
Differences in Use of a Exercise-based Tele-rehabilitation Service
Delivered as Substitute of or Supplement to Conventional Care
S. M. Jansen-Kosterink, M. H. A. Huis in ‘t Veld
Roessingh Research and Development, Telemedicine group, Roessinghsbleekweg 33b, Enschede, The Nederlands
D. Wever
Roessingh Centre of Rehabilitation, Roessinghsbleekweg 33, Enschede, The Netherlands
H. J. Hermens, M. M. R. Vollenbroek-Hutten
Roessingh Research and Development,Telemedicine group, Roessinghsbleekweg 33b, Enschede, The Nederlands
University of Twente, Faculty of Electrical Engineering, Mathematics and computer Science
Telemedicine group, Enschede, The Netherlands
Keywords: Tele-rehabilitation, Service Configuration, Compliance, Use, Usability.
Abstract: The aim of this paper is to explore the use of an exercise-based tele-rehabilitation service in patients with
mild or severe chronic obstructive pulmonary disorder (COPD). The service is delivered to the patients in
two ways: as substitute of (a part of) their pulmonary rehabilitation or as supplement to their pulmonary
rehabilitation. Given their reduced amount of conventional pulmonary rehabilitation, it is likely to assume
that the use of the service is higher in the substitute group compared to the supplement group. Use is
parameterized as the time between log-in and log-out time of patients interacting with the tele-rehabilitation
service for each week. Next to this the number of weeks patients used the service to exercise as well as the
average frequency of use per week and average duration of use per week were determined. Analyses were
performed on a group and individual level. Results showed that patients of the substitute group (n=29) used
the tele-rehabilitation service slightly more than the patients (n=15) of the supplement group, but these
differences were not significant.
1 INTRODUCTION
It is know that compliance, defined as the extent to
which a patient’s behaviour coincides with the
healthcare professional advice (Sackett & Haynes,
1976) to exercise treatment, has a positive effect on
clinical outcomes (Cramer, Benedict, Muszbek,
Keskinaslan, & Khan, 2008). To specify patient’s
compliance with a tele-rehabilitation service it is
important to know if patients used the tele-
rehabilitation for a sufficient amount of time
(frequency and duration). The use of a tele-
rehabilitation service by patients is easily to monitor,
by investigating the time between log-in and log-out.
The use of exercise-based tele-rehabilitation is
investigated in various papers. Van den Berg et al.
(van den Berg et al., 2006; van den Berg et al., 2007)
showed that for a home-based physical activity
intervention for patients with rheumatoid arthritis,
the number of patients who logged on to the website
declines during treatment. However, no information
is given about the duration of use and whether
patients used the website for the same amount of
time during treatment despite of the decline of
frequency of use. In addition Huis in ’t Veld et al.
(Huis in 't Veld et al., 2010) who examined the use
of a tele-treatment application for chronic pain
patients, showed a decline in use over time. They
used the average time the service was used, as
measure for use. In the first week the average use
was 14.3 hours and this declined to 9.5 hours in the
final week.
44
Wever D., Vollenbroek M., Jansen-Kosterink S., Hermens H. and Huis in ’t Veld R. (2012).
Differences in Use of a Exercise-based Tele-rehabilitation Service Delivered as Substitute of or Supplement to Conventional Care.
In Proceedings of the Sixth International Symposium on e-Health Services and Technologies and the Third International Conference on Green IT
Solutions, pages 44-51
DOI: 10.5220/0004473900440051
Copyright
c
SciTePress

In both studies the tele-rehabilitation service is
delivered to the patients as an autonomous
treatment. Is the decline in use for this service
configuration a pattern or a coincidence? And is this
decline in use also shown in tele-rehabilitation
service once integrated as a partially substitute of or
supplement to conventional care? Information about
the use of the tele-rehabilitation services is important
and should be addressed properly since it could
influence the results found for clinical effectiveness.
To the best of our knowledge the use of a tele-
rehabilitation service for the various service
configurations, i.e. as substitute of or as supplement
to conventional care has not been investigated yet.
However, information about differences in use for
different service configurations could provide
valuable knowledge on how to optimally implement
the service in conventional care.
In this paper the use of two different service
configurations of an exercise-based tele-
rehabilitation service will be investigated. This
service, designed within the CLEAR (= Clinical
Leading Environment for the Assessment of
Rehabilitation protocols in home care) project
(http://www.habiliseurope.eu), is implemented in the
pulmonary rehabilitation of patients with
mild/severe or severe chronic obstructive pulmonary
disorder (COPD). The service is delivered to the
patients in two ways: [1] as a substitute (of a part) of
conventional rehabilitation for patients with
mild/severe COPD. After an introduction period of
four weeks, the service substitutes one of the three
treatment days per week (group substitute) for ten
weeks. Or [2] as supplement to conventional
rehabilitation care in patients with severe COPD.
After an introduction period of four weeks, the
service was a supplement of the two treatment days
per week (group supplement) for ten weeks.
It is our empirical hypothesis that patients are
more willing to rehabilitate at home using the tele-
rehabilitation services when the service is delivered
to them as substitute of the pulmonary rehabilitation
compared to when the service is delivered
supplementary to their conventional pulmonary
rehabilitation. For the first service configuration, we
think that patients will use the tele-rehabilitation
service for a sufficient amount of hours to deal with
the substituted hours. For the second service
configuration, we think that the service is maybe
considered to be too much for patients next to their
already intensive pulmonary rehabilitation program.
The aim of this paper is to explore the use
(frequency and duration) of an exercise-based tele-
rehabilitation service in patients suffering from
pulmonary disease and to explore the difference
between the two service configurations (substitute or
supplement).
2 METHODS
Subjects were recruited between September 2010
and December 2011, by rehabilitation centre Het
Roessingh, Enschede, the Netherlands. Patients
directed, by their rehabilitation physician, to the
outpatient pulmonary rehabilitation for COPD
patients were asked to use the exercise tele-
rehabilitation service during their three months of
rehabilitation. Subjects with COPD were included if
they had sufficient understanding of the Dutch
language and were aged above 18 years.
The study was approved by the appropriate
ethics committee. All participants gave their
informed consent prior to participation.
2.1 Exercise Tele-rehabilitation Service
The exercise tele-rehabilitation service is facilitated
by a notebook with webcam, with newly developed
software giving access to a database of exercise
videos and a teleconference service to facilitate
contact between the patient and healthcare
professional. With this new service the healthcare
professional can compose a tailored exercise
program for his patient. The patient can carry out the
program on a self-scheduled time at home. Every
week the patient records an exercise with the
webcam and the recorded exercise will be assessed
by the healthcare professional. Patient and
healthcare professional can contact each other by
teleconference to discuss the rehabilitation progress.
The healthcare professional can schedule, add and
delete exercises in the exercise program of the
patient during the rehabilitation. The exercise tele-
rehabilitation service enables patients to exercise at
home at moments preferred by patients, which fits in
the current trend of self management of patients
(Kennedy, Rogers, & Bower, 2007).
During the instruction period, four weeks, all
subjects received an extended training on how to use
the exercise tele-rehabilitation service.
The demographic characteristics of the two
groups will be measured by means of a
questionnaire asking for age, gender, height, weight,
education level and the availability of a computer
with internet access. In addition, symptoms
(shortness of breath) prior to participation are
measured by means of VAS scales (Gift, 1989).
Differences in Use of a Exercise-based Tele-rehabilitation Service Delivered as Substitute of or Supplement to
Conventional Care
45

Figure 1: The exercise tele-rehabilitation service (1).
Figure 2: The exercise tele-rehabilitation service (2).
Patients are asked to rate their experienced level of
shortness of breath during the past week. The VAS
consists of a 10 cm horizontal line with ‘no
discomfort at al’ on the left and ‘as much discomfort
as possible’ on the right extremity of the line.
Psychometric properties have proven to be
sufficient.
2.2 Measurements
Use of the Service: Frequency and Duration
The use of the service was determined by various
parameters:
• The time between log-in and log-out of each
single session, this is registered by the service
automatically. Interval smaller than two minutes
were excluded, because the average duration of
an exercise video was two minutes and in
smaller intervals patients were not able to
exercise. The intervals larger than two hours
were also excluded, because it is unlikely that
patients will exercise longer than two hours in
one session. It was assumed that in these cases
patients forgot to log-out.
• The number of weeks the patients used the
service during their three months period
conventional rehabilitation program.
• The average frequency and duration of use per
week (in minutes).
Usability
It is likely to assume that the actual use of the tele-
rehabilitation service is influenced by the perceived
usability of the service. Differences in perceived
usability, between the two groups, might cause
differences in use irrespective of the type of service
configuration. For this reason we investigate the
perceived usability of the exercise-based tele-
rehabilitation service. All patients are asked to
complete the System Usability Scale (SUS) (Brooke,
1995) after their pulmonary rehabilitation. This
questionnaire includes 10 items which provide a
global view of subjective assessment of service’s
usability. Each item was rated on a five-point scale
form one (disagree totally) to five (agree totally).
The items score were calculated to give an overall
score ranging from 10 to 100 points. The SUS has
been shown by the author to be a robust and reliable
evaluation tool, but its psychometric properties are
still under investigation. There is no validated Dutch
version of the SUS. For this study the SUS is
translated to Dutch.
2.3 Statistical Analyses
Analyses were performed using standard software
(SPSS version 17). The normality of variables was
evaluated by the Kolmogorov-Smirnov test.
Descriptive statistics (means and SD) were
calculated for all socio-demographic variables,
shortness of breath and SUS score.
Group Level
Differences in frequency and duration of use of the
tele-rehabilitation service between groups were
investigated by means of an independent t-test or
Chi-square test in case of percentage. To investigate
the use (duration and frequency) of the service per
week, for the two groups, mixed-model analysis for
repeated measures will be used. Treatment week was
used as a within-subjects factor and type of service
delivery as a between-subject factor. Post hoc
comparisons were made when required and Sidak
adjustments were used to correct for multiple test.
EHST/ICGREEN 2012
46
Individual Level
To investigate difference in use of the service
between the groups on an individual level the
parameters number of weeks, frequency and
duration are categorized. Based on this
categorization the percentages of patients in the
various categories were assessed.
The categories for number of weeks used during
treatment are: often (more than 8 weeks) regularly
(between 7 and 4 week) and sometimes (less than 3
weeks). The categories for average frequency of use
per week are: often (more than 1.5 times a week),
regularly (between 1.4-1 time(s) a week) and
sporadic (less than once a week). The categories for
average duration of use per week are: long-term
(more than 60 minutes a week), regularly (between
30-59 minutes a week), sometimes (between 10-29
minutes a week) and short-term (less than 10
minutes a week). These categories are arbitrary
chosen and discussed with the health-care
professionals. Group differences in category
distribution are assessed by Chi-square testing.
3 RESULTS
In total, 85 COPD patients are informed about tele-
rehabilitation service and 58 patients (68%) gave
written informed consent to participate. Patients
were instructed how to work with the tele-
rehabilitation service. After this instruction period of
four weeks, 54 patients started to use the tele-
rehabilitation service as substitute of (group
substitute, n=20) or as supplement of (group
supplement, n=34) their rehabilitation program. In
the time period between the start to use the tele-
rehabilitation service and the end of the
rehabilitation program 10 patients (19%) dropped
out because of technical problems with the
equipment or personal circumstances, such as lack
of time or motivation. Thus, 44 patients used the
tele-rehabilitation service during the full length (10
weeks) of their rehabilitation program.
Of the 44 patients, 15 patients suffered from
severe COPD and used the tele-rehabilitation as
supplement of their rehabilitation program. Twenty-
nine patients suffered from mild/severe COPD and
used the tele-rehabilitation as substitute of their
rehabilitation program. The demographic
characteristic, shortness of breath and SUS score of
the two groups (group substitute and group
supplement) are shown in Table 1. Patients of group
substitute are significant younger (p=0.045) than the
patients of group supplement. Beyond, there are no
significant differences between the two groups.
Patients in both groups rated the usability of the
exercise tele-rehabilitation service as acceptable
with a SUS score of 70. For a product with a SUS
score in the 60s and 70s, although promising, but do
not guarantee high acceptability of the product in the
field (Brooke, 1995). On usability there are also no
differences between the two groups.
Use of the Tele-rehabilitation Service
In total, 293 interval blocks (time between log-in
and log-out time) were available on the server of the
tele-rehabilitation service. Fourteen (5%) of the
interval blocks were excluded, 11 blocks were
smaller than two minutes and three blocks were
larger than two hours.
Table 1: Demographic characteristic, shortness of breath and SUS score of the two groups.
Group substitute Group supplement p-value
Number 29 15
Pathology mild/severe COPD severe COPD
Age 55 years (SD 11) 62 years(SD 9) p=0.045
Height 177 cm (SD 11) 172 cm (SD 10) p=0.131
Weight 87 kg (SD 19) 82 kg (SD 26) p=0.482
Gender
Male: 66%
Female: 34%
Male: 47%
Female: 53%
p=0.228
Education
- primary
- secondary
- higher
3%
69%
28%
7%
79%
14%
p=0.517
PC with internet available at home Yes: 97% Yes: 80% p=0.107
Shortness of breath last week (VAS) 5.3 cm (SD 1.9) 6.1 cm (SD 2.0) p=0.224
SUS score post-test 70 (SD 17) 70 (SD 20) p=0.985
Differences in Use of a Exercise-based Tele-rehabilitation Service Delivered as Substitute of or Supplement to
Conventional Care
47
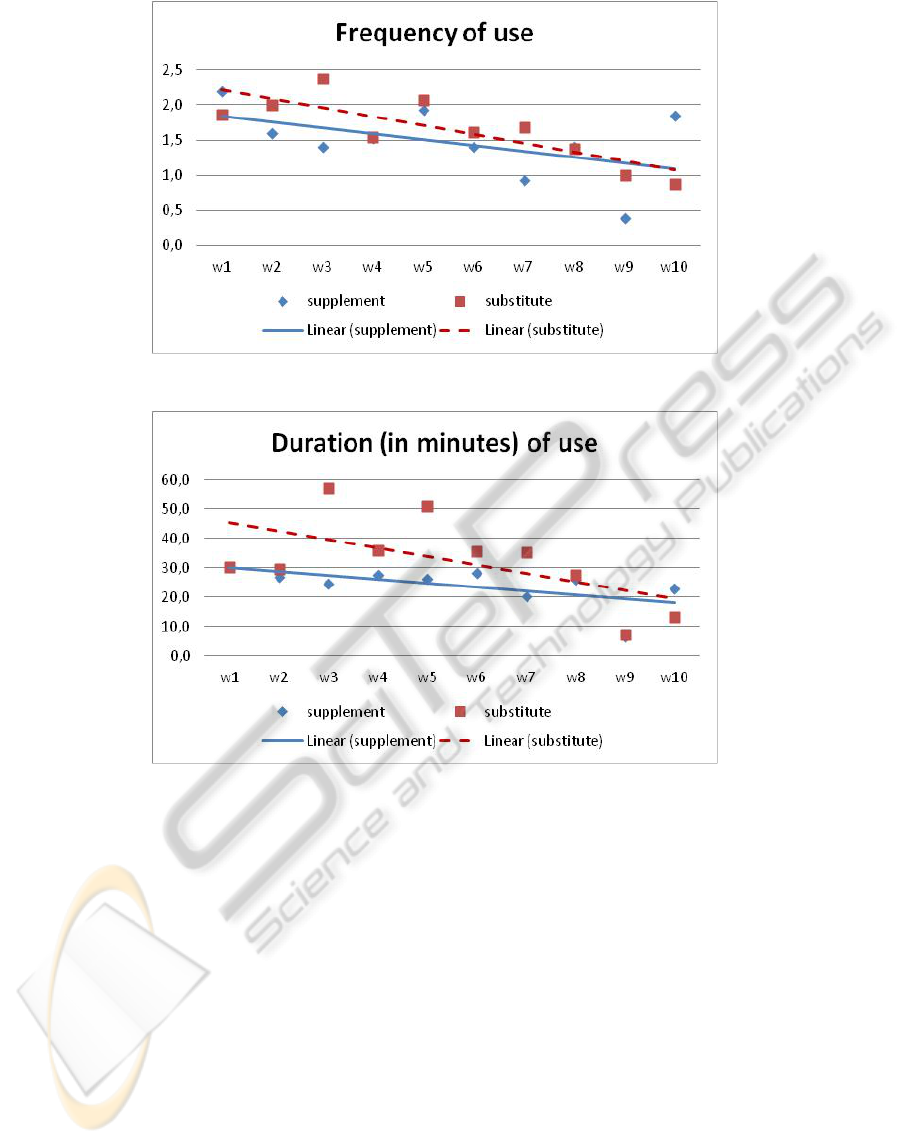
Figure 3: Frequency of use of the tele-rehabilitation service during the treatment weeks.
Figure 4: Duration of use of the tele-rehabilitation service during the treatment weeks.
Group Level Analyses
Patients of group substitute used the service average
6.6 weeks (SD2.4) out of the maximum of 10 weeks.
The average frequency of use is 1.7 times a week
(SD1.1) with an average duration of 33 minutes per
week (SD22). Patients of group supplement used the
service average 6.2 weeks (SD2.6) with an average
frequency of 1.4 times a week (SD1.1) and with an
average duration of 24 minutes per week (SD16). In
line with our hypothesis the average use of the tele-
rehabilitation service of the group substitute is
higher than the use of the tele-rehabilitation service
of the group supplement. However this difference
failed to reach significance (p≥0.155).
Figure 3 shows the average frequency of use
during the treatment weeks of the two groups over
the treatment weeks. The average frequency of the
use of the service declines in both groups. The
frequency of use declines for group substitute from
1.9 times a week for the first week to 0.9 times a
week for the final week of treatment. The frequency
of use declines for group supplement from 2.2 times
a week for the first week to 1.9 times a week for the
final week of treatment, notice the frequency of use
in the pre final treatment week was only 0.4 times a
week.
Mixed-model analysis for repeated measures
showed that frequency of use declines significant
over time (p=0.002), without additional effects for
service configurations (substitute or supplement)
(0.424).
Figure 4 shows the average duration of use
during the treatment weeks of the two groups. The
average duration of the use of the service declines
during treatment for both groups. The duration of
use declines for group substitute from 30 minutes a
week for the first week to 13 minutes times a week
for the final week of treatment. The duration of use
EHST/ICGREEN 2012
48
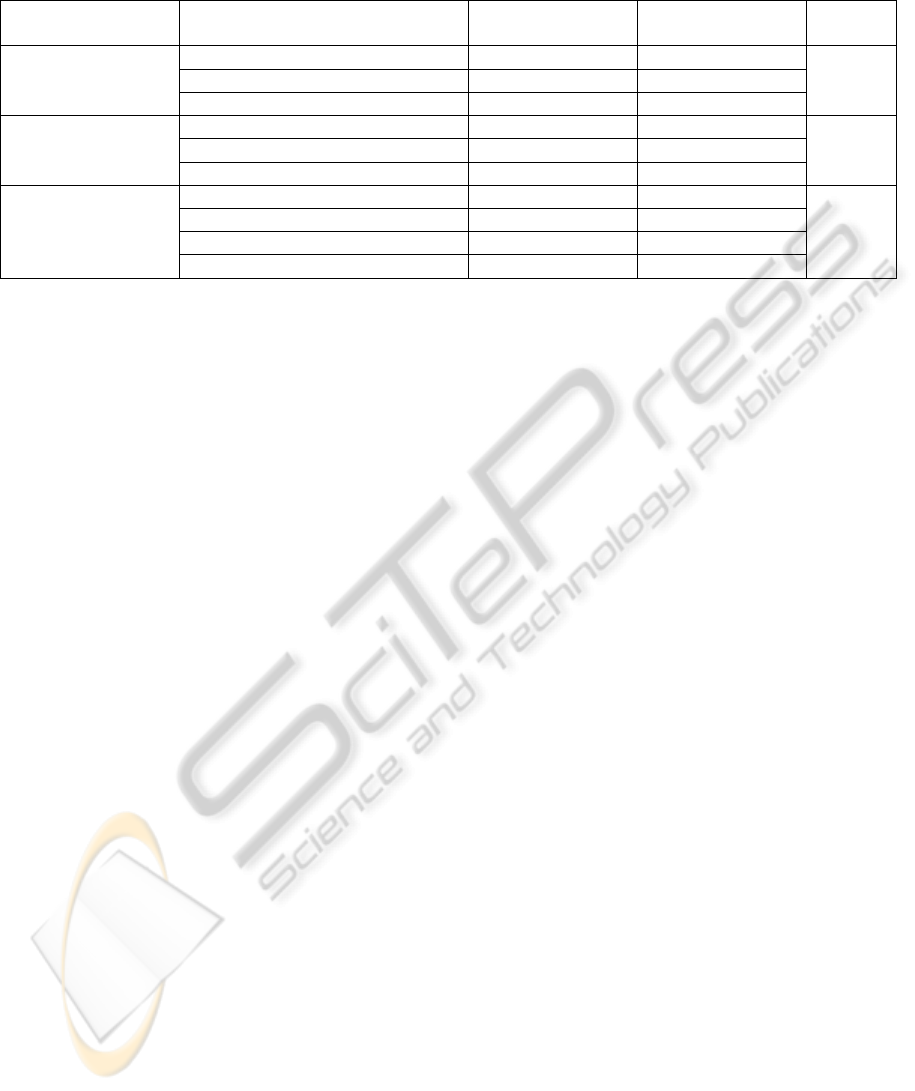
Table 2: Use of the tele-rehabilitation service in total number of days, average frequency per week and average duration per
week in percentages of patients.
Group substitute
n=29
Group supplement
n=15
p-value
Number of weeks of
use during treatment
period
Often 48% 47%
p=0.957
Regularly 42% 40%
Sometimes 10% 13%
Average frequency
per week
Often 24% 33%
p=0.382
Regularly 55% 33%
Sporadic 21% 33%
Average duration per
week
Long-term 7% 0%
p=0.703
Regularly 45% 40%
Sometimes 34% 40%
Short-term 14% 20%
declines for group supplement from 30 minutes a
week for the first week to 23 minutes a week for the
final week of treatment, notice the duration of use in
the pre final treatment week was only 7 minutes a
week.
Mixed-model analysis for repeated measures
showed that duration of use declines significant over
time (p=0.001), without additional effects for service
configurations (p=0.273).
Individual Level Analyses
Table 2 shows that approximately 50% of the
patients used the tele-rehabilitation service eight or
more weeks during their treatment period of three
months. 40% of the patients used the tele-
rehabilitation service four to seven weeks during
their treatment period. Only a small amount of
patients (10%) seem to have used the tele-
rehabilitation sporadically, i.e. less than three week
during their treatment period of three months.
About one-third of the patients (24-33%) used the
tele-rehabilitation service more than 1.5 times a
week; 33-55% of the patients used the tele-
rehabilitation service between 1.4 and 1 time(s) a
week; and 21-33% of the patients used the tele-
rehabilitation service less than 1 time a week.
Only 7% of the patients of group substitute used
the tele-rehabilitation service more than 60 minutes
per week. None of the patients of the group
supplement used the tele-rehabilitation service for
this amount of time. Most patients (40-45%) used
the tele-rehabilitation service between 30-59 minutes
per week. 34-40% of the patients used the used the
tele-rehabilitation service between 29-10 minutes
per week and 14-20% of the patients used the tele-
rehabilitation service less than 10 minutes per week.
However, the differences between the two groups
could not be supported by statistical analysis
(p≥0.382).
4 CONCLUSIONS
The aim of the current paper was to explore use
(frequency and duration) of an exercise-based tele-
rehabilitation service in patients suffering from
pulmonary disease and to explore the difference
between the two service configurations (substitute or
supplement). Almost 50% of all patients (both
groups) used the tele-rehabilitation service during
most weeks of their rehabilitation program, with a
frequency of at least once a week and an average
duration of more than 30 minutes on a basis of
voluntariness of use.
In line with our hypothesis, the patients where
the tele-rehabilitation service was delivered as
substitute of their pulmonary rehabilitation,
substitute group (n=29), used the tele-rehabilitation
service slightly more than the patients of the
supplement group (n=15). The difference between
the two groups is small, on average frequency per
week the delta score between the groups is 0.3 and
on duration this delta score is 9 minutes per week
and failed to reach significance. Furthermore, it is
beyond our expectations to think that these small
differences will be addressed as clinically relevant
by health-care professional either.
A decline in use, frequency and duration of use
per week, is observed in the results of the current
study. The decline of use of our tele-rehabilitation
service can be clarified in two ways. A first
clarification is the possibility that patients’
motivation to use the tele-rehabilitation service
declines. For instance after a couple of weeks
patients are not motivated the use the service and
Differences in Use of a Exercise-based Tele-rehabilitation Service Delivered as Substitute of or Supplement to
Conventional Care
49

reduce the amount of use or do not use the service
anymore. A second clarification is the possibility
that the patients’ need to use the tele-rehabilitation
service declines. After a couple of weeks using the
tele-rehabilitation service patients are aware of the
various exercises and do not need the exercise
videos to perform those exercises. In other words,
thanks to the service patients have become very well
capable of performing their exercises independently
and no longer have to rely on the service. There are
only a small number of papers addressing the use of
exercise-based tele-rehabilitation service. As
described in the introduction of the current paper,
the results of these papers show also a decline in use
(Huis in 't Veld, et al., 2010; van den Berg, et al.,
2006; van den Berg, et al., 2007).
In the current study the use of the service by the
patients was based on voluntariness of use. Patients
were not asked by their healthcare professionals to
use the tele-rehabilitation for a certain amount of
time. Following the Unified Theory of Acceptance
and Use of Technology (UTUAT) (Venkatesh,
Morris, Davis, & Davis, 2003), voluntariness of use
is a key moderator to the determinant social
influence and influences the behavioural intention of
patients to use a tele-rehabilitation service.
Non-mandatory use could be an explanation of
finding no significant differences in the use of the
tele-rehabilitation service between the two service
configurations. Replacing one treatment day (three
hours) of the pulmonary rehabilitation by the tele-
rehabilitation service does not motivate patients to
exercise for the same amount of time per week. So,
patients need an extra motivation, like minimum use
thresholds imposed by the healthcare professional, to
use the tele-rehabilitation service for a sufficient
amount of time.
These thresholds for minimum use should be
determined based on the empirical knowledge of
healthcare professionals or based on the relation
between use and clinical outcome.
Concerning the patient groups in this paper, the
two groups significantly differed on age. Patients of
group supplement were proximally seven years older
than the patients of group substitute. It is unknown if
in the current study age influenced the use of the
tele-rehabilitation service. Despite of this age
differences it can be stated that both patient groups
belong to the same generation 55 to 65 years. Based
on UTUAT (Venkatesh, et al., 2003), age is one of
the mediators that influence the use intention and
actual use of the tele-rehabilitation.
In addition, the two groups also differ in severity
of pathology; mild/severe versus severe COPD.
Prior to use of the service the shortness of breath
score of group supplement are slightly higher than
the score of group substitute. However this
difference did not reach significance
Other limitations of the current paper were the
relatively small sample size (n=43) and the
imbalance in groups size (n=29 vs. n=15) of the two
groups.
Given the results of the current paper clinical
implications can be made. First, healthcare
professionals should be aware of the fact that
different configurations of the same tele-
rehabilitation service do not result in different
patterns of use. Second, the amount of use of a tele-
rehabilitation service can explain possible
disappointing clinical outcome of tele-rehabilitation
services. Third, to find the cause, decline of use
should be addressed between healthcare professional
and patient, to result in optimization of the tele-
rehabilitation service.
This paper focused on the use of the tele-
rehabilitation service but for a future paper it is
recommendable to investigate the relation between
use of this tele-rehabilitation service and the clinical
outcome.
In conclusion, the use (frequency and duration)
of the exercise-based tele-rehabilitation service
declines during treatment. In contrast to our
expectations, there is no difference in use between
two different configurations of the same tele-
rehabilitation service in patients suffering from
pulmonary diseases.
ACKNOWLEDGEMENTS
This work was undertaken with financial support
from the European commission (ICT-PSP CLEAR
224985).
REFERENCES
Brooke, J. (1995). SUS - a quick and dirty usability scale.
In P. W. Jordan, B. Thoma & B. A. Weerdmeester
(Eds.), Usability Evaluation in Industry (pp. 189-194).
Lodon: Taylor & Francis.
Cramer, J. A., Benedict, A., Muszbek, N., Keskinaslan,
A., & Khan, Z. M. (2008). The significance of
compliance and persistence in the treatment of
diabetes, hypertension and dyslipidaemia: a review. Int
J Clin Pract, 62(1), 76-87.
Gift, A. (1989). Visual Analogue Scales: Measurement of
subjective phenomena. Nurs Res, 38, 286-288.
EHST/ICGREEN 2012
50

Huis in 't Veld, R. M., Kosterink, S. M., Barbe, T.,
Lindegard, A., Marecek, T., & Vollenbroek-Hutten,
M. M. (2010). Relation between patient satisfaction,
compliance and the clinical benefit of a teletreatment
application for chronic pain. J Telemed Telecare,
16(6), 322-328.
Kennedy, A., Rogers, A., & Bower, P. (2007). Support for
self care for patients with chronic disease. BMJ,
335(7627), 968-970.
Sackett, D., & Haynes, R. (1976). Compliance with
therapeutic regimens. Baltimore: Johns Hopkins Univ
Pr.
van den Berg, M. H., Ronday, H. K., Peeters, A. J., le
Cessie, S., van der Giesen, F. J., Breedveld, F. C., et
al. (2006). Using internet technology to deliver a
home-based physical activity intervention for patients
with rheumatoid arthritis: A randomized controlled
trial. Arthritis Rheum, 55(6), 935-945.
van den Berg, M. H., Ronday, H. K., Peeters, A. J., Voogt-
van der Harst, E. M., Munneke, M., Breedveld, F. C.,
et al. (2007). Engagement and satisfaction with an
Internet-based physical activity intervention in patients
with rheumatoid arthritis. Rheumatology (Oxford),
46(3), 545-552.
Venkatesh, V., Morris, M. G., Davis, G. B., & Davis, F. B.
(2003). User acceptance of information technology:
Toward a unified view MIS Quarterly, 27(3), 425-478.
Differences in Use of a Exercise-based Tele-rehabilitation Service Delivered as Substitute of or Supplement to
Conventional Care
51
