
preliminary evaluation was carried out from a group
of 18 (eighteen) qualified health professionals
answering a System Usability Scale (SUS)
questionnaire (Brooke, 1996). This survey consists of
ten ranked questions that provide a measurement of
effectiveness, efficiency and satisfaction regarding
the platform’s use. All participants have received
training in using the platform.
Table 1: SUS results.
a b c d e
Will use frequently 0% 0% 6% 28% 66%
Is complex 33% 39% 11% 17% 0%
Easy to use 0% 0% 6% 44% 50%
Need help to use 44% 33% 17% 0% 6%
Integrated functions 0% 0% 17% 33% 50%
Has inconsistencies 33% 56% 11% 0% 0%
Easy to learn 0% 0% 28% 39% 33%
Is complicated 66% 22% 6% 6% 0%
Felt confidant 0% 0% 16% 56% 28%
Had a learning curve 28% 22% 28% 22% 0%
a- Disagree Completely; b- Disagree; c- Neither Agree nor
Disagree; d- Agree; e- Agree Completely
From the analysis of the collected data (Table 1),
it can be determined that 72% of the users agree that
the platform is easy to learn and 94% of them consider
it easy to use.
Furthermore, most users disagree that the system
had a steep learning curve. In terms of usability, 72%
users disagree that the platform is complex and 88%
disagree that it’s complicated.
A total of 89% of the users disagree that there are
inconsistencies with the user interface.
Most users felt confident interacting with the
platform, with 84% agreeing to this fact. This is
further emphasized by users agreeing that they did not
need help to use the platform, totalling 77%.
When it comes to integrated functions, 73% of the
users were satisfied with the tools provided and the
combined functionalities.
Finally, 94% of the users agreed that they would
definitely use the system frequently.
6 CONCLUSIONS
Stop Depression project’s main goal is to improve
clinical outcome when treating clinical depression. It
does so by broadening the screening process,
allowing early detection of depressive symptoms, and
by refining the treatment course, providing tools for
continuous monitoring of diagnosed patients.
This paper describes a state-of-the-art system for
mental health screening and assessment in the
Portuguese primary care, combining computer aided
diagnostic tools, along with other mechanisms such
as rule-based decision support (Abbasi &
Kashiyarndi., 2006), to empower health professionals
in determining the best treatment course and improve
treatment adherence. New, low intensity
interventions were made available in the scope of this
pilot, with the platform having a determinant role in
their implementation.
System usability surveys reveal that users were
pleased with the use of the system during the Stop
Depression clinical trials. Qualified users considered
the platform to be straightforward and with a low
learning curve, having felt confident while using it.
Moreover, an extremely high percentage of users
claimed that they would use the system frequently.
Although healthcare professionals seem to be
generally satisfied with the platform, more research is
currently undergoing to quantify the gains of using
the system from the clinical perspective.
Furthermore, extending the use of the system to other
institutions, particularly in the primary health care,
will likely require an impact analysis of its
interoperation or integration with the platforms
currently in use by the national health system.
ACKNOWLEDGEMENTS
This paper is financed by the ERDF – European
Regional Development Fund through the Operational
Programme for Competitiveness and
Internationalisation - COMPETE 2020 Programme
within project «POCI-01-0145-FEDER-006961»,
and by National Funds through the Portuguese
funding agency, FCT - Fundação para a Ciência e a
Tecnologia as part of project
«UID/EEA/50014/2013».
REFERENCES
Abbasi, M. M., & Kashiyarndi., S. (2006). Clinical
ICT4AWE 2017 - 3rd International Conference on Information and Communication Technologies for Ageing Well and e-Health
214

Decision Support Systems: A discussion on different
methodologies used in Health Care. Marlaedalen
University Sweden.
Almeida, J. M. C., Xavier, M., Cardoso, G., Gonçalves
Pereira, M., Gusmão, R., Corrêa, B., … António, J.
(2013). Estudo Epidemiológico Nacional de Saúde
Mental 1
o
Relatório. Faculdade de Ciências Médicas,
Universidade Nova de Lisboa.
American Psychiatric Association. (2000). Diagnostic and
statistical manual of mental disorders. Diagnostic and
Statistical Manual of Mental Disorders 4th edition TR.
https://doi.org/10.1016/B978-1-4377-2242-0.00016-X.
Brooke, J. (1996). SUS - A quick and dirty usability scale.
Usability Evaluation in Industry, 189(194), 4–7.
https://doi.org/10.1002/hbm.20701.
Cameron, I. M., Crawford, J. R., Lawton, K., & Reid, I. C.
(2008). Psychometric comparison of PHQ-9 and HADS
for measuring depression severity in primary care.
British Journal of General Practice, 58(546), 32–36.
https://doi.org/10.3399/bjgp08X263794.
Diamond, G., Levy, S., Bevans, K. B., Fein, J. A.,
Wintersteen, M. B., Tien, A., & Creed, T. (2010).
Development, Validation, and Utility of Internet-
Based, Behavioral Health Screen for Adolescents.
Pediatrics, 126(1).
Farvolden, P., McBride, C., Bagby, R. M., & Ravitz, P.
(2003). A Web-Based Screening Instrument for
Depression and Anxiety Disorders in Primary Care.
Journal of Medical Internet Research, 5(3), e23.
https://doi.org/10.2196/jmir.5.3.e23.
Fawcett, J. (1993). The morbidity and mortality of clinical
depression. International Clinical Psycho
pharmacology, 8(4), 217–20. Retrieved from
http://www.ncbi.nlm.nih.gov/pubmed/8277138.
Fothergill, K. E., Gadomski, A., Solomon, B. S., Olson, A.
L., Gaffney, C. A., dosReis, S., & Wissow, L. S. (2013).
Assessing the Impact of a Web-Based Comprehensive
Somatic and Mental Health Screening Tool in Pediatric
Primary Care. Academic Pediatrics, 13(4), 340–347.
https://doi.org/10.1016/j.acap.2013.04.005.
Jacobs, D. G., Ross Baldessarini, C. J., Conwell, Y.,
Fawcett, J. A., Horton, L., Meltzer, H., … Simon, R. I.
(2003). Practice Guideline for the Assessment and
Treatment of Patients With Suicidal Behaviors.
Kleiboer, A., Smit, J., Bosmans, J., Ruwaard, J., Andersson,
G., Topooco, N., … Riper, H. (2016). European
COMPARative Effectiveness research on blended
Depression treatment versus treatment-as-usual (E-
COMPARED): study protocol for a randomized
controlled, non-inferiority trial in eight European
countries. Trials, 17(1), 387. https://doi.org/
10.1186/s13063-016-1511-1.
Kroenke, K., Spitzer, R. L., & Williams, J. B. (2001). The
PHQ-9: validity of a brief depression severity measure.
Journal of General Internal Medicine, 16(9), 606–13.
Retrieved from http://www.ncbi.nlm.nih.gov/
pubmed/11556941.
Matcham, F., Carroll, A., Chung, N., Crawford, V.,
Galloway, J., Hames, A., … Hotopf, M. (2017).
Smoking and common mental disorders in patients with
chronic conditions: An analysis of data collected via a
web-based screening system. General Hospital
Psychiatry, 45, 12–18. https://doi.org/10.1016
/j.genhosppsych.2016.11.006.
Mundt, J. C., Marks, I. M., Shear, M. K., & Greist, J. M.
(2002). The Work and Social Adjustment Scale: a
simple measure of impairment in functioning. The
British Journal of Psychiatry, 180(5).
O’Connor, E. A., Whitlock, E. P., Gaynes, B., & Beil, T. L.
(2009). Screening for Depression in Adults and Older
Adults in Primary Care. Screening for Depression in
Adults and Older Adults in Primary Care: An Updated
Systematic Review. Agency for Healthcare Research
and Quality (US). Retrieved from http://
www.ncbi.nlm.nih.gov/pubmed/20722174.
Oromendia, P., Bonillo, A., & Molinuevo, B. (2015). Web-
based screening for Panic Disorder: Validity of a single-
item instrument. Journal of Affective Disorders, 180,
138–141. https://doi.org/10.1016/j.jad.2015.03.061.
Rocha, A., Henriques, M. R., Lopes, J. C., Camacho, R.,
Klein, M., Modena, G., … Warmerdam, L. (2012).
ICT4Depression: Service oriented architecture applied
to the treatment of depression. In Proceedings - IEEE
Symposium on Computer-Based Medical Systems.
https://doi.org/10.1109/CBMS.2012.6266379.
Silberschatz, A., Korth, H. F., & Sudarshan, S. (2011).
Database System Concepts - 6th. ed. Database (Vol. 4).
https://doi.org/10.1145/253671.253760.
Siu, A. L., Bibbins-Domingo, K., Grossman, D. C.,
Baumann, L. C., Davidson, K. W., Ebell, M., … B, D.
(2016). Screening for Depression in Adults. JAMA,
315(4), 380. https://doi.org/10.1001/jama.2015.18392.
spms.min-saude.pt. (2017). Retrieved January 31, 2017,
from http://spms.min-saude.pt/product/sclinicocsp/
Stopdepression.pt. (2017). Retrieved January 31, 2017,
from http://stopdepression.pt.
van Ballegooijen, W., Riper, H., Cuijpers, P., van Oppen,
P., & Smit, J. H. (2016). Validation of online
psychometric instruments for common mental health
disorders: a systematic review. BMC Psychiatry, 16, 45.
https://doi.org/10.1186/s12888-016-0735-7.
Warmerdam, L., Riper, H., Klein, M., van den Ven, P.,
Rocha, A., Ricardo Henriques, M., … Cuijpers, P.
(2012). Innovative ICT solutions to improve treatment
outcomes for depression: the ICT4Depression project.
Studies in Health Technology and Informatics, 181,
339–343.
Whitfield, G. (2010). Group cognitive–behavioural therapy
for anxiety and depression. Advances in Psychiatric
Treatment, 16(3).
Williams, C., & Martinez, R. (2008). Increasing Access to
CBT: Stepped Care and CBT Self-Help Models in
Practice. Behavioural and Cognitive Psychotherapy,
36(6), 675. https://doi.org/10.1017/S135246580
8004864.
World Health Organization. (2012). DEPRESSION A
Global Public Health Concern.
Screening and Evaluation Platform for Depression and Suicidality in Primary Healthcare
215
