
MUSCLE ACTIVATION THRESHOLDS BEFORE
AND AFTER TOTAL KNEE ARTHROPLASTY
Protocol of a Randomized Comparison
of Minimally Invasive vs. Standard Approach
Carlos J. Marques
1, 2
, Hugo Gamboa
4
, Frank Lampe
3
, João Barreiros
1
and Jan Cabri
5
1
Faculty of Human Kinetics, Technical Universitty of Lisbon, Lisbon, Portugal
2
Physikal Therapy and Rehabilitation Department, ENDO-Klinik Hamburg, Hamburg, Germany
3
Joint Replacement Center, Schön Klinik Hamburg-Eilbek, Hamburg, Germany
4
Physics Department, Sciences and Technology Faculty, New University of Lisbon, Lisbon, Portugal
5
Department of Physical Performance, Norwegian School of Sport Sciences, Oslo, Norway
Keywords: Total knee replacement, Minimally invasive surgery, Brake response time, Reaction time, Automobile
driving, Muscle activation thresholds.
Abstract: After total knee arthroplasty (TKA) patients often ask when they can resume car driving. This question was
the aim of some studies in the past, however it is not clear whether minimally invasive surgery (MIS) for
total knee replacement has benefits in terms of faster recovering times. With the present study protocol the
effects of two surgery techniques for TKA (MIS vs. standard approach) on motor performance parameters
will be tested during the performance of an emergency brake in a car simulator. The brake response time
components and the muscle activation thresholds of four muscles involved in the task will be the outcomes
of the study.
1 INTRODUCTION
Minimal invasive surgery (MIS) for total knee
arthroplasty (TKA) has been used for several years
as an alternative to standard approaches. Different
MIS techniques have been described in the literature
(Laskin, 2003): mini-arthrotomy, mini-midvastus
(Floren et al., 2008, Haas et al., 2006), medial
squad-sparing and mini-subvastus (Schroer et al.,
2008). Supporters of MIS techniques go from the
assumption that a smaller soft tissue injury with a
reduction of the muscle quadriceps lesion leads to a
faster rehabilitation with better early functional
outcomes, less pain and shorter stay duration. Critics
fear a reduction of the intra-operative overview with
consecutive failure especially in relation to the
alignment of the prosthesis.
After TKA patients frequently ask when they can
resume car driving. Five studies on this topic were
published in the past years (Spalding et al., 1994,
Pierson et al., 2003, Marques et al., 2008b, Marques
et al., 2008a, Dalury et al., 2010). All studies
investigated the effects of TKA on brake response
time (BRT), an important human factor used in
traffic accident prevention and research. The results
of the studies document a BRT increase after right
TKA. The time frame needed for the BRT to return
to preoperative values varied among the studies and
ranged from 8 (Pierson et al., 2003) to 4 weeks
(Dalury et al., 2010). In a study by Dalury and
colleagues (2010), where the patients were
submitted to “contemporary TKA with less tissue
disruption”, the BRT of all patients returned to
preoperative values 4 weeks after surgery. A small
group of patients reached the preoperative values
already 2 weeks after surgery.
The aim of this randomized controlled trial is to
study the effects of two surgical technics used for
TKA (MIS vs. standard approch) on motor
performance parameters such as brake response time
(BRT), reaction time (RT), foot transfers time
(FTT), brake pedal traveling time (BPTT) and the
activation thresholds of four muscles of the right leg
during the performance of a emergency brake in a
car simulator.
544
Marques C., Gamboa H., Lampe F., Barreiros J. and Cabri J..
MUSCLE ACTIVATION THRESHOLDS BEFORE AND AFTER TOTAL KNEE ARTHROPLASTY - Protocol of a Randomized Comparison of Minimally
Invasive vs. Standard Approach .
DOI: 10.5220/0003318505440547
In Proceedings of the International Conference on Bio-inspired Systems and Signal Processing (BIOSIGNALS-2011), pages 544-547
ISBN: 978-989-8425-35-5
Copyright
c
2011 SCITEPRESS (Science and Technology Publications, Lda.)
2 METHODS AND MATERIALS
2.1 Study Design
To study the effects of both surgical techniques on
the study variables a randomized controlled trial
with one between-subject factor (intervention group:
MIS and Standard) and one within-subject factor
(time: one day before and 8 days, 30 and 40 days
after surgery) was designed. After consent to
participate, the patients will be randomly assigned to
a group
(MIS or Standard approach).
The study protocol was approved by the Ethics-
Committee of the Federal State of Hamburg,
Germany (Project Nr.: PV3349). The trial
registration number at the German Clinical Trial
Database (DRKS) is: DRKS00000552.
2.2 Patient Selection
The patient selection will take place at the Schön
Klinik Hamburg-Eilbek in Hamburg, Germany. The
patients arriving at the clinic for elective right TKA
will be asked if they are car drivers. If the patient
drives regularly (at least once a week) he/she will be
informed about the study and asked to participate.
2.2.1 Inclusion Criteria
Indication for TKA of the right knee;
The patient is an active driver;
Consent to participate in the study.
2.2.2 Exclusion Criteria
Body Mass Index > 40 Kg/m
2
;
Valgus or Varus deformity > 20°;
Range of Motion < 75°;
Neurological disorders such as Parkinson’s
disease;
Rheumatoid arthritis.
2.2.3 Sample Size
A sample size of 2x25 Patients will be aimed.
2.3 The Car Simulator
The car simulator was made based on a European
middle class car. It was used during two previous
studies (Marques et al., 2008a, Marques et al.,
2008b) and was now equipped with new
instruments.
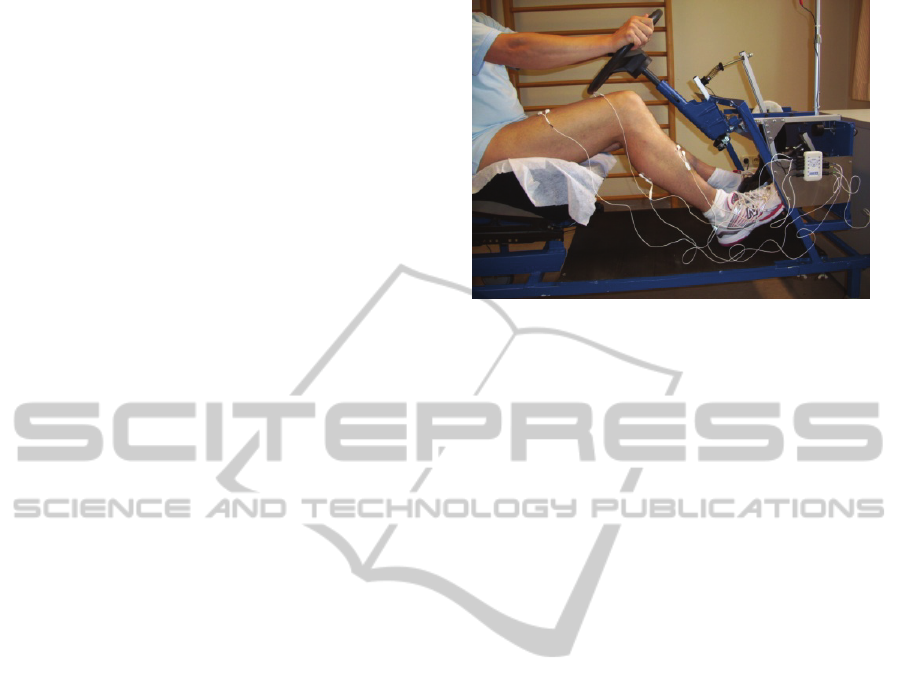
Figure 1: Car simulator with BioPlux Research system.
2.3.1 Instruments / Equipment
The data acquisition system consists of a BioPlux
Research system with wireless connectivity via
Bluetooth (PLUX –wireless biosignals). A trigger
will be used to command the stimulus light (red
LED) turn on/off. Two load cells are connected with
both pedals (break and accelerator). Four surface
electromyography (sEMG) signals will be acquired
from 4 muscles involved in the task. The following
acquisition channels will be used:
Channel 1: Trigger
Channel 2: Load cell of the accelerator
Channel 3: Load cell of the brake pedal
Channel 4: sEMG M. rectus femoris
Channel 5: sEMG M. vastus medialis
Channel 6: sEMG M. tibialis anterior
Channel 7: sEMG M. gastrocnemius
The channel sample rate will be set at 1000Hz.
2.3.2 Electrode Type and Position
Surface EMG signals will be recorded using silver-
silver chloride (Ag/AgCl) pre-gelled electrodes
(MultiBiosensors). The electrode locations will be
found via palpation of the subjects anatomy over the
appropriate muscle belly, according to the
recommendations of the European SENIAM-Project
(Surface Electromyography for Non-Invasive
Assessment of Muscles). Electrode sites will be
shaved, abraded and cleaned with isopropyl alcohol
to reduce impedance.
MUSCLE ACTIVATION THRESHOLDS BEFORE AND AFTER TOTAL KNEE ARTHROPLASTY - Protocol of a
Randomized Comparison of Minimally Invasive vs. Standard Approach
545
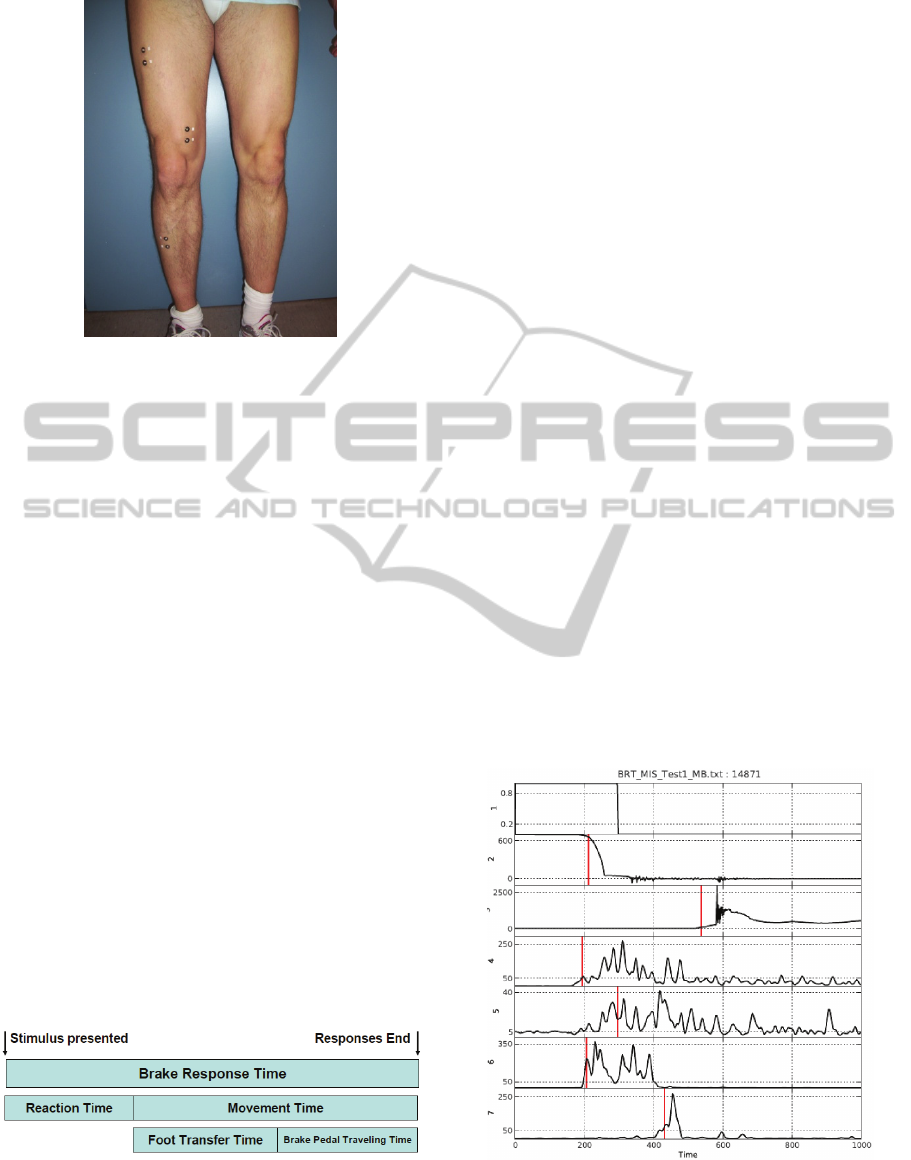
Figure 2: Electrode position.
2.4 Study Outcomes
The brake response time (BRT) is a very important
human factor in accident prevention research. The
BRT can be fractionated in several components. The
primary outcomes of this research project are
components of the BRT and are defined below.
2.4.1 Primary Outcomes
Brake Response Time (BRT): time frame
between the onset of the red LED and the achieving
of a brake force on the brake pedal of 100N (ms);
Reaction Time (RT): time frame between the
onset of the red LED and the initiation of the
movement of the foot on the accelerator pedal (ms);
Foot Transfer Time (FTT): time frame between
the initiation of the movement of the foot on the
accelerator pedal and the first contact with the brake
pedal (ms);
Brake Pedal Travelling Time (BPTT): time
frame between the first contact with the brake pedal
and the achieving of a brake force of 100N on the
brake pedal (ms);
Movement Time (MT): sum of the FTT and
BPTT.
Figure 3: Brake response time components
2.4.2 Secondary Outcomes
The secondary outcomes are the time frames
between the onset of the red LED and the muscle
activation thresholds of the above referred muscles.
3 DATA EXTRACTION
AND ANALYSIS
The patients will perform 10 emergency brake test
trials in a simple task, followed by 10 emergency
brake test trials in a more complex task in a car
simulator. The data of the 10 test trials on each task
(simple and complex) will be saved separately as
text files with the use of the software program
Monitor Plux.
3.1 Data Extraction
The signals collected are of three types: digital
signal (from the light trigger); force signals from the
accelerator and brake pedal load cells; and sEMG
signals from four muscles.
The digital signal is used to slice the signals in
the 10 breaks in each of the tasks. The force signals
are calibrated considering that in the initial instant
the foot is not pressing any of the pedals and the
acquired value in the initial 100ms is considered the
zero of the load cells. This signal is low pass filtered
with cut frequency at 10Hz with a 4
th
order
Butterworth IIR filter.
Figure 4: Graphic of one test trial in the simple task with
the 7 channels (1 Trigger; 2 Accelerator; 3 Brake pedal; 4-
7 sEMG signals of the 4 muscles) and the red lines
marking the detected thresholds for each signal.
BIOSIGNALS 2011 - International Conference on Bio-inspired Systems and Signal Processing
546

The sEMG signals are filtered with an envelope
detector that consists of a low pass filter of 5 Hz
(Butterworth IIR filter 4
th
order) after computing the
absolute value.
An adaptation of the Hodges onset detector
(Hodges and Bui, 1996) was created to be used on
force and sEMG signals on positive or negative
transitions.
3.2 Data Analysis
Mean values of the ten test trials for each task will
be calculated for each subject. A 2x4 ANOVA for
repeated measures will be performed to detect
differences within a surgery group along the time
and between the two groups (MIS vs. standard) at
each assessment day. Multiple comparisons will be
made with paired t tests using the Bonferroni
adjustment of alpha. All statistical tests will be
carried out using the SPSS software. For all
statistical tests, the .05 level of probability will be
accepted as the criterion for statistical significance.
4 DISCUSSION
The available evidence on which physicians and
doctors can relay when advising patients on when
they should resume car driving after TKA is few.
The components of BRT were investigated in 4
studies (Spalding et al., 1994, Marques et al., 2008b,
Marques et al., 2008a, Dalury et al., 2010). Ten days
after TKA central aspects related with stimulus
perception, response selection and response
initiation seem not to be affected, once RT was not
changed (Marques et al., 2008a, Marques et al.,
2008b). TKA seems to affect peripheral aspect
related to the execution of the movement. The soft
tissue lesion may be the cause of such performance
decreases after TKA.
In the past years minimally invasive approaches
for TKA have been used. The question whether a
smaller tissue lesion will improve the performance
of the patients will be investigated in this study.
The results of this study will increase the body of
evidence on this issue and will add a comparison of
two surgical techniques with a more detailed view
over the brake response time components and over
the effects of TKA on neuromuscular function of
four muscles involved in the task.
ACKNOWLEDGEMENTS
We thank the Technical Department at the Schön
Klinik Hamburg-Eilbek for the technical changes
and adaptations made in the car simulator.
REFERENCES
Dalury, D. F., Tucker, K. K. and Kelley, T. C. (2010) Clin
Orthop Relat Res.
Floren, M., Reichel, H., Davis, J. and Laskin, R. S. (2008)
Oper Orthop Traumatol, 20, 534-43.
Haas, S. B., Manitta, M. A. and Burdick, P. (2006) Clin
Orthop Relat Res, 452, 112-6.
Hodges, P. W. and Bui, B. H. (1996) Electroencephalogr
Clin Neurophysiol, 101, 511-9.
Laskin, R. S. (2003) Clin Orthop Relat Res, 151-3.
Marques, C. J., Barreiros, J., Cabri, J., Carita, A. I.,
Friesecke, C. and Loehr, J. F. (2008a) Knee, 15, 295-8.
Marques, C. J., Cabri, J., Barreiros, J., Carita, A. I.,
Friesecke, C. and Loehr, J. F. (2008b) Arch Phys Med
Rehabil, 89, 851-5.
Pierson, J. L., Earles, D. R. and Wood, K. (2003) J
Arthroplasty, 18, 840-3.
Schroer, W. C., Diesfeld, P. J., Reedy, M. E. and LeMarr,
A. R. (2008) J Arthroplasty, 23, 19-25.
Spalding, T. J., Kiss, J., Kyberd, P., Turner-Smith, A. and
Simpson, A. H. (1994) J Bone Joint Surg Br, 76, 754-
6.
MUSCLE ACTIVATION THRESHOLDS BEFORE AND AFTER TOTAL KNEE ARTHROPLASTY - Protocol of a
Randomized Comparison of Minimally Invasive vs. Standard Approach
547
