
A Mobile System for Treatment of Depression
Pepijn van de Ven
1
, Mário Ricardo Henriques
2
, Mark Hoogendoorn
3
, Michel Klein
3
,
Elaine McGovern
1
, John Nelson
1
, Hugo Silva
4
and Eric Tousset
5
1
University of Limerick, Limerick, Ireland
2
INESCP, Porto, Portugal
3
VU University, Amsterdam, The Netherlands
4
PLUX, Lisbon, Portugal
5
AARDEX, Liège, Belgium
Abstract. This paper presents a mobile treatment system developed as part of
the FP7 ICT4Depression project. The project targets the efficient treatment of
minor and major depression. To this end, treatments that have traditionally been
administered via relatively simple web-based interfaces, have been translated
for use on a smart phone. The delivery of the treatments is supported by an evi-
dence-based approach to patient progression and treatment adherence monitor-
ing. The mobile system consists of a graphical user interface, biomedical sen-
sors to measure the patient’s affective state, a medication adherence system, an
activity monitor and a server based reasoning system to combine the various
sensor data streams and obtain abstracted information relating to patient status
and progression, thereby allowing for appropriate feedback and advice for both
patient and medical staff.
1 Introduction
In recent years depression has received significant attention as a disorder with a far-
fetching impact on individuals and society as a whole. Studies show that in 2003 the
occurrence of major depressive disorder ranged from 3% (in Japan) to 16.9% in the
US with most countries showing a prevalence of 8% to 12% [1]. The burden of de-
pression is on the rise and by the year 2030, depression is expected to have the highest
disease burden in high income countries. There thus is a real need for effective treat-
ment of depression within the cost constraints of health services.
Treatments have already been adapted for online use to allow for more cost effec-
tive treatment and such systems have been shown to be of value [2]. The aim of the
ICT4Depression project is to take this approach a step further and provide various
treatment modules not only on a personal computer, but also on a mobile phone. The
advantages of this approach are that users can be provided with continuous treatment,
are free to decide when to interact with the system, can be monitored throughout the
day and can effectively include and integrate day-to-day duties and habits in their
customized treatment. Of particular interest in this regard is the recent insight that the
van de Ven P., Henriques M., Hoogendoorn M., Klein M., McGovern E., Nelson J., Silva H. and Tousset E..
A Mobile System for Treatment of Depression.
DOI: 10.5220/0003891700470058
In Proceedings of the 2nd International Workshop on Computing Paradigms for Mental Health (MindCare-2012), pages 47-58
ISBN: 978-989-8425-92-8
Copyright
c
2012 SCITEPRESS (Science and Technology Publications, Lda.)
inclusion of user specific data in the form of ecological momentary assessments
(EMA) is an important goal for future mobile treatment systems [3].
This paper describes the architecture and various sub systems comprising the mo-
bile system used for treatment of depression in the ICT4Depression project.
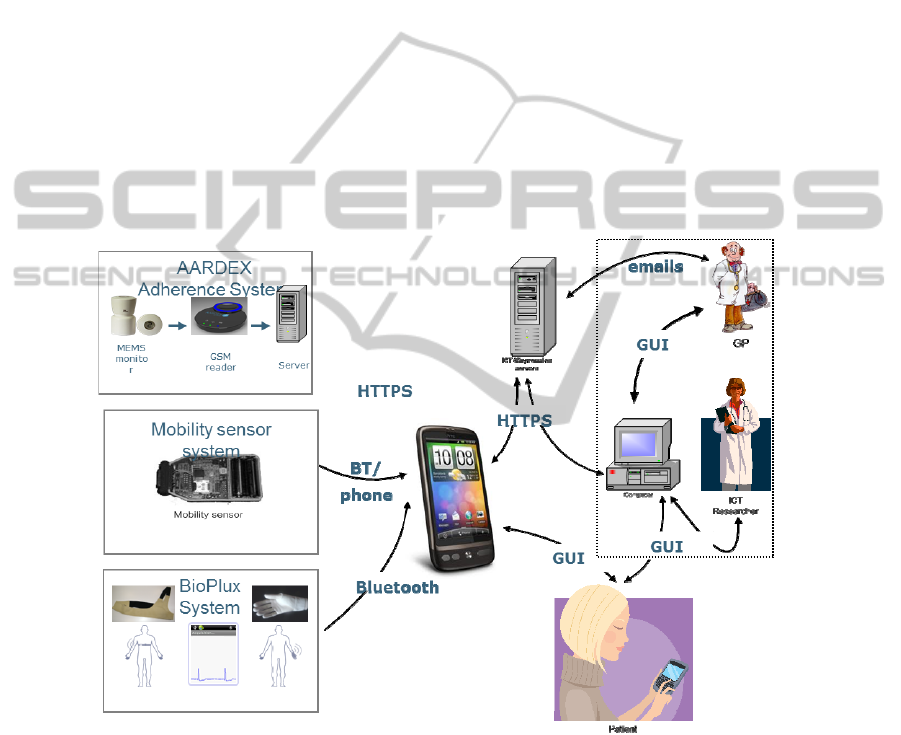
The mobile system architecture is shown in Fig.
1
. For reference, the other com-
ponents of the ICT4Depression system are shown in the dashed box. The user inte-
racts with the mobile system through a Samsung Galaxy S smart phone. A dedicated
graphical user interface presents the user with information on the treatment, allows
the user to execute those parts of the treatment that need user input, incorporates a
calendar and acts as a sensor data aggregator for the biomedical sensors. These con-
sist of a hand worn device for the measurement of electro-dermal activity (EDA) and
blood volume pulse. Whereas the latter yields information on the heart rate, the EDA
is an indicator for a wide range of emotional responses, thus providing the system an
additional insight in the user’s mental state. The second biomedical sensor is a chest
strap that can be worn under normal clothing. The chest strap provides heart rate,
respiration rate and an accelerometer that can be used to infer the trunk orientation of
the user. The latter data is combined with motion data measured directly on the smart
phone to obtain accurate information on patient physical activities.
Fig. 1. Overview of the ICT4Depression System.
Treatment of depression is normally supported by medication and the adherence to
the prescribed medication regimen is often low. For this reason, a smart pill box is
used to monitor medication intake. All sensor data is sent to a dedicated server where
analysis of the data takes place in a reasoning system that incorporates models of the
user and their progression. This system can assess whether the treatment is successful
48
and provides the medical staff and user with advice for further treatment. The rest of
this paper will discuss the system in more detail. In Section 2 the graphical user inter-
face will be discussed after which the various sensors will be introduced in Section 3.
Sections 4 and 5 introduce the reasoning system and server infrastructure respectively
and conclusions are presented in Section 6.
2 Graphical User Interface
The patient has access to the ICT4Depression system through a smart phone interface.
The interface is developed using html and java scripts, which are stored on the phone
such that the application can also be used if there is no connectivity. For conformity
in the presentation of the treatment modules to the patient and for ease of treatment
module development, a structure of available module screens was developed.
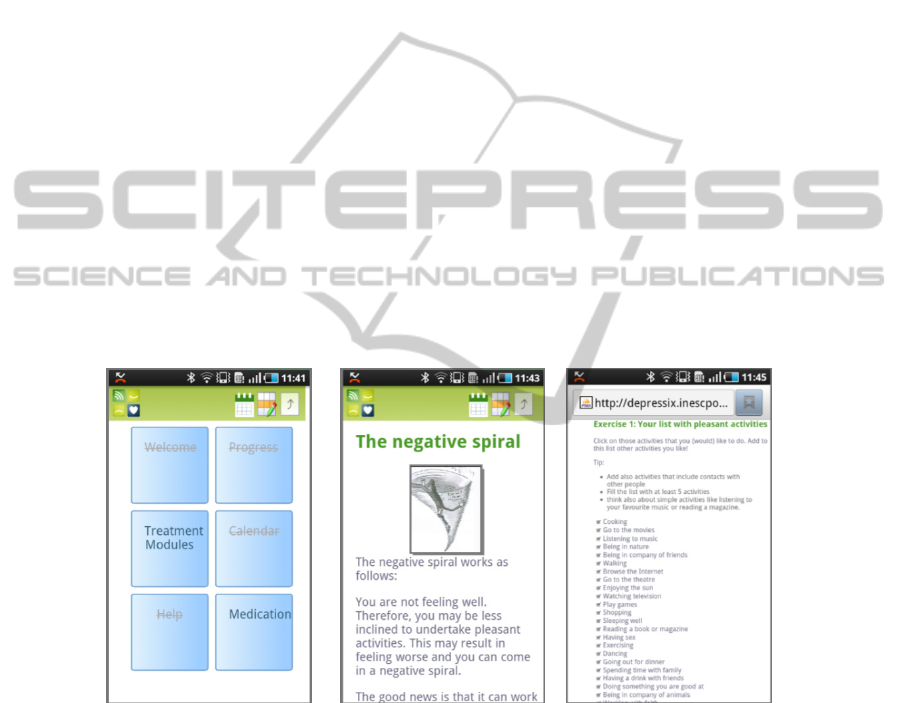
The first category of screens is the navigation screen, which is depicted in
Fig. 2.
Its primary function is to facilitate navigation through and around the application.
Through the use of these screens, patients can access further navigation controls, read
module content or undertake module centric activities.
The module content screens, as depicted in Fig.
3, allow the patient to read about
the treatments available in the ICT4Depression application.
The third category of screen is the patient input screen, an example of which is
shown in Fig.
4. This page type requires interaction between the patient and the mod-
ule to assist in the patient’s treatment.
Fig. 2. Navigation Screen.
Fig. 3. Module Content
Screen.
Fig. 4. Patient input screen.
A logo is present on every screen which acts as a link that will allow the patient to
immediately link back to their home page. Because the patient should be able to re-
turn to the source screen, a button with sitemap functionality is integrated into the
application. On clicking this button, the patient is able to navigate back to a previous
screen. An additional button for inclusion in the ICT4Depression application is the
49

calendar quick link. This button enables the patient to view, edit and add module
activities to their personalised calendar as necessary. Finally an activities quick link
was included to enable patients to access their exercises and activities from anywhere
within the application.
3 Sensor Systems
One of the innovative aspects of this system is the use of sensors in various ways to
elicit information on the user’s well-being and treatment progression. To this end,
biomedical sensors are used to measure heart rate, breathing rate and electro-dermal
activity, the phone itself is used to measure user physical activity and a medication
adherence system monitors the user’s medication intake.
3.1 Biosignal Acquisition System
Two wearable sensor form factors can be used by the patient enabling the measure-
ment of multiple biosignals. The devices are controlled by the mobile phone through
an Application Programming Interface (API) and corresponding software develop-
ment kit (SDK) and are used to sample raw sensor data. The relevant characteristics,
like the heart rate [4] or skin resistance changes [5,6] are detected and extracted from
the signal. Finally, the resulting data are sent to the mobile phone via the wireless
Bluetooth protocol. In the next sections we describe the Chest Strap and Glove proto-
types.
3.1.1
Chest Strap
The chest strap, which is shown in Fig. 5 has three embedded sensors and one acquisi-
tion system. The sensors are an ECG (Electrocardiography), Respiration sensor and
tri-axial accelerometer that are situated in the chest of the wearer. All the embedded
electronics are easily removable and reassembled, to allow the wearer to machine-
wash the chest band when the need arises.
Fig. 5. Textile enclosure and device for chest use.
The chest strap form factor allows an easy and seamless placement of the acquisi-
tion system and sensors. In the following pictures, the acquisition system and the
50
sensors are embedded inside the textile band. It is slid in the narrow space between
two seams. This creates the needed stability to obtain a good respiration signal. The
chest band opening that houses the acquisition system and the sensors, is closed by
means of a metallic snap or a zipper. The three electrodes of the ECG sensor must be
aligned with three small holes in the textile and then the snaps must be closed. This is
essential to obtain the ECG signal and it will help also in maintaining the system in its
place while in use. The technical specifications are described in Table 1.
Table 1. Specifications of the chest strap device.
Sensor Specifications
Accelerometer
±5G
3-axis
MEMS technology
Respiration
1 Hz low-pass filter
Piezofilm technology
ECG
Gain 1000
0.05-30 Hz band pass filter
110 dB CMRR
> 100 MOhm input impedance
3.1.2 Glove
The glove has two embedded sensors and one acquisition system. The sensors are an
EDA (Electro-dermal Activity) and BVP (Blood Volume Pulse) that are situated in
the palmar side of the non-dominant hand of the wearer (for this document the left
hand is used). All the embedded electronics are easily removable and reassembled, to
allow the wearer to machine-wash the glove when the need arises.
The acquisition system and the sensors must be placed in the correct locations before
the user puts the glove on. The BVP sensor is passed through a small opening in the
textile. This sensor will stay in its place by means of Velcro or a metallic snap. For
the EDA sensor, the process is also very simple. The two wires with metallic elec-
trodes must be aligned with the two small holes in the textile and then the snaps must
be closed.
Fig. 6 depicts the sensor system and placement in the hand. Through the
integrated sensors, this system enables us to acquire heart rate and skin conductance
response (SCR). The technical specifications are described in
Table 2.
Table 2. Specifications of the glove device.
Sensor Specifications
EDA
3 Hz low-pass filter
> 1 TOhm input impedance
BVP
Double emitter/Single detector setup
Infrared wavelength range
51

Fig. 6. Textile enclosure and device for hand useTextile enclosure and device for hand use.
3.2 Physical Activity Monitor
On the mobile phone the accelerometers are used to obtain a better insight in user
physical activity behaviors. Raw acceleration data is used in a physical activity moni-
toring algorithm to determine periods of lying, sitting, standing, walking, running and
energy expenditure. To obtain further insights in the user’s activities, the phone’s
GPS is used to obtain a geo-location based perspective on user behavior without con-
tinuously tracking the user location. The user defines a list of places in which they
perform social and exercise activities. Whenever the GPS indicates that the phone is
within a preset distance from any of these points, this is logged and thus an indication
of the frequency and duration of time spent in these locations is obtained.
3.3 Medication Adherence System
Sub-optimal adherence to prescribed medicines is frequently the principal obstacle to
successful pharmacotherapy in ambulatory patients, especially when unrecognized
clinically, as often occurs [7]. Sub-optimal adherence is highly prevalent, associated
with poor outcomes of treatments that, when administered correctly, have well-
established benefits. For unclear reasons, sub-optimal adherence and its conse-
quences have been a largely neglected aspect of therapeutics. Across all fields of
ambulatory pharmacotherapy, a large number of patients do not adhere to effective
treatments including circumstances in which life-saving medicines are available for
life-threatening diseases.
Electronic monitoring of ambulatory patients’ dosing histories has repeatedly re-
vealed that their drug intake is frequently irregular, spanning a wide spectrum of dev-
iations from the prescribed regimen. It is strongly skewed toward under-dosing,
created by delayed and omitted doses, sometimes occurring in multiple, sequential
omissions of prescribed doses. Those deviations, in turn, tend to nullify therapeutic
actions of the drugs in question, contributing thereby to worsening of disease, and
increased health care costs.
Given the clinical and economic impact of non-adherence, urgent actions need to
be taken to enhance patient adherence to drug therapies. During the last decade, many
interventions have been tested but few of them have addressed simultaneously both
the intentional and unintentional aspects of non-adherence to medications [8]; [9];
[10]; [11]. These successful interventions rely on the two principal values of electron-
52
ic monitoring: first, it provides objective and reliable information on patient’s dosing
history, which defines the extent of the exposure to the prescribed medication;
second, the dosing history serves as a crucial element of intervention methods to
manage adherence to medication [12].
Until recently, those interventions took place at clinical visits, typically every few
months, and were corrective by nature. Today, new ICT technologies allow the re-
mote monitoring of patients’ adherence to drug therapies, providing timely informa-
tion to both caregivers and patients to support effective medication management.
3.3.1
Adherence Monitoring System
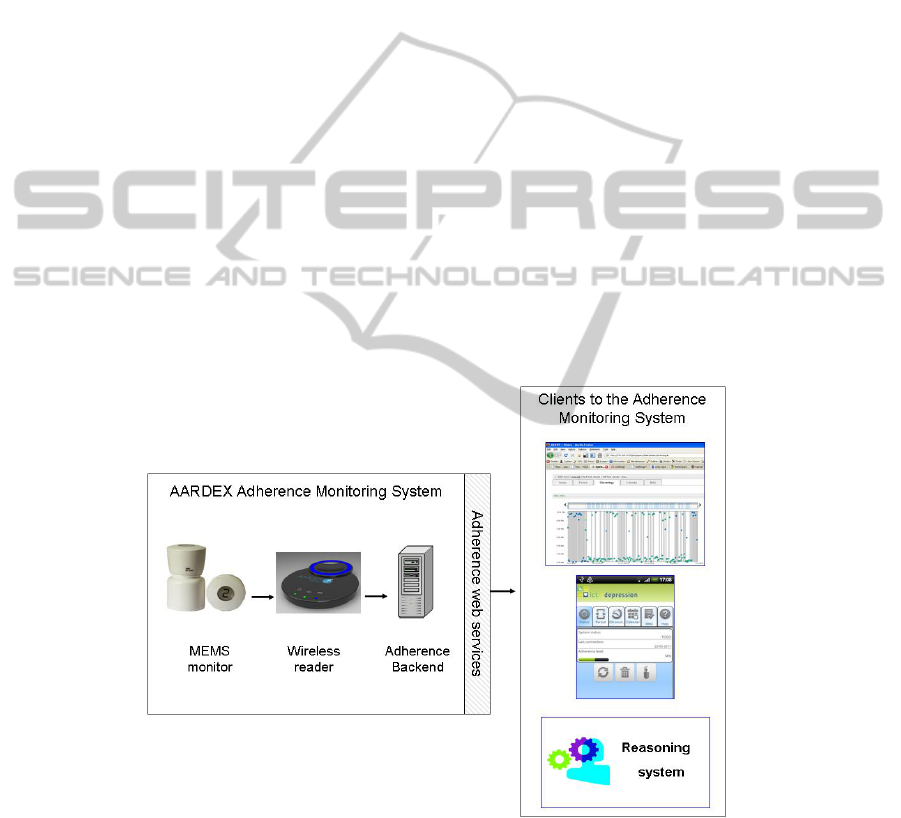
The adherence system is depicted in Figure 7. This system covers the chain needed to:
Monitor adherence data
Wirelessly transfer adherence data to a dedicated server
Provide information on adherence to different types of client
The main goal of the adherence monitoring system is to assure the collection of adhe-
rence data but, more importantly, to facilitate their integration in external systems.
These systems require different levels of integration. Some may simply need a visua-
lization of adherence data while others expect more advanced feedbacks based on the
detection of highly contextual adherence issues (e.g risk of treatment discontinuation
in depressed patients, detection of drug holidays in HIV patients). Some systems may
push the integration a step further by accessing raw adherence data for pharmacoki-
netic-pharmacodynamic modeling.
Fig. 7. Adherence monitoring system.
The architecture of the adherence system is based on the following elements:
53

The MEMS monitor is a pill container with integrated electronic micro circuitry
designed to record the date and time of each opening and closing of the container. It
also provides direct basic feedback to the patient through an LCD screen.
The wireless reader is used to download data from the MEMS monitor and wire-
lessly transfer these data to the adherence backend.
The adherence backend stores adherence data and supports their interpretation.
This backend can be accessed in a secured way through web-services by different
clients.
Finally, specific components have also been developed to facilitate the integration
of adherence data into those clients. An android and a javascript adherence module
have been developed.
4 Reasoning System
One of the key elements of the overall system is an intelligent reasoning system to
support the patient in a highly personalized manner. The system essentially combines
the data that has been obtained from sensors (including the information that the pa-
tient has provided to the system, e.g. rating of mood) to an overall picture of how the
patient is functioning. Based upon this overall picture, the system can then decide to
provide feedback to the patient (in the form of motivational messages or reminders),
but the system can also decide to suggest therapeutic changes. Four main parts are
distinguished that establish this behavior: (1) a data abstraction component, (2) a
virtual patient component, (3) an evaluation component, and (4) a communication
component. In Fig.
8 the overall structure of the reasoning system is shown.
Fig. 8. Overview of the reasoning system.
On a high level, the reasoning system first abstracts the data to determine the cur-
rent state of the patient (e.g. how much is the patient involved in the therapy). Besides
assessing the actual behavior of the patient, the reasoning system also comprises of a
virtual patient that makes predictions about the state of the patient (the component
virtual patient) given his/her characteristics (obtained from the sensor data) and the
type of therapy. In the evaluation component the current state of the patient is eva-
luated as well as the therapeutic success. This is performed by analyzing the measured
reasoning
system
data
abstraction
virtualpatient
sensordata
evaluation
communication
generation
assessedstates
and detaileddata
evaluationoftherapy
messages
54

state itself, but also by comparing these states with the predictions of the virtual pa-
tient. Finally, in the component communication generation the evaluation is used to
advice a different therapy in case another therapy is expected to be more successful.
Furthermore, more instant forms of feedback are generated based upon the sensory
data including the sending of reminders, and providing of motivational messages.
Below, each of the components is treated in more detail.
4.1 Data Abstraction
In the data abstraction component the idea is to compose an abstract overall picture of
the patient. This overall picture indicates the patient state and the trends in the patient
state (e.g. the general patient state is good, but the trend is negative) and similar for
the therapeutic state (e.g. the involvement is bad, but an increasing trend in involve-
ment can be seen). In order to establish this behavior, a dedicated language to express
complex temporal patterns called the Temporal Trace Language (TTL) has been used
(cf. [13]). First, the measurements are abstracted in a temporal fashion (e.g. calculat-
ing the average mood during a day), thereafter trends are identified in this abstracted
data (e.g. the average mood was good during that particular day). Finally, the trends
of multiple measurements are aggregated into a single overall patient and therapeutic
state, which makes the approach more robust against missing data. In this aggrega-
tion, each particular measurement is assigned a certain weight in the overall compila-
tion of the picture.
4.2 Virtual Patient
The second component concerns a so-called virtual patient model. This model is able
to make predictions about the development of the patient during a certain therapy. In
order to do so, dedicated computational models are present that express the states
within the patient (e.g. mood, appraisal) and how these states influence each other. In
addition, the therapeutic influence is also modeled. The models incorporated in the
virtual patient prediction component are described in more detail in [15,16,17]. As an
input for these models, the characteristics for the patient as provided in a question-
naire are used. The output of the prediction is the development of the general patient
state and therapeutic development over time given a certain therapy which is fol-
lowed.
4.3 Evaluation
The evaluation component creates an assessment of the patient by comparing the
predictions using the model with the actual state of the patient. In case the patient is
significantly underperforming, a process is started to evaluate alternative therapies
and see whether these might be more effective. This evaluation again takes place
using the virtual patient model, thereby possibly altering the parameters of the model
to make sure that the model is an accurate description of the patient. As a result, the
component derives whether a therapeutic change should be advised. A more detailed
55
description of the evaluation process can be found in [14].
4.4 Communication Generation
The final component is the generation of communication to the patient. This commu-
nication can either concern information about a therapeutic switch (due to the evalua-
tion made in the previously discussed component), but can also involve motivational
messages and reminders. The messages are generated using dedicated rules that ex-
press in what situation what information should be communicated to the patient. Note
that not only the high level assessment are hereby considered, but also the immediate
sensory information, for instance a positive mood rating by the patient could trigger a
message expressing that it is good to hear that the patient is feeling well.
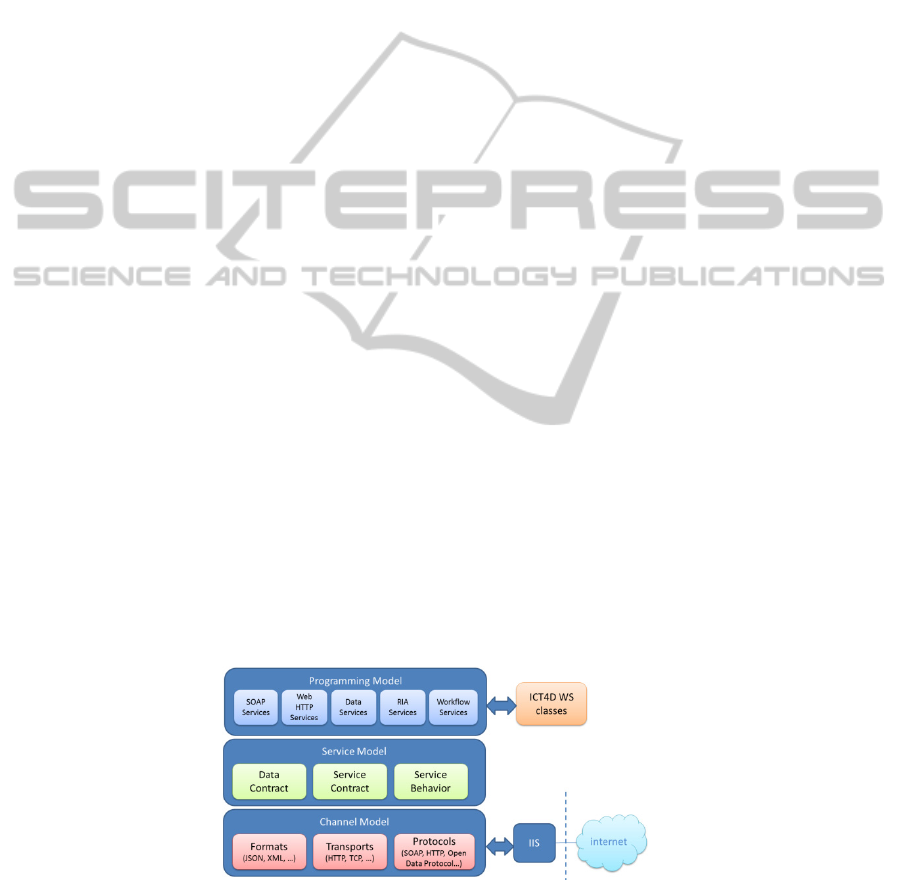
5 System Server and Infrastructure
The server main goal is to work as an information repository to be accessed in a web,
decentralized and in an interoperable fashion. The current clients are developed with-
in the project consortium, but this architecture allows expandability and openness to
new market players.
The repository uses the Microsoft SQL 2008 database management system. To en-
sure the standard data protection, the database TDE (Transparent Data Encryption)
[18] feature was used. For the information exchange the option in use was the Web
Service development over the WCF (Windows Communication Foundation) [19]
targeting .NET Framework 4. This framework, as other modern frameworks, allows
the use of WS (Web Services) standards, which enable the development of service
oriented applications. As such, the ICT4Depression is a SOA (Service Oriented Ar-
chitecture) that relies on WS to send and receive data. The main advantage is the
loose coupling between client applications and repository. This implies that any client
created on any platform can connect to the ICT4Depression system according to es-
tablished information access policies, as long as the essential contracts [20] are met.
The current client applications are WS client applications, a web client PHP applica-
tion and a mobile application running on Android. They implement the therapy mod-
ules and use XML/JSON over HTTPS to communicate to the server, which imple-
ments both the synchronous and asynchronous web method invocation.
Fig. 9. ICT4D SOA layers.
56

6 Conclusions
In this paper a mobile system designed for the continuous treatment of depression is
presented. The mobile system uses a smart phone to provide the treatment to the user,
obtain input from the user and display feedback and advice. Biomedical sensors and
the phone itself measure parameters which are linked to emotional markers to obtain
further information on the user’s well-being and treatment progression. The user’s
adherence to the set medication regimen is monitored using a dedicated medication
adherence system. All information is gathered in a server where a reasoning system
analyses the data, determines the treatment progression and provides feedback to the
user. The system will be tested with real users in 2012.
Acknowledgements
This work was funded by the Seventh Framework Programme (FP7) under the
ICT4Depression project (grant agreement 248778) and by the Fundação para a
Ciência e Tecnologia (FCT) under the grant SFRH/BD/65248/2009, whose support
the authors gratefully acknowledge.
References
1. Andrade L. et al.: The epidemiology of major depressive episodes: results from the Interna-
tional Consortium of Psychiatric Epidemiology (ICPE) Surveys (2003) Int J Methods Psy-
chiatr Res.;12(1):pp3-21
2. Andersson G., Cuijpers P. Pros and cons of on-line cognitive behaviour therapy. (2008)
British Journal of Psychiatry, 193, 270–271.
3. Heron, K. E, Smyth, J. M. Ecological momentary interventions: Incorporating mobile
technology into psychosocial and health behaviour treatments (2012) British Journal of
Health Psychology, 15, 1–39
4. Agelink, Marcus, Cavit Boz, Heiko Ullrich, and Jurgen Andrich., (2002) Relationship
between major depression and heart rate variability. Clinical consequences and implications
for antidepressive treatment. Psychiatry Research 113:139-149.
5. Fraguas, Renerio, et al., (2007) Autonomic reactivity to induced emotion as potential pre-
dictor of response to antidepression treatment. Psychiatry Research 151:169-172.
6. Iacono, William, David Lykken, Lori Peloquin, Ann Lumry, Roger Valentine, and Vicente
Tuason, (1983) Electrodermal Activity in Euthymic Unipolar and Bipolar Affective Dis-
orders. Arch Gen Psychiatry 40:557-565.
7. Osterberg L, Blaschke T., Adherence to medication. 2005, N Engl JMed, Vol. 5, pp. 487-
97.
8. Burnier M, Schneider M. P., Chiolero A., Stuci C. L., Brunner H. R., Electronic compliance
monitoring in resistant hypertension: the basis for rational therapeutic decisions. 19, (2001),
J Hypertension, pp. 335- 41
9. Schmitz, J. M. et al. Medication compliance during a smoking cessation clinical trial: a
brief intervention using MEMS feedback. 2, (2005), J.Behav.Med, Vol. 28, pp. 139-47.
10. Mooney, M. E., et al. Adding MEMS feedback to behavioral smoking cessation therapy
increases compliance with bupropion: a replication and extension study. 4, (2007), Ad
57

dict.Behav, Vol. 32, pp. 875-80
11. Vrijens B., Belmans A., Matthys K., de Klerk E., Lesaffre E. Effect of patient intervention
and compliance-enhancing pharmaceutical care on adherence with atorvastatin. (2006),
Pharmacoepidemiol Drug Saf, Vol. 15, pp. 115-21.
12. Blaschke T, Osterberg L., Vrijens B., Urquhart J. Adherence to Medications: Insights Aris-
ing from Studies on the Unreliable Link Between Prescribed and Actual Drug Dosing His-
tories. (2012) Annu. Rev. Pharmacol. Toxico, (in press).
13. Bosse, T., Jonker, C. M., Meij, L. van der, Sharpanskykh, A., and Treur, J., Specification
and Verification of Dynamics in Agent Models. International Journal of Cooperative In-
formation Systems, vol. 18, 2009, pp. 167 - 193.
14. Both, F., and Hoogendoorn, M., Utilization of a Virtual Patient Model to Enable Tailored
Therapy for Depressed Patients. In: Proceedings of the 18th International Conference on
Neural Information Processing, ICONIP 2011. Lecture Notes in Computer Science, Sprin-
ger Verlag, to appear.
15. Both, F., Hoogendoorn, M., Klein, M. C. A., and Treur, J., Computational Modeling and
Analysis of the Role of Physical Activity in Mood Regulation and Depression. In: Wong,
K. K. W., Mendis, B. S. U., Bouzerdoum, A. (eds.), Neural Information Processing: Theory
and Algorithms, Proceedings of the 17th International Conference on Neural Information
Processing, ICONIP'10. Lecture Notes in Artificial Intelligence, vol. 6443. Springer Verlag,
2010, pp. 270-281.
16. Both, F., Hoogendoorn, M., Klein, M. C. A., and Treur, J., Computational Modeling and
Analysis of Therapeutical Interventions for Depression. In: Yao, Y., Sun, R., Poggio, T.,
Liu, J., Zhong, N., and Huang, J. (eds.), Proceedings of the Second International Confe-
rence on Brain Informatics, BI'10. Lecture Notes in Artificial Intelligence, vol. 6334,
Springer Verlag, 2010, pp. 274-287.
17. Both, F., Hoogendoorn, M., Klein, M. A., and Treur, J., Formalizing Dynamics of Mood
and Depression. In: M. Ghallab, C. D. Spyropoulos, N. Fakotakis and N. Avouris (eds.),
Proceedings of the 18th European Conference on Artificial Intelligence, ECAI'08. IOS
Press, 2008, pp. 266-270.
18. Microsoft, "Understanding Transparent Data Encryption," [Online]. Available:
http://msdn.microsoft.com/en-us/library/bb934049.aspx.
19. Microsoft, "Windows Communication Foundation Architecture," [Online]. Available:
http://msdn.microsoft.com/en-us/library/ms733128.aspx.
20. Microsoft, "Fundamental Windows Communication Foundation Concepts," [Online].
Available: http://msdn.microsoft.com/en-us/library/ms731079.aspx.
58
