
KNOWLEDGE BASED DECISION SUPPORT FOR THE
MANAGEMENT OF CHRONIC PATIENTS
Sara Colantonio, Massimo Martinelli, Ovidio Salvetti
Institute of Information Science and Tecnologies, ISTI-CNR, Via G. Moruzzi, 1-56124, Pisa, Italy
Giuseppe De Pietro, Massimo Esposito, Alberto Machì
Institute for High Performance Computing and Networking, ICAR-CNR, Via P. Castellino, 111-80131, Napoli, Italy
Keywords: Decision support, Knowledge formalization, Ontologies.
Abstract: Due to the current socio-economic impact of chronic diseases, a strong effort is being spent in the
development of ICT applications able to support a new care paradigm specialized for chronic patients. Such
applications are mainly based on patients’ telemonitoring for the collection of a number of relevant
physiological parameters aimed at identifying and preventing acute events, while maximizing patients’
quality of life and reducing clinical costs. The most advanced and challenging features of these ICT
applications are intelligent services devoted to the interpretation of monitored patients’ data for supporting
clinicians in their routine management of chronic patients. In this paper, a Knowledge-based Clinical
Decision Support System (KB-CDSS) is presented, which is aimed at aiding clinical professionals in
managing chronic patients on a daily basis, by assessing their current status, helping face their worsening
conditions, and preventing disease exacerbation events. The CDSS has been developed by encoding the
relevant knowledge elicited from clinicians who have a large experience in patients’ monitoring. A
formalism based on ontologies and rules was selected to build the Knowledge Base according to a scenario-
based approach. The system is currently under validation for the management of real clinical cases.
1 INTRODUCTION
Chronic diseases are one of the leading causes of
disability and death in most of the industrialized
countries, and have a deep impact on today’s
society, with social health-security systems under
constant pressure, both for financial and
organizational aspects, especially in many European
countries. A chronic disease usually causes major
limitations in patient’s daily living and are
characterized by acute or deterioration events, which
can happen more or less frequently and often cannot
be totally relieved, causing a worsening of patient’s
conditions.
Health organizations all over the world are more
and more focusing on the development of specific
programmes for the management of chronic patients
in the long term. These are mainly based on the
regular collection of information about patients’
status and actions, their compliance to the therapy,
the situation around them, and their interactions with
the environment, in a long-stay setting. Tele- or
home-monitoring programmes are, hence, being
studied and applied for care delivery and
management in cases of chronic diseases (Parè et al.,
2007). ICT solutions are being developed for this
task, and range from (i) “light” applications, based
on video or phone consultations of patients for
assessing their current conditions (Cleland et al.,
2005; Vitacca et al., 2009), to (ii) the continuous or
frequent acquisition of patients’ vital signs through
dedicated sensors, often wearable (e.g., Pentland,
2004), till (iii) complex platforms that merge such a
sensor infrastructure with intelligent services for
data interpretation (e.g., Chiarugi et al., 2010).
The intelligent components are the most
advanced and challenging feature of these
telemonitoring platforms. The intelligence can be
implemented at different level of complexity: (i) as
simple alarming services, which identify variations
in patient’s vital signs, (ii) as interpretation methods,
which recognize exacerbation events, or (iii) as
220
Colantonio S., Martinelli M., Salvetti O., De Pietro G., Esposito M. and Machì A..
KNOWLEDGE BASED DECISION SUPPORT FOR THE MANAGEMENT OF CHRONIC PATIENTS.
DOI: 10.5220/0003657902200225
In Proceedings of the International Conference on Knowledge Engineering and Ontology Development (KEOD-2011), pages 220-225
ISBN: 978-989-8425-80-5
Copyright
c
2011 SCITEPRESS (Science and Technology Publications, Lda.)
complex Clinical Decision Support Systems (CDSS),
which are aimed at supplying to clinicians full
assistance in their management of chronic patients.
In this paper, a knowledge-based CDSS is
proposed for managing chronic patients by
interpreting data acquired through a sensor
infrastructure deployed in patients’ normal life
environment. Such a system combines acquired data
with patient’s clinical information, issues possible
alarms and supplies motivated suggestions. Though
the modelling strategy is valid for any chronic
disease, two pathologies were considered for initial
application, namely Chronic Obstructive Pulmonary
Disease (COPD) and Chronic Kidney Disease
(CKD). The system was developed within the EU
IST Project CHRONIOUS which is aimed at
defining a generic platform schema for health status
monitoring, addressed to and specialized for people
suffering from chronic diseases (Rosso et al., 2011).
In the following sections, the strategy followed
is described in more detail, presenting and
motivating the CDSS design, the data it handles and
the knowledge it utilizes. Particular focus is
dedicated to how this knowledge is formalized.
2 THE INTELLIGENT SUPPORT
TO CHRONIC DISEASES
MANAGEMENT
For being effective and profitable, the management
of chronic patients requires monitoring patients in
order to follow up their conditions and detect the
incoming or the occurring of acute events.
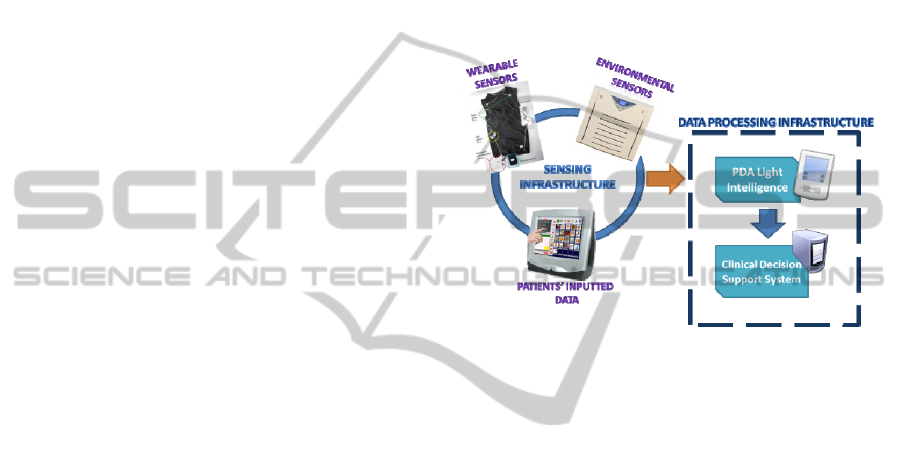
For making this possible, a platform of services
was devised to acquire and store data through a
sensing infrastructure consisting of (i) a set of
wearable sensors for the acquisition of patients’
physiological parameters, (ii) a set of environmental
sensors for the acquisition of contextual information
and (iii) a touch-screen device used for the
acquisition of patient’s answers to questionnaires.
Data collected during patient’s clinical visits were,
also, gathered by the platform and stored in the
internal repository (for a more detailed description
of the platform please refer to (Rosso et al., 2011)).
Intelligent services were added into the platform
in order to automatically process the collected sensor
data, identify worrying patient’s conditions and
alerting clinicians. In particular, to reach a high level
of flexibility and reliability, two levels of sensor data
interpretation were conceived: the data acquired by
the sensing infrastructure are firstly processed by a
light intelligence deployed on a smart Personal
Digital Assistance device (PDA) for detecting
possible changes in patient’s vital signs by applying
simple rules related to the collected parameters.
Worrying changes are reported as an alert to clinical
personnel and data are passed to a second level of
intelligence, i.e., the CDSS, which supplies more
accurate suggestions thanks to its ability to process a
larger piece of information. Figure 1 summarizes the
main components of the monitoring platform. Focus
of this paper is on the CDSS described in next
sections.
Figure 1: The main components of the patients’
monitoring platform: the Sensing infrastructure and the
Data Processing infrastructure consisting of two levels of
intelligence.
2.1 The Decision Support System
The CDSS was designed to be really effective,
efficient and to be perceived really useful by the
clinicians it should support. Its main functionalities
can be listed as follows:
analysing the acquired sensor data for identifying
worrying conditions;
alerting clinicians when an acute event happens;
merging the heterogeneous patient’s information
for providing pertinent suggestions.
The data are gathered by a sensorized vest that
collects parameters pertaining patient’s
electrocardiographic activity, respiratory activity,
arterial oxygen saturation, skin temperature. These
data are acquired by the sensors on the vest and,
then, collected by a Data Handler, wired to the vest,
which sends them to the PDA via a Bluetooth
connection. The acquired parameters are the
following:
heart rate;
respiration rate, inspiration and expiration time;
inspiration and expiration volume;
ambient temperature and humidity;
motion activity and fall;
KNOWLEDGE BASED DECISION SUPPORT FOR THE MANAGEMENT OF CHRONIC PATIENTS
221

cough and snoring.
A touch-screen workstation, the Home Patient
Monitor (HPM), is employed to collect a number of
other physiological and contextual parameters. More
in detail, an environmental device, installed in
patient’s living room and cable-connected with the
HPM (USB connection), acquires contextual data
related to ambient light, carbon monoxide, volatile
organic compound and air particle. Body weight,
blood pressure and blood glucose are measured
using commercially available devices, which send
data to the HPM via a Bluetooth connection. Finally,
information pertinent to patient’s lifestyle, food and
drug intake, and psychological conditions is
collected through questionnaires proposed on the
touch-screen of the HPM. All these data are
gathered, on a regular time basis via a wireless
connection, by a PDA assigned to each patient. The
PDA performs a first data processing by applying
simple range checking rules and detects possible
alarming situations, alerting, in this case, the
personnel on duty, and requires an in-depth analysis
of the situation by the CDSS.
Indeed, the CDSS was designed to be invoked
each time new data to be analyzed are available, and
this happens in three scenarios:
when the PDA detects a worrying condition
and issues an alarm: in this case, the sensor
data collected are sent to the CDSS;
at the end of each day: when the PDA stores all
the collected data and sends them to the CDSS
for their analysis;
when a patient undergoes a clinical visit: the
newly collected data are sent to the CDSS for
interpretation.
In all these cases, the CDSS correlates these data
with historical patient’s data according to the
knowledge modeled into its Knowledge Base (KB),
and supplies, as a response, a diagnosis about
current patient’s status, plus suggestions about what
to do. The KB is the main component of the system
and is modeled for inferential reasoning, through a
dedicated inference engine, as described in the next
section.
2.2 The Knowledge Base
The clinical knowledge modeled for developing the
KB consists of:
the structure of the domain knowledge, namely
the declarative knowledge;
the knowledge about the procedures of the
decision making activity, namely the procedural
knowledge.
In particular, the declarative knowledge concerns
the domain compositional elements, such as raw and
abstract concepts, their properties and inter-relations.
On the other hand, procedural knowledge captures
the behavioral logic and provides more explicit
information about which actions/conclusions can be
taken/drawn from declarative knowledge. The
formalism selected for encoding both these types of
knowledge consisted in one ontology and a set of
production rules (i.e. a set of conditional statements
expressed in form of "if antecedents then
consequent") built on the top of it.
The main purpose of the ontology and rules is to
represent domain-specific knowledge necessary to
remotely support clinical operators in the daily
home-monitoring of chronic patients. The approach
is generally aimed at the chronic disease
management, but specific focus was given to the two
pathologies chosen for system demonstration, i.e.,
COPD and CKD.
The way the knowledge is represented for
clinical decision support is one of the most key
facets for having a successful CDSS, starting from
the analysis and design of the CDSS at the very
beginning and ending to the implementation of the
CDSS at the final stage. Ontologies combined with
production rules seemed the most suitable and up-to-
date methodology for solving this task since easily
understandable by a non-specialized audience, e.g.
clinicians. In this way, they could be involved not
only in the knowledge elicitation and representation,
but also in the process of modification/updating of
existing knowledge.
In fact, the eliciting process ran through several
meetings with clinicians for systematizing the
approach to patients’ monitoring. The list of
monitored parameters was used as the starting point
to formalize all the statements about the different
situations and conditions that a patient can go
through and that can be identified by these
parameters. A great help to this process came from
the fact that clinicians were already skilled in
patients’ telemonitoring and were already trained at
interacting with computerized applications for
processing of clinical data.
The result of the elicitation was the formalization
of evidence-based statements which were used to
define the suggestions that should be provided by
the CDSS. The clinicians supplied these statements
in a rule-like form, written in natural language.
These were discussed and extended for creating a set
of consistent and complete rules to be processed by
an automated rule engine. The ontology was defined
to list up all the relevant concepts, selecting a
KEOD 2011 - International Conference on Knowledge Engineering and Ontology Development
222
terminology recognized and agreed by all the
clinicians involved in the elicitation process.
The Web Ontology Language, OWL (2009), was
chosen as ontology language, in order to grant both
formality and expressive power. As regards to the
rule representation, Jena rule language (Carroll et
al., 2004) was identified as the most appropriate
language for writing rules that can be combined with
OWL ontologies. In particular, such a language
enables to build rules starting from the
terminological elements defined in the OWL
ontology. Thanks to its concise but at the same time
very expressive syntax, Jena rule language was not
only easy to use for writing rules but also extremely
simple to read and understand also for non-technical
users and, thus, it was very adequate to provide
reasoning support that met the CDSS requirements.
Moreover, the Jena framework includes a Rule
Engine used for inference on the base of encoded
rules.
2.2.1 The Ontology
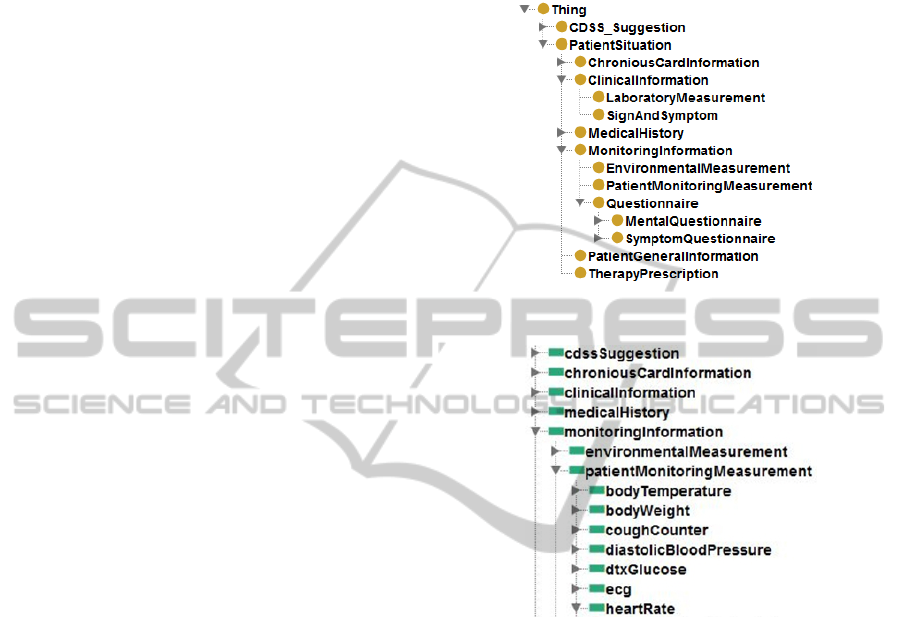
The ontology models all the clinical data coming
from different possible information sources, such as
medical history, patient’s general information,
laboratory assays, patient’s monitoring
measurements or environmental measurements
gathered at the patient's home, questionnaires about
mental problems or symptoms opportunely filled up
by the patient at home. Moreover, the ontology also
models the results of the inferences generated by the
CDSS in terms of suggestions to be reported to the
clinicians. Such suggestions are expressed in the
form of alerts, i.e. messages with a different
severity, varying according to the current patient’s
condition, that can require or not the attention of a
clinical operator. Each suggestion can also indicate a
variation of the patient's health status with respect to
the morbidity he/she is affected by. It includes in
natural language the specific clinical guideline
applied by CDSS and delineates the action which
has to be performed in response to the generated
alert.
According to this high-level description, the
ontology concepts and properties are defined. Figure
2 shows the concept taxonomy.
As regards the properties, it is worth noting that
all the properties defined in the ontology are
datatype properties according to the definition of
OWL language. Figure 3 shows the taxonomy of
properties. The use of only datatype properties
simplifies the writing of rules and their final
structure since in the rule antecedents and
consequents it is necessary to indicate only the
appropriate datatype properties, corresponding to
semantically defined terms, opportunely linked to
the concepts they are associated to.
Figure 2: The concept taxonomy.
Figure 3: A piece of the property taxonomy.
2.2.2 The Base of Rules
Based on the introduced ontology, production rules
were devised for the three scenarios introduced in
the previous section, with the final aim of
representing the procedural knowledge.
Rules are simple conditional declarations that
link a logical combination of antecedent conditions
to a consequent, according to the following “if-then”
structure: If (antecedents) then consequent
As a result, the structure of each rule is
composed of one or more antecedents, expressed in
terms of ontology properties concatenated by logical
conjunctive operators, which can be evaluated to be
either true or false. Disjunction is not supported. As
an example, a rule pertaining to the HypoVolemia
for CKD disease is reported in natural language as
follows:
All individuals with values of systolic blood pressure
<110 mmHg, heart rate > 115 beats/min, symptoms
of nausea or vomiting determined by means of the
KNOWLEDGE BASED DECISION SUPPORT FOR THE MANAGEMENT OF CHRONIC PATIENTS
223

CKD Symptom Questionnaire are classified as being
in an abnormal condition due to HypoVolemia. An
alert with red severity is contextually sent to the
medical doctor to report the situation
.
The implementation of this rule in accordance
with the Jena rule syntax and in terms of the
ontology concepts and datatype properties
corresponds to a group of rules: one of them has the
following form
HypoVolemia_Guideline_1_rule_3:
(?p rdf:type
CKD:PatientMonitoringMeasurement),
(?p CKD:systolicBloodPressure_curr ?a),
lessThan(?a,110),
(?p CKD:heartRate_curr ?b),
greaterThan(?b,115),
(?q rdf:type CKD:CKDSymptomQuestionnaire),
(?q CKD:neauseaOrVomiting ?c),
equal(?c,’true’^^xsd:boolean),
(?s rdf:type CKD:CDSS_Suggestion) ->
(?s CKD:inferredPatientCondition
‘Suspected Hypovolemia’^^xsd:string)
3 SYSTEM DEVELOPMENT &
RESULTS
The CDSS was modeled as a resource of a
monitoring platform as introduced in the previous
section and it is called on demand to analyze new
data about patient’s situation. This assures the
generality and flexibility of this system, which can
be easily plugged into any similar platforms.
The implementation of the system was organized
in decisional services, which are called when
specific events occur. The granularity of these
services was decided in accordance to the data flow
and the requirements of clinicians about the
intervention of the support system. It appeared, then,
profitable to make a correspondence between the set
of services and the set of identified scenarios
introduced in the previous section, which can be
named as follows:
the Alarm Checking scenario, which corresponds
to an assessment of patient’s status after an alarm
has been issued by the PDA, for alerting about a
possible exacerbation;
the Home Monitoring scenario, which
corresponds to a periodic assessment of patient’s
status, more precisely once a day, even without
any alerting exacerbation;
the Clinical Assessment scenario, which
corresponds to the evaluation of patient’s status
after a clinical visits, i.e., when new data comes
from the clinical environment.
Several advantages are assured by this approach,
since separated and well-focused services are: (i)
simpler to integrate; (ii) more flexible; (iii) can be
straightforwardly modified; (iv) their complexity can
be managed more easily. Moreover, this approach
made the implementation strategy of the system
straightforward: the decisional services were
mapped onto a Service Oriented Architecture
approach, and hence implemented as Web Services.
This assures the interoperability of the CDSS, whose
implementation does not depend on the platform:
thanks to the Web Services approach, the system can
be integrated in any other general platform without
any change to its structure.
The first step in the development of the
decisional services regarded the determination of
their mapping to the clinical domains, i.e. COPD and
CKD. Two services, named COPD_Decisional_
Service and CKD_Decisional_Service, were realized
respectively for COPD and CKD diseases. Each
service was delineated from a functional perspective
in terms of its operations, where each operation is
coarse-grained and models how the CDSS works for
a whole distinct usage scenario. Coarse-grained
services avoid the need to maintain state information
between service invocations, reduce the number of
network interactions required to implement a given
usage scenario, improving, this way, performance
and simplifying recovery in the case of failure.
For the development of the KB behind these
services, as introduced in the previous section, the
ontology was developed using OWL. Currently, it
consists of 28 concepts and 860 properties,
organized as outlined. The rules were structured in
scenarios and divided between the two pathologies:
totally the base of rules contains 435 rules for CKD
and 273 rules for COPD.
Results provided by the CDSS consist in an
advice about the status of the patient and a
suggestion about the action to be undertaken for
managing the situation. In agreement with
clinicians’ requirements, the results are shown as a
kind of alert/alarm through a Clinician GUI, listing
up a number of information. More in detail, the
CDSS results report:
an advice about patient’s status diagnosis;
a suggestion about what to do;
some additional information, for better
presenting such results;
a colour that indicates the severity of the advice
or alarm;
an explanation of the advice and suggestion
produced.
As an example, Figure 4 shows the results inferred
KEOD 2011 - International Conference on Knowledge Engineering and Ontology Development
224
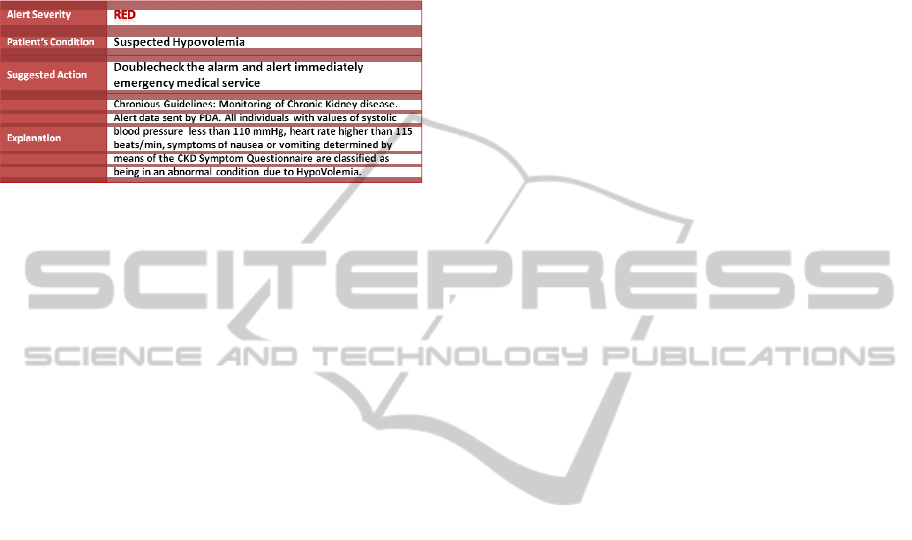
by CKD_Decisional_Service in terms of suggestions
generated in response to abnormal values firstly
identified by the PDA and then passed to the CDSS.
The system has been released to the clinicians
and the validation phase has started for testing the
system in action.
Figure 4: An example of results inferred by
CKD_Decisional_Service. The Explanation field states
that the suggestion is issued according to the guidelines
defined within the project, after an alert sent by PDA (i.e.,
the scenario) and the natural language form of the
guideline.
4 CONCLUSIONS
Due to the socio-economic impact of chronic
diseases, a large effort is being spent to develop
monitoring platforms able to follow up chronic
patients and support clinicians in their management.
In this paper, a knowledge based Clinical Decision
Support System has been presented which encodes
the relevant knowledge elicited from clinicians who
have a large experience in patients’ monitoring.
A formalism based on ontologies and rules was
selected for its expressive power and, at the same
time, ease of use and understanding also by non
technical users that can be involved in an eventual
upgrade process. A scenario-based approach was
adopted to implement the system by mapping each
scenario on a decisional service. Web Services were,
then, used to implement such services, assuring, in
this way, interoperability of the system and the
possibility to plug it into any monitoring platform of
the same kind.
The system was developed within the EU project
CHRONIOUS which is, currently, starting the
validation phase, during which the system will be
deployed to the clinical sites and its functioning
precisely tested.
ACKNOWLEDGEMENTS
This work has been partly funded by the EC IST
Project FP7-ICT-2007–1–216461 CHRONIOUS:
http://www.chronious.eu
. The authors wish to
acknowledge their gratitude and appreciation to all
the project partners for the development of the ideas
and concepts presented in this paper.
In particular, the authors would like to thank
Prof. M. Vitacca from Fondazione Salvatore
Maugeri, and Prof. Cusi and his team from the
University of Milan. The authors want to thanks all
the partners for their support. This paper was written
as a joint contribution; authors are listed in
alphabetical order and grouped by their affiliations,
besides they have equally contributed to this paper.
REFERENCES
Carroll J. J., et al. Jena: Implementing the semantic web
recommendations. In Proceedings of the 13
th
Int.l
World Wide Web conference on Alternate track
(WWW Alt.'04). ACM, New York, USA, 74-83
Chiarugi F., Colantonio S., Emmanouilidou D., Martinelli
M., Moroni D., Salvetti O. Decision support in heart
failure through processing of electro- and
echocardiograms. In: Artificial Intelligence in
Medicine, vol. 50 pp. 95 - 104. Elsevier, 2010
Cleland J. G. F., et al. 2005. Noninvasive Home
Telemonitoring for Patients with Heart Failure at High
Risk of Recurrent Admission and Death: The Trans-
European Network-Home-Care Management System
(TEN-HMS) study. Journal of the American College
of Cardiology, Volume 45, Issue 10, 17 May 2005,
Pages 1654-1664
OWL 2009. http://www.w3.org/TR/owl-features/
Paré G., Jaana M., Sicotte C., 2007. Systematic Review of
Home Telemonitoring for Chronic Diseases: The
Evidence Base. J. of the American Medical
Informatics Association, Vol. 14, Issue 3, May-June
2007, Pages 269-277
Pentland, S., 2004. Healthwear: Medical Technology
Becomes Wearable. in IEEE Computer, 37(5). May
2004. 34-41
Rosso R., Munaro G., Salvetti O., Colantonio S., Ciancitto
F., 2010 CHRONIOUS. In: EMBC 2010 pp. 6850 -
6853. IEEE.
Vitacca M., Bianchi L., Guerra A., Fracchia C.,
Spanevello A., Balbi B., Scalvini S., 2009. Tele-
assistance in chronic respiratory failure patients: a
randomised clinical trial. Eur Respir J; 33: 411–418
KNOWLEDGE BASED DECISION SUPPORT FOR THE MANAGEMENT OF CHRONIC PATIENTS
225
