
ENVISIONING uHEALTH
An Ontological Framework
Arkalgud Ramaprasad and Shazia A. Sathar
University of Illinois at Chicago, Chicago, IL 60607, U.S.A.
Keywords: uHealth, Ontology, eHealth.
Abstract: Ubiquitous health care (uHealth) is becoming feasible today, more so than ever before, due to rapid
advances in information technology. We can glimpse its possibilities in the care of the wounded in war and
the diagnosis and treatment of diseases from a distance. However, the visions of uHealth are many and
partial, ill-defined and unclear. We present a set of four ontologies to envision uHealth systemically. The
ontologies deconstruct uHealth into spatial, temporal, and semiotic ubiquity. Each aspect of ubiquity is
further deconstructed into three components. These ontologies can be used to construct a comprehensive
natural-language narrative of uHealth. They can also be used to (a) map the states-of-the-potential, art, and -
practice of uHealth, and (b) systematically design the trajectory for the transformation to uHealth.
1 INTRODUCTION
Health care at its core is an interaction based on
extensive information transportation and translation
– from the patient to the provider, from the provider
to the patient, from within the patient to the
diagnostician (for example, endoscopy), from the
researcher to the clinician, from the provider to the
insurer, from the provider to the pharmacist, and so
on (Ramaprasad, Papagari, & Keeler, 2009;
Ramaprasad, Valenta, & Brooks, 2009). In
combination with the internet – a revolutionary
information transportation system, evolving into a
translation system with the semantic web – there
have emerged many new alternatives to traditional
face-to-face health care. The new visions of health
care seek to transform the processes and outcomes
of traditional health care.
Pervasive health care, for example, is defined as
“healthcare to anyone, anytime, and anywhere by
removing locational, time and other restraints while
increasing both the coverage and the quality. The
pervasive healthcare applications include pervasive
health monitoring, intelligent emergency
management system, pervasive health- care data
access, and ubiquitous mobile telemedicine.”
(Varshney, 2007, p. 113) In a similar vein u-Health
is defined as “ubiquitous health care, health
management and medical services anytime
anywhere.” (Kugsang, Eun-young, & Dong Kyun,
2009, p. 829) Earlier in the development of these
concepts eHealth was defined as “the use of
emerging information and communication
technology, especially the Internet, to improve or
enable health and health care.” (Eng, 2001) Another
variation of the concept is m-Health, the use of
“mobile computing, medical sensor, and
communications technologies for health-care.”
(Istepanian, Jovanov, & Zhang, 2004, p. 405).
Related to the above broad visions of health care
are a number of capabilities envisaged because of
advances in information technology. The following
are some examples. The Bank of Health wherein
“[t]hrough a health “ATM” system what would
work like banking ATMs, the consumer will have
secure, private, and global access to a healthcare
“checking account” containing information like
blood types, medications, and personal family
medical histories.” (Ball & Lillis, 2001, p. 6)
Bardram envisages “a context-awareness
infrastructure in place in a hospital that various
clinical applications can access and use to adapt to
the context in which they are currently running…a
context-aware Electronic Patient Record (EPR), a
context-aware pill container, and a context-aware
hospital bed.” (Bardram, 2004, p. 1574) Intelligent
Biomedical Clothing (IBC) could weave together
“textile fibers, biomedical sensors and wireless and
411
Ramaprasad A. and Sathar S..
ENVISIONING uHEALTH - An Ontological Framework.
DOI: 10.5220/0003290004110416
In Proceedings of the International Conference on Health Informatics (HEALTHINF-2011), pages 411-416
ISBN: 978-989-8425-34-8
Copyright
c
2011 SCITEPRESS (Science and Technology Publications, Lda.)

mobile telecommunications” (Lymberis & Olsson,
2003, p. 379) Intelligent agents could actively sense
and gather “information across the [health care]
delivery network….” (Weagraff, 2005, p. 3) Further
they “could provide care themselves….act on behalf
of the enterprise to correct faults or provide
information in a proactive manner….” (Weagraff,
2005, p. 3).
Each of the many visions of future health care
represents a part of the potential. In the parable of
the six blind men and the elephant, each man
experiences a part of the elephant and infers an
incorrect image of the whole. The real elephant
remains invisible to all of them (Ramaprasad, 2009)
until a wise man integrates the image of the whole
from the parts. Similarly, today the ‘elephant’ called
uHealth remains invisible. The objective of this
paper is to make it visible. We present an
ontological method to envision the complexity of
uHealth concisely and comprehensively, using
natural English, and at different levels of
granularity. It is a method to envision the whole, the
parts, and the relationship between the two.
2 ONTOLOGY OF uHEALTH
2.1 Ontology of eHealth
The proposed ontology of uHealth is based on the
ontology of eHealth (Ramaprasad, Papagari et al.,
2009) shown in Figure 1. It encapsulates the
definition of eHealth as ‘transporting information to
transform health care.’ The five axes of the ontology
are information, spatial transportation, temporal
transportation, semiotic transportation, and heath
care. Each axis is defined by a taxonomy (one- or
two-level) of attributes. The axes are presented left
to right in Figure 1 with connecting words/phrases
between the columns.
A natural language descriptor of eHealth can be
concatenated by combining a category from each
column with the connecting words/phrases
(Ramaprasad, Papagari et al., 2009). For example:
• Transporting personal health information intra-
enterprise locally in real time as data to transform
outcomes of wellness.
• Transporting medical research information inter-
enterprise nationally in advance as action to
transform outcomes of illness.
• Transporting business financial intra-enterprise
regionally in real time as data to transform
management of revenue.
Ubiquity in health care is a combination of spatial,
temporal, and semiotic ubiquity. We will extend the
eHealth ontology to uHealth by including the
corresponding axes and desconstructing them
further into three components.
2.2 Ontology of uHealth
A colloquial expression for ubiquity is ‘any-place,
any-time’; it connotes spatial and temporal ubiquity.
To these two commonly used axes of ubiquity we
add the third axes of semiotic ubiquity – ‘any-
information’. It connotes the complete semiotic
cycle (Ramaprasad & Rai, 1996) – the
morphologics, syntactic, semantics, and pragmatics
of the generation and application of information.
Thus, we define uHealth as ‘transporting
information ubiquitously – spatially, temporally, and
semiotically – to transform health care.’ The
corresponding ontology is shown in Figure 2. The
Information and Health Care axes are the same as in
the eHealth ontology; the third (middle) axis is
Ubiquity is new and includes the three categories of
ubiquity.
The following are six of the 36 basic
connotations of uHealth which can be derived from
the ontology, each with an example.
1. Transporting personal information spatially
ubiquitously to transform health care outcomes.
For example, having a person’s emergency
contact information available anywhere.
2. Transporting medical information temporally
ubiquitously to transform health care outcomes.
For example, having a person’s prescription
information available anytime.
3. Transporting business information temporally
ubiquitously to transform health care quality.
For example, knowing a clinic’s complete
billing history to determine potential fraud.
4. Transporting personal information semiotically
ubiquitously to transform health care quality.
For example, interpreting socio economic data
to tailor treatment plan.
5. Transporting medical information semiotically
ubiquitously to transform health care quality.
For example, interpreting genetic information to
tailor drug treatment individually (Eichelbaum,
Ingelman-Sundberg, & Evans, 2006).
HEALTHINF 2011 - International Conference on Health Informatics
412
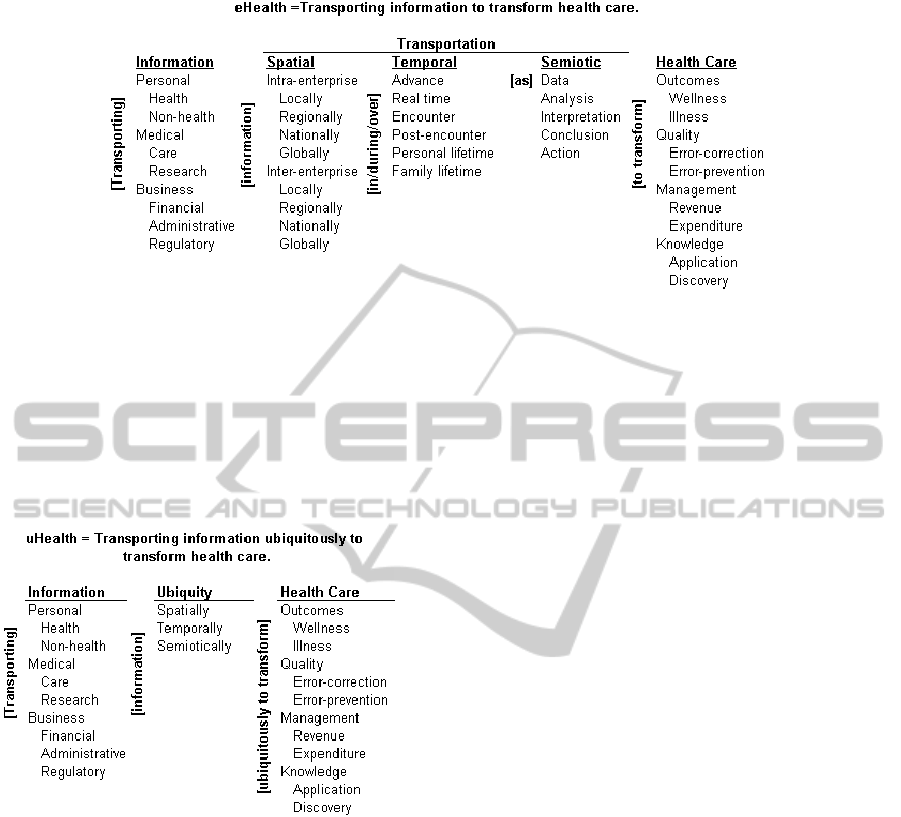
Figure 1: Ontology of eHealth.
6. Transporting personal information semiotically
ubiquitously to transform health care
knowledge. For example, recommending
actions based on knowledge of personal and
family demographic history.
We can refine the concepts of spatial, temporal, and
semiotic ubiquity further as discussed below.
Figure 2: uHealth Ontology.
2.3 Ontology of Spatial Ubiquity
The concept of spatial ubiquity can be deconstructed
into three components, namely: spatial distribution,
spatial range, and spatial locus. These three are
shown as separate axes in Figure 3. The figure
articulates the statement ‘transporting information
spatially ubiquitously to transform health care’. The
Information and Health care axes of the ontology are
the same as in Figures 1 and 2.
Spatial Distribution describes the density of the
ubiquity. At the lower extreme ubiquity may be
defined by the ability to transport information
from/to fixed locations. As long as the relevant fixed
locations are covered one could describe the system
as being minimally ubiquitous. For example, as long
as all the clinics of a health care provider are
covered, a system may be described as being
ubiquitous. At the upper extreme ubiquity may be
defined as the ability to transport information
from/to a continuous space. Thus, the requirement
for ubiquity may be anywhere in the geographical
region covered by the clinics. Between these two
extremes spatial distribution may be defined by
networked points or mobile points from/to where
information has to be transported.
Spatial Range describes the scale of the ubiquity.
The ubiquity may be at a very close range; for
example, within a hospital room. Or, it may be at a
remote range; for example, anywhere within a city,
region, or country.
Spatial Locus describes the focus or origin of
ubiquity. It may be any one or a combination of the
health care providers listed in Figure 3. It may also
be described differently in terms of the facilities
such as clinics, hospitals, etc.
Combining Spatial Distribution and Spatial
Range, spatial ubiquity may range from fixed points
at a very close range to continuous points at remote
range. Further combining it with Spatial Locus, the
technology required for transporting information
from/to fixed points at very close range from/to
patient would be different from that for transporting
information from/to continuous points at remote
range from/to patients. Thus, spatial distribution,
range, and locus can impose different requirements
on a uHealth system.
2.4 Ontology of Temporal Ubiquity
The concept of temporal ubiquity can be
deconstructed into three components, namely:
temporal interval, temporal range, and temporal
locus. These three are shown as separate axes in
ENVISIONING uHEALTH - An Ontological Framework
413
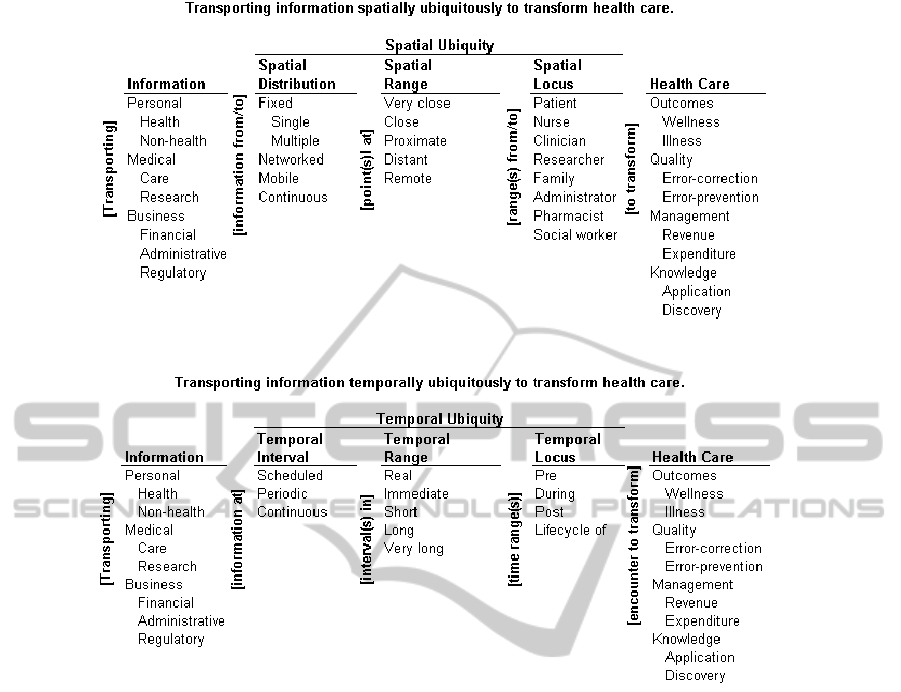
Figure 3: Ontology of spatial ubiquity.
Figure 4: Ontology of temporal ubiquity.
Figure 4. The figure articulates the statement
‘transporting information temporally ubiquitously to
transform health care’. The Information and Health
care axes of the ontology are the same as in Figures
1 and 2.
Temporal Interval describes the frequency of
transportation of information. It ranges from the
Scheduled through Periodic to Continuous.
Scheduled transportation would be the least
ubiquitous temporally, Continuous the most. The
temporal interval for transportation would be
determined by the temporal characteristics of the
information. Scheduled ubiquity may be adequate
for a low frequency or unchanging information such
as weight and height; Continuous ubiquity may be
necessary for high frequency information such as a
heart monitor from an ambulance.
Temporal Range describes the period over which
information has to be transported for uHealth. Real
time anchors the low end of the axis; Very long
periods, which may be as long as a person’s life time
or even a family’s lifetime (in the case of certain
genetically inherited diseases), anchors the high end
of the axis. Between the two anchors are three
categories labeled Immediate, Short, and Long. The
clock-time equivalents of these ranges may vary
between contexts. Real time range for lifestyle
change may be Very long range for chronic heart
failure.
Temporal Locus describes the location of the
temporal range relative to an encounter. It ranges
from Pre (before) the encounter to During, Post, and
the Lifecycle of the encounter. For transient events
such as a common infection the locus may be just
during the encounter; on the other hand, for a
chronic condition such as diabetes it would have to
be during the Lifecycle of the disease.
Combining Temporal Interval and Temporal
Range, temporal ubiquity may range from
Scheduled intervals in Real time range to
Continuous interval in Very long time range. Further
combining it with Temporal Locus, the technology
required for transporting information at scheduled
intervals in real time range Pre encounter would be
HEALTHINF 2011 - International Conference on Health Informatics
414
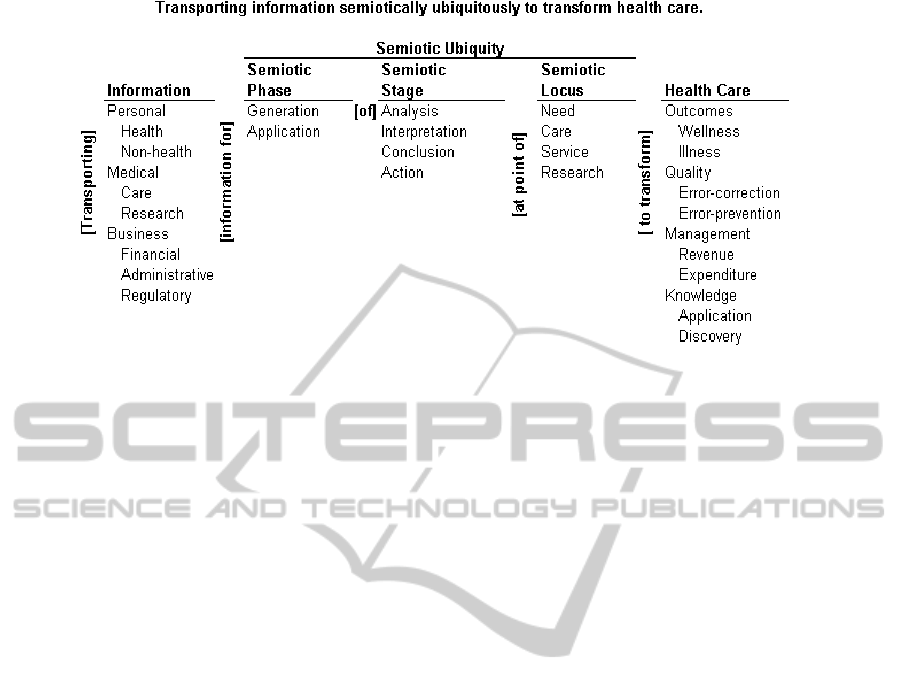
Figure 5: Ontology of Semiotic Ubiquity.
different from that for transporting information at
Continuous interval in Very long time range for the
Lifecycle of the encounter. Thus temporal interval,
range, and locus can impose different requirements
on a uHealth system.
2.5 Ontology of Semiotic Ubiquity
The concept of semiotic ubiquity can be
deconstructed into three components, namely:
Semiotic Phase, Semiotic Stage, and Semiotic
Locus. These three are shown as separate axes in
Figure 5. The figure articulates the statement
‘transporting information semiotically ubiquitously
to transform health care’. The Information and
Health Care axes are the same as in Figures 1 and 2.
Semiotic Phase describes the two broad phases
of the semiotic cycle, Generation and Application of
information(Ramaprasad & Rai, 1996). Repeated
completion of both phases is necessary for
translating information into action and obtaining
information about action (Ramaprasad, Valenta et
al., 2009). Clinical research, for example, may focus
more on the Generation of information; clinical
practice, on the Application of information.
Similarly, continuous monitoring devices may focus
primarily on the ubiquitous Generation of
information with a small component of Application
to discover potential emergency alerts. An aspect of
semiotic ubiquity is the inclusion of both phases.
Semiotic Stage describes the four broad stages of
the semiotic cycle: Analysis, Interpretation,
Conclusion, and Action. The first three correspond
to the commonly used syntactics, semantics, and
pragmatics (Ramaprasad & Rai, 1996) categories.
The value of information is enhanced at each stage.
The full value of information is realized only when
the cycle is complete. An aspect of semiotic ubiquity
is the completion of all the four stages.
Semiotic Locus describes the location of the
semiotic process. It may be at the point of Need,
Care, Service, or Research. Other locations may be
added to the list. The Semiotic Locus may also
include multiple locations. Ideally, uHealth would
entail the ability to complete the semiotic cycle from
any locus – the ability to translate information at any
place and time.
Combining Semiotic Phase and Semiotic Stage,
Semiotic Ubiquity would include Generation and
Application of Analysis, Interpretation, Conclusion,
and Action. The integration of these at any Locus
would be the objective of Semiotic Ubiquity. The
practice of evidence based medicine, for example,
requires the ability to transport Medical information
for Generation/Application of Interpretation,
Conclusion, and Action at the point of Care.
3 CONCLUSIONS
Ubiquity is polymorphic. Thus the meaning of
uHealth can vary by the context and the
corresponding needs. The ability to access one’s
electronic medical records (EMR) in any physician’s
office in a geographical region may be the state-of-
the-need of ubiquity in a developed country. On the
other hand, the ability to access a physician within
half a day’s travel by foot may be the state-of-the-
need in a developing country. A physician practicing
evidence based medicine (EBM) may desire
semiotic ubiquity at the point of care through access
to online reviews, journals, and decision support
ENVISIONING uHEALTH - An Ontological Framework
415

tools. A physician practicing in a remote village may
be content to collect the data from the patient and
send it by snail-mail for analysis, interpretation, and
action to a specialized tertiary care hospital.
Effective strategies are systemic and systematic
responses to a problem. For uHealth, they have to be
based on the integrated image of the whole
‘elephant’ called uHealth, not on fragmented images
of its parts. If uHealth strategies are to be effective
in the new internet age, they have to be designed,
developed, and implemented systematically in the
context of the particular health care system. Ad hoc,
fragmented strategies will be ineffective.
The ontological framework for conceptualizing
uHealth discussed in this paper provides a language
and logic for designing and developing a coherent
uHealth strategy. The framework can be used to map
the states-of-the-art, -need, and –practice; and from
these maps to assess the gaps between the states and
determine strategies to bridge the gaps. The
ontologies can be adapted to a context by changing
the axes and taxonomies accordingly. Thus, one can
envision the trajectory of transformation from
traditional health to uHealth in the age of the new
internet – perhaps the age of the Übernet.
REFERENCES
Ball, M. J., & Lillis, J. (2001). E-health: transforming the
physician/patient relationship. International Journal of
Medical Informatics, 61(1), 1-10.
Bardram, J. (2004). Applications of context-aware
computing in hospital work: examples and design
principles. Paper presented at the SAC '04, Nicosia,
Cyprus.
Eichelbaum, M., Ingelman-Sundberg, M., & Evans, W.
(2006). Pharmacogenomics and individualized drug
therapy. Annual Review of Medicine, 57, 119-137.
Eng, T. R. (2001). The eHealth Landscape: A Terrain
Map of Emerging Information and Communication
Technologies in Health and Health Care: Princeton,
NJ: The Robert Wood Johnson Foundation.
Istepanian, R. S. H., Jovanov, E., & Zhang, Y. T. (2004).
Guest Editorial Introduction to the Special Section on
M-Health: Beyond Seamless Mobility and Global
Wireless Health-Care Connectivity. Information
Technology in Biomedicine, IEEE Transactions on,
8(4), 405-414.
Kugsang, J., Eun-young, J., & Dong Kyun, P. (2009).
Trend of wireless u-Health. Paper presented at the
ISCIT 2009, Incheon, Korea.
Lymberis, A., & Olsson, S. (2003). Intelligent biomedical
clothing for personal health and disease management:
state of the art and future vision. Telemedicine Journal
and e-Health, 9(4), 379-386.
Ramaprasad, A. (2009). Ubiquitous Learning: An
Ontology. Ubiquitous Learning: An International
Journal, 1(1), 57-65.
Ramaprasad, A., Papagari, S. S., & Keeler, J. (2009).
eHealth: Transporting Information to Transform
Health Care. In L. Azevedo & A. R. Londral (Eds.),
Proceedings of HEALTHINF 2009 – Second
International Conference on Health Informatics (pp.
344-350). Porto, Portugal: INSTICC Press.
Ramaprasad, A., & Rai, A. (1996). Envisioning
management of information. Omega-International
Journal of Management Science, 24(2), 179-193.
Ramaprasad, A., Valenta, A., & Brooks, I. (2009).
Clinical and Translational Science Informatics:
Translating Information to Transform Health Care. In
L. Azevedo & A. R. Londral (Eds.), Proceedings of
HEALTHINF 2009 – Second International Conference
on Health Informatics. Porto, Portugal: INSTICC
Press.
Varshney, U. (2007). Pervasive healthcare and wireless
health monitoring. Mobile Networks and Applications,
12(2), 113-127.
Weagraff, S. (2005). The Case for Intelligent Agents
Preparing for the future of care. Paper presented at
the, International Conference on Computational
Intelligence for Modelling, Control and Automation,
2005 and International Conference on Intelligent
Agents, Web Technologies and Internet Commerce.
HEALTHINF 2011 - International Conference on Health Informatics
416
