
A CRITIQUE OF THE BENEFITS STATEMENT 2006/2007 FOR
THE UK NHS NATIONAL PROGRAMME FOR IT
Angus G. Yu
Stirling Management School, University of Stirling, Stilling, U.K.
Keywords: Value-based framework, Project value, Benefits management, Assessment methodology.
Abstract: With all the discussions of value and benefits based approach for managing information technology (IT)
investments, few organizations publish a benefits statement for an actual project or programme. Thus the
Benefits Statement 2006/2007 published by the UK NHS National Programme for IT (NPfIT) provides a
valuable sample for us to inspect and draw lessons from. This paper examines the statement from the
perspective of a value-based framework for project assessment. It is found that the NPfIT benefits statement
is defective for a number of reasons. In addition to an admittedly immature theory of IT value assessment,
the NPfIT authority did not start the programme with a baseline value proposition or a value assessment
methodology. It also failed to make a good use of a centrally prescribed methodology by the UK
government. It even ignored specific benefits estimates suggested by the government’s audit office. Most if
not all of these defects can be attributed to the lack of a coherent conceptual framework for project value
assessment in the NPfIT authority.
1 INTRODUCTION
There are many open questions regarding assessing
value contributions for any IT-based project or
programmes. Is it even possible to give an accurate
account of the value contribution of an IT project? If
it is, what is the overall framework for guiding the
compilation of such an account? This paper
contributes to answering the above questions
through a critique of a published benefits statement
(NHS, 2008) by the National Health Services (NHS)
in the UK on its large scale IT programme. The
critique is based on a value-based framework for
assessing project success.
The main contribution of the paper is to draw
methodological lessons on how the value and
benefits may be measured and presented for large-
scale IT-based projects and programmes. The paper
is organized as follows. First, the value based
framework is briefly introduced and its suitability as
the basis of the critique is discussed. Then the NHS
Benefits Statement 2006/2007 is introduced briefly.
A critique of the publication is then given from a
number of perspectives.
2 THE VALUE BASED
APPROACH
We proceed based on the assumption that an
important channel for information technology to
contribute to organizational value is through various
information systems and the information contained
therein. The design, development and
implementation of the information systems through
project and programme are a necessary part of value
creation process. Therefore, this paper is anchored
on the literature of the value-based approach (in
contrast to the alternatives like the multi-
dimensional approach, see e.g. Shenhar at el., 2001)
for assessing project and programme success. It
should be acknowledged that the value of
information and information systems might be
considered on their own, a project-based view is by
no means unique (Farbey et al., 1992; Love et al.,
2005; Thomas et al., 2007)
There is a degree of consensus for the value-
based approach for project and programme
management (Thiry, 2002; Yu et al., 2005; Winter
and Szczepanek, 2008; Tohidi, 2011). Yu et al.
(2005) proposed a specific value-based framework
for assessing project success which will be the
conceptual basis for the critique in this paper. A
482
G. Yu A..
A CRITIQUE OF THE BENEFITS STATEMENT 2006/2007 FOR THE UK NHS NATIONAL PROGRAMME FOR IT.
DOI: 10.5220/0003597804820487
In Proceedings of the 13th International Conference on Enterprise Information Systems (EIT-2011), pages 482-487
ISBN: 978-989-8425-55-3
Copyright
c
2011 SCITEPRESS (Science and Technology Publications, Lda.)

brief summary of the framework is given here for
the purpose of this paper. Readers are advised to
refer to the full paper for more details.
Assuming a classic product-based project
lifecycle, Yu at al. (2005) defined the concepts of
net project execution cost (NPEC) and net product
operational value (NPOV) as part of their value-
based assessment framework. At the initial project
execution stage, project cost dominates ancillary
project value, hence the net project cost and value is
designated as NPEC. By the end of project activities,
a product is produced which embodies the value for
the project sponsoring organization. This value is
represented by NPOV which is the sum total of all
the future values of the product, net any cost
associated with realising the values.
The concepts of NPEC and NPOV may be used
for assessing project success. They may be also be
used for describing how a decision is made to go
ahead with a project. These two uses correspond
roughly to “predictive evaluations” and “prescriptive
evaluations” (Remenyi & Sherwood-Smith 1999;
Thomas et al., 2007). However, project evaluation
should not be restricted to these two occasions alone.
There should be an on-going evaluative effort
through a project (Remenyi & Sherwood-Smith
1999). Of course, the earlier the evaluation in a
project lifecycle, the more it depends on estimates
and thus less certain. The later it is in a project
lifecycle, the more likely the factual evidence may
be available. Whenever the evaluation is carried, it
depends on an appropriate conceptual framework to
guide the necessary evaluative activities. A lack of
such a conceptual framework may lead to wasted
efforts and opportunities of project evaluation.
As a large scale IT-based change programme,
The UK Government’s NHS National Programme
for IT (NPfIT) is associated with a huge budget
(more later), and thus is always subject to public
scrutiny in terms of its value and benefits to the
public. The Benefits Statement 2006/2007 (NHS,
2008) is a welcome disclosure of how the
programme authority views the investment and
associated benefits. However, the publication reveals
that the NPfIT authority does not have a coherent
conceptual framework guiding its programme
benefits evaluation. The main motivation for this
paper is to provide a critique to NHS (2008) so that
methodological lessons may be learned for future
similar efforts.
There is a growing body of literature on project
and programme benefits management (Lin &
Pervan, 2003; Ward and Daniel, 2006; Docherty et
al., 2008). The words “value” and “benefit” may be
used in somewhat different ways in different
contexts but for the purpose of this paper, we treat
them as synonyms. The following section provides a
brief background to the programme, mainly based
on NAO (2006, 2008) and NHS (2007).
3 THE NHS NATIONAL
PROGRAMME FOR IT
3.1 Background
The NHS National IT Programme (NPfIT) is a
large-scale IT-based change programme. NPfIT was
initiated in 2002 by the UK central government and
aimed to deliver “four key developments” according
to its initiation document (NPfIT, 2004):
An electronic integrated care records service
including a nationally accessible core data
repository and digital images.
The provision of facilities for electronic
booking of appointments.
The electronic transmission of prescriptions.
An underpinning IT infrastructure with
sufficient connectivity and broadband capacity
to meet future NHS needs.
Other projects are also mentioned, including a
“Picture Archive and Communications Systems
(PACS)”.
At the beginning of NPfIT, the budget was
estimated to be £6.2 billion. By 2007, the budget had
increased to over £12.4 billion (NHS, 2008). Its
value for money has often been called into question.
Hence the NPfIT authority published a Benefits
Statement for the year 2006/2007, attempting to
provide an account of the benefits and thus value of
the Programme (NHS, 2008). This is in response to a
government audit report calling for quantified
financial benefits and service improvements for the
programme (NAO, 2006; Collins, 2008).
The NPfIT has been subject to studies from other
perspectives (see e.g. Hendry et al., 2005; Currie &
Guah, 2007). This paper focuses on the programme
authority’s effort in assessing the value and benefits
of the programme through its publication of the
Benefits Statement 2006/2007.
3.2 The Benefits Statement for NPfIT
2006/2007
The NPfIT Benefits Statement 2006/2007 is the only
such statement available for the programme, despite
the fact that the programme has been in existence
A CRITIQUE OF THE BENEFITS STATEMENT 2006/2007 FOR THE UK NHS NATIONAL PROGRAMME FOR IT
483
since 2002. Though the NPfIT authority promised an
annual benefits statement in NHS (2008), no further
report was published in 2009 or 2010. It has been
reported that a draft benefits statement for
2007/2008 does exist (Collins, 2009) but is not
published. There are some benefits statements within
the sub-organizations of NHS but this paper limits
the considerations to NPfIT at the national level.
3.2.1 The Declared Methodology
NHS (2008) provides some details on its adopted
methodology for measuring benefits. The categories
of benefits are given as follows (p28):
cash releasing savings
other measurable benefits to which a financial
value can be attributed
non-measurable benefits which provide local
value.
This is a quite restrictive list of benefits to be
considered, though not entirely out of line with
recommendations from some sources (HM Treasury,
2003; Ward & Daniel, 2006; OGC, 2007). There are
other suggestions to categorise benefits. For
example, Farbey et al. (1992) suggested a scheme
with categories of strategic, tactical and operational
benefits (see also Love et al., 2005). The list of
benefits given by NHS (2008) might be regarded as
tactical and operational. There is no discussion of
strategic and “intangible” benefits in the report.
Even within such a restrictive list, NHS (2008)
only really reported the first category with little
attention paid to the others, as the benefits included
in the report are limited to:
“real savings and other benefits derived from
IT systems and services that have had time to
‘bed in’” (p28)
The report goes on further to clarify that:
“The inevitable time lag between benefits being
realised and evidence being collected and
analysed means that not all benefits realised
from that period have yet been reported.” (p28)
Therefore, NHS (2008) seems to have taken a
historical approach, only including those benefits
which are “real” and have been “realised”. Further,
the report claims that it is based on data from 20% of
the NHS organization involved in the NPfIT. It does
not explain how the sample organizations are
decided and how representative they are.
3.2.2 The Scope of the Programme
NHS (2008) reports roughly the same scope of the
programme as that given in NPfIT (2004) as shown
in Table 1. There is no obvious expansion or
reduction of the scope observed. Arguably, a change
of scope should be accommodated within a value-
based project evaluation methodology since the
increase of scope is theoretically associated with the
increase of cost, and vice versa.
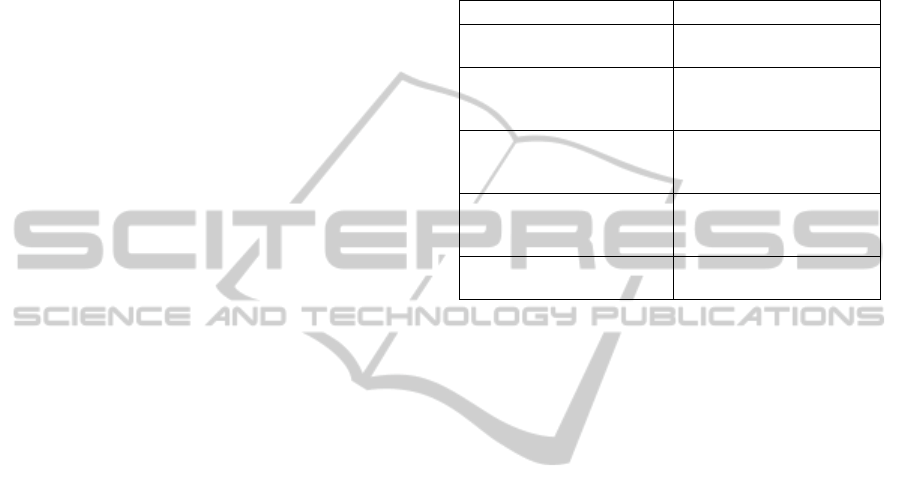
Table 1: Comparing the main programme elements
reported in NPfIT (2004) and NHS (2008).
NPfIT (2004) NHS (2008)
An electronic integrated
care records service
NHS Care Records
Service
Picture Archive and
Communications Systems
(PACS)
Picture Archiving
Communications
Systems (PACS)
The provision of facilities
for electronic booking of
appointments
Choose and Book
System
The electronic
transmission of
prescriptions
Electronic Prescription
Service
An underpinning IT
infrastructure
The National Network
for the NHS (N3)
3.2.3 The Cost
The overall budget for NPfIT is estimated to be
£12.4 billion by 2012. The Benefits Statement
reports a cumulated expenditure of £2.4 billion by
31 March 2007. This is about £2 billion less than the
predicted £4.5 billion (Collins, 2008). Cost is not the
focus of this paper and will not be discussed further.
3.2.4 The Benefits
NHS (2008) reported a figure of benefits totalling
£1,138.1 million. This is made up of three elements.
The first is the reported savings of £208.4 million to
31/03/2007. The second counts further seven years’
savings from 2007 to 2014 based on an annualised
figure of £119.1 million derived from the first
element. The third element is a further adjustment of
£96 million for the whole contract period due to “a
higher level of certainty based on the sample size”.
The explanation in NHS (2008) for this element is
no detailed. Suffice it to say that, while the previous
two elements are more based on evidence, this is
more an estimate, though there is no reason to
question its validity.
4 DISCUSSIONS
This section raises a number of issues regarding
NHS (2008) and its adopted methodology of benefits
assessment and reporting.
ICEIS 2011 - 13th International Conference on Enterprise Information Systems
484

4.1 The Feasibility of Value Assessment
There are clearly concerns on how feasible it is to
conduct a full assessment of the value contribution
of an information system to a business organization
(Remeni, 2000; Love et al., 2005). Common reasons
given include a) cost and benefits change and evolve
over time and some benefits tend to be intangible; b)
managers do not understand the importance of the
investment evaluation process or the concepts
involved; and c) organisational problems (such as
lack of time, management support, and
organisational structure) hindering the evaluation
process (Thomas et al., 2007). However, there are
likely to be more fundamental reasons. A piece of
equipment (e.g. an automated production line) in a
business represents an investment, just like many
projects. The value contributions of capital assets to
a business is captured at sales and are recorded in
the accounts as a whole, not always discernable for
each asset. The accounting system simply treats
capital assets as one of the inputs into an operational
black box. It is difficult to separate the contributions
made by each input. It is so difficult that it might be
counter-productive considering the cost involved.
The activity-based-costing (ABC) method is one
attempt to isolate value contributions from different
inputs. Its success has been rather limited (Katz,
2002; Agndal & Nillson, 2007). Even the ABC
method does not attempt to isolate the value
contributions from every input. It regards some
activities simply as “business sustaining” (Drury,
2007, p231). While further research should be
encouraged to see how the ABC method can help
evaluate projects, the cost and benefit of doing so
should be assessed at the same time.
However, a value assessment is compulsory at
the project initiation stage. Without a full value
assessment, how could any project investment
decision be taken? Even a “business sustaining”
investment has its attached value if we believe
everything can be measured (Hubbard, 2007). The
important thing is to document whatever assessment
assumptions and methodology used so that they may
be peer reviewed both before and after project go-
ahead decisions on a continuous basis.
It has to be acknowledged that with our current
understanding of the economics of information
(Remenyi, 2000), not all benefits can be
meaningfully separated from other sources of value
contributions and measured accordingly (HM
Treasury, 2003). In other words, the theory of
benefits measurement for IT investment is simply
not mature enough. For this reason, NHS (2008) is a
useful and courageous attempt.
4.2 The Baseline for Value Assessment
This section aims to address the question of how a
project assessment may be linked into the initial
business case (IBC). An IBC should provide a
baseline in terms of project scope, cost, time and
value propositions as well as project expenditure.
Assuming that the project sponsor is rational, the
estimated project value should exceed the total
project cost. In the language of Yu et al. (2005), the
initial estimated NPOV (V
0
) should exceed that of
NPEC (C
0
) in order that a project may be authorised
to proceed. It stands to reason that any assessment of
the project value should be benchmarked against V
0
.
However, this is not the case with NHS (2008), in
which the IBC is not mentioned. This is clearly an
oversight in NHS (2008), demonstrating the lack of
a clear conceptual framework within the NPfIT
authority in constructing the benefits statement.
There is a specifically documented overall business
case (NPfIT, 2004) and individual business cases for
constituent projects within the programme.
However, the IBC for the programme (NPfIT,
2004) is itself lacking in necessary details. In
addition to providing baseline value propositions, an
IBC should also make reference to a methodology
on assessing project benefits. The same
methodology should then be used at different project
stages to ensure consistency. The IBC for NPfIT
does not make reference to such a methodology.
4.3 Methodology of Assessment
Considering that NPfIT is undertaken within the UK
government where useful ideas for benefits
measurement have originated (HM Treasury, 2003;
OGC, 2007), the NPfIT authority could have made
use of readily available methodologies like HM
Treasury (2003). As a major government run
programme, there is really no need to re-invent a
methodology for benefits assessment. There is even
less excuse not to apply it when it is readily
available. It would be better of course for the
programme authority to have adapted guidelines in
HM Treasury (2003) to its circumstances. After all,
any large-scale programme has its specific
assumptions and circumstances that a general
methodology will not be able to cover. There is no
evidence that either the programme’s IBC (NPfIT,
2004) or its benefits statement (NHS, 2008)
articulated a coherent methodology of assessment.
A CRITIQUE OF THE BENEFITS STATEMENT 2006/2007 FOR THE UK NHS NATIONAL PROGRAMME FOR IT
485

4.4 The Actual vs. the Estimates
According to Yu et al. (2005), value assessment for
a product-based project may be undertaken at any
time, either during the project lifecycle or
afterwards. The earlier the assessment is undertaken,
the more it is based on estimates. The later it is in
the project-product lifecycle, the more it may be
based on actual evidence. Whenever the assessment
is undertaken, it is important to take account of both
the actually realised value and the future expected
value so that the sum total of the benefits may stay
relatively stable.
The evidence is that the authors of NHS (2008)
take a somewhat contradictory position in dealing
with this aspect of assessment. On the one hand,
NHS (2008) claims that it only includes those
benefits which are “real” and have been “realised”.
On the other hand, the report does extrapolate the
reported benefits to seven future years.
Following the suggestions above, the NPfIT
authority should have maintained an account of
“expected benefits”. As these benefits are realised,
they can be moved to an account of “realised
benefits”. The total of the two should stay more or
less stable.
4.5 Cost Savings vs. Value
Contributions
The figures reported in NHS (2008) are almost
exclusively based on “cash releasing savings”,
despite other acknowledged categories in its
methodology (see Section 3.2.1). While cost saving
may be relatively easy to count, it may not even be
the most important reason for undertaking a project.
Following an audit of NPfIT, NAO (2006)
acknowledged (p2):
“The Programme has the potential to generate
substantial benefits for patients and the NHS.
The main aim is to improve services rather than
to reduce costs.”
If the focus is restricted to cost savings and
neglects other benefits, it may easily lead to the
impression that the programme cost exceeds its
benefits when it may not be the case. This is what
happened with NHS (2008). With a programme
budgeted to cost £12.4 billion, the benefits statement
is only able to show benefits of £1.138 billion.
Compared with counting cost savings,
measuring “strategic” and “intangible” benefits of a
project is considerably more challenging. However,
it is not entirely impossible. In fact, NAO (2006)
provided helpful estimates of “patient safety benefits
expected from the Programme” (p26):
£2.5 billion as the human value of preventable
fatalities from medication errors arising from
inadequate information about patients and
medicines.
A large proportion of the £500 million spent
each year on treating patients who are harmed
by medication errors and adverse reactions.
A reduction in the payments by NHS Trusts
each year (approximately £430 million each
year) for settlements made on clinical
negligence claims.
Assuming the first figure is on an annual basis
like the other two, and further assuming that the
introduction of better information systems by NPfIT
can reduce these costs by 50%, the savings could
add up to £17.15 billion over 10 years. This is
considerably more than the cost savings reported in
NHS (2008). Patient safety is one of the reasons for
undertaking NPfIT according to its initiation
document (NPfIT, 2004). However, NHS (2008)
made no effort in quantifying these benefits.
5 CONCLUSIONS
With all the discussions of value and benefits based
approach for managing information technology
investments, few organizations publish a benefits
statement for an actual project or programme. For
this reason, NHS (2008) provides an excellent
opportunity for us to see a large-scale IT-based
change programme’s value assessment in practice.
This is particularly so since NHS (2008) was
produced within an environment where the thinking
on benefits management and “value for money” is
strongly advocated (HM Treasury, 2003; NAO,
2006; OGC, 2007). However, NHS (2008) as a
benefits statement is defective for a number of
reasons. First of all, an important underlying reason
is perhaps that the theory of benefits measurement
for IT investment is simply not mature enough.
However, it is useful for NPfIT to publish such a
statement so that lessons can be learned from it.
Secondly, despite all the discussions of value
management and benefits assessment, the NPfIT
programme was started without a baseline value
proposition or a value assessment methodology
specified in the initial business case. Thirdly, while
the NPfIT authority does not have its own
methodology, it failed to make a good use of a
centrally prescribed methodology by the UK
government. As a result, NHS (2008) focused on a
ICEIS 2011 - 13th International Conference on Enterprise Information Systems
486

narrow range of benefits, missing the opportunity of
providing a proper account of the value propositions
of the programme. The report even ignored specific
estimates suggested by the government’s audit
office. Most if not all of these defects can be
attributed to the lack of a coherent conceptual
framework for project value assessment in the NPfIT
authority.
REFERENCES
Agndal, H. and Nilsson, U. (2007) Activity-based costing:
effects of long-term buyer-supplier relationships,
Qualitative Research in Accounting Management, vol.
4, no. 3, pp222-245.
Collins, T. (2008) NPfIT spending £1.5bn less than
expected._http://www.computerweekly.com/blogs/pub
lic-sector/2008/03/npfit-spending-15bn-less-than.html.
Collins, T. (2009) Ministers sit on draft NPfIT report,
http://www.computerweekly.com/blogs/public-
sector/2009/09/ministers-may-sit-on-draft-npf.html.
Currie, W. L. and Guah, M. W. (2007) Conflicting
institutional logics: a national programme for IT in the
organisational field of healthcare, Journal of
Information Technology, vol. 22, pp235-247.
Doherty, N. F., Dudhal, N., Coombs, C., Summers, R.,
Vyas, H., Hepworth M. and Kettle, E. (2008)
Towards an Integrated Approach to Benefits
Realisation Management – Reflections from the
Development of a Clinical Trials Support System, The
Electronic Journal of Information Systems Evaluation,
vol. 11 (2), pp. 83-90.
Drury, C. (2007) Management and Cost Accounting,
Cengage Learning.
Farbey, B., Land, F. and Targett, D. (1992) Evaluating
investments in IT, Journal of InformationTechnology,
vol. 7, pp109-122.
Hendy, J. and Reeves, B. C. and Fulop, N. and Hutchings,
A. and Masseria, C. (2005) Challenges to
implementing the National Programme for
Information Technology (NPfIT): a qualitative study.
British medical journal, 331 (7512). pp. 331-336.
HM Treasury (2003) Appraisal and Evaluation in Central
Government. HM Treasury.
Hubbard, D. W. (2007) How to Measure Anything:
Finding the Value of ''Intangibles'' in Business, Wiley.
Katz, D. M. (2002) Activity-Based Costing,
http://www.cfo.com/article.cfm/3007694.
Lin, C. and Pervan, G. (2003) The practice of IS/IT
benefits management in large Australian
organizations, Information & Management, 41 (1),
pp13-24.
Love, P. E. D., Irani, Z., Standing, C., Lin, C. and Burn, J.
M. (2005) The enigma of evaluation: benefits, costs
and risks of IT in Australian small-medium-sized
enterprises, Information & Management, vol. 42, no.
7, pp947-964.
NAO (2006) The National Programme for IT in the NHS.
HC 1173, Session 2005-2006, The National Audit
Office, London.
NHS (2008) National Programme for IT in the NHS:
Benefits Statement 2006/07, National Health Service,
http://webarchive.nationalarchives.gov.uk/200808211
11207/http://www.connectingforhealth.nhs.uk/about/b
enefits/statement0607.pdf.
NPfIT (2004) National Programme Initiation Document,
NHS National Programme for IT.
OGC (2007) Managing successful programmes, 3rd edn,
Office of Government Commerce, Stationery Office.
Remenyi, D. (2000) The elusive nature of delivering
benefits from IT investment, Electronic Journal of
Information Systems Evaluation, vol. 3, no. 1, pp1-10.
Remenyi, D. and Sherwood-Smith, M. (1999) Maximise
information systems value by continuous participative
evaluation, Logistics Information Management, vol.
12, no. 1, pp14-31.
Shenhar, A. J., Dvir, D., Levy, O. and Maltz, A. C. (2001)
Project Success: A Multidimensional Strategic
Concept, Long Range Planning, vol. 34, no. 6, pp699-
725.
Thiry, M. (2002) Combining value and project
management into an effective programme
management model, International Journal of Project
Management, vol. 20, no. 3, pp221-227.
Tohidi, H. (2011) Review the benefits of using value
engineering in information technology project
management, Procedia Computer Science, vol. 3,
pp917-924.
Thomas, G., Seddon, P. B. and Fernandez, W. (2007) IT
Project Evaluation: Is More Formal Evaluation
Necessarily Better? PACIS 2007 Proceedings.
Winter, M. and Szczepanek, T. (2008) Projects and
programmes as value creation processes: A new
perspective and some practical implications,
International Journal of Project Management, vol. 26,
no. 1, pp95-103.
Ward, J. & Daniel, E. (2006) Benefits management:
delivering value from IS & IT investments. Wiley.
Yu, A. G., Flett, P. D. and Bowers, J. A. (2005)
Developing a value-centred proposal for assessing
project success, International Journal of Project
Management, vol. 23, no. 6, pp428-436.
A CRITIQUE OF THE BENEFITS STATEMENT 2006/2007 FOR THE UK NHS NATIONAL PROGRAMME FOR IT
487
