
A Real-World Case Scenario in Business Process Modelling for Home
Healthcare Processes
Latifa Ilahi
1
, Sonia Ayachi Ghannouchi
1
and Ricardo Martinho
2,3
1
RIADI Laboratory - National School of Computer Science, University of Manouba, Manouba, Tunisia
2
CINTESIS, FMUP, University of Porto, Porto, Portugal
3
ESTG, Polytechnic Institute of Leiria, Leiria, Portugal
Keywords: Home Healthcare, BPM, BPMN, Tunisia, Real World Case Scenario.
Abstract: Organizations strive to improve the quality of provided services to their customers by making efficient use
of Business Process Management (BPM). Home healthcare structures are considered as an enabler for
linking daily life of patients with Information and Communication Technologies (ICTs). BPM relies first on
business process model specifications that capture the desired workflows in the organization and how
exceptional conditions should be handled. Home healthcare is still less developed in Tunisia than in other
countries such as Canada, United States, Australia, France and Italy. This is due to many reasons, being one
of the most relevant the expensive cost of hospitalization at home with no support from health insurances. In
addition, it is badly organized, with many ad-hoc processes, making them hard to implement and improve.
In this paper, we assess a real-world case scenario of home healthcare in Tunisia through interviews with
involved actors in a private clinic. Also, we present the derived process models of home healthcare for this
case. Our main goal is to have a sound starting point for the BPM cycle, by accurately modelling all
business processes involved in home healthcare. With these models, we intent to: 1) optimize the processes
by automating and rationalizing some activities, 2) implement them in a Business Process Management
System (BPMS), 3) execute them, and 4) improve them through instance harvesting and remodeling.
1 INTRODUCTION
The healthcare domain holds one of the world's
largest hybrid organizations (Ilahi et al., 2014). In
fact, the increased life expectancy leads to a more
than proportionate increase of people called
"fragile", which may suffer from chronic diseases,
are not autonomous and need assistance with the
direct consequence of increased costs of care and
hospitalization. Governments and health insurance
companies are sensitized by such conditions.
Accordingly, the establishment of an efficient
logistics support for these people becomes a
necessity. In this context, many economic, public
and private actors are seeking solutions to maintain
the quality of healthcare system ensuring lower cost.
One of the options for that is the transfer of some
hospital care to home (Zefouni, 2012 and FNEHAD,
2009). Indeed, this focus is interesting from both
social (for instance, ensuring a degree of autonomy
to the elderly and respect their wishes to be treated
at home and close to their families) and financial
aspects (including the high costs of hospitalization
or living in special homes).
However, continuity and collaboration problems
of care remain and persist. These problems have
already been emphasized by several works (Kun,
2001 and Bricon-Souf et al., 2005). We could
observe them in our home healthcare processes case
study, where continuity and collaboration are
ensured in an unorganized manner, and need more
improvements.
From 2014’s demographic statistics (INS, 2014)
about aging of Tunisian population, life expectancy
is around 80 years. Tunisia now has 11% of the
population over 60 years. People aged over 75 years
already represent 8.6% of the population, and they
will almost double in ten years.
As we have found, care collaboration is one of
the major challenges of home healthcare. The
technologies of Business Process Management
(BPM) and, more specifically, the design (modeling)
aspect, are known to typically offer collaboration
support by information technologies. The aim of this
166
Ilahi, L., Ghannouchi, S. and Martinho, R.
A Real-World Case Scenario in Business Process Modelling for Home Healthcare Processes.
DOI: 10.5220/0005654301660174
In Proceedings of the 9th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2016) - Volume 5: HEALTHINF, pages 166-174
ISBN: 978-989-758-170-0
Copyright
c
2016 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

research work is to elicit process models of home
healthcare in a Tunisian private clinic, since there is
no supported home healthcare in the public sector.
Also, we present some of Business Process
Modeling (BPMo) challenges specifically focusing
on home healthcare processes. This is in order to be
able to begin the Business Process Management
(BPM) cycle. For this, we performed interviews with
involved actors to design main home healthcare
processes carried out in Tunisia. We could also
benefit from our previous experiences in modeling
telemedicine processes (Ilahi and Ghannouchi, 2013
and Ilahi et al., 2014).
The remainder of this paper is organized as
follows: Section II describes the basic concepts
regarding home healthcare. Section III highlights
BPM for home healthcare. Section IV describes our
case study in Tunisia of home healthcare processes,
along with the associated process models. Section V
presents our next research steps and, finally, in
section VI, we present main conclusions.
2 HOME HEALTHCARE
Home healthcare is a system of care provided by
skilled practitioners to patients in their homes under
the direction of a physician. Home healthcare
services include nursing care; physical,
occupational, and speech-language therapy; and
medical social services (Bachouch, 2010).
Home healthcare has grown into a vital source of
healthcare, especially for older adults, who represent
72% of recipients (Redjem, 2013). It represents a
very open term and may cover every treatment at
home: from basic home healthcare to advanced
home healthcare. The basic home healthcare consists
at rendering health services to the aged or disabled
individuals in their home. In this case, different
persons and services are implied (medical and para-
medical professionals, nursing services, physical,
homemaker services, and social services). Also,
family members are involved in the healthcare
delivery. Concerning advanced home healthcare, it
may comprise the introduction of technological
solutions as e-mail consultations, clinical robots,
advanced sensor surveillance (for collecting vital
signs and physiological parameters), etc. In this
case, the patient may be less frequently visited by
involved actors than in regular basic home
healthcare (Arbaoui et al., 2012). Our work focuses
on advanced home healthcare and the use of
Information and Communication Technologies
(ICT), namely BPM technologies, to support and
improve it.
Unfortunately, home healthcare has to face
several challenges, such as funding limitations, large
geographic distances that make such resources often
more costly for rural patients, and issues of clinical
workforce distribution that impose access barriers to
these services. It is a general premise that ICT can
address these challenges and enhance home
healthcare services (Arbaoui et al., 2012). In fact,
advances in telecommunications have the potential
to support healthcare delivery and education. The
use of ICT can lead to a fundamental redesign of
home care processes based on the use and
integration of electronic communication at all levels
(Ellenbecke, 2008).
2.1 Basic Concepts
Home care providers deliver services at the patient's
own home. The goals of home healthcare services
are to help individuals to improve function and life
with greater independence; to promote the patient’s
optimal level of well-being; and to assist the patient
to remain at home, avoiding hospitalization or
admission to long-term care institutions (Demiris,
2010).
We may have recourse to home healthcare
according to different types of care (Zefouni, 2012
and FNEHAD, 2009):
Occasional care, especially in case of unstable
state of disease. Technical and complex care for
a predefined period (e.g. chemotherapy or
antibiotics);
Care rehabilitation at home, especially following
the acute phase of a neurological or heart
disease, or orthopedic treatment or early return
after childbirth;
Palliative care, especially intended to support
long term diseases;
Home healthcare goals stem mainly from the degree
of sector development in the government. Based on
the reports of (Lasbordes, 2010 and FNEHAD,
2009), the main goals of home healthcare are:
Ensure the safety of people dependent at home;
Ensure care quality, accessibility and
coordination.
Keeping patients in their homes areas. This is in
order to preserve the autonomy of the individual
and to avoid the breakdown of social ties;
Ensure the continuity of care, including keeping
the records of care and interventions in person
care at home;
Minimize the cost of care at home.
A Real-World Case Scenario in Business Process Modelling for Home Healthcare Processes
167
2.2 Current State Worldwide and in
Tunisia
Home healthcare structures have attracted a great
interest in the United States, Canada, Scandinavian
countries and the United Kingdom. Certainly, the
approaches differ from one country to another
(Polton, 2003), or within the same country (Abelson,
2004), but all seem to find a promising and
interesting field to be developed.
Some countries have resorted to these new home
healthcare support modes in order to free up hospital
beds. Others aim to control hospital costs. The
improvement of life quality of the patient was not a
primary objective for the countries studied by
(Raffy-Pihan, 1994).
According to a study by (Chevreul et al., 2004),
the French home healthcare system is closer to the
Australian one. This is from the point of view of
partial or total substitution of the offer acute care
hospitalizations in short-stay service. In the UK, the
system is closer to the Canadian’s, with oriented
continuous care for maintain or return to home of the
chronically ill or elderly patients. In Table I, we
present country examples home healthcare structures
studied by (Chevreul et al., 2004) and we added
Tunisia to this table, regarding the same factors
analyzed, namely the main reasons for recourse to
home healthcare and the nature of delivered care:
Table 1: Examples of worldwide structures (Chevreul et
al., 2004).
Countries
Main reasons for recourse
to home healthcare
Nature of delivered care
United
Kingdom
The overcrowding of care
beds at hospital due to not
justified clinically
accommodation and to
deficiencies in ambulatory
care.
Basic care, continuous,
for maintain / return to
home chronically ill or
elderly patients.
Canada
Compression of hospital
beds.
Basic care, long term
care substituting for
institutional care and
acute hospital care.
Australia
Inadequate traditional
hospital services
Highly technical care
France
The overcrowding of beds
at traditional hospital
Highly technical care,
acute or episodic care,
continuous care, follow-
up and rehabilitation
care
Tunisia
No supported home
healthcare in the public
sector.
Basic care, continuous
care for maintain / return
to home chronically ill or
elderly patients.
2.2.1 Description of the State of the Art in
Other Countries
Based on two experiences in Tunisia and Portugal
and some literature studies on related field (Raffy-
Pihan, 1994, Chevreul et al., 2004, Wendt, 2004 and
HAS, 2009), we present a description of home
healthcare in some countries. In fact, hospitals are
just one component in the overall organization of a
care system which includes primary care, accessible
during a first contact for unselected health problems,
and responsible for ensuring the continuity of care.
The responsibility of primary care falls mostly at the
local level (region, municipality or department).
While the general doctor is considered as the
entry point to focus on primary care, the direct
access to a specialist in primary care settings is
possible directly in Germany, Austria, Belgium,
France, and Switzerland. In these countries, the
number of specialists practicing in the primary care
setting is important. In several countries (UK,
Sweden, Portugal, Finland and Greece), primary
care is provided by multidisciplinary health centers.
In Sweden and the United Kingdom, the first contact
with a health professional is often performed by a
nurse. Finland has beds in its care center, making it
truly an intermediary structure between outpatient
care and hospitalization. In order to limit recourse to
general hospitals, most countries recommend the
primary care structure as the entry level of care,
either in a partial (Germany, Austria, Portugal,
Switzerland, France, Belgium, Finland, Spain) or
total manner (Denmark, Great Britain, Italy,
Norway, Netherlands).
To ensure hospital care, European countries rely
on three types of structures: public hospitals, non-
profit private hospitals and for-profit private
hospitals. Only a few countries rely almost all of
their hospital services in public hospitals (Denmark,
Finland, Norway, Sweden) or a majority of private
structures typically nonprofit (Belgium,
Netherlands). Most rely on both the public sector
and large private sector. The structures are often
small, and the number of beds is generally more
important in the public sector than in the private
sector. Moreover, private structures are, in most EU
countries, mostly non-profit hospitals (except
Austria and France).
In some countries (particularly Germany), a part
of the private institutions is providing care only to
some selected patients. We may identify three
groups of countries: those who had a lot of
equipment of any kind (Finland, Switzerland,
Austria, and Belgium), those who were poorly
HEALTHINF 2016 - 9th International Conference on Health Informatics
168

equipped (UK, Spain), and those that were heavily
equipped in some areas but weak in others (France,
Germany).
The responsibility of primary care falls mostly at
the local level (region, municipality or department).
This is the case for Denmark, Spain, Finland,
Greece, Great Britain, Ireland, Italy, Norway,
Portugal and Sweden. In countries with social
insurance systems (Germany, Austria, Belgium,
France and Switzerland), the insurance of credit
unions are responsible for supporting costs. While
the general doctor is considered as the entry point to
focus on primary care, the direct access to a
specialist in primary care settings is possible directly
in Germany, Austria, Belgium, France, and
Switzerland. In these countries, the number of
specialists practicing in the primary care setting is
important (48.5% in Germany, 50% in Austria).
In many countries, primary care is provided by
health centers. In this context, the access to a
specialist in primary care is sometimes possible,
particularly for obstetrics and gynecology, minor
surgery and psychiatry (Spain, Finland, Greece,
Portugal and Sweden). However for other
specialties, access to a specialist when needed is
done almost exclusively at general hospitals.
Registration with a doctor or health center, for a
time period and with limited choice, is the most
common model (Denmark, Spain, Great Britain,
Ireland, Italy, Norway, Netherlands, Portugal, and
Sweden). In other countries and most recently,
registration is encouraged by a financial incentive
mechanism (Germany and France). The status of
medical doctors is mostly liberal, but in health
centers, medical doctors are sometimes hired
employees (Finland, Portugal and Sweden).
Home healthcare includes home help
(housekeeping, cooking) and nursing. Home help is
not included in health care, but is considered part of
social services. However, nursing is part of health
care. They include rehabilitation care, support,
health promotion and technical nursing care for sick
people at home. Such care is provided in very
different ways from one country to another. They
vary depending on the chosen organizational model.
In some countries the nursing at home have long
been highly developed (Belgium, Denmark, Finland,
Ireland, Netherlands and United Kingdom), while in
others they are still developing (Austria, Greece,
Italy, Luxembourg, Portugal and Spain).
3 BPM FOR HOME
HEALTHCARE
Some research works highlight the importance of the
organizational aspects in the success of an ICT-
home healthcare project (Arbaoui et al., 2012).
Other works on home healthcare (Koch, 2004) have
dealt more with developing technical-based
solutions for home monitoring or home
telemedicine, leaving process aspects questions
unanswered (Arbaoui et al., 2012). Indeed, some
observations (Hamek et al., 2005) show that the
requirements of the home healthcare actors (nurses,
physicians, home healthcare organizations,
caregivers and patient’s family members) are more
oriented towards the improvement of the
organization and management of the home
healthcare system over a more intensive use of home
telemedicine (Arbaoui et al., 2012).
BPM represents a valuable asset in the healthcare
domain (Stefanelli, 2004), given the
competitiveness, rapid advancement and especially
the expansion of communication techniques and new
technologies in all research areas, as well as the
effectiveness of BPM tools to automate and better
manage business processes of organizations. It relies
on process models to identify, review, validate,
represent and communicate process knowledge
(Kunzle, 2011 and Müller, 2011).
Regarding several success stories on the uptake
of BPMS in industry and the emergent process-
orientation of enterprises, BPM technologies have
not had a widespread adoption in the healthcare
domain (Reichert, 2011 and Stefanelli, 2004). A
main reason for this has been the rigidity enforced
by the first generation of workflow management
systems, which inhibits the ability of a hospital to
respond to process changes and exceptional
situations in an agile way (Dadam, 2000). Process-
aware hospital information systems must be able to
cope with exceptions, uncertainty, and evolving
processes (Reichert, 2011). In this context, BPM
represents a response to design, manage, automate
and evaluate care processes. Another work of
Arbaoui et al. (2012) adopts a process based
approach to tackle home healthcare domain in order
to highlight the importance of organizational aspects
in the success of an ICT-home healthcare project.
They consider that a home healthcare may comprise
three sub-processes: 1) Organizational; 2)
Organizational care and 3) Care sub-processes. In
our work, we adopt a BPMN-based modeling
approach to organize home healthcare processes and
tackle associated challenges. Also, we adopt the
A Real-World Case Scenario in Business Process Modelling for Home Healthcare Processes
169
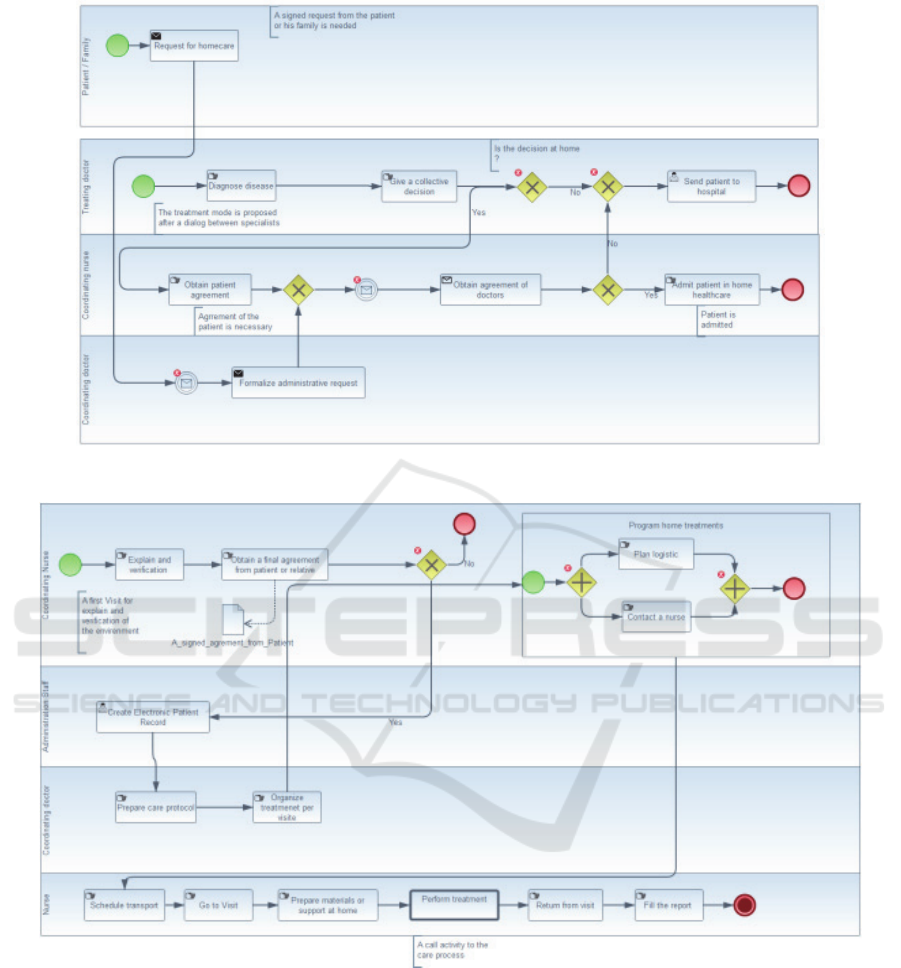
Figure 1: Organizational process model according to BPMN 2.0 Standard.
Figure 2: Organizational care process model according to BPMN 2.0 Standard.
division depicted by (Arbaoui et al., 2012).
4 HOME HEALTHCARE
PROCESSES: A CASE STUDY
IN TUNISIA
In this section, and following our interviews with the
involved actors (2 doctors, 3 nurses &
administration staff), we describe how home
healthcare is realized in Tunisia, who are the actors,
which are the different tasks and how we can design
all this information in a process model. We also
identify particular problems of home healthcare
processes concerning roles and task assignments
observed during real-world care process execution in
a home medical environment.
HEALTHINF 2016 - 9th International Conference on Health Informatics
170

4.1 Collecting Home Healthcare
Information
To study home healthcare processes, we led a field
research in which we interviewed actors with
different roles in the patient homecare (mainly nurse
coordinators, health aides and medical doctors). We
also followed the professionals in their daily work.
These observations have given us an overview on
the home healthcare management.
4.2 Proposed Models
The overall home healthcare process is divided into
three sub-processes, namely: 1) patient admission; 2)
organizational care; and 3) patient care.
4.2.1 Patient Admission Sub-process
This sub-process represents the result from
multidisciplinary consultation carried out between
different specialists. Once accepted to the home
healthcare mode, it will only be possible to involve
the treating doctor, the patient and her/his family.
The later should give an initial agreement with a
favorable opinion for the financial burden estimate.
Fig. 1 presents the organizational process model
according to the BPMN 2.0 standard. In fact, when
the disease is detected for a patient after diagnosis,
treatment and mode of treatment are proposed after a
dialog between different specialists. If the patient is
not accepted for home healthcare, s/he will be
treated in institutions or in traditional
hospitalization. This assumption of home care
management will be proposed to the patient under
her/his agreement. As shown in Fig. 1, the written
request of care is sent to the home healthcare
structure accompanied with details of treatment for
the patient. This request is then regulated by a doctor
and a nurse coordinator according to geographic,
medical, social and environmental criteria. In reality,
very few requests end up with a refuse (Bricon-souf
et al., 2005). Once the request is accepted, the type
of support of home healthcare is defined for patient,
which means the end of the admission sub-process.
4.2.2 Organizational Care Sub-process
Once the patient is admitted, a home visit is made by
the nurse coordinator of the establishment. S/he aims
to explain the full list of support programs for the
patient and to identify her/his needs. Then, the
patient may decide to be treated at home or to stay in
the hospital. If s/he goes for home healthcare,
hospitalization at home is definitely confirmed and
the record of patient will be created for a fixed
period.
As shown in Fig. 2, the patient's final
confirmation leads to a programming of home
treatments respecting the sequence of predefined
care prescriber and written by her/his treating
doctor. It is insured by the nurse coordinator of
home healthcare establishment. The next step of the
organization is to inform the planning of care for
logistics, nurses and treating doctor. Once the actors
defined, the nurse coordinator has the mission to
explain the care management and dates at which the
patient will need their intervention.
4.2.3 Patient Care Sub-process
The care sub-process is the core of home healthcare.
It is here where the various internal and external
actors are involved around the patient to deliver care
or services. This sub-process depends on the nature
of the diagnosis. At this step, there will be the
execution of care by appropriate actors and the
immediate reporting of related information as
follows:
Team providing care coordinating doctor of
home healthcare structure treating doctor
According to the patient’s diagnosis, the set of
involved actors becomes revealed (e.g., nurses,
physicians or other caregivers). In our care process
model, we present a lane for a coordinating nurse
which will notify all the needed actor(s) to be in
charge of care execution at home. This process
begins with a prescription from a treating doctor.
After that, the coordinating doctor will prepare the
care protocol in order to be organized per visit.
Then, the coordinating nurse informs all involved
actors. After treatment per visit is done, the nurse
must follow-up the patient’s health state and prepare
a report. If the state is abnormal, the information
should pass to a treating doctor urgently. At this step
and according to received data from our
interviewees, the treating doctor makes a decision
either on an update of the care protocol or by
making a visit before updating. This update may
result into a new instance of the “Organize treatment
per visit” task.
On the other hand, if patient health state is
normal a conditional gateway takes place in order to
control if current treatment is the last one or still
other visits with other treatments should follow. So,
if there is another visit, the process will return to the
“Accomplishment of treatment(s)” task by the nurse.
Otherwise, i.e. no other treatment, the nurse must
A Real-World Case Scenario in Business Process Modelling for Home Healthcare Processes
171
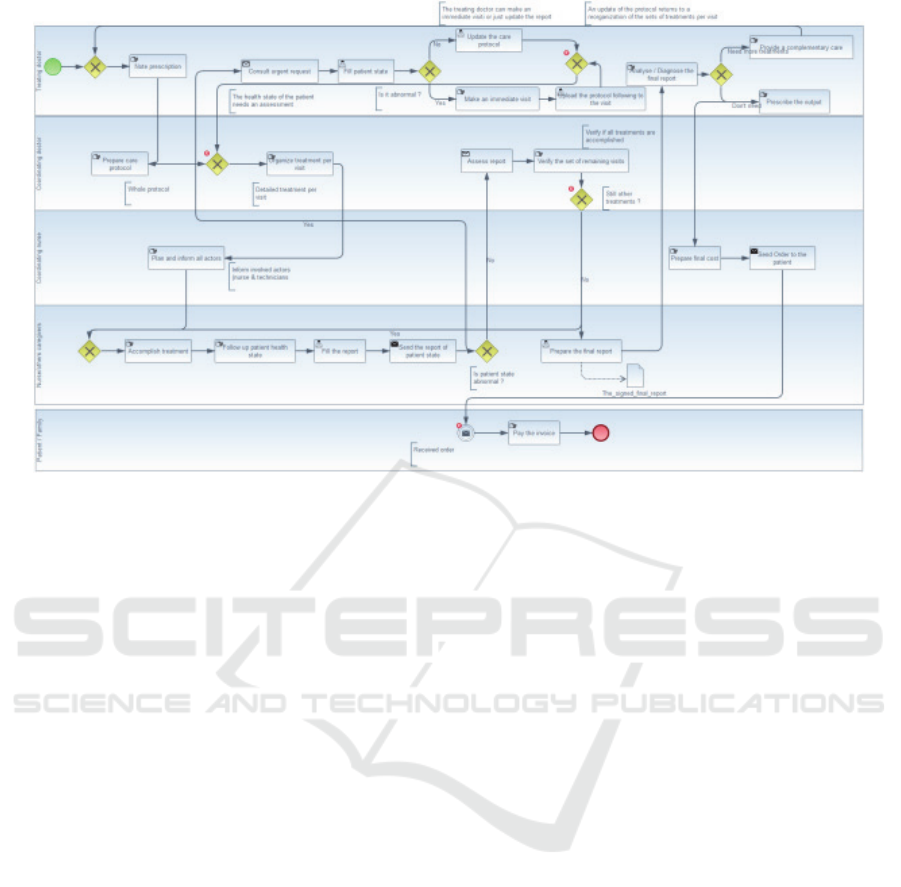
Figure 3: Care process model according to BPMN 2.0 Standard.
prepare a final report. It will be analyzed by treating
doctor in order to make a decision about the patient:
providing a complementary care or prescribing the
output from hospitalization at home. This leads to
preparing a final cost assessment. Finally, the pay of
the invoice ends the process.
4.3 Identified Problems
In this case study in Tunisia, we have identified
some related issues from the interviews performed.
For instance, information about the collaboration
between actors is often lost, e.g. when the patient’s
health state is critical an immediate intervention
from the treating doctor at home is forced. This is
due to the lack of a communication system between
nurse and treating doctor. Currently, the only
communication medium is the mobile. Also, the full
process is mainly based on manual tasks e.g. treating
doctor must go to the patient’s home for frequent
visits. This is due to the lack of ICT-based home
healthcare (electronic records, telemedicine).
Another related problem is the lack of support from
health insurances and lack of home healthcare
related culture. In addition, care coordination is a
challenge. Health professionals need to coordinate
care for a better and fast intervention. Another issue
is that organizational processes (and patient-care
processes in particular), change over time. This may
be due to unpredicted (home healthcare) situations.
4.4 BPMN Coverage for Home
Healthcare Processes
Proposed models describe the care tasks for the
Tunisian home healthcare processes case. Also,
while refining these process models with the
involved home healthcare actors, they do not have
difficulties in identifying the process activities and
actors.
Modeling complex processes, such as those of
home healthcare, has always been a continuous
challenge. As an important factor in modeling,
models must be easily understood by their target
users. Also, an appropriate level of detail aims to
fulfill their development purposes. In addition,
healthcare systems have specific modeling
requirements such as collaboration,
understandability and flexibility.
Following interviews with involved actors, we
assume that our proposed models follow a more
imperative (prescriptive) modelling approach. This
can be observed in the first and second models. On
the other hand, regarding the third care clinical
process, it requires a more declarative modelling
approach, since there may be some tasks that are
executed in a different order from instance to
instance, and unforeseen exceptions may happen.
HEALTHINF 2016 - 9th International Conference on Health Informatics
172

5 NEXT RESEARCH STEPS
In further work, we plan to optimize these models by
analyzing which tasks can be automated or
rationalized. Then we intent to implement these
models of home healthcare processes within the
jBPM BPMS (Cumberlidge, 2007). Then, and after
registering execution instances, we will perform an
analysis in order to identify bottlenecks and
challenges reported from users of the implemented
BPMS. After that, we expect to propose an
improved business process, and again perform the
BPM cycle.
Parallel to these steps, we are aiming to perform
additional interviews on home healthcare processes,
in order to assess the degree of similarity between
business processes for home healthcare in other
countries. From here, we plan to propose a group of
home healthcare processes that can serve as template
and guidelines to help normalize home healthcare in
more than one organization/country.
6 CONCLUSIONS
In this work we have documented process models
which reflect real-world scenario from a private
clinic which provides home healthcare in Tunisia.
Our proposed process models describe all care tasks
in a Tunisian private clinic. We could also observe
that, for these home healthcare processes, the BPMN
language is mostly suited for the first two
organizational and organizational-care processes,
which are more static and rigid. Care (clinical)
processes revealed to be unstable, requiring a
different modeling approach. That is why we agreed
with our interviewed personnel on a more generic
care process, not only because it varies on the
diagnosis, but also because real cases are not too
much predictable.
REFERENCES
Abelson, J., Gold, S. T., Woodward, C., O’Connor, D., &
Hutchison, B., 2004, Managing under managed
community care: the experiences of clients, providers
and managers in Ontario’s competitive home care
sector. Health Policy, 68(3), 359-372.
Arbaoui, S., Cislo, N., & Smith-Guerin, N., 2012. Home
healthcare process: Challenges and open issues. arXiv
preprint arXiv:1206.5430.
Bachouch, R. B., 2010. Pilotage opérationnel des
structures d'hospitalisation à domicile (Doctoral
dissertation, INSA de Lyon).
Bricon-Souf, N., Anceaux, F., Bennani, N., Dufresne, E.,
& Watbled, L., 2005. A distributed coordination
platform for home care: analysis, framework and
prototype. International Journal of Medical
Informatics, 74(10), 809-825.
CHEVREUL, K., COM-RUELLE, L., MIDY, F., &
PARIS, V., 2004. Le développement des services de
soins hospitaliers à domicile: éclairage des expériences
australienne, britannique et canadienne. Questions
d'économie de la santé, (91), 1-8.
Cumberlidge, M., 2007. Business Process Management
with JBoss jBPM. Packt Publishing Ltd.
Dadam, P., Reichert, M., & Kuhn, K., 2000. Clinical
workflows the killer application for process-oriented
information systems? (pp. 36-59). Springer London.
Demiris, G., 2010. Information technology and systems in
home health care. In The role of human factors in
home health care: Workshop summary (pp. 173-200).
Ellenbecker, C. H., Samia, L., Cushman, M. J., & Alster,
K., 2008. Patient safety and quality in home health
care. Patient Safety and Quality: An Evidence-Based
Handbook for Nurses. Rockville (MD).
FNEHAD, 2009, Fédération Nationale des Etablissements
d’Hospitalisation A Domicile, Institutional Report.
Livre Blanc des systèmes d’information en
hospitalisation à domicile (Retreived from
www.fnehad.fr).
Hamek, S., Anceaux, F., Pelayo, S., Beuscart-Zéphir, M.
C., & Rogalski, J., 2005. Cooperation in healthcare-
theoretical and methodological issues: a study of two
situations: hospital and home care. In Proc. of the
2005 annual conference on European association of
cognitive ergonomics (pp. 233-240). University of
Athens.
HAS, 2009. Le recours à l’hôpital en Europe.
Ilahi, L., & Ghannouchi, S. A., 2013. Improving
Telemedicine Processes Via BPM. Procedia
Technology, (9), 1209-1216.
Ilahi, L., Ghannouchi, S. A., & Martinho, R., 2014.
Healthcare information systems promotion: from an
improved management of telemedicine processes to
home healthcare processes. In Proc. of the 2nd Int.
Conf. on Technological Ecosystems for Enhancing
Multiculturality (pp. 333-338). ACM.
Koch, S., 2004. ICT-based Home Healthcare:-Research
State of the Art.
Kun, L. G., 2001. Telehealth and the global health
network in the 21 st century. From homecare to public
health informatics. Computer methods and programs
in biomedicine, 64(3), 155-167.
Künzle, V., & Reichert, M., 2011. PHILharmonicFlows:
towards a framework for objectaware process
management. Journal of Software Maintenance and
Evolution: Research and Practice, 23(4), 205-244.
Lasbordes, P., 2010. La télésanté, un nouvel atout au
service de notre bien-être. Soins la revue de reference
infirmiere, (750), 26.
Müller, R., & Rogge-Solti, A., 2011. BPMN for healthcare
processes. In Proceedings of the 3rd Central-
A Real-World Case Scenario in Business Process Modelling for Home Healthcare Processes
173

European Workshop on Services and their
Composition (ZEUS 2011), Karlsruhe, Germany.
Polton, D., 2003. Décentralisation des systèmes de santé:
Quelques réflexions à partir d'expériences
étrangères. Questions d'économie de la santé, (72), 1-8.
Raffy-Pihan, N., 1994. L’Hospitalisation à Domicile: un
tour d’horizon en Europe, aux Etats-Unis et au
Canada, rapport n 1045. IRDES (ex. CREDES).
Redjem, R., 2013. Aide à la décision pour la planification
des activités et des ressources humaines en
hospitalisation à domicile (Doctoral dissertation,
Université Jean Monnet-Saint-Etienne).
Reichert, M., 2011. What BPM technology can do for
healthcare process support. In Artificial Intelligence in
Medicine (pp. 2-13). Springer Berlin Heidelberg.
Stefanelli, M., 2004. Knowledge and process management
in health care organizations. Methods Inf Med, 43(5).
Wendt, C., & Thompson, T., 2004. Social austerity versus
structural reform in European health systems: a four-
country comparison of health reforms. International
Journal of Health Services, 34(3), 415-433.
Woodward, C. A., Abelson, J., & Hutchison, B. G.,
2001. My home is not my home anymore: improving
continuity of care in homecare. Canadian Health
Services Research Foundation Fondation canadienne
de la recherche sur les Services de santé.
Zefouni, S., 2012. Aide à la conception de workflows
personnalisés: application à la prise en charge à
domicile (Doctoral dissertation, Université de
Toulouse, Université Toulouse III-Paul Sabatier).
HEALTHINF 2016 - 9th International Conference on Health Informatics
174
