
Healthcare Recommendations from the Personalised ICT Supported
Service for Independent Living and Active Ageing
(PERSSILAA) Study
Rónán O’Caoimh
1,2, 3
, D. William Molloy
1,2
, Carol Fitzgerald
1
, Lex Van Velsen
4,5
, Miriam Cabrita
4,5
,
Mohammad Hossein Nassabi
5
, Frederiek de Vette
5
, Marit Dekker-van Weering
4
,
Stephanie Jansen-Kosterink
4
, Wander Kenter
4
, Sanne Frazer
4
, Amélia P. Rauter
6
, Antónia Turkman
6
,
Marília Antunes
6
, Feridun Turkman
6
, Marta S. Silva
6
, Alice Martins
6
, Helena S. Costa
7,8
,
Tânia Gonçalves Albuquerque
7,8
, António Ferreira
6
, Mario Scherillo
9
, Vincenzo De Luca
10
,
Maddalena Illario
10
,
Alejandro García-Rudolph
11
, Rocío Sanchez-Carrion
11
,
Javier Solana Sánchez
12,13
, Enrique J. Gomez Aguilera
12,13
, Hermie Hermens
4,5
and Miriam Vollenbroek-Hutten
4,5
1
Centre for Gerontology and Rehabilitation, University College Cork, St Finbarrs Hospital, Cork City, Ireland
2
COLLaboration on AGEing, University College Cork, Cork City, Ireland
3
Health Research Board, Clinical Research Facility Galway, National University of Ireland, Galway, Ireland
4
Roessingh Research and Development, Enschede, Netherlands
5
University of Twente, Enschede, Netherlands
6
Fundação da Faculdade de Ciências da Universidade de Lisboa, Lisboa, Portugal
7
Instituto Nacional de Saúde Doutor Ricardo Jorge, IP, Lisboa, Portugal
8
REQUIMTE/LAQV, Faculdade de Farmácia da Universidade do Porto, Porto, Portugal
9
Nexera Centro Direzionale Isola, Napoli, Italy
10
Federico II University Hospital, Napoli, Italy
11
Institut Guttmann, Institut Universitari de Neurorehabilitació adscrit a la UAB, Badalona, Barcelona, Spain
12
Biomedical Engineering and Telemedicine Center. ETSI Telecomunicacion. Centre for Biomedical Technology,
Universidad Politécnica de Madrid, Madrid, Spain
13
Centro de Investigación Biomédica en Red, Biomateriales y Nanomedicina (CIBER-BBN), Zaragoza, Spain
Keywords: Frailty, Pre-frailty, Information and Communication Technology, Clinical, Healthcare Recommendations,
Guidelines.
Abstract: In the face of demographic ageing European healthcare providers and policy makers are recognising an
increasing prevalence of frail, community-dwelling older adults, prone to adverse healthcare outcomes. Pre-
frailty, before onset of functional decline, is suggested to be reversible but interventions targeting this risk
syndrome are limited. No consensus on the definition, diagnosis or management of pre-frailty exists. The
PERsonalised ICT Supported Service for Independent Living and Active Ageing (PERSSILAA) project
(2013-2016 under Framework Programme 7, grant #610359) developed a comprehensive Information and
Communication Technologies (ICT) supported platform to screen, assess, manage and monitor pre-frail
community-dwelling older adults in order to address pre-frailty and promote active and healthy ageing.
PERSSILAA, a multi-domain ICT service, targets three pre-frailty: nutrition, cognition and physical
function. The project produced 42 recommendations across clinical (screening, monitoring and managing of
pre-frail older adults) technical (ICT-based innovations) and societal (health literacy in older adults,
guidance to healthcare professional, patients, caregivers and policy makers) areas. This paper describes the
25 healthcare related recommendations of PERSSILAA, exploring how they could be used in the
development of future European guidelines on the screening and prevention of frailty.
O’Caoimh, R., Molloy, D., Fitzgerald, C., Velsen, L., Cabrita, M., Nassabi, M., Vette, F., Weering, M., Jansen-Kosterink, S., Kenter, W., Frazer, S., Rauter, A., Turkman, A., Antunes, M.,
Turkman, F., Silva, M., Martins, A., Costa, H., Albuquerque, T., Ferreira, A., Scherillo, M., Luca, V., Illario, M., García-Rudolph, A., Sanchez-Carrion, R., Sánchez, J., Aguilera, E., Hermens,
H. and Vollenbroek-Hutten, M.
Healthcare Recommendations from the Personalised ICT Supported Service for Independent Living and Active Ageing (PERSSILAA) Study.
DOI: 10.5220/0006331800910103
In Proceedings of the 3rd International Conference on Information and Communication Technologies for Ageing Well and e-Health (ICT4AWE 2017), pages 91-103
ISBN: 978-989-758-251-6
Copyright © 2017 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
91

1 BACKGROUND
With demographic ageing the number of older
Europeans, aged over 65 years, has increased
(Rechel, 2013), resulting in a higher prevalence of
frailty (Collard, 2012). Despite the lack of an
accepted definition most experts consider frailty to
be an age-associated loss of physiological reserve,
characterised by an increased vulnerability to
adverse healthcare outcomes (Sternberg, 2011),
(Borges, 2011), (Rodríguez-Mañas, 2013), (Morley,
2013).
Pre-frailty, is a prodromal ‘risk’ state before the
onset of frailty. However, no definition of pre-frailty
is yet available. Instead, a cut-off score on a frailty
screen or frailty assessment scale defines it as an
intermediate level before the development of
functional decline. The proportion of frail,
community dwelling older adults is variable
depending on the sample and setting surveyed but
can be as high as half (Collard, 2012). A greater
percentage, up to 60% of those aged over 65, can be
classified as pre-frail (Santos-Eggimann, 2009),
although again this depends on the approach used to
categorise pre-frailty (Roe, 2016).
While the development of frailty is often
considered permanent, some patients may convert
from frail to pre-frail and even become robust again
(Gill, 2006). Nevertheless, once established, frailty
is challenging or near impossible to reverse (Lang,
2009) with less than 1% of patients transitioning
back over five years of follow-up (Gill, 2006).
Given that the onset of frailty is associated with an
increased incidence of chronic medical conditions
(Gray, 2013), (Sergi, 2015), hospitalisation
(O’Caoimh, 2012a), (O’Caoimh, 2014a),
(O’Caoimh, 2015a), hospital readmission (Kahlon,
2015), healthcare costs (Robinson, 2011),
institutionalisation (Sternberg, 2013), and death
(Song, 2010), there is a need to promote active and
healthy ageing and instigate measures to prevent
frailty (Morley, 2013), (Bousquet, 2014),
(O’Caoimh, 2015b), (Fairhill, 2015), (Michel, 2016).
From a practical perspective targeting pre-frailty is a
reasonable approach. Specifically, the use of multi-
factorial interventions to screen, monitor and
manage prodromal states related to pre-frailty such
as subjective or mild cognitive impairment
(Fiatarone, 2014), (Ngandu, 2015), (O’Caoimh,
2015c), and reduced physical activity (Bherer,
2013), (Pahor, 2014) may be the best approach.
Likewise combinations of proactive, coordinated
and targeted interventions, delivered in the
community, can reduce adverse healthcare outcomes
among older adults (Beswick, 2008).
To date, few clinical trials have used frailty as an
outcome measure (Lee, 2012), examined whether
frailty can be prevented or studied whether directing
interventions towards pre-frail community-dwelling
older adults delays onset of frailty and functional
decline. Specifically, no study has examined the use
of a multi-domain, information and communications
technology (ICT) platform. Although several
national and international Geriatric Medicine
societies have provided best practice
recommendations for addressing frailty (Morley,
2013), (Turner, 2014), given the paucity of studies,
no guidelines exist for the management of pre-
frailty.
2 OVERVIEW OF THE
PERSSILAA PROJECT
The PERsonalised ICT Supported Services for
Independent Living and Active Ageing
(PERSSILAA) project is a small or medium-scale
focused research project, funded under the European
Commissions’ Framework Programme 7 (FP7)
(2013-2016, grant #610359). It consists of a
consortium of eight partners from five European
Union countries from across the social, medical and
technological sciences as well as industry, academia
and end-user organisations. The primary objective of
PERSSILAA was to develop an ICT-based platform
to identify and manage community dwelling older
adults at risk of functional decline and frailty. This
multimodal service model focuses on important pre-
frailty domains, namely: nutrition, cognition and
physical function. It is supported by an interoperable
ICT service infrastructure, using an intelligent
decision support system and gamification strategies
to encourage end-users to engage with the platform.
PERSSILAA was designed specifically for
community-dwelling older adults (aged >65 years)
who as part of the project were (1) screened using
continuous trained rater and or self-assessment
strategies to identify and stratify their “frailty level”,
(2) triaged to the appropriate ICT based solution to
meet their needs (targeting one, more or all three
frailty domains), (3) monitored (unobtrusively) and
(4) managed with ICT supported services through
local community services.
In summary, the intervention consisted of both
face-to-face and remote ICT components. Suitable
participants identified in one of the two evaluation
sites, Enschede, the Netherlands (older adults aged
65-75 recruited through primary care, selected by
their family doctor) and Campania, Italy (older
adults >65 recruited through local church
communities), were screened for frailty using a two-
ICT4AWE 2017 - 3rd International Conference on Information and Communication Technologies for Ageing Well and e-Health
92

step screening process. Once identified,
PERSSILAA services were used first to deliver
specific trainings modules for health and ICT
literacy and where appropriate, based on the
screening and triage component, to physical training,
cognitive training (Guttmann
NeuroPersonalTrainer®) and nutritional advice
(NUTRIAGEING
TM
website). The PERSSILAA
services are accessible and offered online via
personal or tablet computers so older adults can use
them independently. In addition to a standard
version there is also a gamified version which wile
designed to be fun and interactive, encourages
participation and compliance with the intervention,
something referred to as ‘serious gaming’. For
example in one version subjects are challenged to
build a boat to escape from a virtual island but can
only gather the pieces required by using the trainings
modules. Gamification encourages older people to
use telemedicine (de Vette, 2015) with a recent
systematic review showing that it generates more
engaging assessment strategies for cognition (brain
training), (Lumsden, 2016).
The PERSSILAA study investigated the extent
to which this ICT platform was first acceptable to
older adults, then efficacious and ultimately
effective in a real world setting, in preventing pre-
frail older adults from becoming frail. As this was an
evaluation rather than a validation study, the priority
was on demonstrating acceptability and proof of
concept. PERSSILAA services were studied in two
different communities of older adults in Italy and the
Netherlands. Two different evaluation studies were
performed. In Campania, a prospective cohort study
was conducted to examine the uptake, acceptability
and usability of the platform among older Italians. In
Enschede, a multiple cohort randomised controlled
trial (mcRCT) design was used recruiting 82
participants from several Dutch sites across the
region (46 of whom received the intervention). Cost
effectiveness was assessed with the Monitoring and
Assessment Framework for the European Innovation
Partnership on Active and Healthy Ageing tool
(Boehler, 2015) developed under the European
Innovation Partnership on Active and Healthy
Ageing (EIP on AHA). The PERSSILAA study was
funded for three years with the evaluation
component conducted over the last two years.
Subjects were consented and assessed at baseline,
scheduled intervals and the end-point. More details
of the project including a full list of publications are
available at www.perssilaa.eu.
3 RECOMMENDATIONS FROM
THE PERSSILAA PROJECT
Given the interdisciplinary nature of the
PERSSILAA project, the results derived from it are
multi-dimensional and can be broadly categorised
into three thematic areas: Healthcare related
recommendations, ICT-related recommendations
and Organisational (institutional) related
recommendations. This review summarises the
healthcare findings relating to the project.
To compile these, partners were grouped
according to their relevant specialty to develop
recommendations based on the work completed in
the preparation of the project including an expert
external review and the results emerging from the
project. Each component was evaluated separately
and once complete all partners provided feedback
and the recommendations were grouped as described
above.
There are several recommendations within each
theme. The results presented in this paper describe
the clinically relevant outcomes of the study and
how these could be used to contribute to the
development of European guidelines for the
screening of and prevention of frailty in older adults.
3.1 Definition of Pre-frailty
Although pre-frailty may be characterised as a
prodromal state before onset of frailty and
subsequent functional decline, no clear definition of
pre-frailty exists. Instead it is most often
characterised only as a transitional stage between
robust and frail states, measured by several short
frailty screens and defined by a cut-off score above a
robust level but below that for frailty. It is
acknowledged that there is a need to identify this
prodrome so that measures to effectively target
frailty can be developed (Fairhall, 2015). In order to
select a sample, the PERSSILAA investigators
produced a definition of pre-frailty following a
detailed state of the art literature review. After
reviewing several possible definitions, the
investigators developed a multi-domain definition
targeting the key frailty domains (nutrition,
cognition and physical function) of the project. As
several of the partners were involved in the EIP on
AHA A3 Action Group on frailty prevention (Illario
2016), the definition of pre-frailty was based upon
the A3 groups’ definition of frailty. This describes
pre-frail older adults those at increased risk for
future poor clinical outcomes, such as the
development of disability, dementia, falls,
hospitalisation, institutionalisation or increased
mortality as evidenced by the presence of one or
Healthcare Recommendations from the Personalised ICT Supported Service for Independent Living and Active Ageing (PERSSILAA)
Study
93
more prodromal frailty states (e.g. mild cognitive
impairment, sarcopenia, physical and functional
impairment, dysthymia and social isolation).
Recommendation: The EIP on AHA definition of
frailty could be adapted to define pre-frailty.
Recommendation: The EIP on AHA action group
A3 should take the lead in developing a definition of
pre-frailty, which could support and stimulate
debate on a consensus definition of this important
condition and public health priority.
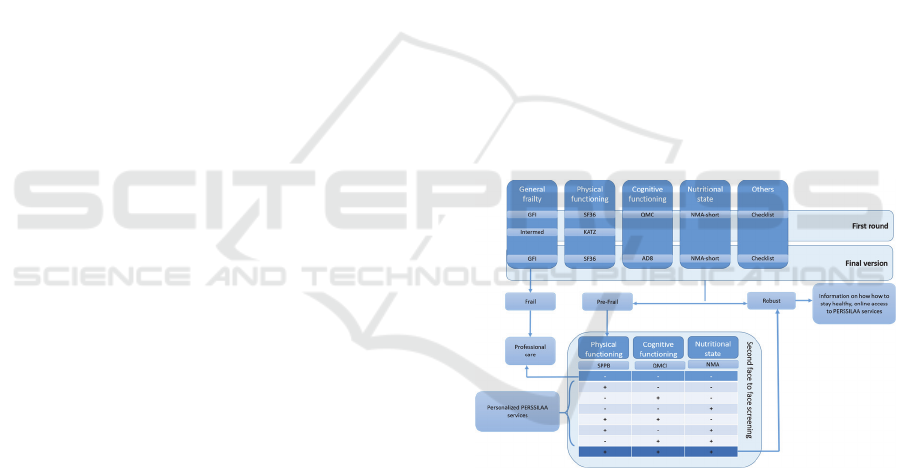
3.2 Screening for Pre-frailty
Multiple short frailty screening instruments are
currently available (de Vries, 2011), though no
single instrument is recommended (Morley, 2013).
Further, only a few scales are able to discriminate
the pre-frail. PERSSILAA was predicated on a two-
step screening and assessment approach in an
attempt to correctly categorise subjects as frail.
Staged screening followed by more comprehensive
assessment is recommended given the high
prevalence of pre-frailty in community samples and
the resources involved to screen in this setting (van
Kempen, 2015). Instruments were selected following
a literature review. This two-stage selection involved
(1) the screening of people aged 65 years and older
by trained volunteers/self-screening either by email
or postal questionnaire to exclude robust subjects
and those with established frailty and (2) a second-
level face-to-face assessment by multidisciplinary
staff of those classified as pre-frail in order to
confirm if they were pre-frail. Each of the three
domains included in PERSSILAA were screened
using this approach i.e. physical, nutritional and
cognitive pre-frailty. The specific instruments used
at each stage of the process are presented in Figure
1. During the first iteration (the first round) the
scales were rationalised resulting in a more
streamlined version (final version).
In summary, in the first step subjects were
divided into robust, pre-frail and frail using a
‘global’ frailty scale and individual measures of
nutrition, cognition and physical function. Two
‘global’ instruments were initially selected (1) the
Groningen Frailty Indicator (GFI), a 15-point yes-no
questionnaire exploring physical, cognitive, social
and psychological components of frailty taking a
cut-off of ≥4/15 for moderate-severe frailty
(Steverink, 2001) and (2) the INTERMED (self-
rated version) screen, a reliable, self-administered
20-question survey covering biological,
psychological, social factors and the extent of recent
healthcare usage (Peters, 2013). As the INTERMED
did not provide sufficient additional information,
only the GFI was used in the final version, as it was
shorter, validated in the languages of the project and
easier to use. Participants were further screened
using instruments specific to the selected pre-frailty
domains using appropriate cut-off scores. The final
instruments selected were the Mini-Nutritional
Assessment (MNA) short form for nutrition, the 8-
item Alzheimer’s disease 8 questionnaire (AD8) for
cognitive impairment (Galvin, 2005) and the Short-
form 36 questionnaire (SF-36) for physical
impairment. The KATZ activities of daily living
(ADL) scale and Quick Memory Check (QMC) were
initially trialled in the ‘first round’ (see Figure 1) but
were felt to be impractical for self-screening.
In the second step (face-to-face assessment),
older adults were assessed to confirm if they were
pre-frail. Nutritional deficits were identified using
the remainder of the MNA (G-R), mild cognitive
impairment was identified with the brief Quick Mild
Cognitive Impairment (Qmci) cognitive screen
(O’Caoimh, 2012), (O’Caoimh, 2013), (O’Caoimh,
2014a), (Bunt, 2015), (O’Caoimh, 2016), using age
and education adjusted cut-offs, (O’Caoimh, 2017),
and a short physical performance battery (using the
Timed Up-and-Go Test, the Two-Minute Step Test,
the Chair-Stand Test, and the Chair-Sit-and-Reach
Test) were used for physical function.
Figure 1: Two-step screening protocol for the
PERSSILAA project showing the first and final version of
the first screening step.
The results showed that the two-step
PERSSILAA screening-service, when combined
with additional demographic data seems a good
method to quickly and accurately classify
community-dwelling older adults into robust, pre-
frail and frail. In all, 4071 participants were pre-
screened (step one). The majority of these
participants were classified as robust (60%) at first
step screening. A further 916 (23%) were
characterised as having a high probability of being
pre-frail and suitable for further assessment (step
ICT4AWE 2017 - 3rd International Conference on Information and Communication Technologies for Ageing Well and e-Health
94

two). The second face-to-face screening confirmed
that of these 90% were pre-frail.
Receiver operating characteristic curve analysis
showed that the marker of nutrition, the MNA, was
the most accurate predictor of pre-frailty (area under
the curve of 0.80). Logistic regression was used to
confirm whether those screening positive were truly
pre-frail and showed that the first-step screening
process had an overall good to excellent accuracy
(area under the curve of 0.87 with a sensitivity of
77% and specificity of 84%). Further analysis of the
second level assessment showed a good agreement
among the classifications of pre-frail and robust
individuals. Thus, the results suggest that the two-
step screening approach developed as part of the
PERSILLAA is able to correctly categorise pre-frail
community-dwelling older adults.
Recommendation: Pre-frailty should be
considered a multi-domain, multi-factorial
syndrome.
Recommendation: Several, different pre-frailty
sub-domains should be addressed when screening
for and assessing pre-frailty among older adults and
should include cognitive, physical, nutritional and
social domains.
Recommendation: More research is required in
this area and future studies should capture multiple
pre-frailty domains along with global measures of
frailty.
Recommendation: A two-step screening
approach is an acceptable and accurate means to
identify pre-frailty in a community setting, though
more research to confirm this approach is required.
3.3 ICT Training Modules to Manage
Pre-frailty
Three training modules were developed as part of
PERSSILAA, one for each of the three domains
targeted by the project: nutrition, cognition and
physical function. This section outlines how each
module was developed, the results of their
implementation, the conclusions drawn by the
PERSSILAA researchers and the recommendations
made. This section also puts a special emphasis on
health literacy, an important and often overlooked
element in the care of older adults. It also includes a
preliminary analysis of the effects of the training
platform on quality of life.
3.3.1 Nutrition Training Module
Nutrition plays an important role across the life span
but especially for older adults. Among community-
dwelling older people between 10-35% are
undernourished i.e. at risk of malnutrition (Schilp,
2012) or malnourished (Shakersain, 2016). The
prevalence can reach 45% in hospital (O’Shea,
2016) and between 30%-65% for those in
institutionalised care (Pauly, 2007) though figures
vary by setting and sample characteristics. The cause
is often inappropriate food consumption (van
Staveren, 2011), manifest by a gap between actual
nutrient consumption and recommended dietary
intakes. Education on healthy eating and nutrition is
important to provide adequate and reliable
information to consumers to promote healthy diets.
The NUTRIAGEING website
(http://nutriageing.fc.ul.pt/) is an easy-to-use, “app-
like” interface with minimal menus or other clutter
designed to promote translate scientific knowledge
into usable person-centred nutritional advice for the
general public. It’s three areas are: (1) Healthy
eating, (2) Recipes and videos, and (3) Vegetable
gardens. The “Recipes and videos” subsection
includes 15 videos of recipes developed by the
famous Portuguese Chef Hélio Loureiro. The
functionality of the website was tested in two day
care centres in Portugal with 45 older adults and
their caregivers. In free text feedback sessions,
participants rated the site as excellent but noted that
ICT bridging science and public knowledge such as
the NUTRIAGEING
TM
website should be: (1) easy
to use, (2) evidence based and evaluated by experts
and (3) have their contents presented in an appealing
and enjoyable format to encourage access and
learning.
Recommendation: Nutritional education,
required to promote healthier eating habits among
the general population and in particular pre-frail
older adults, can be delivered successfully online.
Recommendation: Educating caregivers on the
benefits of nutrition using ICT-supported platforms
such as the NUTRIAGEING
TM
website is important
and may benefit older adults directly – more
research is required to confirm this.
Recommendation: Educating cooks and
professionals involved in food preparation on the
benefits of healthy foods and nutrition using ICT
supported platforms such as the NUTRIAGEING
TM
website is important and may benefit older adults
directly – again research is required to confirm this.
Healthcare Recommendations from the Personalised ICT Supported Service for Independent Living and Active Ageing (PERSSILAA)
Study
95

Recommendation: ICT platforms, if user friendly
and intuitively designed, can provide the general
population but also older persons and healthcare
professionals with reliable information and easy-to-
use tools, which may increase their knowledge of
nutrition and healthy eating.
3.3.2 Cognition Training Module
Demographic ageing is associated with an increased
prevalence of cognitive impairment including mild
cognitive impairment (Plassman, 2008) and
dementia (Prince, 2013). Recent data suggest that
the incidence (Satizabal, 2016) and prevalence
(Matthews, 2013), (Langa, 2016) of dementia may
be falling in developed countries, possibly reflecting
improved education, socioeconomic factors and
cardiovascular brain health, all of which may
contribute to cognitive reserve (Norton, 2014).
Further, studies trialling multi-domain interventions
targeting at risk populations show that cognitive
stimulation when deployed with other lifestyle
measures and cardiovascular risk-factor assessment
and treatment may reduce progression to dementia
(Ngandu, 2015), Cognitive training, often called
‘brain training’ typically involves guided practice on
a set of standardised tasks designed to reflect
particular cognitive functions.
In PERSSILAA the mean AD8 score for the
total sample of 4,071 participants screened at step
one was 0.66±1.22 compared to 1.03±1.28 for pre-
frail older adults. A score of two or greater is
suggestive of cognitive impairment (Galvin, 2005),
though specificity is low at this cut-off (Larner,
2015). The mean Qmci score of pre-frail participants
at the second step was 64.5/100 ±11.32, within the
accepted range of cut-off scores for separating mild
cognitive impairment from normal cognition:
between 64 and 70/100 (O’Caoimh, 2017).
Over the course of the evaluation, pre-frail older
adults were asked to complete the cognitive training
modules over 12 weeks, 3 times per week with each
session designed to last one hour. The cognitive
training tasks were selected from the Guttmann
NeuroPersonalTrainer® and incorporated into the
platform in two blocks. The first group (Block 1)
were assessment-oriented tasks and the second
group (Block 2) training-oriented tasks. Block 1 was
composed of 10 different tasks, Block 2 25 tasks.
Both groups of tasks cover the main cognitive
functions involved in ADL. The therapeutic range
was set between 65%-85% and difficulty levels were
adjusted up/down if the number of correct
answers/responses were less or exceeded this.
Cognitive training was trialled in both evaluation
sites. In Enschede (Netherlands) 18 older adults
participated individually completing a total of 893
tasks during 107 sessions. In Campania (Italy) 53
participated in 15 collective (group) sessions: a total
number of 223 individual log in’s. Usability testing
performed in both regions showed satisfactory
results. In the Netherlands eight participants were
tested, ten in Italy. The mean score across both sites
on the system usability scale (SUS), a subjective 10-
item Likert scale measuring usability (Brooke,
1996), was 64/100 suggesting that the cognitive
training was usable. Based upon the results the
following recommendations were made:
Recommendation: Cognitive training tasks for
use with pre-frail older adults should be easy to
understand and use. Important information should
be provided in a large, conspicuous, non-crowded
format in the person’s central visual field.
Recommendation: The visual display on
cognitive training devices for pre-frail older adults
should be simple; avoiding distracting visual stimuli
(such as elaborate backgrounds and flashing or
flickering lights) unless they are used judiciously to
signal a specific required action or function.
Recommendation: Clear instructions should be
provided to pre-frail older adults before each
cognitive training task, particularly where
additional effort is required on behalf of the end
user (e.g. sustained attention tasks).
Recommendation: Immediate feedback should
always be provided to pre-frail older adults after
completing individual cognitive training activities.
Aggregated information should also be provided to
show trends or evolution in performance over time.
Recommendation: The difficulty of cognitive
training tasks for pre-frail older adults should be
tailored to each individual’s level based upon
normative data for these tasks.
Recommendation: Cognitive training modules
for pre-frail older people should be adapted to
mobile/smart technologies and devices. Engagement
with training should be encouraged with techniques
such as gamification or through the use of group
work (either remotely or at centralised locations).
Recommendation: Fields that represent pre-frail
older adults’ interests or hobbies should be used
throughout cognitive tasks (in the form of images,
texts, words etc.) to personalise the experience for
older adults
.
ICT4AWE 2017 - 3rd International Conference on Information and Communication Technologies for Ageing Well and e-Health
96

3.3.3 Physical Training Module
Frailty and pre-frailty are associated with
sarcopenia, osteopenia and osteoporosis that
contribute to adverse outcomes such as falls and hip
fractures (Liu, 2015). Regular physical activity,
particularly resistance exercises, may prevent onset
of frailty (Liu, 2011). Data also suggests that
exercise interventions can improve ADL function
among frail older adults and delay progression of
functional impairment or disability (Giné-Garriga,
2014). The Otago Exercise Programme (OEP), an
established, validated, cost-effective home-based
tailored falls prevention programme (Robertson,
2001), reduces the risk of falls and mortality among
community-dwelling older adults (Thomas, 2010),
though it is unknown whether it can be used
remotely by pre-frail older patients.
A technology-supported self-management,
physical training module platform, based on the
OEP, was developed for use on the PERSSILAA
platform. This was structure around an existing
platform called the Condition Coach (CoCo) for
patients with Chronic Obstructive Pulmonary
Disease (Tabak, 2014), containing advice and
instructional videos, which was reconditioned for
use with pre-frail older through a iterative design
approach until a final version was released. A more
extensive description of the development of the
physical module is presented elsewhere
(Vollenbroek-Hutten, 2015).
Participants using the physical training module
were requested to train online three times a week for
three months. Few participants dropped out mainly
due to their own health problems, which prevented
them from exercising. Initial technical problems e.g.
with browsers were resolved by setting up a
helpdesk. Of the participants finishing the complete
protocol (i.e. 12 weeks of training), the majority
continued using the service for up to one year. Most
who used the module were very satisfied and
evaluated the module as excellent, scoring a mean of
84/100 on the SUS. In the mcRCT the mean values
of the Chair Stand Test and Two minutes step test
increased for those using the physical training model
compared to controls.
Recommendation: Strategies to motivate pre-
frail older adults to begin and to continue using
physical training modules on ICT supported
platforms should be included as part of the
implementation process.
Recommendation: A ‘home’ online physical
training module provided on an ICT supported
platform is feasible for pre-frail older adults, though
professional support seems useful and should be
provided as back up.
Recommendation: The provision of physical
training modules on ICT supported platforms to pre-
frail older adults, at risk of frailty or functional
decline may enable them to improve their physical
fitness.
3.3.4 Health and ICT literacy
As older adults represent the fastest growing section
of our population and the biggest users of healthcare,
insufficient attention is paid to their understanding
of health literature. It is known that simple measures
can rapidly improve older person’s understanding
(Manafo, 2012). This also applies to eHealth literacy
skills (Norman, 2006). In PERSSILAA health and
ICT literacy programmes were developed in Italy.
This worked on a train the trainer model with
healthcare experts teaching local volunteers. In all
2,560 older adults attended classes, with a mean
attendance of 13.5 older adults per lesson. Feedback
was excellent and older adults reported in
subsequent surveys that they required this education
in order to interact with the training and monitoring
modules (see Section 3.5)
3.4 Effects on Quality of Life
Frailty has a negative impact upon quality of life
(Strawbridge, 1998). At the beginning of the project
a survey conducted with participants suggested high
levels of loneliness and depressive symptoms. In all,
73% reported feeling empty and 74% mow mood or
depressive symptoms. Thus, in addition to the pre-
frailty screening and assessment scales, the
European Quality of Life–5 Dimensions
questionnaire or EQ-5D (Euroqol), scored from 0
(worst imaginable health state) to 100 (best
imaginable health state), was used to measure the
effects of the PERSSILAA training modules on
quality of life. This was also included to facilitate an
economic analysis of the cost effectiveness of the
project. The EQ-5D was measured at baseline and
end-point for those participating in the mcRCT. The
final mean score increased compared with the initial
assessment by a mean of 10 points suggesting that
those using PERSSILAA reported a higher quality
of life after using the platform. The Short-Form 12
(SF-12), which includes physical and mental
domains taken from the SF-36 was used to measure
perceived health. Higher scores were found on the
Mental Component Survey of the SF-12 for those
using PERSSILAA training services compared to
the control group, suggesting that better mental
health is associated with the used of the platform.
Healthcare Recommendations from the Personalised ICT Supported Service for Independent Living and Active Ageing (PERSSILAA)
Study
97
Recommendation: Engaging in online mulit-
domain training modules to manage pre-frailty may
improve the perceived quality of life of older adults.
3.5 Monitoring for the Development of
Frailty – Frailty Transitions
Studies of frailty trajectories show that few older
adults can transition from frail to pre-frail or robust
(Gill, 2006). These have been limited by the type of
data available, which relies on face-to-face
assessment. While technology is suggested to allow
for unobtrusive monitoring, it may distract end-users
and lead to ‘attention theft’, necessitating a more
non-invasive approach in the home environment,
particularly when daily activities are being measured
(Bitterman, 2011). Further, while useful with
younger adults, it is unclear if such models are
applicable to community-dwelling older adults.
While older adults do engage with ICT, its uptake is
low (Selwyn, 2003). Older people perceive ICT to
be of little utility and frequently rank their
technology skills as low (Scanlon, 2015). Further, it
is challenging to combine all the information
collected in a meaningful way in order to obtain an
overview of the everyday functioning of pre-frail
older adults.
Different approaches to monitoring were used in
PERSSILAA depending on the pre-frailty domain
assessed. To facilitate monitoring software was
provided on the portal and on mobile and home
sensing devises. All data were collected
automatically and uploaded into the PERSSILAA
database for analysis. Transitions between different
frailty states (robust, pre-frail and frail) were
examined using the GFI data at baseline and end-
point. To monitor nutrition two questionnaires were
placed on the PERSSILAA portal to evaluate eating
habits: the 24-hour dietary recall and an additional
‘general’ questionnaire developed by the
PERSSILAA investigators. To supplement this, a
‘smart scale’ (weighing scale connected wirelessly
to a computer application) was chosen to monitor
weight on a daily basis. For cognition a shorter
version of the full Guttmann
NeuroPersonalTrainer® was developed to enable
monitoring of cognitive function over time in short
sessions of less than 15 minutes comparing each
score with baseline and the previous results. For
physical function a step counter was chosen to
monitor daily physical activity and obtain an
overview of physical functioning, all collected by
means of a smartphone application. Wellbeing was
also measured daily using a smartphone application
recorded. The acceptability of the monitoring
module was evaluated through semi-structured
interviews and by measuring how frequently the
technology was used over one month.
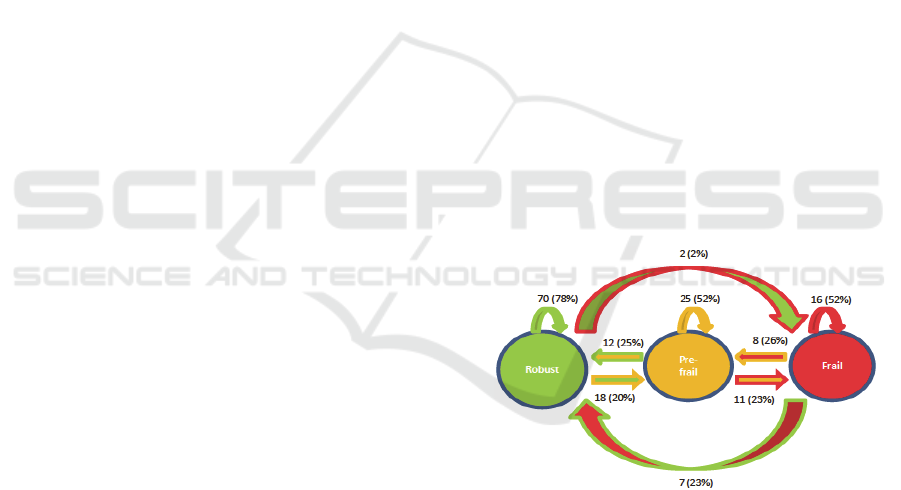
In all, 169 participants had completed the GFI at
baseline and end-point at the last follow-up. Of
these, 78% remained robust, while half remained
pre-frail or frail. One quarter transitioned from frail
to pre-frail and from pre-frail to robust. One fifth
converted from pre-frailty to established frailty.
These data are presented in Figure 2. The proportion
transitioning is higher than that reported previously
and likely represents differences in the way that data
is collected and a shorter period of follow-up. There
was no difference in overall ‘global’ frailty status as
measured by the GFI between those included in the
mcRCT as cases utilising the PERSSILAA training
modules and pre-frail controls, p<0.05. Twelve
community-dwelling older adults participated in the
monitoring feasibility sub-study. At baseline each
was surveyed to determine their self-reported
familiarity, comfort and level of daily use of ICT.
Over the following month their daily weight and
physical activity were measured and monitored
using the ‘smart scale’ and pedometer provided. At
the end a semi-structured interview was conducted.
Overall, compliance was modest with participants
stressing that ICT monitoring devices should be
designed with their needs in mind. Participants
stated that they were knew that maintaining a
healthy weight has benefits and enjoyed access to
healthy recipes.
Figure 2: Frailty transitions (n=169) for participants with
baseline & end-point Groningen Frailty Indicator scores.
Examining the cognitive domain, it was found
that older adults also enjoyed the ‘brain training’
games but do not want to be confronted or compared
with the results of peers. Likewise, older adults
stated that physical activity is important for overall
health.
These approaches to continuous ICT monitoring
showed mixed results and confirmed that older
adults while keen to engage technology for the
betterment of their health will only do so when it is
acceptable to them. Future studies should be
designed to study the effects and ultimately
ICT4AWE 2017 - 3rd International Conference on Information and Communication Technologies for Ageing Well and e-Health
98

incorporate health and ICT literacy in their designs.
Striking the balance between non-invasive
monitoring that is non-obtrusive and avoids
‘attention theft’ and more obvious strategies that
increase awareness of the need to engage with ICT
to prevent frailty and subsequent functional decline
will be the challenge.
Recommendation: There is likely to be no ‘one-
size-fits-all’ approach to monitoring older
community dwellers for pre-frailty. However, ICT
training is required for older adults in order for
them to engage with monitoring, particularly where
end-user feedback is required.
Recommendation: Monitoring of everyday
function must be complemented by meaningful
(older adult-specific) information to support the
adoption of healthier behaviours.
Recommendation: Technology to support the
prevention of functional decline must go beyond the
disease oriented-perspective and focus, instead, on
strategies to maintain independence in daily
activities.
Recommendation: When remotely monitoring
older adults health (pre-frailty) status using ICT
technologies, systems should provide feedback on
the data collected.
4 CONCLUSIONS
The results of the three-year, FP7 funded,
PERSSILAA project show the potential to use an
ICT-based, multi-domain service module to target
pre-frail older adults at risk of becoming frail and
developing functional decline. These results discuss
the healthcare recommendations that can be drawn
from the project and which could form the basis of a
European guideline on managing pre-frailty.
Specifically, PERSSILAA demonstrated the
acceptability and usability of this approach with
older adults, who may not find the use of such
technology easy (Scanlon, 2015), especially where
there is coexisting disability (Gell, 2015). To our
knowledge, this is the first paper to explore the use
of ICT with pre-frail, community-dwelling older
adults and the results showed that they rated the
three training modules (nutritional, cognitive and
physical) high for usability. This was similar for the
two distinct populations sampled: older Dutch
citizens attending primary care and older Italians
living in communities centred around their local
church. Only Portuguese citizens rated the
NUTRIAGEING
TM
website though it unlikely that
these differ considerably from other participants.
Another key finding of PERSSILAA is that health
literacy and ICT literacy are both important in
allowing older adults access such services. Older
Italians felt they benefited from the social
environment created by the classrooms provided.
Dutch participants however, preferred to train alone
and not compare results with their compatriots. This
may reflect different cultural backgrounds and
suggests that a one size fits all approach is unlikely
to be successful when integrating ICT into the every
day lives of older Europeans to improve their health
status. PERSSILAA is also one of the first studies to
study the effects of gamification (de Vette, 2015) on
older adults and how it may help engage them with
ICT training modules.
The results also highlight many of the challenges
of undertaking a study like this with a difficult
population to sample: pre-frail, older adults, who
while at risk for subsequent frailty and functional
decline may not be aware of this or motivated
enough to engage with screening processes. The
two-stage process enhanced the screening pathway
developed to recruit suitable participants. Several of
screens have excellent sensitivity though relatively
poor specificity meaning that a face-to-face
assessment was required to ensure that participants
were pre-frail. The results suggested that this
strategy was accurate. Due to resource limitations
not all those screening positive for pre-frailty had a
repeat assessment at the end-point of the study and
only a small number were monitored. The study was
also able to demonstrate frailty transitions during the
evaluation period but these may not be
representative of the true trajectory of frailty in this
population. Such proportionally high (approx. 20%)
transitions from one frailty state to another over a
short period are in contrast with data presented
elsewhere in larger samples over longer periods
(Gill, 2006). Therefore, it is likely that this reflects
the limitations of the screening and assessment
process itself, delivered both remotely and face-to-
face using validated instruments but not senior
physician/geriatrician assessment. However, this
project aimed to show the potential for lay or self-
screening, something that is likely to become more
widely accepted as healthcare becomes more
proactive and less reactive, stepping away from the
traditional medical model. Another limitation is that
only a small sample trialled the full platform,
released in stages as it was developed, which meant
that no significant impact upon GFI scores were
Healthcare Recommendations from the Personalised ICT Supported Service for Independent Living and Active Ageing (PERSSILAA)
Study
99

seen. This limits the project to the development and
evaluation of a service platform, which was the main
focus of the research. Thus, as a proof of concept
PERSSILAA shows the potential to use a multi-
domain ICT-based platform with older, pre-frail
adults. This, however, reduces the generalisability of
the results, which nevertheless present useful lessons
from both the development and implementation of
the platform
Overall, the 25 healthcare-related
recommendations presented provide guidance on
how to address the development and evaluation of
ICT supported services to tackle the emerging public
health challenge that an increasingly ageing and frail
older population represents. To our knowledge, this
is the first study to show the potential for an ICT
platform targeting key pre-frailty areas (i.e.
nutritional, cognitive and physical domains) in the
screening, monitoring and managing of pre-frailty.
The results of the evaluation are being analysed
further and future research is being planned to
validate the PERSSILAA platform with a suitably
powered RCT to determine if ICT-supported
services can truly prevent or delay onset of frailty
and functional decline in pre-frail community-
dwelling older adults.
ACKNOWLEDGEMENTS
The authors wish to thank all the PERSSILAA
participants throughout the three years of the project.
Specifically , the authors thank - all older adults who
joined the project: for Italy this includes residents
from the Confalone, Pilar, Rogazionisti and Santa
Maria della Salute communities; for the Netherlands
this includes those in the municipalities of Enschede,
Hengelo, Tubbergen and Twenterand. The
researchers would also like to acknowledge the not
for profit organizations in Italy who collaborated
(Progetto Alfa, Saluta in Collina), the healthcare
professionals from Campania (Local Health Agency
Naples 1, CRIUV) and the health systems including
General Practitioners who supported the project in
the Netherlands.
REFERENCES
Beswick, A.D., Rees, K., Dieppe, P., Ayis, S.,
Gooberman-Hill, R., Horwood, J., Ebrahim, S. 2008.
Complex interventions to improve physical function
and maintain independent living in elderly people: a
systematic review and meta-analysis. The Lancet, 371,
725-735.
Bherer, L., Erickson, K.I., Liu-Ambrose, T. 2013. A
review of the effects of physical activity and exercise
on cognitive and brain functions in older adults.
Journal of aging research, 11;2013.
Bitterman, N., 2011. Design of medical devices—A home
perspective. European journal of internal
medicine, 22(1), pp.39-42.
Boehler, C.E., de Graaf, G., Steuten, L., Yang, Y.,
Abadie, F. 2015. “Development of a web-based tool
for the assessment of health and economic outcomes
of the European Innovation Partnership on Active and
Healthy Ageing (EIP on AHA),” BMC Med. Inform.
Decis. Mak 15 (S3), p. S4.
Borges, L.L. and Menezes, R.L., 2011. Definitions and
markers of frailty: a systematic review of literature.
Reviews in Clinical Gerontology, 21(01), pp.67-77.
Bousquet, J., Michel, J.P., Strandberg, T., Crooks, D.,
Iakovidis, I., Iglesia, M. 2014. The European
innovation partnership on active and healthy ageing:
the European geriatric medicine introduces the EIP on
AHA column. Eur Geriatr Med 5:361–362.
Brooke, J. 1996. "SUS: a "quick and dirty" usability
scale". In P. W. Jordan, B. Thomas, B. A.
Weerdmeester, & A. L. McClelland. Usability
Evaluation in Industry. London: Taylor and Francis.
Bunt, S., O’Caoimh, R., Krijnen, W.P., Molloy, D.W.,
Goodijk, G.P., van der Schans, C.P., Hobbelen, J.S.M.
2015. Validation of the Dutch version of the Quick
Mild Cognitive Impairment Screen (Qmci-D). BMC
Geriatrics 15:115 DOI 10.1186/s12877-015-0113-1.
de Vette, F., Tabak, M., Dekker-van Weering, M.,
Vollenbroek-Hutten, M. 2015. Engaging Elderly
People in Telemedicine Through Gamification. JMIR
Serious Games, 3(2):e9.
de Vries, N.,M., Staal, J.,B., van Ravensberg, C.,D.,
Hobbelen, J.,S.,M., Olde Rikkerte, M.,G.,M., Nijhuis-
van der Sanden, M.,W.,G. 2011. Outcome instruments
to measure frailty: A systematic review. Ageing
Research Reviews, 10: 104–114.
Fairhall, N., Kurrle, S.E., Sherrington, C., Lord, S.,R.,
Lockwood, K., John, B., Monaghan, N., Howard, K.,
Cameron, I,.D. 2015. Effectiveness of a multifactorial
intervention on preventing development of frailty in
pre-frail older people: study protocol for a randomised
controlled trial. BMJ Open. 5(2):e007091.
Fiatarone Singh, M.A., Gates, N., Saigal, N., et al. 2014.
The Study of Mental and Resistance Training
(SMART) study-resistance training and/or cognitive
training in mild cognitive impairment: a randomized,
double-blind, double-sham controlled trial. J Am Med
Dir Assoc, 15(12): 873–80.
Galvin, J.E., Roe, C.M., Powlishta, K.K., Coats, M.A.,
Muich, S.J., Grant, E., Miller, J.P., Storandt, M. and
Morris, J.C., 2005. The AD8 A brief informant
interview to detect dementia. Neurology, 65(4);
pp.559-564.
Gell, N.,M., Rosenberg, D.,E., Demiris, G., LaCroix,
A.,Z., Patel, K.,V. 2015. Patterns of technology use
among older adults with and without disabilities.
Gerontologist, 55(3):pp412-21.
ICT4AWE 2017 - 3rd International Conference on Information and Communication Technologies for Ageing Well and e-Health
100

Gill, T.M., Gahbauer, E.A., Allore, H.G, Han, L. 2006.
Transitions between frailty states among community-
living older persons. Arch Intern Med, 166(4):418-23.
Giné-Garriga, M., Roqué-Fíguls, M., Coll-Planas, L.,
Sitjà-Rabert, M., Salvà, A. 2014. Physical Exercise
Interventions for Improving Performance-Based
Measures of Physical Function in Community-
Dwelling, Frail Older Adults: A Systematic Review
and Meta-Analysis. Archives of physical medicine and
rehabilitation, 95 (4):pp 753–769.e3.
Gray, S.L, Anderson, M.L, Hubbard, R.A., LaCroix, A.,
Crane, P.K., McCormick, W., Bowen, J.D, McCurry,
S.M., Larson, E.B. 2013. Frailty and incident
dementia. J Gerontol A Biol Sci Med Sci, 68(9):1083-
90.
Illario, M., Iaccarino, G., Piazza, O., Menditto, E.,
Coscioni, E. 2016. Proceedings of the EIP on AHA:
A3 Action Group on Frailty. Transl Med UniSa.
31;13:1-3.
Kahlon, S., Pederson, J., Majumdar, S.R., Belga, S., Lau,
D., Fradette, M., Boyko, D., Bakal, J.A., Johnston, C.,
Padwal, R.S. and McAlister, F.A., 2015. Association
between frailty and 30-day outcomes after discharge
from hospital. Canadian Medical Association
Journal, 187(11): pp.799-804.
Lang, P.O., Michel, J.P., Zekry, D. 2009. Frailty
syndrome: a transitional state in a dynamic process.
Gerontology, 55(5):539-49.
Langa, K.M., Larson, E.B., Crimmins, E.M., et al. 2016. A
comparison of the prevalence of dementia in the
United States in 2000 and 2012. JAMA Intern Med
doi:10.1001 /jamainternmed.2016.6807
Larner, A.J., 2015. AD8 Informant Questionnaire for
Cognitive Impairment Pragmatic Diagnostic Test
Accuracy Study. Journal of geriatric psychiatry and
neurology, 28(3): pp.198-202.
Lee, P.H., Lee, Y.S., Chan, D.C. 2012. Interventions
targeting geriatric frailty: a systemic review. Journal
of Clinical Gerontology and Geriatrics, 3(2):47-52.
Liu, C.K. and Fielding, R.A., 2011. Exercise as an
intervention for frailty. Clinics in geriatric medicine,
27(1), pp.101-110.
Liu, L.K., Lee, W.J., Chen, L.Y., Hwang, A.C., Lin, M.H.,
Peng, L.N. and Chen, L.K., 2015. Association between
frailty, osteoporosis, falls and hip fractures among
community-dwelling people aged 50 years and older
in Taiwan: results from I-Lan longitudinal aging
study. PLoS one, 10(9), p.e0136968.
Lumsden, J., Edwards, E.A., Lawrence, N.S., Coyle, D.
and Munafò, M.R., 2016. Gamification of cognitive
assessment and cognitive training: a systematic review
of applications and efficacy. JMIR Serious Games,
4(2).
Manafo, E., Wong., S. 2012. Health literacy programs for
older adults: a systematic literature review. Health
Educ Res. 27(6):947-60.
Matthews, F.E., Arthur, A., Barnes, L.E., et al. 2013.
Medical Research Council Cognitive Function and
Ageing Collaboration. A two-decade comparison of
prevalence of dementia in individuals aged 65 years
and older from three geographical areas of England:
results of the Cognitive Function and Ageing Study I
and II. The Lancet, 382(9902):1405-1412.
Michel, J.P., Dreux, C., Vacheron, A. 2016. Healthy
ageing: evidence that improvement is possible at every
age. European Geriatric Medicine, 7(4), pp.298-305.
Morley, J.E., Vellas, B., van Kan, G.A., et al. 2013. Frailty
consensus: a call to action. Journal of the American
Medical Directors Association 14:392–7.
Ngandu, T., Lehtisalo, J., Solomon, A., Levälahti, E.,
Ahtiluoto, S., Antikainen, R., Bäckman, L., Hänninen,
T., Jula, A., Laatikainen, T. and Lindström, J., 2015. A
2 year multidomain intervention of diet, exercise,
cognitive training, and vascular risk monitoring versus
control to prevent cognitive decline in at-risk elderly
people (FINGER): a randomised controlled trial. The
Lancet, 385(9984), pp.2255-2263.
Norman, C., Skinner, H. 2006. eHealth literacy: Essential
skills for consumer health in a networked world. J
Med Internet Res, 8:e9.
O’Caoimh, R., Gao, Y., McGlade, C., Healy, L.,
Gallagher, P., Timmons, S., Molloy, D.W. 2012.
Comparison of the Quick Mild Cognitive Impairment
(Qmci) screen and the SMMSE in Screening for Mild
Cognitive Impairment. Age and Ageing 41(5):624-9.
O’Caoimh, R., Gao, Y., Gallagher, P., Eustace, J.,
McGlade, C., Molloy, D.W. 2013. Which Part of the
Quick Mild Cognitive Impairment Screen (Qmci)
Discriminates Between Normal Cognition, Mild
Cognitive Impairment and Dementia? Age and Ageing
42: 324-330.
O’Caoimh, R., Svendrovski, A., Johnston, B., Gao, Y.,
McGlade, C., Timmons, S., Eustace, J., Guyatt, G.,
Molloy, D.W. 2014a. The Quick Mild Cognitive
Impairment Screen correlated with the Standardised
Alzheimer`s Disease Assessment Scale-cognitive
section in clinical trials. Journal of Clinical
Epidemiology 67, 87-92.
O’Caoimh, R., Gao, Y., Svendrovski, A., Healy, E.,
O’Connell, E., O’Keeffe, G., Leahy-Warren, P.,
Cronin, U., O’Herlihy, E., Cornally, N., Molloy, D.W.
2015a. The Risk Instrument for Screening in the
Community (RISC): A New Instrument for Predicting
Risk of Adverse Outcomes in Community Dwelling
Older Adults. BMC Geriatrics 15:92. doi:
10.1186/s12877-015-0095-z.
O’Caoimh, R., Sweeney, C., Hynes, H. et al. 2015b.
COLLaboration on AGEing – COLLAGE: Ireland's
three star reference site for the European Innovation
Partnership on Active and Healthy Ageing (EIP on
AHA). Eur Geriatr Med 6:505–511.
O’Caoimh, R., Sato, S., Wall, J., Igras, E., Foley, M.J.,
Timmons, S., Molloy, D.W. 2015c. Potential for a
"Memory Gym" Intervention to Delay Conversion of
Mild Cognitive Impairment to Dementia. Journal of
the American Medical Directors Association 16 (11),
pp.998-999.
O’Caoimh, R., Timmons, S., Molloy, D.W. 2016.
Screening for Mild Cognitive Impairment:
Healthcare Recommendations from the Personalised ICT Supported Service for Independent Living and Active Ageing (PERSSILAA)
Study
101

Comparison of "MCI Specific" Screening Instruments.
Journal of Alzheimer’s disease 51(2):619-29.
O’Caoimh, R., Gao, Y., Gallagher, P., Eustace, J., Molloy,
W. 2017. Comparing Approaches to Optimize Cut-off
Scores for Short Cognitive Screening Instruments in
Mild Cognitive Impairment and Dementia. Journal Of
Alzheimer’s Disease, in press.
O’Shea, E., Trawley, S., Manning, E. et al. 2016.
Malnutrition in hospitalised older adults: A
multicentre observational study of prevalence,
associations and outcomes J Nutr Health Aging
doi:10.1007/s12603-016-0831-x
Pahor, M., Guralnik, J.M., Ambrosius, W.T., Blair, S.,
Bonds, D.E., Church, T.S., Espeland, M.A., Fielding,
R.A., Gill, T.M., Groessl, E.J. and King, A.C. 2014.
Effect of structured physical activity on prevention of
major mobility disability in older adults: the LIFE
study randomized clinical trial. Jama, 311(23),
pp.2387-2396.
Pauly, L., Stehle, P., Volkert, D. 2007. Nutritional
situation of elderly nursing home residents. Z Gerontol
Geriatr 40(1):3-12.
Peters, L.L., Boter, H., Slaets, J.P., Buskens, E. 2013.
Development and measurement properties of the self
assessment version of the INTERMED for the elderly
to assess case complexity. Journal of Psychosom Res
;74(6):518-522.
Plassman, B.L., Langa, K.M., Fisher, G.G., Heeringa,
S.G., Weir, D.R., Ofstedal, M.B., Burke, J.R., Hurd,
M.D., Potter, G.G., Rodgers, W.L. and Steffens, D.C.,
2008. Prevalence of cognitive impairment without
dementia in the United States. Annals of internal
medicine, 148(6), pp.427-434.
Prince, M., Bryce, R., Albanese, E., Wimo, A., Ribeiro,
W., Ferri, C.P. 2013. The global prevalence of
dementia: a systematic review and meta-analysis.
Alzheimers Dementia, 9(1):63-75.
Rechel, B., Grundy, E., Robine, J.M., Cylus, J.,
Mackenbach, J.P., Knai, C., et al. 2013. Ageing in the
European Union. The Lancet, 381(9874):1312–22.
Robertson, M.C., Devlin, N., Scuffham, P., Gardner,
M.M., Buchner, D.M., Campbell, A.J. 2001.
Economic evaluation of a community based exercise
programme to prevent falls. J Epidemiol Community
Health 55:600-606.
Rodríguez-Mañas, L., Féart, C., Mann, G., Viña, J.,
Chatterji, S., Chodzko-Zajko, W., Harmand, M.G.,
Bergman, H., Carcaillon, L., Nicholson, C., Scuteri, A.
2013. Searching for an operational definition of frailty:
a Delphi method based consensus statement. The
frailty operative definition-consensus conference
project. The Journals of Gerontology Series A:
Biological Sciences and Medical Sciences, 68(1):62-7.
Roe, L., O’Halloran, A., Normand, C., Murphy, C. 2016.
The impact of frailty on public Health Nurse Service
Utilisation: Findings from the Irish Longitudinal Study
On Ageing (TILDA).
Santos-Eggimann, B., Cuenoud, P., Spagnoli, J., Junod, J.
2009. Prevalence of Frailty in Middle-Aged and Older
Community-Dwelling Europeans Living in 10
Countries. Journals of Gerontology Series a-
Biological Sciences and Medical Sciences
, 64, 675-
681.
Satizabal, C.L., Beiser, A.S., Chouraki, V., Chêne, G.,
Dufouil, C., Seshadri, S.2016. Incidence of dementia
over three decades in the Framingham Heart Study. N
Engl J Med, 374(6):523-532.
Scanlon, L., O’Shea, E., O’Caoimh, R., Timmons, S.
2015. Technology use, frequency and self-rated skills:
A survey of community dwelling older adults. Journal
of American Geriatrics Society 63(7):1483-4.
Schilp, J., Kruizenga, H.M., Wijnhoven, H.A., Leistra, E.,
Evers, A.M., van Binsbergen, J.J., Deeg, D.J. and
Visser, M., 2012. High prevalence of undernutrition in
Dutch community-dwelling older individuals.
Nutrition, 28(11), pp.1151-1156.
Selwyn, N., Gorard, S., Furlong, J. and Madden, L., 2003.
Older adults' use of information and communications
technology in everyday life. Ageing and society,
23(05), pp.561-582.
Sergi, G., Veronese, N., Fontana, L., De Rui, M., Bolzetta,
F., Zambon, S., Corti, M.C., Baggio, G., Toffanello,
E.D., Crepaldi, G. and Perissinotto, E. 2015. Pre-
frailty and risk of cardiovascular disease in elderly
men and women: the Pro. VA study. Journal of The
American college of cardiology, 65(10), pp.976-983.
Shakersain, B., Santoni, G., Faxén-Irving, G., Rizzuto, D.,
Fratiglioni, L., Xu, W. 2016. Nutritional status and
survival among old adults: an 11-year population-
based longitudinal study. European Journal of
Clinical Nutrition, 70, 320-325.
Song, X., Mitnitski, A., Rockwood, K. 2010. Prevalence
and 10-year outcomes of frailty in older adults in
relation to deficit accumulation. J Am Geriatr Soc
58(4):681-7.
Sternberg, S.A., Schwartz, A.W., Karunananthan, S.,
Bergman, H., Clarfield, A.M. 2011. The Identification
of Frailty: A Systematic Literature Review. Journal of
the American Geriatrics Society, 59, 2129-2138
Steverink, N., Slaets, J.P.J., Schuurmans, H., Van Lis, M.
2001. Measuring frailty: developing and testing the
GFI (Groningen Frailty Indicator). Gerontologist.
2001;41(Special Issue 1):236.
Strawbridge, W.,J., Shema, S.,J., Balfour, J.,L., Higby,
H.,R., Kaplan, G.,A. 1998. Antecedents of frailty over
three decades in an older cohort. J Gerontology
53b(1);ppS9-16.
Tabak, M., Brusse-Keizer, M., van der Valk, P., Hermens,
H. and Vollenbroek-Hutten, M. 2014. A telehealth
program for self-management of COPD exacerbations
and promotion of an active lifestyle: a pilot
randomized controlled trial. International journal of
chronic obstructive pulmonary disease, 9, p.935.
Thomas, S., Mackintosh, S. and Halbert, J. 2010. Does the
‘Otago exercise programme’reduce mortality and falls
in older adults?: a systematic review and meta-
analysis. Age and Ageing, 39(6):pp681-7.
Turner, G., Clegg, A; British Geriatrics Society; Age UK;
Royal College of General Practioners. 2014. Best
practice guidelines for the management of frailty: a
ICT4AWE 2017 - 3rd International Conference on Information and Communication Technologies for Ageing Well and e-Health
102

British Geriatrics Society, Age UK and Royal College
of General Practitioners report. Age and Ageing,
43(6):pp744-7.
van Kempen, J.A., Schers, H.J., Philp, I., Rikkert, M.G.O.
and Melis, R.J., 2015. Predictive validity of a two-step
tool to map frailty in primary care. BMC
medicine, 13(1), p.1.
van Staveren, W.A. and de Groot, L.C.P. 2011. Evidence-
based dietary guidance and the role of dairy products
for appropriate nutrition in the elderly. Journal of the
American College of Nutrition, 30(sup5), pp.429S-
437S.
Vollenbroek-Hutten, M., Pais, S., Ponce, S., Dekker-van
Weering, M., Jansen-Kosterink, S., Schena, F.,
Tabarini, N., Carotenuto, F., Iadicicco, V. and Illario,
M. 2015. Rest Rust! Physical active for active and
healthy ageing. Translational medicine@ UniSa, 13,
p.19.
Healthcare Recommendations from the Personalised ICT Supported Service for Independent Living and Active Ageing (PERSSILAA)
Study
103
