
Evaluating Multiple Perspectives of a Connected Health Ecosystem
Noel Carroll
1,2
, Marie Travers
2
and Ita Richardson
1,2
1
ARCH, Centre for Applied Research in Connected Health, University of Limerick, Limerick, Ireland
2
Lero, The Irish Software Engineering Research Centre, University of Limerick, Limerick, Ireland
Keywords: Connected Health, Evaluation, Framework, Information Systems, Management.
Abstract: Connected Health is an emerging model of care that engages technology to improve patient care and
(re)habilitation. It encourages self-efficacy by developing client-centred care pathways and evidence-based
interventions to reduce the need for hospital-led care and empower patients in their homes. It also promotes
improved ‘connectivity’ between healthcare stakeholders by means of timely sharing and presentation of
accurate and pertinent information about patient status. Connected Health initiatives can achieve this
through smarter use of data, devices, communication platforms and people. However, there are few efforts
which have established an evaluation model to encapsulate and assess the value and potential impact of
Connected Health solutions from multiple stakeholders’ perspectives. We examined information systems
(IS) and health information systems (HIS) literature to identify whether a model could apply to Connected
Health. However, many of the evaluation models are narrow in focus but have influenced our development
of the Connected Health Evaluation Framework (CHEF). CHEF offers a generic approach which
encapsulates a holistic view of a Connected Health evaluation process. It focuses on four key domains: end-
user perception, business growth, quality management and healthcare practice.
1 INTRODUCTION
Societal and demographic changes, coupled with
economic challenges, have driven the need for us to
reconsider how we deliver health and social care in
our community (Rodrigues et al., 2012). Healthcare
places considerable financial burdens on both public
purse and personal finance. In addition, due to
demographical shifts, there is a growing demand for
care to be delivered in a more personalised context,
delivering ‘smart’ solutions via technological
devices. Connected Health is an emerging and
rapidly developing field which has the potential to
transform healthcare service systems by increasing
its safety, quality and overall efficiency.
While considered a disruptive technological
approach in healthcare, Connected Health is used by
different industries in various sector contexts (for
example, healthcare, social care and the wellness
sector). Thus, various definitions exist with different
emphasis placed on healthcare, business, technology
and support service providers, or any combination of
these.
Within the research community, Connected
Health is not well defined and remains an
ambiguous concept. The ECHAlliance (2014) group
promote the concept of Connected Health to act as
“the umbrella description covering digital health,
eHealth, mHealth, telecare, telehealth and
telemedicine”. In addition, Caulfield and Donnelly
(2013) defines of Connected Health as “a conceptual
model for health management where devices,
services or interventions are designed around the
patient’s needs, and health related data is shared, in
such a way that the patient can receive care in the
most proactive and efficient manner possible”. The
key here is the connectedness and the manner in
which technological solutions enable healthcare
solutions. In addition, the FDA (2014) describes
Connected Health as “electronic methods of health
care delivery that allow users to deliver and receive
care outside of traditional health care settings.
Examples include mobile medical apps, medical
device data systems, software, and wireless
technology”. Thus, as technological solutions seek
to enable new healthcare relationships and
partnerships, there is a growing interest in
examining information and communications
technology (ICT) to support the development of
Connected Health. Connected Health has been
defined by Richardson (2015) as “patient-centred
Carroll, N., Travers, M. and Richardson, I.
Evaluating Multiple Perspectives of a Connected Health Ecosystem.
DOI: 10.5220/0005623300170027
In Proceedings of the 9th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2016) - Volume 5: HEALTHINF, pages 17-27
ISBN: 978-989-758-170-0
Copyright
c
2016 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
17

care resulting from process-driven health care
delivery undertaken by healthcare professionals,
patients and/or carers who are supported by the use
of technology (software and/or hardware)”.
Therefore Connected Health can be considered to be
a socio-technical healthcare model which extends
healthcare services beyond healthcare institutions.
We capture this in the term ‘ecosystem’. A
Connected Health Ecosystem implies that we to
strike a balance between the various requirements
and dynamics associated with different stakeholder
groups in a modern healthcare sector. For example,
this can include primary care, secondary care,
payers, policy makers, pharmacies, clinicians,
patients, family members, innovators, public
officials, patient groups, academics and
entrepreneurs collaborating to experiment, develop
protocols and tests, and evaluate new Connected
Health service solutions.
As technological solutions seek to enable such
connectivity between healthcare stakeholders
(Hebert and Korabek, 2004), there is a growing
interest in examining how Information and
Communication Technology (ICT) enables
Connected Health solutions. If health technology is
not designed, developed, implemented, maintained,
or used properly, it can pose risks to patients.
Therefore, a continuous evaluation lifecycle is
critical for various stages of the service lifecycle.
However, healthcare technology, such as the case
with Connected Health, lags behind in presenting
evidence-based evaluation on the contribution of
ICT in supporting healthcare services (for example,
Heathfield et al., 1998; Fineout-Overholt et al.,
2005; Misuraca et al., 2013; Tuffaha et al., 2014).
This paper offers an overview of some of the key
evaluation frameworks in e-health and information
systems (IS) and investigates how these can
contribute towards the evaluation of Connected
Health. Bridging these efforts, we propose a
Connected Health Evaluation Framework (CHEF).
CHEF also plays on the fact that we need to evaluate
all of the ‘ingredients’ before we can learn of the
potential impact of Connected Health technology.
2 OBJECTIVE & APPROACH
Connected Health is emerging as a solution which
offers significant promise in how healthcare can
deliver accessible care with improved safety and
patient outcomes. Connected Health encompasses
terms such as wireless, digital, electronic, mobile,
and tele-health and refers to a conceptual model for
health management where devices, services or
interventions are designed around the patient’s
needs.
Considering the emerging nature of Connected
Health, there are few attempts to develop evaluation
frameworks to guide how to investigate the impact
of Connected Health technologies. To address this
gap, we formulate the following research question:
Which technology evaluation models can support
the evaluation of Connected Health solutions?
To explore this question, we undertook a
literature review with a particular emphasis on
information systems (IS) and healthcare IS (HIS)
evaluation literature.
3 IS & HIS EVALUATION
MODELS
The process of evaluation serves a number of
fundamental objectives. Within a healthcare context,
evaluating the impact of IS is important to
understand the dynamic nature of technology and its
ability to improve clinical performance, patient care,
and service operations (Meltsner, 2012). Therefore,
evaluation offers us the ability to learn from past and
present performance (Friedman and Wyatt, 1997)
with a view to improving process, care (Leveille et
al., 2012), economics (Dávalos et al., 2009; Van
Ooteghem et al., 2012) and healthcare satisfaction
for the future (Kuhn and Giuse, 2001; Van Bemmel
and Musen, 1997).
Identifying various methods of evaluation
throughout the IS literature enables us to build on
the current knowledge and identify techniques to
improve healthcare systems (Yusof et al., 2006)
which support the emergence and evidence-base of
Connected Health innovation. We build on the work
of O’Leary et al., (2015) in adopting a generic
approach to untangle the complexity of evaluating
Connected Health innovation.
There have been several well-cited evaluation
models across the IS and healthcare field which we
can examine with a view of developing a Connected
Health Evaluation Framework (CHEF). Various
evaluation approaches on IS were developed with
different outlooks including technical, sociological,
economic, human and organisational. A number of
frameworks also explicitly focus on HIS evaluation.
Our selection criteria were based on the search
for information system evaluation models which
adopts multiple perspectives of assessment. We
discovered that many of the models were too narrow
HEALTHINF 2016 - 9th International Conference on Health Informatics
18

Table 1: Summary of IS Evaluation Frameworks.
Framework Clinical Technical Economic Human Organisational Regulation
4Cs Model
CHEATS Model
TEAM
ITAM
IS Success Model
TAM
HOT-fit Model
Integrated Model
RATER Model
Search Engine
Success Model
in focus and only address a specific element of
information systems which would not be suitable for
the generic nature of Connected Health. We
summarise these perspectives as follows:
Clinical: medical practice, based on observation,
interaction and treatment of patients;
Technical: the application of hardware and
software devices to connect healthcare service
operations in a more efficient manner;
Economic: understanding the processes that
govern the production, distribution and
consumption of goods and services which impact
on healthcare;
Human: training, personnel attitudes,
ergonomics and regulations affecting
employment and patient experience in
healthcare. This can also examine the evolution
of social behaviour and development through the
influence of both internal (e.g. attitudes, emotion,
or health status) and external factors (e.g. service
availability or economics of care);
Organisational: the nature of the healthcare
organisation, its structure, culture and politics
affect an evaluation;
Regulation: a mechanism to sustain and focus
control which is often exercised by a public
agency over activities that are valued by the
healthcare community and its stakeholders.
We examine these key factors in a number of
HIS and IS evaluation models and summarise their
primary focus in Table 1.
Table 1 examines various factors which are
considered in evaluation ranging from clinical,
technical, economic, human, organisation and
regulation. This indicates that there is a lack of a
holistic evaluation approach on healthcare which
must be addressed in Connected Health to deliver
innovative and perhaps ‘disruptive’ solutions
(Christensen et al., 2000; Schwamm, 2014). There
have been some efforts to evaluate HIS including
clinical decision support systems.
3.1 HOT-fit Model
Yosof et al., (2006) proposed the Human,
Organization and Technology-fit (HOT-fit
framework) which was developed from a literature
review on HIS evaluation studies. A review of the
literature revealed that while specific instances of
the evaluation of healthcare technology exists
(Mathur et al., 2007; O’Neill et al., 2012), there is no
evidence of a generic evaluation model which can be
applied to Connected Health to provide a holistic
view of its potential impact.
3.2 4Cs Model
The 4Cs Evaluation Framework steers away from
the technical issues of evaluation and using a social
interactionist perspective, it examines how human,
organisational and social issues are important for
service design, development and deployment. The
4Cs framework examines issues associated with
communication, care, control, and context based on
medical informatics (Kaplan, 1997; Kaplan, 2001).
3.3 CHEATS Model
Another model which evaluates the use of ICT in
healthcare includes the CHEATS framework (Shaw,
Evaluating Multiple Perspectives of a Connected Health Ecosystem
19
2002). It evaluates healthcare through six core areas:
Clinical: focusing on issues such as quality of
care, diagnosis reliability, impact and continuity
of care, technology acceptance, practice changes
and cultural changes;
Human and Organisational: focusing on issues
such as the effects of change on the individual
and on the organisation;
Educational: focusing on issues such as
recruitment and retention of staff and training;
Administrative: focusing on issues such as
convenience, change and cost associated with
health system;
Technical and Social: focusing on issues such
as efficacy and effectiveness of new systems and
the appropriateness of technology, usability,
training and reliability of healthcare technology.
3.4 Team
Another model which evaluates HIS is the Total
Evaluation and Acceptance Methodology (TEAM).
This offers an approach based on systemic and
model theories (Grant et al., 2002) and identifies
three key IS evaluation dimensions in biomedicine:
Role: evaluates IS from the designer,
specialist user, end user and stakeholder
perspective;
Time: identifies four main phases which
provide relative stability of the IS;
Structure: distinguishes between strategic,
tactical or organisational and operational
levels.
3.5 IS Success Model
From an Information Systems (IS) perspective, there
are also several well cited evaluation frameworks
which we examined. For example, the IS Success
Model (DeLone and McLean, 1992; Delone and
McLean, 2003) examines the success of IS from a
number of different perspectives and classifies them
into six categories of success (DeLone and McLean,
2003). The model adopts a multidimensional
framework which measures independencies between
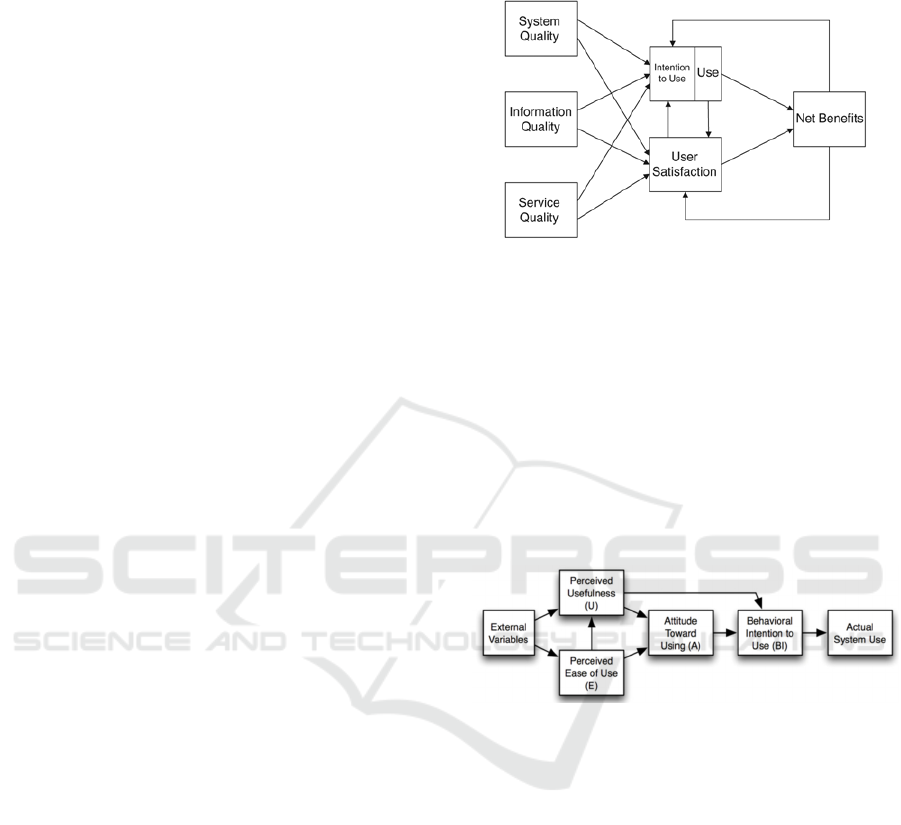
the various categories (Figure 1):
Information
System and service quality
Use (intention to)
User satisfaction
Net benefits
These dimensions suggest that there is a clear
relationship between the six categories and
influences the success of the IS (i.e. net benefits).
The net benefits influence user satisfaction and use
of the information system.
Figure 1: IS Success Model (DeLone and McLean, 2003).
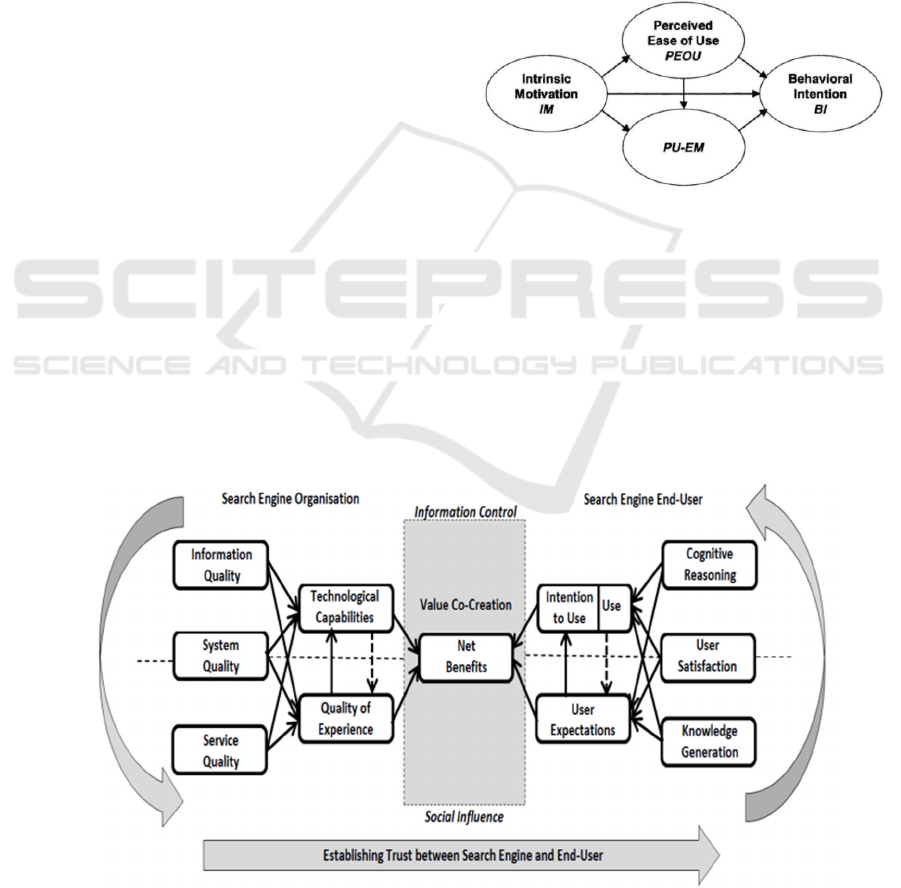
3.6 Tam
The Technology Acceptance Model (TAM)
examines how users accept the use of technology
though a number of important influential factors
(Davis, 1989). Among these factors are (see Figure
2):
The perceived usefulness (U) of the
technology;
The perceived ease-of use (E) of the
technology.
Figure 2: Technology Acceptance Model (Davis, 1989).
TAM suggests that these factors determine
people’s intention to use a technology. While TAM
provides an excellent approach to examining
people’s acceptance of technology, it is limited in
explanatory terms (Gregor, 2006) of technological
‘value’.
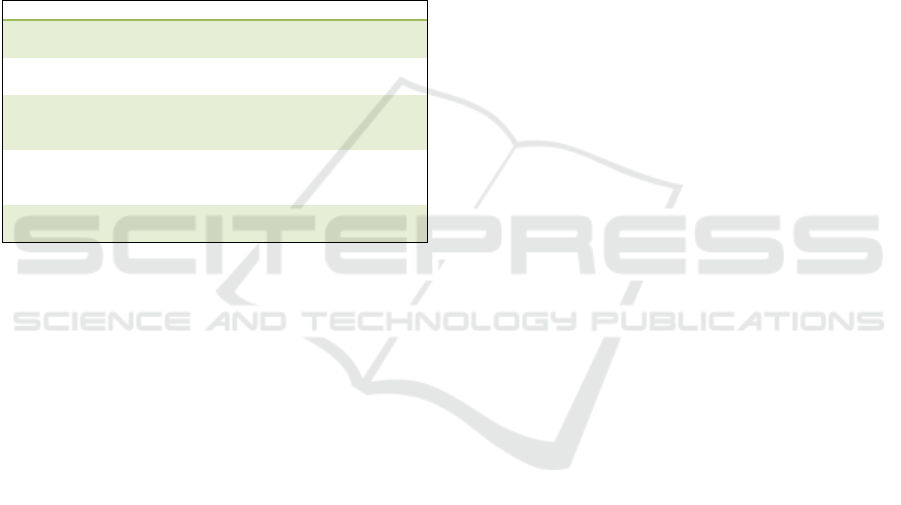
3.7 Search Engine Success Model
In a similar vein, Carroll (2014) extends the IS
Success Model to develop the Search Engine
Success Model and examines the complex task of
evaluating the impact of search engine technology
on users. The independencies between the
components build upon Delone and McLean IS
Success Model but include a more comprehensive
view of the value co-creation relationship between
the organisation and end-user. From a Connected
Health perspective, this model illustrates the cyclical
HEALTHINF 2016 - 9th International Conference on Health Informatics
20
nature of establishing trust to generate and sustain
net benefits. The model adopts a multidimensional
framework which measures independencies between
the various categories (Figure 3):
Information
System and service quality
Use (intention to)
Technological capabilities
Quality of experience
User expectation
User satisfaction
Cognitive reasoning
Knowledge generation
Net benefits through a co-creation relationship
3.8 ITAM
Adopting a similar outlook on technology
evaluation, Dixon (1999) presents a socio-technical
evaluation model which examines the behavioural
aspects of technology using the IT Adoption Model
(ITAM). ITAM provides a framework for using
implementation strategies and evaluation techniques
from an end-user’s perspective (i.e. fit for purpose,
user perceptions of innovation usefulness and ease
of use, and adoption and utilisation). Related
research also focuses on consumer health behaviours
and their adoption of medical technologies. For
example, Wilson and Lankton (2004) examines
consumer acceptance of HIS to support patients in
managing manage chronic disease.
3.9 Integrated Model
Wilson and Lankton (2004) integrated the use of
TAM to extend the model which became known as
the Integrated Model (Figure 4). Their Model
merges the perception of technology’s usefulness
(PU) with extrinsic motivation (EM) in a PU-EM
scale and perception of a technology’s ease of use
(PEOU) scales. The key factors of this model
evaluate healthcare technology by examining the:
Perception of a technology’s usefulness (PU);
Perception of a technology’s ease of use
(PEOU);
Behavioural intention (BI) to use the
technology;
Intrinsic motivation (IM);
Extrinsic motivation (EM) to determine BI.
Figure 3: Integrated Model (Wilson and Lankton, 2004).
The five dimensions identified using the
Integrated Model can also provide a useful lens to
understand the impact of technology in Connected
Health, particularly the influential factors on IT-
enabled innovation and the adoption of solutions.
Identifying gaps in health service sectors is
important to enhance the overall quality of the
service delivery and identify how Connected Health
solutions can address these gaps.
Figure 4: Search Engine Success Model (Carroll, 2014).
Evaluating Multiple Perspectives of a Connected Health Ecosystem
21
3.10 RATER Model
There are a number of methods which evaluate the
quality of services with a view of identifying areas
to prioritise service improvements. For example, the
RATER Model (Zeithaml et al., 1990) offers a
simplified version of the SERVQUAL model
(Parasuraman et al., 1988) using five key customer
service issues (Table 2). They focus on five
dimensions to analyse and improve service
offerings. The five key dimensions can also support
the development of a service plan to improve service
delivery and are particularly apt in Connected Health
solutions.
Table 2: Key Dimensions within the RATER Model.
Dimension Description
Reliability
Ability to provide dependable service,
consistently, accurately, and on-time.
Assurance
The competence of staff to apply their
expertise to inspire trust and confidence.
Tangibles
Physical appearance or public image of a
service, including offices, equipment,
employees, and the communication material.
Empathy
Relationship between employees and
customers and the ability to provide a caring
and personalised service.
Responsiveness
Willingness to provide a timely, high quality
service to meet customers needs.
3.11 Intervention Mapping
Other initiatives which may support the evaluation
of Connected Health solutions include the
Intervention Mapping Framework (IMF). The IMF
provides a systematic and rigorous approach that can
be used to develop and promote health programmes.
It achieves this through developing theory-based and
evidence-based health promotion initiatives. These
initiatives may be incorporated into a Connected
Health evaluation, particularly from a patient-
focused perspective.
3.12 Research Gap
From our literature review, we can conclude that
evaluating the value of HIS is a complex task. This
is also confirmed by a recent report on ‘The Value of
Health Information Technology: Filling the
Knowledge Gap’ (Rudin et al., 2014) which draws
similar conclusions in that the majority of evaluation
articles are limited. They state that evaluation
articles use “incomplete measures of value and fail
to report the important contextual and
implementation characteristics that would allow for
an adequate understanding of how the study results
were achieved”, and provide a conceptual
framework using three key principles for measuring
the value of healthcare IT as follows:
Value includes both costs and benefits;
Value accrues over time;
Value depends on which stakeholder’s
perspective is used.
These principles suggest that a core focus of an
evaluation strategy ought to focus on ‘value’ and
how this can be represented from various
stakeholders’ perspectives. Other models discussed
above referred to this as ‘net benefits’ or ‘value co-
creation’. In summary, while the frameworks
explored in this report evaluate various aspects of
HIS and IS they do not provide a holistic view of
healthcare technology and cannot be successfully
applied to support the board nature of Connected
Health.
With the aim of developing a more universally
adoptable framework for multiple perspectives of
Connected Health, we propose the Connected Health
Evaluation Framework (CHEF). The need for such
an approach was also highlighted by Rudin et al.,
(2014) who raise concerns regarding evaluation in
healthcare: “unfortunately, we have found that few
studies include both costs and benefits in their
definitions of value. Most studies look at only short-
term time horizons, which ignore many of the
downstream benefits of the HIT, and many studies
don’t even explicitly state to whom the value is
accruing.” We set out to address this gap using
CHEF.
4 CHEF
This section presents the Connected Health
Evaluation Framework (CHEF). The development of
CHEF (Figure 5) is influenced by both the strengths
of current HIS/IS models and the limitations of these
models which emerged from the literature review. In
addition, while economics and regulation often
shape innovation, both have been largely overlooked
in many of the evaluation models we identified.
‘Healthcare net benefits’ are presented at the core of
CHEF. CHEF is comprised of four main layers for
Connected Health, broadly addressing clinical,
business, users and systems with a view to determine
how these co-create value. Each of the categories
supports specific Connected Health operations
across all service lifecycle stages, ultimately
generating healthcare net benefits. For example:
Business Growth: as part of the overall
healthcare service strategy phase, this focuses on
HEALTHINF 2016 - 9th International Conference on Health Informatics
22

Figure 5: Connected Health Evaluation Framework (CHEF).
driving change and economics in healthcare and
organisational market share. Particular emphasis
on evaluation focuses on the cultural and strategy
change for introduction Connected Health
innovations. While introducing Connected Health
innovation, an economic evaluation should be
undertaken to examine the potential profits and
costs associated its implementation.
Healthcare Practice: as part of both the
healthcare service design and transition phases,
this focuses on health IT and innovation and how
it alters practice/clinical pathways (O’Leary et al.,
2014). From a technological perspective, an
evaluation is carried out on both the hardware and
software capability to deliver a Connected Health
solution. In addition, the innovativeness of
altering healthcare practice is evaluated from a
socio-technical and ethnography viewpoint. This
allows the examination of the impact of delivering
information in a new format and whether it
enhances the overall connectivity of healthcare
stakeholders.
End-user Perception: as part of both the
healthcare service transition and operations
phases, this focuses on safety and quality of
healthcare innovation for a user’s perspective (e.g.
a doctor, a patient or carer). This phase evaluates
the safety and quality of Connected Health
solutions. From a safety viewpoint, an evaluation
may be carried out on the usability and level of
empowerment a solution may provide in order to
provide a balance in empowerment and safety.
From a quality viewpoint, we can evaluate
whether Connected Health technologies have led
to improved healthcare decision-making and
enhanced usefulness of technological innovations.
Quality Management: as part of both the
healthcare service operations and continuous
service improvement phases, quality management
focuses on technical and regulation requirements
and conformity assessment. This phase can
evaluate the requirements of healthcare
stakeholders to generate awareness of Connected
Health innovation and to support users through
improved training programmes. In addition, an
evaluation may also assess the organisation’s
conformity with medical device regulations in
terms of technology classification and compliance.
This also informs how an organisation can realign
their service strategy – and the service lifecycle
continues through a continuous improvement
philosophy.
Evaluating Multiple Perspectives of a Connected Health Ecosystem
23
Within each of these subcategories, we will
identify key metrics (Rojas and Gagnon, 2008)
associated with the evaluation of Connected Health
solutions. As part of our future work, we will
identify operational key metrics for each category
and its components to support Connected Health
innovation. The outer layer of CHEF comprises of
various service lifecycle stages and highlights the
need to identify value points in each of the service
lifecycle phases.
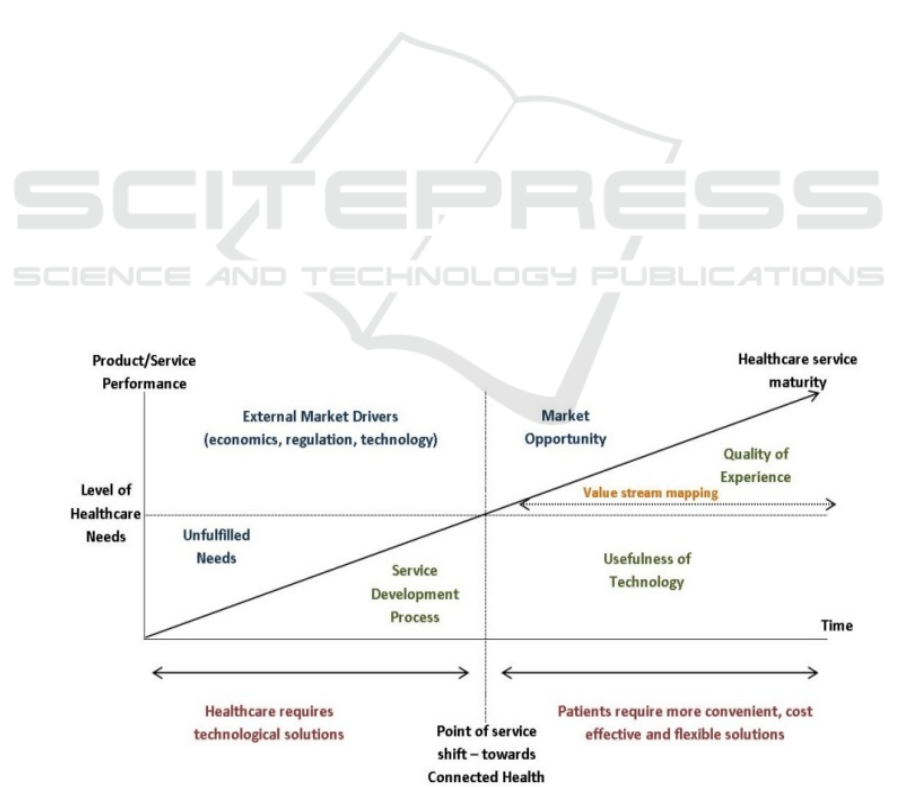
The service lifecycle phases play a critical role
in aligning the service development process and the
market opportunities (Figure 6). The Connected
Health environment addresses healthcare technology
requirements to enhance the level of healthcare
service offerings. Connected Health can potentially
address unfulfilled needs in healthcare as a result of
external forces and various demographic drivers.
Many of these drivers are also opening new market
opportunities which enable Connected Health
solutions to improve healthcare service maturity
through enhanced service performance. The value of
Connected Health solutions includes an improved
quality of experience and usefulness in technological
solutions to deliver healthcare.
While acknowledging that technology can
provide healthcare solutions, it is equally important
to question at each phase of the service lifecycle, for
example “what problem does information solve?”
(Postman, 1992) and “what is the problem to which
this technology is a solution?” (Postman, 1999).
Postman’s question applies equally well to the
Connected Health field as a basic evaluation
question. Building on this, it is critical that as a
starting point, and before we can successfully
identify value in Connected Health, the current
healthcare system is modelled, for example, actor
interaction, value stream mapping, resource
exchange, service bottlenecks, workflows,
organisational structures and mapping the healthcare
solutions market landscape.
CHEF offers an approach to guide the evaluation
process. Thus, the two key aspects as we move
forward in Connected Health evaluation can be
derived in:
Ensuring the systems, devices and services meet
the health and social needs of users through
evidence-based research;
Developing innovative patient-centred
technological solutions to empower people to
effectively manage their health and wellness in the
home and community (Delbanco et al. 2012).
In addition, from a Connected Health
perspective, evaluation must be conducted to assess
its impact across the broad spectrum of care
services. The scope of CHEF explicitly
acknowledges the broad scope and existence of
different stakeholders. CHEF will facilitate
evaluations through an assessment process designed
to provide:
A holistic view of a healthcare system;
Tailored analysis of healthcare service
lifecycle;
Performance metrics on service operations and
patient-focused analytics;
Scorecard and benchmark tools to assess
Figure 6: Connected Health Environment.
HEALTHINF 2016 - 9th International Conference on Health Informatics
24

healthcare technological integrations,
healthcare interventions and healthcare
providers.
These will also form part of our research strategy
in our quest to develop a CHEF and apply it to
various healthcare products and services and derive
core evaluation metrics. There is a clear correlation
between Connected Health functionality and
healthcare net benefits from multiple perspectives.
CHEF will be further validated through continued
industry engagement and Connected Health
technologies to accommodate the rapid growth of
healthcare IT solutions.
CHEF can also promote innovation by guiding
evaluation at all stages of the health IT product
lifecycle and encouraging organisations to consider
the complex socio-technical ecosystem in which
healthcare products are developed, implemented,
and used. Particular interests include the quality
systems in place to govern Connected Health data
management, access to clinical information,
stakeholder communication, knowledge
management and patient privacy. Regulations and
conformity assessment supports the technology
evaluation processes from a health and safety
perspective. We believe that CHEF will also support
organisation in examining potential risks posed by
Connected Health functionality and in comparing
them to the potential net benefits, for example,
developing a benefit-risk profile. In addition, by
meeting the regulatory evaluation of a medical
device, conformity assessment will evaluate whether
they present challenges to Connected Health
innovation. Combined, CHEF promotes the need to
incorporate Connected Health evaluation at various
stages using quality management principles, adopt
continuously revised standards and harness a
learning and continual improvement environment to
improve patient safety.
CHEF will enable organisations to identify
poorly designed healthcare solutions, assess
performance requirements, monitor human
interaction (end-user) and identify potential gaps
within a business strategy. In addition, CHEF offers
a first step towards employing evaluation to extend
the evidence-based foundation for Connected Health
through the assessment of best practice and by
identifying interventions and opportunities for
improvement based on the CHEF evaluation and
evidence gathered.
5 DISCUSSION & CONCLUSION
With significantly greater shifts in demographics
and longevity, the cost of healthcare will show a
corresponding increase. In an attempt to reduce
these growing costs, governments typically attempt
to reduce healthcare overheads, including staffing,
patient contact time, consultation and scheduling
various appointments. This can also create service
bottlenecks which jeopardises the quality and safety
of healthcare.
There is evidence that a paradigm shift to
empower people to take more control of their own
health is occurring. Technology innovation enables
and aligns with these healthcare shifts, providing
greater service efficiencies and effectiveness and
supporting the reduction of costs. Connected Health
presents an exciting approach towards redesigned
healthcare delivery. However, the success of
Connected Health will hinge on evaluation strategies
to determine the real value or benefits (healthcare,
quality of care, economics, etc.) associated with
technological integration in healthcare service
systems. This paper presents an overview of how
existing evaluation frameworks in e-health and
information systems can they influence Connected
Health evaluations.
Bridging these efforts, we propose the CHEF
which we will employ through industry engagement.
Throughout our evaluation research, we also
discovered that that concept of connectedness
through IT-enabled healthcare is a complex socio-
technical environment which is also impacted on
various geography, socio-economic status, and
technological competence – often influencing their
attitudes to Connected Health innovation.
Technology therefore plays a key role in fostering
healthcare relationships given healthcare
stakeholders a sense of being interconnected.
Through evaluation processes, if we can develop a
better understanding of the Connected Health
network structure, we can begin to further evaluate
the impact of IT innovation on a healthcare
ecosystem.
CHEF is a first step in offering a holistic view of
Connected Health and is a step towards an
evaluation of healthcare technological innovations.
As part of our future work, we will continue to
collaborate with industry and academic members
within ARCH - Applied Research for Connected
Health Technology Centre. Through our
multidisciplinary research team, we will extend this
work and validate CHEF with various healthcare
stakeholders and IT providers.
Evaluating Multiple Perspectives of a Connected Health Ecosystem
25

ACKNOWLEDGEMENTS
This work was supported, in part, by ARCH -
Applied Research for Connected Health Technology
Centre (www.arch.ie), an initiative jointly funded by
Enterprise Ireland and the IDA, SFI Lero Grant
(www.lero.ie) 13/RC/2094 and Science Foundation
Ireland (SFI) Industry Fellowship Grant Number
14/IF/2530.
REFERENCES
Carroll, N. (2014). In Search We Trust: Exploring How
Search Engines are Shaping Society. International
Journal of Knowledge Society Research (IJKSR),
5(1), 12-27.
Caulfield, B. M., and Donnelly, S. C. (2013). What is
Connected Health and why will it change your
practice?. QJM, hct114.
Christensen, C. M., Bohmer, R., and Kenagy, J. (2000).
Will disruptive innovations cure health care?. Harvard
business review, 78(5), 102-112.
Dansky, K.H., Palmer, L., Shea, D., Bowles, K.H. (2001).
“Cost Analysis of Telehomecare”. Telemedicine
Journal and e-Health. September, pp. 225-232.
Dávalos, M.E., French, M.T., Burdick, A.E., Simmons,
S.C. (2009). “Economic Evaluation of Telemedicine:
Review of the Literature and Research Guidelines for
Benefit–Cost Analysis”. Telemedicine and e-Health,
December, pp. 933-948.
Davis, F. D. (1989). Perceived usefulness, perceived ease
of use, and user acceptance of information technology.
MIS Quarterly, pp. 319-340.
Delbanco, T., Walker, J., Bell, S. K., Darer, J. D., Elmore,
J. G., Farag, N., Feldman, H.J., Mejilla, R., Ngo, L.,
Ralston, J.D., Ross, S.E. Trivedi, N., Vodicka, E.,
Leveille, S.G. (2012). Inviting patients to read their
doctors' notes: a quasi-experimental study and a look
ahead. Annals of internal medicine, 157(7), 461-470.
Delone, W. H. (2003). The DeLone and McLean model of
information systems success: a ten-year update.
Journal of management information systems, 19(4), 9-
30.
DeLone, W. H., and McLean, E. R. (1992). Information
systems success: the quest for the dependent variable.
Information systems research, 3(1), 60-95.
Department of Communications, Energy and Natural
Resources (2011). Knowledge Society Strategy:
Report on e-Health Developments in Ireland.
Retrieved on 02/02/2015 from Website:
http://tinyurl.com/lrs3aja.
Dixon, D. R. (1999). The behavioral side of information
technology. International journal of medical
informatics, 56(1), 117-123.
ECHAlliance (2014). Connected Health – White Paper.
Retrieved on 09/03/2015 from Website:
http://cht.oulu.fi/uploads/2/3/7/4/23746055/connected
_health.pdf.
Fineout-Overholt, E., Melnyk, B. M., and Schultz, A.
(2005). Transforming health care from the inside out:
advancing evidence-based practice in the 21st century.
Journal of Professional Nursing, 21(6), 335-344.
Friedman, C. P., Wyatt, J.C. (1997). Evaluation Methods
in Medical Informatics. New York: Springer-Verlag.
Grant, A., Plante, I., and Leblanc, F. (2002). The TEAM
methodology for the evaluation of information
systems in biomedicine. Computers in Biology and
Medicine, 32(3), 195-207.
Gregor, S. (2006). The nature of theory in information
systems. MIS Quarterly, 30(3), pp. 611-642.
Heathfield, H., Pitty, D., and Hanka, R. (1998). Evaluating
information technology in health care: barriers and
challenges. BMJ, 316(7149), 1959.
Hebert, M.A, and Korabek, B. (2004). “Stakeholder
Readiness for Telehomecare: Implications for
Implementation”. Telemedicine Journal and e-Health.
March, pp. 85-92.
Kaplan B. (1997). Addressing organizational issues into
the evaluation of medical systems. J Am Med Inform
Assoc.; 4(2): 94-101.
Kaplan, B. (2001). Evaluating informatics applications—
some alternative approaches: theory, social
interactionism, and call for methodological pluralism.
International journal of medical informatics, 64(1), 39-
56.
Kuhn, K. A., Giuse, D.A. (2001). "From Hospital
Information Systems to Health Information Systems -
Problems, Challenges, Perspective," Yearbook of
Medical Informatics, 63-76.
Leveille, S. G., Walker, J., Ralston, J. D., Ross, S. E.,
Elmore, J. G., and Delbanco, T. (2012). Evaluating the
impact of patients' online access to doctors' visit notes:
designing and executing the OpenNotes project. BMC
medical informatics and decision making, 12(1), 32.
Mathur, A., Kvedar, J.C. and Watson, A.J. (2007).
“Connected health: A new framework for evaluation
of communication technology use in care
improvement strategies for type 2 diabetes,” Current
Diabetes Reviews, vol. 3, no. 4, pp. 229–234.
Meltsner, M. (2012). A patient's view of OpenNotes.
Annals of internal medicine, 157(7), 523-524.
Misuraca, G., Codagnone, C., and Rossel, P. (2013). From
practice to theory and back to practice: Reflexivity in
measurement and evaluation for evidence-based policy
making in the information society. Government
Information Quarterly, 30, S68-S82.
O’Leary, P., Carroll, N., and Richardson, I. (2014). The
Practitioner's Perspective on Clinical Pathway Support
Systems. In Healthcare Informatics (ICHI), 2014 IEEE
International Conference on (pp. 194-201). IEEE.
O’Leary, P., Carroll, N., Clarke, P. and Richardson, I.
(2015). Untangling the Complexity of Connected
Health Evaluations, IEEE International Conference on
Healthcare Informatics 2015 (ICHI 2015) Dallas,
Texas, USA, October 21-23.
O’Neill, S.A., Nugent, C.D., Donnelly, M.P., McCullagh,
P., and McLaughlin, J. (2012). Evaluation of
HEALTHINF 2016 - 9th International Conference on Health Informatics
26

connected health technology,” Technology and Health
Care, vol. 20, no. 4, pp. 151–167.
Parasuraman, A., Zeithaml, V. A., and Berry, L. L. (1988).
Servqual. Journal of retailing, 64(1), 12-40.
Postman, N. (1992). Technopoly: The surrender of culture
to technology. New York: Vintage Press.
Postman, N. (1999). Building a Bridge to the 18th
Century: How the Past Can Improve Our Future. New
York: Alfred A. Knopf Publishers.
Richardson, I. (2015). Connected Health: People,
Technology and Processes, Lero-TR-2015-03, Lero
Technical Report Series, University of Limerick.
Rodrigues, R., Huber, M., and Lamura, G. (2012). Facts
and figures on healthy ageing and long-term care.
Itävalta: European Centre for Social and Welfare
policy and Research: Vienna.
Rojas, S. V., and Gagnon, M. P. (2008). A systematic
review of the key indicators for assessing
telehomecare cost-effectiveness. Telemedicine and e-
Health, 14(9), 896-904.
Rudin, R.S., Jones, S.S., Shekelle, P., Hillestad, R.J. and
Keeler, E.B. (2014). The Value of Health Information
Technology: Filling the Knowledge Gap. The
American Journal of Managed Care, Special Issue:
Health Information Technology, Vol. 20, No. SP 17.
Schwamm, L. H. (2014). Telehealth: Seven Strategies To
Successfully Implement Disruptive Technology And
Transform Health Care. Health Affairs, 33(2), 200-
206.
Shaw, N. T. (2002). ‘CHEATS’: a generic information
communication technology (ICT) evaluation
framework. Computers in biology and medicine,
32(3), 209-220.
Tuffaha, H. W., Gordon, L. G., and Scuffham, P. A.
(2014). Value of information analysis in healthcare: a
review of principles and applications. Journal of
medical economics, 17(6), 377-383.
Van Bemmel, J.H. and Musen, M.A. (1997). Handbook of
Medical Informatics. Springer-Verlag, Heidelberg.
Van Ooteghem, J., Ackaert, A., Verbrugge, S., Colle, D.,
Pickavet, M., and Demeester, P. (2012). Economic
viability of eCare solutions. In Electronic Healthcare
(pp. 159-166). Springer Berlin Heidelberg.
Wilson, E. V., and Lankton, N. K. (2004).
Interdisciplinary Research and Publication
Opportunites in Information Systems and Health Care.
The Communications of the Association for
Information Systems, 14(1), 51.
Yusof, M. M., Paul, R. J., and Stergioulas, L. K. (2006).
Towards a framework for health information systems
evaluation. In System Sciences, HICSS'06.
Proceedings of the 39th Annual Hawaii International
Conference on (Vol. 5, pp. 95a-95a). IEEE.
Zeithaml, V. A., Parasuraman, A., and Berry, L. L. (1990).
Delivering quality service: Balancing customer
perceptions and expectations. Simon and ssSchuster.
Evaluating Multiple Perspectives of a Connected Health Ecosystem
27
