
Health Information Exchange and Related IT-security Practices in
European Hospitals
Sylvestre Uwizeyemungu
1
and Placide Poba-Nzaou
2
1
Département des Sciences Comptables, Université du Québec à Trois-Rivières (UQTR),
3351, Boul. des Forges, C.P. 500, Trois-Rivières (Québec), Canada
2
Département d’Organisation et Ressources Humaines, ÉSG – Université du Québec à Montréal (UQAM),
315, Ste-Catherine Est, Montréal (Québec), Canada
sylvestre.uwizeyemungu@uqtr.ca, poba-nzaou.placide@uqam.ca
Keywords: IT Security, Privacy, Confidentiality, Integrity, Availability, Health Information Exchange, Healthcare
Information Technology, Electronic Health Records, e-Health.
Abstract: Alongside other health information technologies (HIT), several projects aimed at implementing electronic
health information exchange (HIE) have been initiated in European countries, with the hope of improving the
coordination, safety, and efficiency in healthcare systems. However, the electronic exchange exposes health
data to information technology (IT)-related vulnerabilities and threats, raising concerns among patients, health
care providers, and policy-makers. Drawing on data from a sample of 1123 European hospitals, we conducted
a cluster analysis to determine to what extent hospitals do live up to the IT security and privacy challenges of
electronic HIE. We produced two sets of clusters, one related to HIE usage and another related to the
implementation of IT-security practices. Through a cross-comparison, we proceeded to a match/mis-match
analysis. The results of this study depict a mixed situation: even though most of surveyed hospitals (79.2%)
have implemented IT-security practices consistent with their HIE usage levels, hospitals that have failed to
do so (20.8%) pose a threat to the entire healthcare system which is becoming more and more interconnected.
1 INTRODUCTION
Developed countries have undertaken the reform of
their healthcare systems in the quest to achieve what
has been called the “triple aim”, that is (1) improving
individual care experience, (2) improving population
health, and (3) reducing per-capita cost of healthcare
(Berwick et al., 2008). The adoption of health
information technologies (HIT) is at the heart of the
healthcare reform.
The use of Health IT is now widely accepted as a
cornerstone of modern healthcare delivery, and the
question has shifted from whether IT should be used
in health care to which models of care delivery should
HIT support (Bitton et al., 2012). It then makes sense
to analyze the challenges that would impede the
unleashing of the full potential of IT in healthcare
settings in order to alleviate their effects. Among
these challenges, security and privacy concerns are of
utmost importance for at least three reasons.
First, health IT systems in general, and electronic
health records (EHR) in particular compile a wide
range of highly sensitive information including not
only current data related to tests, diagnoses, and
treatments, but also past medical history (Häyrinen et
al., 2008). Concerns of patients as well as health
professionals with regard to ensuring security and
privacy of highly-sensitive records might fuel their
resistance to trust and embrace HIT (Ancker et al.,
2012; O’Donnell et al., 2011; Vogel et al., 2014).
Second, by turning health information into bits, a
HIT increases health records’ portability, which is
convenient in multiple ways, but in so doing, it
increases their vulnerability to security and privacy
breaches that are paramount in other digital media
(Tejero et al., 2012).
Third, in order to obtain the full potential from any
HIT, the highly sensitive information it contains has
to be readily accessible to healthcare professionals as
well as to patients (Tejero et al., 2012) at any moment
and everywhere it is justifiably needed. Therefore, an
effective HIT goes hand in hand with electronic
health information exchange (HIE). However,
security and privacy concerns stem from the fact that
an electronic HIE multiplies parties that have access
to health information and increases patients’ feeling
538
Uwizeyemungu, S. and Poba-Nzaou, P.
Health Information Exchange and Related IT-security Practices in European Hospitals.
DOI: 10.5220/0006263305380545
In Proceedings of the 3rd International Conference on Information Systems Security and Privacy (ICISSP 2017), pages 538-545
ISBN: 978-989-758-209-7
Copyright
c
2017 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

of limited control over health care providers’ use of
that information (O’Donnell et al., 2011). In a survey
of patients (Ancker et al., 2012), 68% respondents
expressed privacy and security concerns. These
concerns are especially about who will have access to
the health information including the risks of
unauthorized access and the nature of sensitive
information that would be shared (Simon et al., 2009).
In this study, we measure the implementation
levels of electronic HIE against the IT-security
related practices in European hospitals. Our main
research question is: are European hospitals living up
to the IT security and privacy challenges of electronic
Health Information Exchange?
Drawing on data collected by the European
Commission through 2013 eHealth survey (European
Commission, 2014), we first proceeded to a cluster
analysis of European hospitals with regards 1) to their
HIE usage levels and 2) to their IT-security practices
implementation levels. We then compared the two
sets of clusters. Secondly, after developing an
electronic HIE implementation Index (referred to as
« HIE Index » from now on) as well as an IT-security
index for each surveyed hospital, we compared each
hospital’s HIE Index to its IT-security Index to assess
whether the implementation of electronic HIE is
accompanied by the enforcement of required IT-
security and privacy practices.
Our results depict a mixed situation: even though
most of surveyed hospitals (79.2%) have
implemented IT-security practices consistent with
their HIE usage levels, hospitals that have failed to do
so (20.8%) pose a threat to the entire healthcare
system which is becoming more and more
interconnected. In addition, a fine analysis of our
results shows a more complex situation that led us to
call for more IT-security practices implementation in
hospitals given the sensitive nature of health
information. Indeed, over 60% hospitals that are well
advanced in using health information exchange do not
adopt IT-security practices that are consistent with the
associated IT-security risks.
2 BACKGROUND
2.1 IT Security Concerns About HIE
Various stakeholders in healthcare systems have
concerns over the security and privacy of health
information stored in, or transmitted across, different
health IT systems. Patients have concerns related to
the risk of their sensitive health information falling
into unauthorized hands or being exploited by third
parties without their informed consent (Hwang et al.,
2012). Healthcare providers, health IT suppliers, as
well as health policy-makers are preoccupied by the
adverse effects of IT security and privacy breaches.
Healthcare providers may loose patients’ trust and
confidence that are necessary for the laters’
willingness to consent to the usage of their
information in HIE. Consequently, HIE would not
meet the “meaningful use” requirement, a failing that
will undermine the efficiency and effectiveness of
healthcare delivery and public health surveillance.
Healthcare providers are also preoccupied by
healthcare professional responsibilities and liabilities
(Zwaanswijk et al., 2013). Reports from the USA
(Absolute Software Corporation, 2015) mention data
breaches that cost hospitals up to US$ 2.5 million in
settlement payments.
Concerns of patients, healthcare providers, and
policy-makers over health information exposure to IT
security and privacy breaches are justified if one
considers the results of recent surveys in healthcare
organizations (HIMSS, 2015; ISMG, 2014; Ponemon
Institute, 2016). In the 2014 survey of Information
Security Media Group (ISMG), three quarters (75%)
of surveyed healthcare providers reported to have
experienced at least one IT security related breach
affecting under 500 individuals; and 21% reported at
least one security incident affecting over 500
individuals (ISMG, 2014, p. 6). A Healthcare
Information and Management Systems Society
(HIMSS) survey conducted in 2015 found that at least
one major security incident recently occurred in 68%
of respondent healthcare organizations (HIMSS,
2015, p. 15). In a survey by Ponemon Institute
(Ponemon Institute, 2016, p. 19), 89% of surveyed
healthcare organizations reported to have suffered a
data breach leading to the loss or theft of patient data
during the 24 months preceding the survey.
2.2 IT Security Reference for HIE
Considering HIE-related concerns over data
breaches, the implementation of HIE should be
accompanied with an appropriate IT security policy,
which is “a collection of rules that allow or disallow
possible actions, events, or something related to
security” (Bahtiyar et al., 2014, p. 164).
IT-security requirements are generally
determined with reference to the so-called CIA triad:
confidentiality, integrity, and availability (Dehling et
al., 2014; von Solms, 2005). The confidentiality
requirement is met if only people with valid
authorization can have access to data obtained from,
or transmitted through HIE. This can be achieved
Health Information Exchange and Related IT-security Practices in European Hospitals
539

through encryption of data in storage or being
transmitted, as well as through access control of
workstations.
The integrity requirement aims at guaranteeing
specific and authorized ways health data can be
modified (White, 2004). It is meant to avoid any
undue alteration or effacement of health data, whether
it is intentional and malicious or unintentional, and
whether it comes from authorized or unauthorized
users (Dehling et al., 2014).
A HIE that is accessible and operates at its full
capacity whenever an authorized user needs it meets
the availability requirement. In order to meet this
requirement, a HIE has to respond adequately even in
peak periods (scalability), to resist to hardware and/or
software failures (resilience), and to be designed in a
fashion that allows to immediately or very quickly
recuperate data after any kind of disaster
(recoverability) (Dehling et al., 2014).
3 METHODS
3.1 Data Source
For the purposes of this study, we used data collected
by the European Commission through the 2013
eHealth survey (Joint Research Centre, Institute for
Prospective Technological Studies). The survey
targeted acute care hospitals across the European
Union (27 member states, plus Croatia, Iceland, and
Norway), with the objective of benchmarking the
level of eHealth use (European Commission, 2014).
3.2 Sample
The European Commission survey collected data
from a total of 1753 acute care hospitals. But as our
aim was to study the HIE usage and related IT-
security practices, we dropped all hospitals that
declared to not use any form of HIE. This led us to a
sample of 1293 hospitals, which represent 73.8% of
all surveyed hospitals. From this sample, we dropped
170 cases (13.2%) due to missing values on HIE-
related measuring variables (no answer or ‘don’t
know’ response). This led us to a final sample of 1123
hospitals. The statistical tests for non-response bias
analysis were non significant.
Seven out of 10 hospitals in our sample are public
hospitals. They are mostly non-university hospitals
(84.6%). Independent hospitals make up almost three
quarters (73.4%) of the sample. Medium hospitals
(between 101 and 750 beds) make up two thirds
(67.1%) of the sample. 6 out of 10 hospitals (60.2%)
rated themselves to being in an intermediate phase on
their way in transition from a paper-based system
towards a fully electronic-based system. For slightly
more than half of hospitals (51.3%), the IT budget
represents between 1 to 3% of the total hospital
budget. As for IT-security regulation reference,
71.9% of sampled hospitals reported to have
developed an in-house regulation, 65.5% and 33.6%
reported to rely respectively on national-level and
regional-level regulations.
3.3 Measurement
For this study, our contextual variables were
measured through either multiple choice questions
(e.g. status), dichotomous questions (e.g. hospital
university), interval scales (e.g. size), or ordinal
scales (e.g. transition level from paper to electronic-
based system).
As for the clustering variables, namely HIE-
related variables as well as IT-security related
variables, they were all but one measured through
dichotomous questions: yes (1) for the presence of a
practice related to either information exchange (Table
1) or to IT-security (Table 2), and no (0) if the practice
was not implemented. The sole exception is for the
second availability-related question: hospitals were
asked how much time it would take them to restore
their critical clinical systems in the wake of a disaster
causing a complete loss of data. Hospitals were asked
to choose only one response among the following:
immediately, less than 24 hours, less than 2 days, less
than 1 week, less than 1 month, and more than 1
month. A hospital that would be able to immediately
restore data was given the full score on this point (1)
while a hospital that would need more than a month
was given a null score (0). Hospitals in between these
two extremes were given scores of 0.8 (less than 24
hours), 0.6 (less than 2 days), 0.4 (less than 1 week),
and 0.2 (less than 1 month).
The HIE index with which we measure to what
extent a given hospital electronically exchanges
health information was developed based on the “yes”
answers to questions in Table 1. These questions
allow to know which information (4 types of
information) a hospital electronically exchanges and
with whom the exchange is done (5 types of partners).
As 1 point is attributed to a “yes” answer to any
type of exchange with any type of partner, and zero
to a “no” answer, the score obtained is theoretically
comprised between 0 (there is no electronic exchange
at all) and 20 (exchange of all 4 types of information
with all 5 categories of partners). For convenience,
the score was calibrated to a 10-scale measure.
ICISSP 2017 - 3rd International Conference on Information Systems Security and Privacy
540
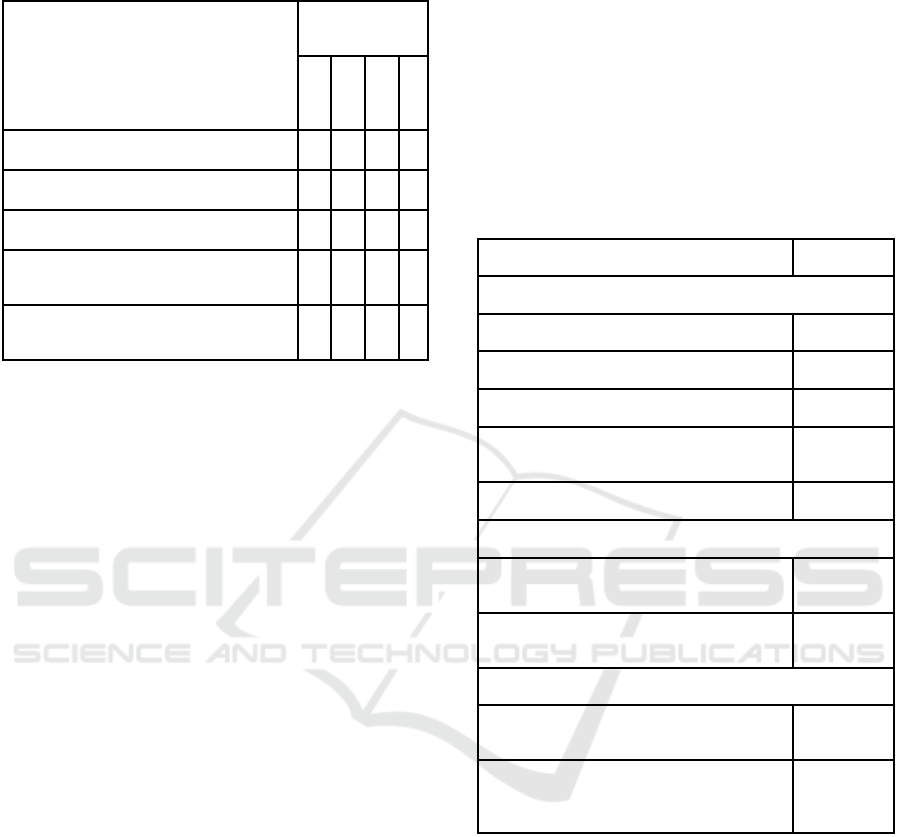
Table 1: HIE Usage Levels.
Does your hospital exchange
electronically:
A. Clinical care information
B. Laboratory results information
C. Medication lists information
D. Radiology images and reports
Measure (Yes: 1
/ No: 0)
A B C D
a). With other hospitals
b). With external general practitioners
c). With external specialists
d). With health care providers in other EU
countries
e). With health care providers outside the
EU countries
We also developed an IT-security index taking
into account the IT-security practices implemented
(Table 2). Consistent with our definition of IT-
security, the IT-security index allows to assess the
level of IT security practices implementation
alongside three dimensions: confidentiality, integrity,
and availability. The confidentiality component of IT
security was captured through five (5) questions
related to data encryption and data access control;
each of the integrity and availability components was
measured through two (2) questions. Before
calibrating the overall IT-security index on a 10-scale
measure, all its three dimensions were equivalently
weighted (2 points for each one); this step allowed us
to avoid that an over-weight be put on the
confidentiality component due to its being captured
through more questions (5) than the other components
(2 questions each).
3.4 Cluster Analysis
We performed two cluster analyses, one on HIE usage
dimensions and another on IT-security practices. We
used SPSS’s agglomerative hierarchical clustering
algorithm, with Ward’s minimum variance and
squared Euclidian distance as grouping criterions. To
decide the optimal number of clusters, we inspected
the Euclidian distances across dendrograms produced
by the algorithm. From this inspection a 3-cluster
solution emerged as a probable optimal solution for
HIE usage, while two solutions (a 3-cluster and a 4-
cluster solutions) appeared to be plausible for IT-
security practices. To confirm the HIE-related cluster
and to decide which solution among the two related
to IT security would be better, we applied Ketchen
and Shook’s (1996) recommendation: using SPSS’s
random selection functionality, we constituted
subsamples of about successively 70% and 40%, on
which we performed the already described clustering
procedure, after which we analyzed the resulting
dendrograms. The results of this analysis confirmed
the robustness of the 3-cluster solutions for both HIE
usage and IT-security practices. Once the clusters
were formed, we performed the Tamhane’s T2 (post-
hoc) test to ascertain pair-wise differences between
clusters’ means.
Table 2: IT-ecurity Practices Measures.
Practice Measure
1. Confidentiality
1.1. Encryption of stored data Yes / No
1.2. Encryption of transmitted data Yes / No
1.3. Access control through cards Yes / No
1.4. Access control through fingerprint
information
Yes / No
1.5. Access control through a password Yes / No
2. Integrity
2.1. Data entry in the hospital’s IT system
certified with digital signature
Yes / No
2.2. Clear structured rules on reading-writing
patients’ electronic medical data
Yes / No
3. Availability
3.1. Hospital archive strategy for long-term
storage and disaster recovery
Yes / No
3.2. Time laps to restore critical clinical
information system operations after a disaster
causes the complete loss of data
Hours / Days
/ Weeks /
Months
4 RESULTS AND DISCUSSION
4.1 Results of Cluster Analysis
We present in Table 3 the HIE usage patterns
resulting from our cluster analysis. But, before
scrutinizing the differences between clusters, we can
note from the grand means in Table 3 that overall,
clinical care information is the most electronically
exchanged information (with an average of 1.68 types
of partners), followed by laboratory results
information (1.46), while radiology images and
reports (1.03) as well as medication lists information
Health Information Exchange and Related IT-security Practices in European Hospitals
541
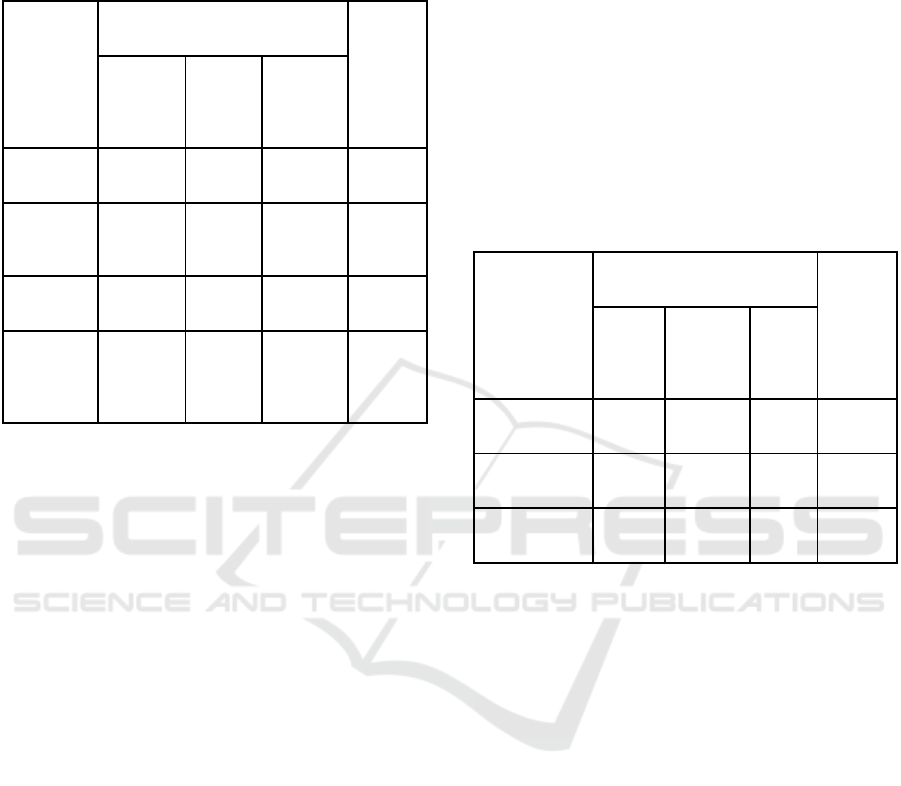
(0.72) are the least exchanged.
Table 3: HIE Usage Patterns Resulting from Cluster
Analysis.
Variable
(Grand
Mean)
Cluster Label
(n; %)
Anova
(F Test)
Advanced
(240;
21.4%)
Mean
Average
(348;
31.0%)
Mean
Laggards
(535;
47.6%)
Mean
Clinical
Care (1.68)
H
2.74
a
H
2.64
a
L
0.58
b
1026.89*
Laboratory
Results
(1.46)
H
2.64
a
M
1.90
b
L
0.65
c
377.79*
Medication
Lists (0.72)
H
2.65
a
L
0.13
c
M
0.24
b
1309.17*
Radiology
Images and
Reports
(1.03)
M
1.88
b
L
0.72
c
H
2.52
a
150.01*
Legend:
•
*: p<0.001 (two-tailed test);
•
a,b,c: Within rows, different subscripts indicate significant
(p<0.05) pair-wise differences between means on Tamhane’s
T2 (post-hoc) test;
•
H (High), M (Medium), and L (Low) indicate relative
magnitude of the group means on each variable across the
three clusters
Three clearly distinct clusters emerged from our
analysis. We labelled these clusters according to the
intensity of HIE usage given by the means calculated
based on how many different types of health
information are electronically exchanged with how
many types of healthcare partners (cf. Table 1). The
first cluster we labelled “Advanced HIE users” is the
smallest group (21.4%) and exhibits the highest levels
of exchanges in 3 out of 4 types of exchanged health
information (clinical care, laboratory results,
medication lists), and in the fourth (radiology images
and reports), it comes in the second position. The
second and third clusters account respectively for
31% and 47.6% of hospitals in our sample, and they
both score « high » in one type of health information
exchanged, they both come in the middle position
once, and they both score « low » twice. At this point
they seem quite similar, but they are distinct in that
their respective high, medium and low scores are
realized on different types of health information.
Besides, the third cluster is markedly more
unipolar than the second cluster: hospitals in the third
group exchange almost exclusively one type of health
information (radiology images and reports), while
hospitals in the second cluster, in addition to
remarkably exchanging clinical care information,
also exchange laboratory results to a certain extent.
Thus, we labelled the second cluster « Average HIE
Users » and the third cluster « Laggard HIE Users ».
We present in Table 4 the results of our cluster
analysis, based this time on IT-security practices. For
this analysis, we used data on 1068 hospitals (instead
of 1123 - loss of 55 observations) due to missing data
on key IT-security variables for the 55 dropped
observations.
Table 4: IT-Security Practices Patterns Resulting from
Cluster Analysis.
Variable
(Grand Mean)
Cluster Label
(n; %)
Anova
(F Test)
Strong
(281;
26.3%)
Mean
Moderate
(520;
48.7%)
Mean
Weak
(267;
25.0%)
Mean
Confidentiality
(0.99)
H
1.18
a
M
0.96
b
L
0.85
c
28.12*
Integrity
(1.23)
H
2.00
a
L
0.90
c
M
1.08
b
847.18*
Availability
(1.49)
H
1.77
a
H
1.75
a
L
0.68
b
2223.44*
Legend:
•
*: p<0.001 (two-tailed test);
•
a,b,c: Within rows, different subscripts indicate significant
(p<0.05) pair-wise differences between means on Tamhane’s
T2 (post-hoc) test;
•
H (High), M (Medium), and L (Low) indicate relative
magnitude of the group means on each variable across the
three clusters
Generally speaking, it appears that the
“availability” component of IT-security is the most
implemented practice (grand mean of 1.49), followed
by the “integrity” dimension (1.23), while the
“confidentiality” dimension comes in the last position
(0.99).
Based on levels of IT-security practices
implemented, we labelled the derived three clusters
“Strong IT-Security”, “Moderate IT-Security”, and
“Weak IT-Security”. The cluster labelled “Strong IT-
Security” is comprised of 26.3% of surveyed
hospitals and exhibits the highest levels on all the
three dimensions of our IT-security index. On the
other end of the spectrum one finds the cluster with
low levels of IT-security practices implemented. This
cluster labelled “Weak IT-Security” accounts for
25% of our sample. The largest group (48.7%) is the
ICISSP 2017 - 3rd International Conference on Information Systems Security and Privacy
542
“Moderate IT-Security” cluster which exhibits high
levels on the availability component of IT-security,
while exhibiting relatively moderate levels on the
confidentiality component, and low levels on the
integrity dimension.
4.2 HIE Usage and IT-security
Practices: Cross-comparison
Hospitals that electronically exchange health
information are more exposed to IT-security breaches
than hospitals that do not. It was then expected that
higher levels of HIE usage would be associated with
higher levels of IT-security practices implemented.
To test this hypothesis, we present in Table 5 a cross-
tabulation of HIE patterns and IT-security practices
patterns.
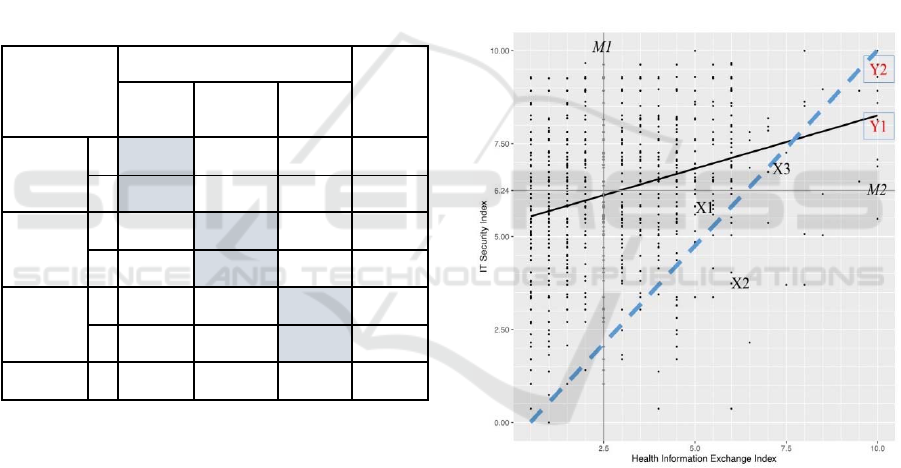
Table 5: Cross-Tabulation of the Two Sets of Clusters.
HIE Patterns*
IT-Security Practices Patterns
TOTAL
Strong
(26.3%)
Moderate
(48.7%)
Weak
(25.0%)
Advanced
(21.3%)
n 87 103 38
228
% 38.2% 45.2% 16.7%
100.0%
Average
(31.4%)
n 94 160 81
335
% 28.1% 47.8% 24.2%
100.0%
Laggards
(47.3%)
n 100 257 148
505
% 19.8% 50.9% 29.3%
100.0%
TOTAL n 281 520 267 1068
*The percentages are here slightly different from the
percentages in Table 3 because of 55 dropped observations for
the clustering analysis on IT-security practices.
The “perfect match” between HIE usage levels
and IT-security practices implementation occurs for
only 395 (= 87 + 160 + 148) hospitals (37.0% of all
the sample).
More precisely, it is worth noting, from Table 5,
that only 38.2% of “advanced HIE users” are at the
same time “strong IT-security practices”
implementers. This means that over 60% hospitals
that are well advanced in using health information
exchange do not adopt IT-security practices that are
consistent with the associated IT-security risks. More
preoccupying are the 16.7% of hospitals that are
extensively using HIE while exhibiting weak IT-
security practices implementation. On the positive
note, one can emphasize that 70.7% (19.8% + 50.9%)
of hospitals that are far behind with regard to HIE
usage (laggards) have already in place IT-security
practices that would allow them to securely step up
their HIE usage should the need arises.
We pushed further our analysis by comparing
each hospital’s level of HIE usage with its
implementation level of IT-security practices. To do
so, we used the HIE Index and the IT-security Index
described in section 3.3. In Figure 1, we plotted each
hospital’s HIE index (horizontal axis) against its IT-
security index (vertical axis). Both indices are on a
10-scale measure.
From the median lines (M1 and M2), one can note
that half of the sampled hospitals:
are very weakly involved in health information
exchange (the median is 2.5 on a 0 to 10 scale);
have already made over the half path in
implementing IT-security practices (median of
6.24 on a 0 to 10 scale).
Figure 1: HIE Index and IT-Security Index.
The ascending slope of the regression line (Y1)
suggests that overall, there is a trend toward
enhancing IT-security measures as hospitals intensify
their electronic HIE usage. This is a rather positive
result, but upon close scrutiny, one has to moderate
the positive impression. Indeed, the points are
scattered all over a large part of the surface of the
figure, instead of being roughly grouped along the
regression line, which suggests a lack of a consistent
trend: the variability within hospitals is too high.
Even though there are many hospitals that have
implemented IT-security practices at a high level
while using HIE at lower levels, there are other many
Health Information Exchange and Related IT-security Practices in European Hospitals
543

hospitals in the opposite situation (weak IT-security
practices implemented and higher levels of HIE
usage).
As we hypothesized that hospitals would have to
adopt IT-security measures consistent with their
electronic HIE levels, the diagonal line in Figure 1
reflects the theoretical “perfect” alignment between
IT-security practices and HIE usage. Stating this, we
are aware of the fact that the health information
exchange is not the only determinant of IT-security
measures. It is possible that a hospital weakly or not
at all involved in electronic HIE would feel the need
to stage up its IT-security practices due to its being
well advanced in the transition towards a fully
electronic-based hospital management system (which
does not yet include HIE). Thus, in our view, the
diagonal line defines the coordinates (HIE Index, IT-
Security Index) that indicate the minimum threshold
of IT-security practices any hospital using electronic
HIE at some extent must implement. More precisely,
any hospital above the diagonal line (like the hospital
represented by the coordinate X1) displays an IT-
security index above the minimum it is required to
attain considering its level of electronic HIE usage.
Conversely, a hospital represented by the coordinate
X2 below the diagonal line should step up its IT-
security practices to meet the minimal security
requirements of its level of HIE usage. The IT-
security index of hospital X3 right on the diagonal
line is consistent with its HIE usage level.
The analysis of the dispersion of points in Figure
1 leads to conclusions that are consistent with the
results stemming from our cluster analysis, and
specifically from the cross-comparison of HIE usage
clusters and IT-security practices clusters (Table 5).
From the Figure 1, we note that there are many points
above than below the diagonal line, which means that
most hospitals have already in place IT-security
measures that would allow them to securely go
further with electronic HIE. Hospitals in this position
are mainly “HIE laggards” that are either “moderate
IT-security” practices implementers (50.9% of HIE
laggards - Table 5) or “strong IT-security” practices
implementers (19.8%); they also include “average
HIE users” that are “strong IT-security” practices
implementers (28.1%).
5 IMPLICATIONS AND
CONCLUSION
Our study allows to shed light on the state of HIE in
European hospitals. First of all, we found that 73.8%
of surveyed hospitals are engaged in one form or
another of electronic HIE. A higher rate of hospitals
that have already adopted electronic HIE is rather a
good news. Indeed, previous studies have proven that
an electronic HIE can be instrumental not only in
improving patient care and safety (Cochran et al.,
2015; Kaelber et al., 2007), but also in alleviating the
health system’s financial burden through significant
reduction of laboratory tests and radiology
examinations (Yaraghi, 2015). However, the mere
adoption in itself is not enough to yield the potential
benefits expected from HIE. Hospitals have to reach
the “meaningful use”. As HIE usage levels vary from
one hospital to another, we grouped hospitals
according to their HIE usage patterns. Hospitals that
emerged as “advanced HIE users” represent only
21.4% of surveyed hospitals. A relatively important
proportion of hospitals (47.6%) exhibit HIE usage
patterns that put them in the category of “laggard HIE
users”. From these results, it is clear that there is still
a long way to go in order to achieve the “meaningful
use” of HIE in European hospitals.
With regard to IT-security practices, only 26.3%
of surveyed hospitals display a strong position. In
absolute terms, this rate is very low considering the
highly sensitive nature of health information.
However, back to our research question, our main
objective was to ascertain whether European
hospitals do live up to the IT security and privacy
challenges of HIE. In this regards, our results are
rather mixed: we found that most of surveyed
hospitals have in place an IT-security apparatus that
is either consistent with their HIE usage (37.0%) or
more ambitious than what would be required of them
considering their HIE usage level (42.2%). These two
groups make up 79.2% of surveyed European
hospitals. The remaining hospitals (20.8%) would
need to step up their IT-security practices in order to
keep up with their electronic HIE usage levels.
This global picture seems positive, but it hides
some preoccupying situations that appear when one
scrutinizes the HIE clusters. The group of “Advanced
HIE users” is composed of 228 hospitals, among
which 141 (=103 + 38) do not live up to the security
challenges that their HIE usage entails. This
represents 63.7% of the group that needs the most to
implement IT-security practices. The same analysis
can be done with the group labelled “Average HIE
users”: this group comprises 335 hospitals, among
which 81 (24.2%) do not meet the threshold of IT-
security practices implementation that would be in
line with their HIE usage level.
In spite of some limitations (usage of secondary
data, assumption of a linear relationship between HIE
ICISSP 2017 - 3rd International Conference on Information Systems Security and Privacy
544

usage and IT-security practices), this study addresses
one of the major concerns surrounding the electronic
HIE usage: the IT-security practices that are required
to ensure the trust of both patients and healthcare
providers. In future works, it would be worthwhile to
pursue and deepen the analysis of factors that
determine the levels of HIE usage and IT-security
practices implementation.
REFERENCES
Absolute Software Corporation, 2015. The Cost of a Data
Breach: Healthcare Settlements Involving Lost or
Stolen Devices. Austin, Texas: Absolute Software
Corporation.
Ancker, J. S., Edwards, A. M., Miller, M. C., & Kaushal,
R., 2012. Consumer perceptions of electronic health
information exchange. American Journal of Preventive
Medicine, 43(1), 76-80.
Bahtiyar, S., & Çaglayan, M. U., 2014. Trust Assessment
of Security for e-Health Systems. Electronic Commerce
Research and Applications, 13(3), 164-177.
Berwick, D.M., Nolan, T. W., & Whittington, J., 2008. The
Triple Aim: Care, health, and cost. Health Affairs,
27(3), 759-769.
Bitton, A., Flier, L. A., & Jha, A. K., 2012. Health
information technology in the era of care delivery
reform: To what end? The Journal of the American
Medical Association, 307(24), 2593-2594.
Cochran, G. L., Lander, L., Morien, M., Lomelin, D. E.,
Sayles, H., & Klepser, D. G., 2015. Health care
provider perceptions of a query-based health
information exchange: barriers and benefits. Journal of
Innovation in Health Informatics, 22(2), 302-308.
Dehling, T., & Sunyaev, A., 2014. Secure provision of
patient-centered health information technology services
in public networks--leveraging security and privacy
features provided by the German nationwide health
information technology infrastructure. Electronic
Markets, 24(2), 89-99.
European Commission, 2014. European hospital survey:
Benchmarking deployment of eHealth services (2012-
2013). Luxembourg: JRC Scientific and Policy Reports
- Institute for Prospective Technological Studies.
Häyrinen, K., Saranto, K., & Nykänen, P., 2008. Definition,
Structure, Content, Use and Impacts of Electronic
Health Records: A Review of the Research Literature.
International Journal of Medical Informatics, 77(5),
291-304.
HIMSS, 2015. 2015 HIMSS Cybersecurity Survey.
Chicago, IL: HIMSS.
Hwang, H.-G., Han, H.-E., Kuo, K.-M., & Liu, C.-F., 2012.
The differing privacy concerns regarding exchanging
electronic medical records of Internet users in Taiwan.
Journal of Medical Systems, 36(6), 3783-3793.
ISMG, 2014. Healthcare Information Security Today. 2014
Survey Analysis: Update on HIPAA Omnibus
Compliance, Protecting Patient Data (pp. 38).
Retrieved from http://6dbf9d0f8046b8d5551a-
7164cafcaac68bfd3318486ab257f999.r57.cf1.rackcdn.
com/2014-healthcare-information-security-today-
survey-pdf-5-h-53.pdf.
Kaelber, D. C., & Bates, D. W., 2007. Health information
exchange and patient safety. Journal of Biomedical
Informatics, 40(6 SUPPL), S40-S45.
Ketchen, D. J., & Shook, C., 1996. The Application of
Cluster Analysis in Strategic Management Research:
An Analysis and Critique. Strategic Management
Journal, 17(6), 441-458.
O’Donnell, H. C., Patel, V., Kern, L. M., Barrón, Y.,
Teixeira, P., Dhopeshwarkar, R., & Kaushal, R., 2011.
Healthcare consumers’ attitudes towards physician and
personal use of health information exchange.
Journal of
General Internal Medicine, 26(9), 1019-1026.
Ponemon Institute, 2016. Sixth annual benchmark study on
privacy & security of healthcare data. Traverse City,
MI, USA: Ponemon Institute.
Simon, S. R., Benjamin, A., Delano, D., & Bates, D. W.,
2009. Patients’ attitudes toward electronic health
information exchange: Qualitative study. Journal of
Medical Internet Research, 11(3), e30.
Tejero, A., & de la Torre, I., 2012. Advances and Current
State of the Security and Privacy in Electronic Health
Records: Survey from a Social Perspective. Journal of
Medical Systems, 36(5), 3019-3027.
Vogel, J., Brown, J. S., Land, T., Platt, R., & Klompas, M.,
2014. MDPHnet: Secure, distributed sharing of
electronic health record data for public health
surveillance, evaluation, and planning. American
Journal of Public Health, 104(12), 2265-2270.
von Solms, S. H., 2005. Information security governance:
Compliance management vs operational management.
Computers & Security, 24(6), 443-447.
White, P., 2004. Privacy and security issues in
teleradiology. Seminars in Ultrasound, CT and MRI,
25(5), 391-395.
Yaraghi, N., 2015. An empirical analysis of the financial
benefits of health information exchange in emergency
departments. Journal of the American Medical
Informatics Association, 22(6), 1169-1172.
Zwaanswijk, M., Ploem, M. C., Wiesman, F. J., Verheij, R.
A., Friele, R. D., & Gevers, J. K., 2013. Understanding
health care providers' reluctance to adopt a national
electronic patient record: an empirical and legal
analysis. Medicine And Law, 32(1), 13-31.
Health Information Exchange and Related IT-security Practices in European Hospitals
545
