
A Systematic Review of eHealth Interventions for Healthy Aging:
Status of Progress
Idrissa Beogo
1
, Phillip Van Landuyt
2
, Marie-Pierre Gagnon
1,3
and Ronald Buyl
2
1
Research Center of the Centre Hospitalier de Québec-Université Laval, 10 de l’Espinay, Quebec, Canada
2
Faculty of Medicine and Pharmacy, Vrije Universiteit Brussel, Laarbeeklaan 103, Jette, Belgium
3
Faculty of Nursing Sciences, Université Laval, Québec, 1050 Avenue de la Medecine, Quebec, Canada
Keywords: eHealth, Healthy Aging, Aging, Systematic Review.
Abstract: Worldwide, old age population is projected to attained 2 billion by 2050, raising challenges for healthcare,
social security, pension and long-term care. Several eHealth interventions have been as proposed as promising
avenues to support healthy aging (HA), but effectiveness has not been synthesised. This study aims to
systematically review the effectiveness of eHealth interventions for HA. We performed standardized searches
in relevant databases to identify (quasi)-experimental studies evaluating the effectiveness of eHealth
interventions for HA. Outcomes of interest are: wellbeing, quality of life, activities of daily living, leisure
activities, knowledge, evaluation of care, social support, skill acquisition and healthy behaviours. We also
consider adverse effects such as social isolation, anxiety, and burden on informal caregivers. Two reviewers
will independently assess studies for inclusion. Data extraction is based on standardised tools and done
independently by two reviewers. An initial search led to 7039 potentially relevant citations. After screening
titles and abstract, 60 full text articles were further assessed, of which 12 (presenting 11 studies) were finally
retained for the review. Effect sizes related to each type of eHealth intervention will be calculated on the final
selection. If not possible, we will present the findings in a narrative form. This systematic review will provide
unique knowledge on the effectiveness of eHealth interventions for supporting HA.
1 INTRODUCTION
Worldwide, the proportion of people aged over 65
years is projected to attain 2 billion by 2050 (Kinsella
and Phillips, 2005). This change, associated with
progresses in healthcare but mostly with
improvements in living conditions, put aging at the
forefront of public concerns. However, population
aging also associated with an increase in the
prevalence of chronic diseases (Reis et al., 2013),
which challenges the sustainability of healthcare and
social services delivery (Illario et al., 2015). In view
of these challenges, following the World Health
Organization (WHO) meeting on healthy aging
(World Health Organization, 2002), several
initiatives has spurred, among which eHealth
Interventions for Healthy Aging.
Healthy aging (HA) is defined as “the process of
optimizing opportunities for physical, social and
mental health to enable older people to take an active
part in society without discrimination and to enjoy an
independent and good quality of life” (Swedish
National Institute of Public Health, 2006).
HA includes an active engagement with life,
optimal cognitive and physical functioning and low
risk of disease that enables older people to participate
within their limitations and continue to be physically,
cognitively, socially and spiritually active (Hansen-
Kyle, 2005). People live longer and want to stay
active, happier, and healthy although the decline in
the biological, physiological and cognitive systems
inherent to aging may limit full social, cultural and
intellectual engagement in the elderly (Jin et al.,
2015). As the first wave of baby-boomers reaches the
retirement age, policies are levied to keep seniors
active in prolonging the working period in several
countries (e.g. Greece, France, Denmark) (Hofäcker,
2014, Hofäcker and Naumann, 2015). This cohort and
onward generations in the “early old age” (50 years
and above) use e-tools in their daily activities (Pew
research Center, 2014). Ensuring HA for the
population is thus a priority in developed countries,
but also in developing countries that foresee aging of
their population in a near future (Henriquez-Camacho
et al., 2014).
eHealth is an overarching term that encompasses
122
Beogo, I., Landuyt, P., Gagnon, M-P. and Buyl, R.
A Systematic Review of eHealth Interventions for Healthy Aging: Status of Progress.
In Proceedings of the International Conference on Information and Communication Technologies for Ageing Well and e-Health (ICT4AWE 2016), pages 122-126
ISBN: 978-989-758-180-9
Copyright
c
2016 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

the various uses of Information and Communication
Technology (ICT) and web-driven application in the
sphere of health care and health promotion, such as
telemedicine, electronic health records, virtual
interventions and personal health monitoring. With
respect to HA, eHealth applications offer older adults
the opportunity to access health information and
receive health and social care in their homes. These
interactive interventions can empower, engage, and
educate older adults (Hall et al., 2012). eHealth
interventions are among the promising avenue and
receive increasing attention because of their potential
to support a healthy life and the recognition of their
central role in today’s society. In synthesizing the
latest updates, Lattanzio et al. highlight three main
domains of development related to eHealth
innovation: (1) disease management, (2) intelligent
devices to address mobility risks (i.e., falls in elders),
and (3) specific needs for HA (Lattanzio et al., 2014).
In total, they are designed for virtual physical exercise
(Silveira et al., 2013, Wu and Keyes, 2006) ─
wirelessly or not─, to promote social networking
(Rébola, 2015), lifestyle (Cook et al., 2015);
smartphone application are developed to support
elderly autonomy (Willner et al., 2015). Interestingly,
recent studies contended a high intention to adopt e-
tools among older adults (Rosella et al., 2014) as well
as a recognition of their safety (Heinbuchner et al.,
2010, Londei et al., 2009), and their relevance
(Mihailidis et al., 2008). Some other reported that
they are adapted and usable and offer independence
and confidence (Brownsell and Hawley, 2004).
eHealth is evolving rapidly. In the first quarter of
2014 the number of health and wellbeing apps has
reached the cape of 100.000 (Research2guidance,
2014), targeting predominantly chronically ill
patients (31%) and health and fitness-interested
people (28%). Approximately, 500 million
smartphone users worldwide will be using a
healthcare application by the end of 2015. A
substantial part of them are senior clients using these
applications to help themselves to stay fit, monitor
their own health status or keep in contact with their
healthcare provider. In contrast to the growing use of
eHealth to support HA, knowledge about effective
technologies and interventions for HA is clearly
absent. Decision makers need evidence on effective
strategies that could be implemented in order to
maximize health and wellbeing of older adults.
2 OBJECTIVES
This systematic review intends to shed light on the
promise of eHealth interventions in promoting HA
among older adults. This project targets two main
objectives: 1) to identify and systematically summarize
the best available evidence on the effectiveness of
eHealth interventions on HA; 2) to explore how
specific eHealth interventions (age-friendly,
community intervention, public policies) and their
characteristics (e.g.: mode of implementation) may be
implemented to effectively impact HA.
3 METHODS
We are conducting a systematic review of the
literature based on the Cochrane Collaboration
methods (Higgins and Green, 2011).
3.1 Types of Participants
This review considers studies that include male and
female adults aged 50 or more (as 50 years is
generally set as the beginning of the young old age
(Swedish National Institute of Public Health, 2006),
living in the community or in institutional
arrangement (e.g. nursing home), and who were
offered any intervention using eHealth for HA.
Exclusion criteria: 1) People with a terminal illness;
hospitalized in-patients; 2) Older adults with severe
impaired cognition, as measured by the Mini Mental
State Examination(Folstein et al., 1975)
3.2 Types of Interventions
This review consists of studies that evaluate
interventions on HA as defined above, and delivered
through eHealth, including teleHealth and
telemedicine, remote monitoring, internet, mobile
smart phones, interactive digital games, electronic
information systems. The interventions may take place
at home, in a community health center or another
relevant setting. The interventions may be delivered
individually or in groups. The interventions may last
one or more sessions of various time frames. Exclusion
criteria: Interventions that include an important face-
to-face component; Interventions using conventional
telephone, television or radio; Interventions using
technologies without an interactive component;
Interventions targeting treatment, or prevention of
complications of health problems.
3.3 Types of Outcomes
This review considers studies that include one or
A Systematic Review of eHealth Interventions for Healthy Aging: Status of Progress
123

more of the following outcome measures as defined
by the “Outcomes of interest to the Cochrane
consumers & communication review group”
(Cochrane Consumers in Communication Review
Group, 2012). Primary outcomes include: wellbeing,
quality of life, activities of daily living, leisure
activities, biological measures, health-enhancing
lifestyle, self-efficacy, and other related outcomes.
Secondary outcomes include: 1) knowledge and
understanding; 2) Participant decision-making
including decision made and satisfaction with
decision taken; 3) Evaluation of care including goal
attainment; 4) social support; 5) skills acquisition 6)
health behavior including adherence to treatment and
screening; and 7) other relevant outcomes. This study
will also consider adverse effects related to eHealth
interventions on HA in the targeted population.
Adverse effects may include: social isolation,
anxiety, burden on informal caregivers.
3.4 Types of Studies
The review includes any experimental study design
including randomized controlled trials, non-
randomized controlled trials; and quasi-experimental,
before and after studies for inclusion.
Studies published from 2000 up to 2015 in
English, Dutch, French or Spanish are considered for
inclusion.
3.5 Search Strategy
The search strategy aims to find both published and
unpublished studies. A three-step search strategy was
used. An initial exploratory search of Medline and
CINAHL was undertaken followed by an analysis of
the words contained in the title and abstracts, and of
the keywords and index terms used to describe
articles. A second search using all identified
keywords and index terms was then undertaken
across all included databases. Thirdly, after removing
duplicates from the reference manager Endnote, 7039
reference were obtained and are under the first round
of screening to map out those fitting the inclusion
criteria. Further, references list of included studies
will be screened for additional studies.
A final search is planned once ready to draft the
manuscript to identify any new relevant studies on the
topic. The search strategy (table 1) was adapted and
conducted in the following databases: CINAHL,
Cochrane Library, Embase, Eric, Campbell
Collaboration Library, PsycINFO, Web of Science,
and Social Work Abstracts.
3.6 Assessment of Methodological
Quality
Studies selected for retrieval were assessed by two
independent reviewers (IB & PV) for methodological
quality prior to inclusion in the review using the
Cochrane Risk of Bias tool (Higgins and Green,
2011). The disagreements that arose between the
reviewers were resolved through discussion with a
third reviewer (MPG or RB).
3.7 Data Extraction
Data will be extracted from studies included in the
review using a standardized data extraction tool based
on our previous reviews. The data extracted will
include specific details about the interventions,
populations, study methods and outcomes of
significance to the review question and specific
objectives. If needed, we will contact authors of
primary studies for missing information or to clarify
unclear data.
3.8 Data Synthesis
Where possible, data will be pooled in statistical
meta-analysis. Effect sizes expressed as odds ratio
(for categorical data) and weighted mean differences
(for continuous data) and their 95% confidence
intervals will be calculated for analysis.
Heterogeneity will be assessed statistically using the
standard Chi-square and also explored using
subgroup analyses based on the different study
designs included in the review. If statistical pooling is
not possible, we will present the findings in a
narrative form. We will undertake a qualitative
analysis of the descriptions of the interventions, as
provided in each report, to detail the interventions
components, inspired from the taxonomy of
interventions developed by EPOC (Effective Practice
and Organisation of Care (EPOC), 2015).
4 RESULTS
Figure 1 presents the flow diagram of the systematic
review. We have already conducted initial searches in
bibliographic databases and retrieved 7039 citations.
After initial screening of titles and abstracts, 60
publications were kept for further evaluation. The
study selection led to a final sample of 12 publications
describing 11 studies (see figure 1). Data extraction
from selected studies will be done from February to
ICT4AWE 2016 - 2nd International Conference on Information and Communication Technologies for Ageing Well and e-Health
124
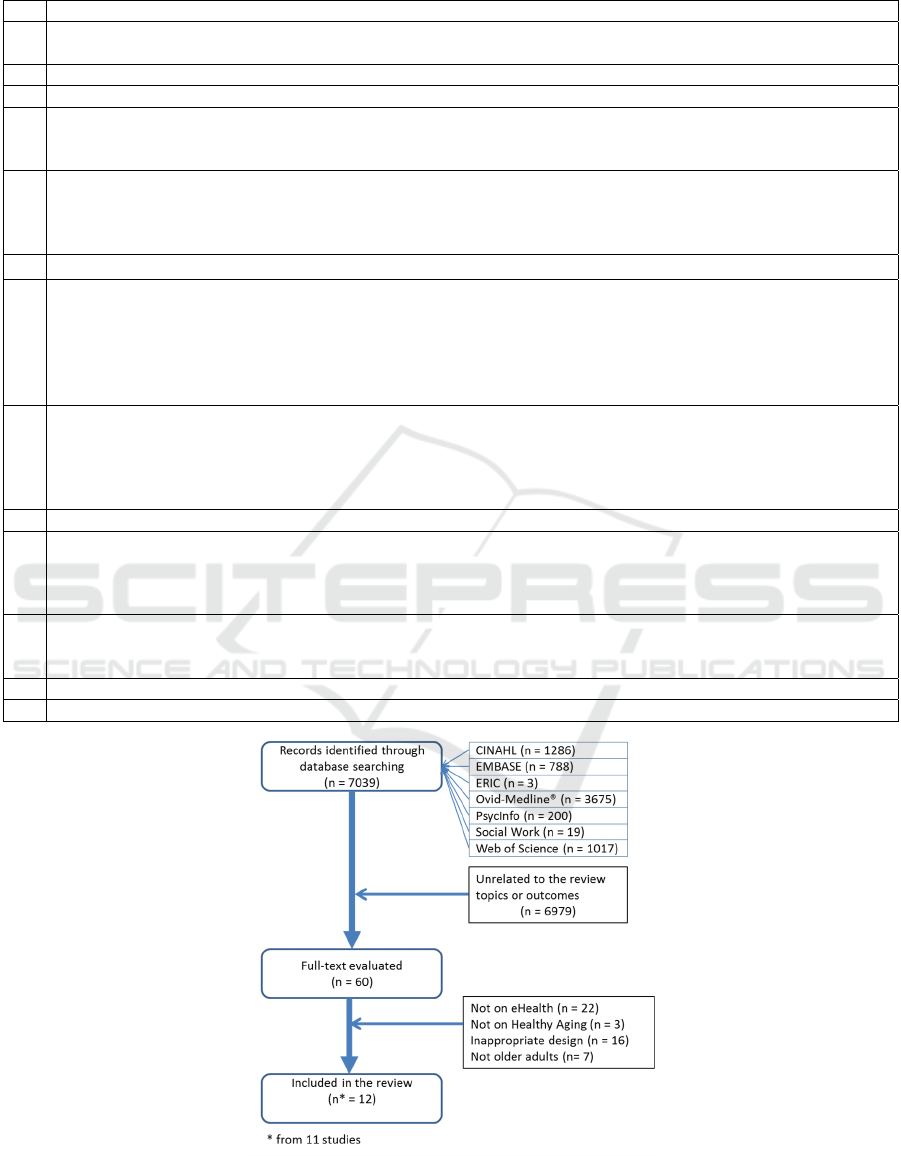
Table 1: Search strategy used in OVID-Medline ®.
No Concept equations
1 ("active ageing" or "active aging" or "Healthy ageing" or "Healthy aging" or Aging or "Middle Aged" or Aging or
Ageing or old or elder* or senior).ab,ti.
2 Middle Aged.mp. or exp Middle Aged/ or exp Aging/ or exp Aged/
3 1 or 2
4 (Project or program or Support or programme or intervention or "Health Education" or "Health Promotion" or
"Occupational Health Services" or "Health Services for the Aged" or "Preventive Health Care" or "Primary
Prevention").ab,ti.
5 Health Education.mp. or exp Health Education/ or Health Promotion.mp. or exp Health Promotion/ or
Occupational Health Services.mp. or exp Occupational Health Services/ or Health Services for the Aged.mp. or
exp Health Services for the Aged/ or Primary Prevention.mp. or exp Primary Prevention/ or Occupational Health
Nursing.mp. or exp Occupational Health Nursing/
6 4 or5
7 ("Health Communication" or Telenursing or Tele-nursing or "Health Informatics" or "Information Technology" or
"Information Technology Personnel" or internet or "World Wide Web" or Smartphone or online or on-line or web-
based or "web based" or webbased or "remote monitor*" or "interactive digital game" or "electronic information
system" or "Computer-Assisted" or "Computerized Health Record" or Telemedicine or Tele-medicine or
TeleHealth or TeleHealth or "Mobile health" or "Remote Consultation" or "Electronic Health Records" or "Public
Health Informatics" or "personal digital assistant").ab,ti.
8 Health Communication.mp. or exp Health Communication/ or exp Remote Consultation/ or Telenursing.mp. or
exp Telemedicine/ or exp Telenursing/ or exp Internet/ or exp Medical Informatics/ or Information
Technology.mp. or Information Technology Personnel.mp. or smartphone.mp. or exp Cell Phones/ or exp
Electronic Health Records/ or Computerized Health Record.mp. or TeleHealth.mp. or Public Health
Informatics.mp. or exp Public Health Informatics/
9 7 or 8
10 Health Education.mp. or exp Health Education/ or exp Health Behavior/ or exp Health Knowledge, Attitudes,
Practice/ or Health Knowledge.mp. or Quality of Life.mp. or exp "Quality of Life"/ or Self Efficacy.mp. or exp
Self Efficacy/ or Social Support.mp. or exp Social Support/ or Life Style.mp. or exp Life Style/ or Health
Literacy.mp. or exp Health Literacy/ or Risk Reduction Behavior.mp. or exp Risk Reduction Behavior/
11 ("Health Knowledge" or "Health Behavior" or "Quality of Life" or "Self-Efficacy" or "Social Support" or "Life
Style" or "health education" or "health knowledge attitude and practice" or "health Attitude" or "Health Literacy"
or "Health Behaviour" or "Quality of Life" or "psychco-Social Support" or "Risk Reduction Behavior").ab,ti.
12 10 or 11
3 and 6 and 9 and 12
Figure 1: Study selection and flow diagram.
A Systematic Review of eHealth Interventions for Healthy Aging: Status of Progress
125

March 2016, and data synthesis will be completed in
May 2016.
5 CONCLUSIONS
Aging population is a worldwide topical issue and
eHealth a promising resource to address this raising
challenge. This review, first of its kind, will shed light
on eHealth as promising resource to support HA. The
findings from this systematic review stemmed from
salient eHealth interventions implemented will
engender insight regarding the role of eHealth to
answer the increasing needs of an aging population.
The findings will offer possible alternatives for better
policy making option for HA.
REFERENCES
Brownsell, S & Hawley M.S. 2004. Automatic fall
detectors and the fear of falling. Journal of
Telemedicine and Telecare, 10, 262-266.
Cochrane consumers in communication review group 2012.
Outcomes of Interest to the Cochrane Consumers &
Communication Review Group 2012.
Cook, R. F., Hersch, R. K., Schlossberg, D. & Leaf, S. L.
2015. A Web-based health promotion program for older
workers: randomized controlled trial. Journal of
medical Internet research, 17.
Effective practice and organisation of care (EPOC) 2015.
Suggested risk of bias criteria for EPOC reviews. EPOC
Resources for review authors. Oslo: Norwegian
Knowledge Centre for the Health Services,.
Folstein, M., Folstein, S. & Mchugh, P. 1975. Mini-mental
state : a practical method for grading the cognitive state
of patients for the clinician. J Psychiatr Res, 12, 189-
198.
Hall, A. K., Stellefson, M. & Bernhardt, J. M. 2012.
Healthy Aging 2.0: The Potential of New Media and
Technology. Preventing Chronic Disease.
Hansen-Kyle, L. 2005. A Concept Analysis of Healthy
Aging. Nursing Forum, 40, 45-57.
Heinbuchner, B., Hautzinger, M., Becker, C. & Pfeiffer, K.
2010. Satisfaction and use of personal emergency
response systems. Z Gerontol Geriatr, 43, 219-23.
Henriquez-Camacho, C., Losa, J., MirandA, J. J. & Cheyne,
N. E. 2014. Addressing healthy aging populations in
developing countries: unlocking the opportunity of
eHealth and mHealth. Emerg Themes Epidemiol, 11,
136.
Higgins, J. & Green, S. 2011. Cochrane handbook for
systematic reviews of interventions Version 5.1. 0
[updated March 2011].
Hofäcker, D. 2014. In line or at odds with active ageing
policies? Exploring patterns of retirement preferences
in Europe. Ageing and Society, 35, 1529-1556.
Hofäcker, D. & Naumann, E. 2015. The emerging trend of
work beyond retirement age in Germany. Increasing
social inequality? Z Gerontol Geriatr, 48, 473-9.
Illario, M., Vollenbroek-Hutten, M., Molloy, D. W.,
Menditto, E., Iaccarino, G. & Eklund, P. 2015. Active
and Healthy Ageing and Independent Living. J Aging
Res, 2015, 542183.
Jin, K., Simpkins, J. W., Ji, X., Leis, M. & Stambler, I.
2015. The Critical Need to Promote Research of Aging
and Aging-related Diseases to Improve Health and
Longevity of the Elderly Population. Aging Dis, 6,
1-5.
Kinsella, K. & Phillips, D. 2005. Global Aging: The
Challenge of Success. Population Reference Bureau,
Washington DC,.
Lattanzio, F., Abbatecola, A. M., Bevilacqua, R., Chiatti,
C., Corsonello, A., Rossi, L., Bustacchini, S. &
Bernabei, R. 2014. Advanced technology care
innovation for older people in Italy: necessity and
opportunity to promote health and wellbeing. J Am Med
Dir Assoc, 15, 457-66.
LondeI, S. T., Rousseau, J., Ducharme, F., St-Arnaud, A.,
Meunier, J., Saint-Arnaud, J. & Giroux, F. 2009. An
intelligent videomonitoring system for fall detection at
home: perceptions of elderly people. J Telemed
Telecare, 15, 383-90.
Mihailidis, A., Cockburn, A., Longley, C. & Boger, J. 2008.
The acceptability of home monitoring technology
among community-dwelling older adults and baby
boomers. Assist Technol, 20, 1-12.
Pew Research Center 2014. Older Adults and Technology
Use.
Rébola, C. B. 2015. Designed Tecnologies for Healthy
Aging, Morgan & Claypool Publishers.
Reis, A., Pedrosa, A., Dourado, M. & Reis, C. 2013.
Information and Communication Technologies in
Long-term and Palliative Care. Procedia Technology,
9, 1303-1312.
Research2guidance 2014. mHealth App Developer
Economics 2014 The State of the Art of mHealth App
Publishing.
Rosella, L. C., Fitzpatrick, T., Wodchis, W. P., Calzavara,
A., Manson, H. & Goel, V. 2014. High-cost health care
users in Ontario, Canada- demographic, socio-
economic, and health status characteristics. BMC
Health Services Research 14, 1-13.
Silveira, P., Van Het Reve, E., Daniel, F., Casati, F. & De
Bruin, E. D. 2013. Motivating and assisting physical
exercise in independently living older adults: a pilot
study. Int J Med Inform, 82, 325-34.
Swedish National Institute of Public Health 2006. Healthy
aging: a challenge for Europe. Stockholm.
Willner V, Schneider C, Feichtenschlager M. 2015. eHealth
2015 Special Issue: Effects of an Assistance Service on
the Quality of Life of Elderly Users. Appl Clin Inform,
6, 429-42.
World Health Organization 2002. Active Ageing: A Policy
Framework. Geneva.
Wu, G. & Keyes, L. M. 2006. Group Tele-Exercise for
Improving Balance in Elders. Telemedicine and
eHealth, 12, 562-571.
ICT4AWE 2016 - 2nd International Conference on Information and Communication Technologies for Ageing Well and e-Health
126
